Professional Documents
Culture Documents
Chapter 04
Chapter 04
Uploaded by
Jessica GonzalezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 04
Chapter 04
Uploaded by
Jessica GonzalezCopyright:
Available Formats
Chapter 4:
Legal and Ethical Aspects of Nursing
Types of Law and Examples
• Constitutional: Right to free speech
• Statutory: Nurse Practice Acts
• Administrative: State Boards of Nursing
• Criminal: Prosecution of malpractice
• Civil: HIPAA violations of privacy
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Legal Terminology
• Crime
– Deliberate commission of a forbidden act or omission
of an act required by law
• Felony
– Serious crime
• Misdemeanor
– Crime that is considered not as serious as a felony
but is still serious and may be cause for revocation of
a nursing license
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Legal Terminology (cont.)
• Liability
– Legal responsibility for one’s actions or failure to act
appropriately
• Tort
– Injury that occurred because of another person’s
intentional or unintentional actions or failure to act
• Negligence
– Harm done to a client as a result of neglecting duties,
procedures, or ordinary precautions
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Legal Terminology (cont.)
• Malpractice
– Professional negligence
• Assault
– Threat or an attempt to do bodily harm including
physical or verbal intimidation
• Battery
– Physical contact with another person without that
person’s consent
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Legal Terminology (cont.)
• Informed consent
– Tests, treatments, and medications are to be
explained, documented, and signed by client
• Libel
– Written statement or photograph that is false or
damaging
• Slander
– Malicious verbal statements that are false or injurious
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Question
Is the following statement true or false?
It is acceptable to give an injection to clients if they refuse,
and without their written consent.
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Answer
False
Giving an injection that the client refuses amounts to
battery, and hence is illegal. Moreover, the client or a legal
guardian must understand and sign the consent form for
care and treatment.
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Legal Issues of Nursing Practice
• False imprisonment
• Abandonment of care
• Invasion of privacy and confidentiality
– Trespassing
– Illegal search and seizure
– Releasing private information
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Nurse Practice Act
• The law that defines and regulates the practice of nursing
in the United States is called the Nurse Practice Act.
• These laws define the title of “nursing” and regulate the
many aspects of the field of nursing.
• The law or Nurse Practice Act in each state, province, or
territory defines regulations for practical and registered
nursing.
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Components of a Nurse Practice Act
• Definition of practical and registered nursing
• Nursing functions protected by the law
• Requirements for an approved school of nursing
• Establishment of requirements for licensure
• Process and procedures for becoming licensed
• Procedures for maintaining licensure and continuing
education
• Issue and renewal of nursing licenses
• Suspension, revocation, and reinstatement of license
• Interstate endorsement
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Functions of the State Board of Nursing
• The legislative power to initiate, regulate, and enforce
the provisions of the Nurse Practice Act is delegated to a
specific state agency often known as the State Board of
Nursing.
• Boards are subject to legal parameters, but usually they
have some leeway in interpreting aspects of the Nurse
Practice Act.
• In the recent past, the State Boards of Nursing were
responsible for the creation of the licensing examination,
however, now they are written by the National Council of
State Boards of Nursing.
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Precautions Against Lawsuits
• Follow accepted procedures.
• Be competent in your practice.
• Ask for assistance.
• Document well.
• Do not give legal advice to clients.
• Do not accept gifts.
• Do not help a client prepare a will.
• Consider a malpractice insurance policy.
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Question
Is the following statement true or false?
In the case of a client who is terminally ill, has no relatives
present, and requests help, a nurse has the authority to
help the client prepare a will or other legal document.
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Answer
False
A nurse should never attempt to help a client prepare a will
or any other legal document. A graduate nurse may be
asked to witness the signing of a will.
Copyright © 2017 Wolters Kluwer • All Rights Reserved
The Good Samaritan Act
• In effect in most states
• Protects a person from liability:
– if they give emergency care within the limits of first
aid
– if they act in a “reasonable and prudent manner”
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Professional Boundaries
• Power versus vulnerability
– Do not exploit the power to access private client
information
• Boundary crossings
– Questionable behavior
• Boundary violations
– Excessive personal disclosures
• Professional sexual misconduct
– Seductive, sexually demeaning, or harassing behavior
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Advance Directives
• Definition: a legal document in which a person either
states choices for medical treatment or names someone
to make treatment choices if he or she loses decision-
making ability
• Examples
– Living will
– Directive to healthcare providers
– Durable power of attorney for healthcare
– Mental health advance declaration
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Question
Is the following statement true or false?
If a client has a living will kept on file in the healthcare
facility, the nurse is forced to honor the will in the case of
the client being unable to make his own decisions regarding
care.
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Answer
True
A living will is a written and legally witnessed document
that requests no extraordinary measures to be taken to
save a person’s life in the event of terminal illness.
Healthcare providers and nurses are bound by the person’s
wishes.
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Deficient or Harmful Care
• People who are vulnerable to deficient or harmful care
include:
– Children and some adults
– Mentally incompetent or confused persons
– Elderly people
– People living in isolation
• The law protects vulnerable persons from injury, abuse,
or neglect while receiving care in a healthcare facility,
nursing home, school, or their own home.
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Brain Death
• Cessation of breathing after artificial ventilation is
discontinued
• Cessation of heartbeat without external stimuli
• Unresponsiveness to external stimuli
• Complete absence of cephalic reflexes
• Pupils fixed and dilated
• Irreversible cessation of all functions of the brain
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Biologic Death or Clinical Death
• Absence of respirations
• Absence of a heartbeat
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Ethical Issues in Treatment
• Organ transplantation
• Criteria and questions
• Refusal of treatment
• Withholding treatment
• Termination of treatment
• Euthanasia
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Rights and Responsibilities of Healthcare
Clients
• Clients’ Rights
– A Patient’s Bill of Rights
• Clients’ Responsibilities
– Clients are active participants in formulating their
care plan and making healthcare decisions, and have
a responsibility to participate in and cooperate with
care given.
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Provisions and Goals of the HIPAA
Legislation
• In 1996, the Health Insurance Portability and
Accountability Act (HIPAA), Title II, was passed and
serves as federal privacy regulation.
• The HIPAA, Title II act:
– Regulates who can have access to client information
– Sets standards for storage and transmission of client
information
– Requires that healthcare facilities write policies
allowing clients access to their own personal health
information. (The client has the right to request
correction of any errors.)
Copyright © 2017 Wolters Kluwer • All Rights Reserved
Impact of HIPPA on Nursing Care
• Nursing students or staff nurses will most likely be asked
to sign a HIPAA confidentiality statement each year which
certifies that they are familiar with HIPAA regulations and
will follow their guidelines.
• Violation of HIPAA privacy practices is cause for
termination of employment or of student status in most
facilities.
Copyright © 2017 Wolters Kluwer • All Rights Reserved
End of Presentation
Copyright © 2017 Wolters Kluwer • All Rights Reserved
You might also like
- Society in Focus An Introduction To Sociology 9th Edition Ebook PDF VersionDocument62 pagesSociety in Focus An Introduction To Sociology 9th Edition Ebook PDF Versionryan.riley589100% (41)
- Lecture 16 Introduction To Law & Ethics in Dentistry PDFDocument28 pagesLecture 16 Introduction To Law & Ethics in Dentistry PDFبروف فى اللغة الإنجليزية100% (2)
- Ethical and Legal Issues in Pediatric IcuDocument33 pagesEthical and Legal Issues in Pediatric IcuAnisha Mane67% (9)
- The Gift KritikDocument39 pagesThe Gift KritikCrystal Legionaires100% (1)
- Practical Guide To MSCEIT PDFDocument15 pagesPractical Guide To MSCEIT PDFbestateman50% (2)
- From Student To Graduate NurseDocument23 pagesFrom Student To Graduate NurseHannaNo ratings yet
- Chapter 9: Legal and Ethical IssuesDocument31 pagesChapter 9: Legal and Ethical IssuesAaron WallaceNo ratings yet
- Chapter 6 - Patient's Bill of Right and LawDocument27 pagesChapter 6 - Patient's Bill of Right and LawtenawNo ratings yet
- Psychiatric Nursing Notes: LegalDocument47 pagesPsychiatric Nursing Notes: Legalsurviving nursing schoolNo ratings yet
- Chapter 99Document19 pagesChapter 99HannaNo ratings yet
- Legal Psychiatric Nursing Issues Commitment IssuesDocument17 pagesLegal Psychiatric Nursing Issues Commitment IssuesBrandon Arete100% (1)
- Topic 5,6 Legal Aspects of Nursing Practice Acts - NPADocument28 pagesTopic 5,6 Legal Aspects of Nursing Practice Acts - NPA210411No ratings yet
- Week 5 PowerPointDocument11 pagesWeek 5 PowerPointMilan FantasyNo ratings yet
- Chapter 47Document30 pagesChapter 47Jessica GonzalezNo ratings yet
- EthicsDocument48 pagesEthicsTadesse Fenta100% (1)
- CH 09Document20 pagesCH 09api-3697326100% (1)
- Human Rights of Mentally IllDocument5 pagesHuman Rights of Mentally IllShyam100% (2)
- HEALTH STATUS-EC (Tactaquin, H.G.)Document15 pagesHEALTH STATUS-EC (Tactaquin, H.G.)KeepItSecretNo ratings yet
- Doctor Patient Relationship Muk March 2021Document28 pagesDoctor Patient Relationship Muk March 2021Deborah Chemutai100% (1)
- Legal Aspects of NursingDocument33 pagesLegal Aspects of NursingSathish Rajamani100% (5)
- Patient Rights, Informed Consent & Legal Considerations SDocument24 pagesPatient Rights, Informed Consent & Legal Considerations Smalaz husseinNo ratings yet
- Legal and Ethical Issues - GERIADocument33 pagesLegal and Ethical Issues - GERIAApril Mae Magos LabradorNo ratings yet
- Berman Ch04 Lecture 5Document44 pagesBerman Ch04 Lecture 5nabazlava1994No ratings yet
- Legal Issues Affecting MHN 2Document15 pagesLegal Issues Affecting MHN 2Christelle GarciaNo ratings yet
- Patient Rights and Their Limitations - 2013Document23 pagesPatient Rights and Their Limitations - 2013Alberto MayorgaNo ratings yet
- 2 Legal Aspects of GerontologicalNursingDocument27 pages2 Legal Aspects of GerontologicalNursingKate Angel AlbarinaNo ratings yet
- History & Evolution of Medical Ethics and Duties of Doctors & the MDCNDocument31 pagesHistory & Evolution of Medical Ethics and Duties of Doctors & the MDCNScholastica ChinazoNo ratings yet
- Autistic Self Advocacy Network Webinar With Autism NOW July 29 2014Document28 pagesAutistic Self Advocacy Network Webinar With Autism NOW July 29 2014The Autism NOW CenterNo ratings yet
- Legal Issues in Psychiatric NursingDocument24 pagesLegal Issues in Psychiatric NursingRic TinNo ratings yet
- Ethico-Legal Dilemmas Inc Critical CareDocument32 pagesEthico-Legal Dilemmas Inc Critical CareAlexander Blanche PajelaNo ratings yet
- Nursing+Laws+2021+1 1+session+Ethics,+COE+othersDocument65 pagesNursing+Laws+2021+1 1+session+Ethics,+COE+othersjay kusainNo ratings yet
- Challenges To Effective Drug TherapyDocument16 pagesChallenges To Effective Drug TherapyedemcantosumjiNo ratings yet
- DR - AC Ethical and Legal Issues in Midwifery Practice 2021Document91 pagesDR - AC Ethical and Legal Issues in Midwifery Practice 2021dr.anu RkNo ratings yet
- 6 - Ethics, Morality and LawDocument40 pages6 - Ethics, Morality and LawAubrey Princess F. CaceresNo ratings yet
- MODULE 4 Clinical Judgment Lecture 2017 (Autosaved)Document33 pagesMODULE 4 Clinical Judgment Lecture 2017 (Autosaved)william NgassaNo ratings yet
- Human RightsDocument112 pagesHuman RightsAKHILA PKNo ratings yet
- After The Diagnosis (Leslie Fried)Document26 pagesAfter The Diagnosis (Leslie Fried)National Press FoundationNo ratings yet
- The Nursing Process in Drug Therapy and Patient Safety The Nursing Process in Drug Therapy and Patient SafetyDocument18 pagesThe Nursing Process in Drug Therapy and Patient Safety The Nursing Process in Drug Therapy and Patient SafetyJay Clarrise Enteria ErlanoNo ratings yet
- Patients-Rights-Advocacy-in-California-2023Document13 pagesPatients-Rights-Advocacy-in-California-2023CARTERS TECHNOLOGYNo ratings yet
- CM3 - Cu19 Relevant Ethico-Legal Guidelines in Conducting Health AssessmentDocument11 pagesCM3 - Cu19 Relevant Ethico-Legal Guidelines in Conducting Health AssessmentMARY ANNE JUDE ANTHONY100% (2)
- 2 PPT - CH - 03 Copy Decision MakingDocument30 pages2 PPT - CH - 03 Copy Decision MakingSultan SalmanNo ratings yet
- Chapter 5: Legal Issues: Keltner: Psychiatric Nursing, 5 EditionDocument7 pagesChapter 5: Legal Issues: Keltner: Psychiatric Nursing, 5 EditionWarrenPeaceNo ratings yet
- Bioethics ppt2Document43 pagesBioethics ppt2Parthik SojitraNo ratings yet
- Chapter 5 - Medico-Legal IssuesDocument27 pagesChapter 5 - Medico-Legal IssuesLalita A/P AnbarasenNo ratings yet
- 2074 Ethics and Legal Aspect of NursingDocument66 pages2074 Ethics and Legal Aspect of NursingSanjeev MehtaNo ratings yet
- Standards of PsychiatricDocument16 pagesStandards of PsychiatricBrandon AreteNo ratings yet
- Patient's Bill of RightsDocument5 pagesPatient's Bill of RightsSanidad Yani BelNo ratings yet
- Legalandethicalissuesincriticalcarenursing 130411224544 Phpapp02Document33 pagesLegalandethicalissuesincriticalcarenursing 130411224544 Phpapp02Guna RamyaNo ratings yet
- Nursing Jurisprudence - For UploadDocument290 pagesNursing Jurisprudence - For UploadBing58No ratings yet
- Ethico Legal Dilemmas in Critical Care NursingDocument36 pagesEthico Legal Dilemmas in Critical Care NursingNica Marie LumbaNo ratings yet
- Legal Ethics 1Document71 pagesLegal Ethics 1marionchepkirui63No ratings yet
- Ethico Legal CONSIDERATIONS IN Health AssessmentDocument6 pagesEthico Legal CONSIDERATIONS IN Health AssessmentAl Brian SepulvidaNo ratings yet
- Ethico-Legal Considerations in The Care of Older AdultDocument25 pagesEthico-Legal Considerations in The Care of Older AdultMarlone James OcenaNo ratings yet
- Malpraktik Dan Kelalaian MedisDocument33 pagesMalpraktik Dan Kelalaian MedisRey AlwiwikhNo ratings yet
- HIPAA Privacy and Security RulesDocument83 pagesHIPAA Privacy and Security RulessemarmendemxNo ratings yet
- Hipaa: Health Insurance Portability and Accountability ActDocument40 pagesHipaa: Health Insurance Portability and Accountability Actkajal raj100% (1)
- Legal Aspects of Gerontological NursingDocument19 pagesLegal Aspects of Gerontological NursingRodjski MangNo ratings yet
- Ethical-Legal Principles and IssuesDocument12 pagesEthical-Legal Principles and IssuesKhibul LimNo ratings yet
- CH 7. The Health Professional-Patient RelationshipDocument11 pagesCH 7. The Health Professional-Patient Relationshipaberhaneth1163No ratings yet
- FKU-5. Praktis Hukum Kedokteran Di IndonesiaDocument60 pagesFKU-5. Praktis Hukum Kedokteran Di IndonesiaEphineNo ratings yet
- Dr. Jayesh Patidar: PHD., M.Sc. Nursing, Mba Asst. Professor Joitiba College of Nursing, BhanduDocument33 pagesDr. Jayesh Patidar: PHD., M.Sc. Nursing, Mba Asst. Professor Joitiba College of Nursing, BhanduAnonymous XunfAgd2BNo ratings yet
- The Empowered Patient: Navigating the Healthcare System with ConfidenceFrom EverandThe Empowered Patient: Navigating the Healthcare System with ConfidenceNo ratings yet
- Anal Sex Basics (Carlyle Jansen)Document222 pagesAnal Sex Basics (Carlyle Jansen)huora100% (2)
- Glasgow 12-Lead ECG Analysis Program Statement of Validation and Accuracy 3302436.ADocument32 pagesGlasgow 12-Lead ECG Analysis Program Statement of Validation and Accuracy 3302436.AKiattisak PrajongsinNo ratings yet
- Ncp1 317rle Ronquillo BryanDocument2 pagesNcp1 317rle Ronquillo BryanPaul AnteNo ratings yet
- More Reasons To Avoid Beyond Fake Meat PDFDocument8 pagesMore Reasons To Avoid Beyond Fake Meat PDFRocco LamponeNo ratings yet
- Temporary Student Hub - Request LetterDocument3 pagesTemporary Student Hub - Request LetterJeofy PamaNo ratings yet
- FLCCC Summary of The Evidence of Ivermectin in COVID 19Document3 pagesFLCCC Summary of The Evidence of Ivermectin in COVID 19Muhamad ZaidNo ratings yet
- Medical RecordDocument8 pagesMedical RecordKusumadewi WidiarsaNo ratings yet
- The Family and Family Structure Classification Red 2 PDFDocument5 pagesThe Family and Family Structure Classification Red 2 PDFHawraa ThamirNo ratings yet
- Peak Flow Meter 3Document7 pagesPeak Flow Meter 3Anushree DatarNo ratings yet
- Factors Affecting The Activity of Health Caders in The Discovery of Tuberculosis Cases in Kelurahan Sonorejo SukoharjoDocument7 pagesFactors Affecting The Activity of Health Caders in The Discovery of Tuberculosis Cases in Kelurahan Sonorejo SukoharjoIntan AyuNo ratings yet
- Literacy, Health Education, Health Literacy and Health Outcomes - How Do They Fit?Document24 pagesLiteracy, Health Education, Health Literacy and Health Outcomes - How Do They Fit?qwerty123No ratings yet
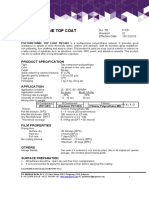
- Finish Epoxy Propan PUT-603Document2 pagesFinish Epoxy Propan PUT-603Yusuf KhoirNo ratings yet
- ECS HFC-227ea - Owner's Manual - February 2001-06-236118-001 - Rev - AADocument36 pagesECS HFC-227ea - Owner's Manual - February 2001-06-236118-001 - Rev - AAgilangolandiaNo ratings yet
- Occupational Safety and Health Risk Assessment of Workers in The Manufacturing IndustryDocument15 pagesOccupational Safety and Health Risk Assessment of Workers in The Manufacturing IndustryCj SesnorioNo ratings yet
- Brochure BOP PODDocument4 pagesBrochure BOP PODtkthird siaminterNo ratings yet
- OPD Group Insurance PolicyDocument26 pagesOPD Group Insurance PolicyRakshith RaghuNo ratings yet
- Shatavari FDocument22 pagesShatavari FAPNEET100% (1)
- How To Remove Gallstones NaturallyDocument11 pagesHow To Remove Gallstones NaturallyRichard Bersola Estonilo100% (4)
- Physical Fitness Short Note (SPSC 1011) Unit One 1. 1. Concepts of Physical Fitness1 1.1. 1. Meanings and Definitions of Physical FitnessDocument62 pagesPhysical Fitness Short Note (SPSC 1011) Unit One 1. 1. Concepts of Physical Fitness1 1.1. 1. Meanings and Definitions of Physical Fitnesseyob astatkeNo ratings yet
- Clinical Face Sheet: - A.M. - P.M. - A.M. - P.MDocument15 pagesClinical Face Sheet: - A.M. - P.M. - A.M. - P.MNikitaCaitlynLeyaleyNo ratings yet
- Unit 11 - Late AdulthoodDocument14 pagesUnit 11 - Late AdulthoodEvet VaxbmNo ratings yet
- Lifting Plan FF - Sprinkler ActivitiesDocument9 pagesLifting Plan FF - Sprinkler ActivitiesFMU KSANo ratings yet
- AzathioprineDocument3 pagesAzathioprinesky.blueNo ratings yet
- Makalah PublikasiDocument35 pagesMakalah PublikasiCERITA SEROJANo ratings yet
- Mastering Leadership and Supervisory SkillsDocument4 pagesMastering Leadership and Supervisory SkillsRysse ZvanNo ratings yet
- Clinical Education: Interpretation of AbgsDocument8 pagesClinical Education: Interpretation of AbgsRumela Ganguly ChakrabortyNo ratings yet
- CooperativeDocument2 pagesCooperativeJ SwishNo ratings yet