100% found this document useful (2 votes)
354 views14 pagesStomach Cancer Seminar Overview
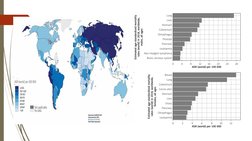
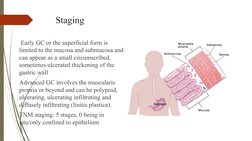
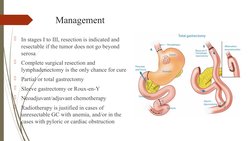
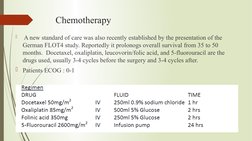
Stomach cancer, also known as gastric cancer, is the fifth most common cancer worldwide and the third leading cause of cancer death. Risk factors include infection with Helicobacter pylori bacteria, smoking, and alcohol consumption. Most stomach cancers are adenocarcinomas, which develop through a process associated with H. pylori infection, inflammation, and cellular changes over many years. Symptoms often do not appear until the cancer has spread, but may include digestion problems, weight loss, and bleeding. Screening, biopsy, and imaging tests are used to diagnose stomach cancer and determine if it has spread. Treatment depends on the stage but may involve surgery, chemotherapy, and targeted therapies.
Uploaded by
Lamy SCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
100% found this document useful (2 votes)
354 views14 pagesStomach Cancer Seminar Overview
Stomach cancer, also known as gastric cancer, is the fifth most common cancer worldwide and the third leading cause of cancer death. Risk factors include infection with Helicobacter pylori bacteria, smoking, and alcohol consumption. Most stomach cancers are adenocarcinomas, which develop through a process associated with H. pylori infection, inflammation, and cellular changes over many years. Symptoms often do not appear until the cancer has spread, but may include digestion problems, weight loss, and bleeding. Screening, biopsy, and imaging tests are used to diagnose stomach cancer and determine if it has spread. Treatment depends on the stage but may involve surgery, chemotherapy, and targeted therapies.
Uploaded by
Lamy SCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd