Professional Documents
Culture Documents
Dka and HHS
Uploaded by
Mouhammad Dawoud100%(2)100% found this document useful (2 votes)
137 views25 pagesDKA and HHS done by dr. Mohamad dawoud
Original Title
DKA AND HHS
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentDKA and HHS done by dr. Mohamad dawoud
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
100%(2)100% found this document useful (2 votes)
137 views25 pagesDka and HHS
Uploaded by
Mouhammad DawoudDKA and HHS done by dr. Mohamad dawoud
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 25
DIABETIC KETOACIDOSIS
Dr. Mohamad dawoud.
DKA
• Diabetic ketoacidosis(DKA) is an acute, life
threatening complication of DM characterized
by hyperglycemia , ketoacidosis and ketonuria.
• Occurs when absolute or relative insuline
deficiency inhibits the ability of glucose to
enter cells for utilization as metabolic fuel.
• After that the liver rapidly begin the process of
breaking down of fat into ketones to employ as
a fuel source.
• Overproduction of ketones ensues, causing
them to accumulate in the blood and urine
and they turn the blood acidic.
• DKA commonly occurs in patients with type 1
DM.
etiology
• Lack of or insufficient insulin replacement therapy:
– Undiagnosed, untreated diabetes mellitus
– Treatment failure in known diabetics: insulin pump failure,
forgotten insulin injection, noncompliance with insulin therapy.
• Increased insulin demand
– Stress: infections, surgery, trauma, myocardial infarction.
– Drugs: glucocorticoid therapy, cocaine use, alcohol abuse.
• In 30% of DKA presented cases are mostly precipitation of
infections ( pneumonia, UTI…) especially in the elderly
populations.
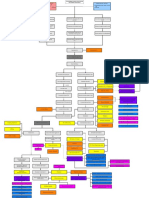
Pathophysiology of DKA.
• Osmotic diuresis and hypovolemia
• Insulin normally elevates cellular uptake of glucose
from the blood.
• In the insulin-deficient state
of DKA, hyperglycemia occurs.
• Hyperglycemia, in turn, leads to progressive volume
depletion via osmotic diuresis.
• Insulin deficiency
→ hyperglycemia → hyperosmolality → osmotic
diuresis and loss of electrolytes → hypovolemia.
PATOPHYSIOLOGY OF DKA
• Metabolic acidosis with increased anion gap.
• Insulin deficiency also increases fat breakdown (lipolysis).
• Metabolic acidosis develops as the free fatty acids generated by lipolysis
become ketones, two of which are acidic (acetoacetic acid and beta-
hydroxybutyric acid).
• Serum bicarbonate is consumed as a buffer for the
acidic ketones. Metabolic acidosis with an elevated anion gap is therefore
characteristic of DKA.
• Insulin deficiency → ↑ lipolysis → ↑ free fatty
acids → hepatic ketone production (ketogenesis) → ketosis→ bicarbonate
consumption (as a buffer) → anion gap metabolic acidosis.
• Extracellular potassium shift because of the overall loss of potassium in
urine; A total body potassium deficit occurs but the level of k+ in the blood
is normal even elevated!
Clinical features
• Polyuria.
• Polydipsia.
• Nausea and vomiting.
• Signs and symptoms of dehydration: dry
mucous membrane, hypotension, decreased
skin turgor.
• Neurological abnormalities:
Altered mental status/lethargy/ coma.
Other specific findings in the DKA:
• Fruity smell from the mouth.
• Rapid onset (<24h).
• Hyperventilation: long, deep breath
(kussmaul’s breathing).
• Abdominal pain.
diagnostics
• Check serum glucose to confirm hyperglycemia.
• Check BMP for serum bicarbonate, anion gap, electrolytes,
and renal function.
• Check for the presence of ketones.
– Urine ketones: Standard urine dipstick assays detect acetoacetate
and acetone but not beta-hydroxybutyrate.
– Serum beta-hydroxybutyrate.
• Check blood gas analysis for pH.
• Diagnostic workup to evaluate the underlying
cause: HbA1c, CBC, ECG, infectious workup.
Electrolytes and renal function in DKA.
• Sodium:
– Hyponatremia is common in both DKA and HHS, due
to hypovolemic hyponatremia
– and hypertonic hyponatremia
– Always check corrected sodium for hyperglycemia.
• Potassium in DKA: normal or elevated (despite a total body
deficit)
• Magnesium levels are typically low.
• Phosphorus levels may be falsely elevated despite a total
body deficit.
• BUN and creatinine are often elevated.
Additional diagnostic workup
• HBA1C
• CBC
• Blood and urine culture.
• Serum lactate.
• Chest x-ray
• Monitor ECG And troponin for cardiac
ischemia.
management
• IV access with two large-bore peripheral IV lines
• Assess the severity of DKA.
• Fluid resuscitation: initially with isotonic saline (0.9%
NaCl), then 0.45% or 0.9% depending on corrected serum
sodium
• Electrolyte repletion (especially potassium)
• Short-acting insulin(regular insulin) therapy
• IV bicarbonate (only in severe metabolic acidosis)
• Identify and treat the underlying cause.
• Consider admission to the ICU.
• First hour with IV repletion: 0.9% Nacl at 15-
20 ml/kg/h.
• Potassium should be >3.3mEq/l before
insuline initiation.
• Maintain potassium level between 4-5mEq/l.
• Recommended regimen of insulin is:
Regular insulin bolus followed by continuous
regular insulin.
Hyperglycemic hyperosmolar state(HHS).
• Is a life threatening condition present
commonly in patients with type 2 DM; it has
a higher mortality rate reaching 5-10%.
• Previously was called hyperosmolar
hyperglycemic coma(HHNC) , terminology
was changed because coma was found in less
than 20%.
etiology
• Present in patients with type 2 DM who have
concomittant illness that reduce fluid intake .
• Infection is the most common cause.
• Stroke and MI
• Some drugs as glucocorticoids, cocaine, and
alcohol abuse.
• Non compliance with oral hypoglycemics or
insulin therapy.
pathophysiology
• The pathophysiology of HHS is similar to that
of DKA.
• However, in HHS, there are still small amounts
of insulin being secreted by the pancreas, and this is
sufficient to prevent DKA by
suppressing lipolysis and, in turn, ketogenesis.
• HHS is characterized by symptoms
of marked dehydration (and loss of electrolytes)
due to the
predominating hyperglycemia and osmotic diuresis
Clinical features
DKA HHS
DM TYPE 1 TYPE 2
HISTORY OF SEVERE STRESS , + +
ILLNESS, HOSPITALIZATION
POLYURIA , POLYDIPSIA + +
NAUSEA, VOMITING + +/-
DEHYDRATION + SEVERE
ALTERED MENTAL STATUS POSSIBLE POSSIBLE
HYPERVENTILATION + -
FRUITY SMELL + -
ONSET RAPID(<24h) INSIDIOUS(DAYS)
DIAGNOSTICS
• Plasma glucose level of 600mg/dl or greater.
• Effective serum osmolality of 320mOsm/kg or
greater.
• Profound dehydration up to 9L.
• Bicarbonate concentration greater than
15mEq/L.
• Small ketonuria and low to absent ketonemia.
• Serum PH >7.3
• Some alterations in consciousness.
• Imaging studies include:
• CXR, abdominal x-ray if patient has abdominal pain or
is vomiting.
• CT brain indicated in patients with focal or global
neurologic changes to exclude hemorrhagic strokes,
subdural hematoma, subarachnoid bleeding..
• ECG rule out ischemia and MI.
• CSF cell count, glucose, protein, and culture in patient
with suspected meningitis.
Difference in lab test between DKA AND HHS
Lab test DKA HHS
GLUCOSE <600mg/dL >600mg/dl
BICARBONATE <18 mEq/l >18mEq/l
ANION GAP Elevated >10 mmol/l Normal <10
URINALYSIS Normal large ketones in Absence of ketones in
urine urine
glucosuria glucosuria
SERUM BETA- elevated normal
HYDROYBUTYRATE
BLOOD GAS PH<7.3 PH>7.3
SERUM OSMOLALITY normal Elevated >320mOsm/kg
MANAGEMENT
• Fluid resuscitation: First line treatment of
patients with HHS is IV crystalloids with 2 large
bores to rehydrate the patient. Isotonic solution
0,9% is usually used first 1 hour of admission at
15-20 ml/kg/h.
• Check for corrected sodium :
If sodium >135mEq/l then 0.45% Nacl is used.
If sodium <15 mEq/l then 0.9% is used.
• Acute management of airway in altered mental status
patient is essential and a first step to maintain patient life
, patient may be mechanically ventilated to support
respiration and prevent arrest.
• IV rapid insulin infusion is needed to decrease blood
glucose and osmotic pressure, although some patient may
not needed after IV fluid resuscitation.
• Always correction of potassium is of high importance
before insulin administration because of the depletion of
intracellular level of potassium even if the level of
potassium is within normal range.
According to American Diabetes association
recommendations:
• If hypokalemia ( k<3.3 mEq/l) has been excluded,
an IV bolus of regular insulin of 0.1U/kg/h should
be administered.
• Continuous insulin infusion of 0.1U/kg/h.
• Monitor blood glucose every hour.
• Continue IV insulin at a goal glucose level of 250-
300mg/dl.
• Electrolytes replacement and potassium replenish
if k<3.3 at first line before insulin infusion.
• Other electrolytes as Mg , P , and Ca are not routinely
replineshed , only in case of severe decrease could be
added.
• Diagnostics and treatment of the underlying cause
responsible for HHS developpment in the diabetic patient
as pneumonia , UTI and treatment with antibiotics.
• Adjustment of the insuline regimen of the patient if
needed or hypoglycemic drugs with maintaining of
normal diet and physical activity after discharge and
regular follow up.
You might also like
- Mark Klimek NotesDocument50 pagesMark Klimek NotesLisette50% (2)
- Kids Nutrition Guide Low v3 PDFDocument63 pagesKids Nutrition Guide Low v3 PDFanon_851515090100% (1)
- PancreatitisDocument59 pagesPancreatitisAarif RanaNo ratings yet
- CBT - Emergency Medicine EditedDocument14 pagesCBT - Emergency Medicine Editedchristy INo ratings yet
- Hypertensive DrugsDocument2 pagesHypertensive DrugsNedaAbdullahNo ratings yet
- High Blood Pressure GuideDocument4 pagesHigh Blood Pressure GuideKhaira CharmagneNo ratings yet
- ACCPCritical Care Medicine Board ReviewDocument491 pagesACCPCritical Care Medicine Board ReviewdianaMDNo ratings yet
- Neonatal Hyperglycemia1Document17 pagesNeonatal Hyperglycemia1Abhinav Mitra VatsNo ratings yet
- Wound AssessmentDocument19 pagesWound Assessmentdrsonuchawla100% (1)
- Diabetes Mellitus Type 2Document16 pagesDiabetes Mellitus Type 2MTs MIFDANo ratings yet
- Diabetic Ketoacidosis (DKA)Document33 pagesDiabetic Ketoacidosis (DKA)Eric Chye Teck100% (1)
- Shock & Fluid TherapyDocument57 pagesShock & Fluid Therapyarnol3090No ratings yet
- Type 2 Diabetes ExplainedDocument11 pagesType 2 Diabetes ExplainedHafiz IbrahimNo ratings yet
- Wilson S DiseaseDocument28 pagesWilson S DiseasemichaelcylNo ratings yet
- Emergency Diabetes 2023 - Septian Mixrova SebayangDocument30 pagesEmergency Diabetes 2023 - Septian Mixrova SebayangFiqri DzulfaqqorNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Acid - Base Balance & Abg AnalysisDocument71 pagesAcid - Base Balance & Abg AnalysisMohan KrishnaNo ratings yet
- Diabetic Ketoacidosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandDiabetic Ketoacidosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Pink Panther - Diabetes Management - Chapter 4Document8 pagesPink Panther - Diabetes Management - Chapter 4jennmoyerNo ratings yet
- Management of diabetic ketoacidosis: principles of management in the first hourDocument13 pagesManagement of diabetic ketoacidosis: principles of management in the first hourAzim Abd Razak100% (1)
- Drug Study Er MedsDocument12 pagesDrug Study Er MedsJerald S. OlaloNo ratings yet
- Diabetes Types, Causes, Symptoms & TreatmentDocument8 pagesDiabetes Types, Causes, Symptoms & TreatmentAradhanaRamchandaniNo ratings yet
- Thyroid StormDocument23 pagesThyroid Stormtogi_siahaanNo ratings yet
- TCA Suppression and DM1Document22 pagesTCA Suppression and DM1Rubyrose TagumNo ratings yet
- Pre Final Exam NCM 118Document26 pagesPre Final Exam NCM 118Faith BugtongNo ratings yet
- Inp RbeDocument13 pagesInp RbeAllaiza CristilleNo ratings yet
- Hyperosmolar Hyperglycemic Nonketotic Syndrome HHNSDocument12 pagesHyperosmolar Hyperglycemic Nonketotic Syndrome HHNSKyle Ü D. CunanersNo ratings yet
- NCP - Gestational DiabetesDocument2 pagesNCP - Gestational DiabetesKailah Rose CabantoyNo ratings yet
- Overview of Nephrotic SyndromeDocument19 pagesOverview of Nephrotic Syndromefarmasi_hm100% (1)
- Nutrition Support in Critically Ill PatientDocument19 pagesNutrition Support in Critically Ill PatienttantoNo ratings yet
- Insulin, Oral Hypoglycaemic Agents, GlucagonDocument63 pagesInsulin, Oral Hypoglycaemic Agents, GlucagonBhavesh kunvarNo ratings yet
- Dka Vs Hhs Edit 1Document25 pagesDka Vs Hhs Edit 1Razeen RiyasatNo ratings yet
- 3a Emergency Care DKA (UK) FINALDocument40 pages3a Emergency Care DKA (UK) FINALDrsarfaraz SiddiquiNo ratings yet
- Type 1 Diabetes: Diabetic Ketoacidos ISDocument16 pagesType 1 Diabetes: Diabetic Ketoacidos ISapi-551073862No ratings yet
- DKA Canadian ProtocolDocument2 pagesDKA Canadian Protocolplay_wright2084No ratings yet
- Hyperglycemic Hyperosmolar StateDocument17 pagesHyperglycemic Hyperosmolar StateAqila Mumtaz50% (2)
- DKA Emergency Management GuideDocument18 pagesDKA Emergency Management GuideDr. Mamunul AbedinNo ratings yet
- Hypertensive Emergencies: Sulaiman Usaid G. MBCHB V Facilatator: DR Jack TDocument44 pagesHypertensive Emergencies: Sulaiman Usaid G. MBCHB V Facilatator: DR Jack TUsaid SulaimanNo ratings yet
- DKA and HHSDocument16 pagesDKA and HHSGepengCungkringNo ratings yet
- DKADocument6 pagesDKAtiffarub91% (11)
- 4.1agents For Hyperuricemia GoutDocument4 pages4.1agents For Hyperuricemia GoutjohntrueNo ratings yet
- HHNK and DkaDocument4 pagesHHNK and Dkagoya100% (1)
- Dka GuidelineDocument16 pagesDka GuidelineGhada HusseinNo ratings yet
- Diabetes Problem Based Learning PDFDocument6 pagesDiabetes Problem Based Learning PDFIfantri Pramana100% (1)
- DKADocument12 pagesDKAAisha SyedNo ratings yet
- Diabetic Ketoacidosis (D.K.A) Beaumont Hospital Protocol: DiagnosisDocument1 pageDiabetic Ketoacidosis (D.K.A) Beaumont Hospital Protocol: Diagnosislouglee9174100% (1)
- Management of Hyperkalaemia and HypokalaemiaDocument21 pagesManagement of Hyperkalaemia and Hypokalaemiaferoza97No ratings yet
- Hypomagnesemia Mcqs PDFDocument7 pagesHypomagnesemia Mcqs PDFSyed Ali AkbarNo ratings yet
- Case StudyDocument6 pagesCase Studyapi-276551783No ratings yet
- Thyrotoxicosis: Giridhar MF 9 TermDocument19 pagesThyrotoxicosis: Giridhar MF 9 TermGiridhar MFNo ratings yet
- Diabetic KetoacidosisDocument5 pagesDiabetic Ketoacidosislpickering33No ratings yet
- Diabetic KetoacidosisDocument41 pagesDiabetic KetoacidosisllaychinNo ratings yet
- Acute Glomerulonephritis in ChildrenDocument6 pagesAcute Glomerulonephritis in ChildrenAnsu MaliyakalNo ratings yet
- DKA Draft 1 AM - Drawio 2Document1 pageDKA Draft 1 AM - Drawio 2Dud AccNo ratings yet
- HTN EmergencyDocument11 pagesHTN EmergencyKaran ChhabraNo ratings yet
- Isotonic Saline (0.9%Nacl-Normal Saline) IndicationDocument3 pagesIsotonic Saline (0.9%Nacl-Normal Saline) IndicationJared AllenNo ratings yet
- Quiz 2 Study Guide - SHOCK!!! 25 Questions READ BOOK!!! Know Charts Esp. Stages of Shock ChartDocument1 pageQuiz 2 Study Guide - SHOCK!!! 25 Questions READ BOOK!!! Know Charts Esp. Stages of Shock Chartjenn1722No ratings yet
- Hyperosmolar Hyperglycemic State (HHS)Document21 pagesHyperosmolar Hyperglycemic State (HHS)Malueth AnguiNo ratings yet
- Diabetic KetoacidosisDocument10 pagesDiabetic KetoacidosisdhanasundariNo ratings yet
- Euglycemic DkaDocument15 pagesEuglycemic DkaVemuri SrinivasNo ratings yet
- Euglycemic KetoacidosisDocument7 pagesEuglycemic KetoacidosisMuhammad BilalNo ratings yet
- Clinical Order Set DKA AdultDocument2 pagesClinical Order Set DKA AdultBashar Al-HamaidehNo ratings yet
- Hyper para Thyroid Is MDocument27 pagesHyper para Thyroid Is MIbrahimWagesNo ratings yet
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycaemic StateDocument55 pagesDiabetic Ketoacidosis and Hyperosmolar Hyperglycaemic StateEva PrimanandaNo ratings yet
- Diabetic Ketoacidosis in PaediatricDocument11 pagesDiabetic Ketoacidosis in PaediatricSana Anam JahanNo ratings yet
- Hyperglycemia Crisis: Dr. Netty NurnaningtyasDocument34 pagesHyperglycemia Crisis: Dr. Netty Nurnaningtyasnetty nurnaningtyasNo ratings yet
- Normocytic Anemia'sDocument14 pagesNormocytic Anemia'sbrown_chocolate87643No ratings yet
- Diabetic Ketoacidosis:: Evidence Based ReviewDocument4 pagesDiabetic Ketoacidosis:: Evidence Based ReviewgracedumaNo ratings yet
- HESI CASE STUDY - Gestational DiabetesDocument17 pagesHESI CASE STUDY - Gestational DiabetesDrSandHill67% (6)
- Ccle Mid002Document23 pagesCcle Mid002Frankenstein MelancholyNo ratings yet
- Accommodation Management 5th Sem. Notes by Kirti PuriDocument25 pagesAccommodation Management 5th Sem. Notes by Kirti PuriAmit MondalNo ratings yet
- JDM Care PlanDocument5 pagesJDM Care PlangopscharanNo ratings yet
- Sick EnoughDocument49 pagesSick EnoughErendira SierraNo ratings yet
- Simplify Insulin Therapy With Co-FormulationDocument26 pagesSimplify Insulin Therapy With Co-FormulationNatasha LaurentiaNo ratings yet
- Edukasi Pengaturan Diet Pasien DMDocument6 pagesEdukasi Pengaturan Diet Pasien DMMWMaramis ChannelNo ratings yet
- Comp - Appraisal Pre Final Assignment 2Document32 pagesComp - Appraisal Pre Final Assignment 2Joanne Bernadette AguilarNo ratings yet
- Rajiv Gandhi University of Health Sciences Karnataka, Bangalore (PDFDrive)Document131 pagesRajiv Gandhi University of Health Sciences Karnataka, Bangalore (PDFDrive)GhhNo ratings yet
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults: TreatmentDocument35 pagesDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults: TreatmentyorghiLNo ratings yet
- Download ebook Endocrine Secrets Pdf full chapter pdfDocument67 pagesDownload ebook Endocrine Secrets Pdf full chapter pdfjason.green261100% (23)
- MSD High Risk Medications Inpatient SettingDocument49 pagesMSD High Risk Medications Inpatient SettingAGUSTINA KNo ratings yet
- Metformin GlucophageDocument1 pageMetformin GlucophageENo ratings yet
- Cobio S50 For VetDocument15 pagesCobio S50 For VetLesterGonzagaNo ratings yet
- Presentation Indonesia Sep 8 2022Document88 pagesPresentation Indonesia Sep 8 2022yuni chanNo ratings yet
- Cebu Normal University: Progress ReportDocument4 pagesCebu Normal University: Progress ReportKaren T. CeletariaNo ratings yet
- Diagnosis and Treatment of Diabetes Mellitus in Chronic PancreatitisDocument7 pagesDiagnosis and Treatment of Diabetes Mellitus in Chronic PancreatitisFarid TaufiqNo ratings yet
- Unit 4: Medical EmergenciesDocument44 pagesUnit 4: Medical EmergenciesMR々๛ AKMツNo ratings yet
- Functional-Foods Use A Novel Dietary Regimen For Type 2 Diabetes Treatment and ManagementDocument6 pagesFunctional-Foods Use A Novel Dietary Regimen For Type 2 Diabetes Treatment and ManagementInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 15.2. Fischer Projections of MonosaccharidesDocument19 pages15.2. Fischer Projections of Monosaccharideszebzeb STEMANo ratings yet