Professional Documents
Culture Documents
I & o
Uploaded by
sara0 ratings0% found this document useful (0 votes)
10 views20 pagesOriginal Title
I & O
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
10 views20 pagesI & o
Uploaded by
saraCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 20
I&O
O Nutrition Assessment reviewed previously
O Weigh/measure patient as ordered
O Scales vs Bed Scales
O Stimulate Appetite
O Small, frequent meals
O Food preferences; rituals
O Encouragement and pleasant environment
O Attractive foods
O Schedule procedures/meds to not interfere with meals; order
late tray if needed
O Control pain, nausea, depression
O Offer alternatives
O Good oral hygiene; comfort
O Remove clutter and free environment of irritating odors
O Arrange tray/set up meals (open packets, etc)
Assisting with Eating
Identify diet ordered!!
O Involve
O Sit at eye level
O Engage patient in conversation
O Napkin, no bib
O Straws and eating utensils
O Glasses and dentures in use
O For visually impaired (explain placement of foods,
compartment plates, similar locations each meal)
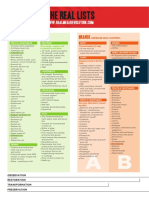
Diets
O Clear Liquid: liquid at room temp; able to see through
O Full Liquid: may have clear liquids + (milk and milk
drinks, puddings, custards, etc)
O Soft Diets: low in fiber and lightly seasoned
O Restricted diets: fat, NA, etc.
O Pureed Diets: blenderized
O Mechanical Soft Diets: regular with texture modifications
O NPO: good oral hygiene, ice chips, discourage eating in
front of patient, alternate activities at mealtimes
Urinary Elimination
O Micturition: process of emptying bladder
O Assess urine for: color, odor, clarity, and presence
of sediment
O Measure U/O
O Ask patient to void in bedpan, urinal, or specimen
hat
O Pour into measuring device
O Flat surface; measure in milliliters
O Record
O Discard
Measuring U/O
O Incontinent: difficult to measure; record number
of times. If precise measurement necessary, may
collaborate with provider for options (catheter)
O Consider toileting q2 hours to attempt to catch
urine
O Indwelling catheter: gloves; measuring device;
place under drainage spout; open clamp; empty
drainage bag; place measuring device on flat
surface; record; discard urine.
Bed Pans and Urinal
Drainage Bag for Indwelling
Catheter
Promoting Normal Urination
O Maintain normal voiding habits
O Promoting fluid intake
O Strengthening muscle tone
O Assisting with toileting
O Schedule
O Urge to void
O Privacy
O Positioning
O Hygiene
Types of Urinary Incontinence
O Stress— because of intraabdominal pressure (pregnancy)
O Urge—
O Mixed—
O Overflow— too much urine in bladder
O Functional— you cant get to the bathroom
O Reflex— neurogenic bladder, spasms
O Total— cant control anything, can be due to a mix of things
Urinary Diversion:
Suprapubic catheter
Urinary Diversion:
Ileal Conduit
Bowel Elimination
O Soft formed brown Q 1-3 days
O Characteristics of Stool Table 38.1
O Note and record: frequency, amount, and
characteristics. Describe unusual observations
related to stool or the act of defecating
Assisting with Bowel Elimination
O Promote regular bowel habits; consider:
O Timing, nutrition, privacy, and exercise
Colostomy
and Ileostomy
Emptying Ostomy Appliance
O Refer to Skills checklist
I&O
O https://www.youtube.com/watch?v=a6ovyZIs9
tg
30 mL in 1 oz
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- MedicationsDocument63 pagesMedicationssaraNo ratings yet
- Blended Competencies, Clinical Reasoning, and Processes of Person-Centered CareDocument30 pagesBlended Competencies, Clinical Reasoning, and Processes of Person-Centered Caresara0% (1)
- Foundations Ati QuizletDocument5 pagesFoundations Ati QuizletsaraNo ratings yet
- Care Plan Concept Map RenalDocument1 pageCare Plan Concept Map RenalsaraNo ratings yet
- Care Plan Concept Map FluidDocument1 pageCare Plan Concept Map Fluidsara0% (1)
- Care Plan Concept Map - RFIDocument1 pageCare Plan Concept Map - RFIsaraNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Muscle and Weight Gain Diet PDFDocument11 pagesMuscle and Weight Gain Diet PDFCavalera Max100% (1)
- 847 - Protein Energy MalnutritionDocument20 pages847 - Protein Energy MalnutritionSandip DuttaNo ratings yet
- QuesDocument13 pagesQuesKeith AndrewsNo ratings yet
- Medical Surgical Challenge and Practice TestDocument12 pagesMedical Surgical Challenge and Practice TestLim Eric100% (1)
- Liver Cirrhosis Powerpoint (Week 2) REVISEDDocument33 pagesLiver Cirrhosis Powerpoint (Week 2) REVISEDJustin CacheroNo ratings yet
- Sports and Nutrition Physical Educatin Class 12Document11 pagesSports and Nutrition Physical Educatin Class 12Srushti BhagitNo ratings yet
- UNISOY GOLD Nutritious Soy MatchaDocument3 pagesUNISOY GOLD Nutritious Soy MatchaYC TeoNo ratings yet
- MSM Sulfur MSM - Methylsulfonylmethane PDFDocument6 pagesMSM Sulfur MSM - Methylsulfonylmethane PDFmarkuswolf11100% (1)
- Clean Blood Vessels and Clogged Arteries Naturally With This Powerful Garlic RemedyDocument6 pagesClean Blood Vessels and Clogged Arteries Naturally With This Powerful Garlic RemedyPurushothaman DhanarajuNo ratings yet
- Tai Sophia Institute Whole Foods Cooking Lab 4 Nutrition 684 Fall 2012 .5 Credits FacultyDocument5 pagesTai Sophia Institute Whole Foods Cooking Lab 4 Nutrition 684 Fall 2012 .5 Credits Facultyapi-96990759No ratings yet
- 1836 18391Document4 pages1836 18391sekharNo ratings yet
- Chemistry Project On Analysis of Vegetable and Fruit JuicesDocument13 pagesChemistry Project On Analysis of Vegetable and Fruit JuicesAnuj Chaudhary100% (1)
- National Blindness Control ProgrammeDocument34 pagesNational Blindness Control ProgrammeSneha Gopalkrishnan100% (1)
- Vitamin B12 ReviewDocument12 pagesVitamin B12 ReviewMunyaradzi Nhambure100% (1)
- Summary of Normal Laboratory ValuesDocument37 pagesSummary of Normal Laboratory ValuesKelly Camero ÜNo ratings yet
- SgaDocument4 pagesSgaLovely Princess Balaba ToraynoNo ratings yet
- Food Production Yield ManagementDocument3 pagesFood Production Yield ManagementArghajoti DeyNo ratings yet
- TrajentaDocument23 pagesTrajentamonicaolivineNo ratings yet
- Black and Decker Bread Maker All in One-Manual PDFDocument37 pagesBlack and Decker Bread Maker All in One-Manual PDFTitel StanNo ratings yet
- Read The Following Text To Answer Questions Number 5 and 6. UsesDocument2 pagesRead The Following Text To Answer Questions Number 5 and 6. UsesRianAngga DinejatRCSNo ratings yet
- Cell Profile Report - Nisal Karawita - Nlkar1Document12 pagesCell Profile Report - Nisal Karawita - Nlkar1Lochana Karawita100% (1)
- CoenzymesDocument60 pagesCoenzymesraddagNo ratings yet
- Meal Mentor Sample Meal PlanDocument20 pagesMeal Mentor Sample Meal Planverdes nicoletaNo ratings yet
- Real Meal RevolutionTHE-LIST-A4Document2 pagesReal Meal RevolutionTHE-LIST-A4fridayschild2012No ratings yet
- Brand Management Case Based Assignments Guidelines and Case StudiesDocument45 pagesBrand Management Case Based Assignments Guidelines and Case StudiesNayanNo ratings yet
- Vera Simovska, MD., PHD, SummaryDocument4 pagesVera Simovska, MD., PHD, SummaryAss. Prof. Vera Simovska, MD., PhD.No ratings yet
- Nclex Rn.2018Document153 pagesNclex Rn.2018Paulo Arwin Baduria86% (14)
- Enzyme NutritionDocument7 pagesEnzyme NutritionViliaminaNo ratings yet
- Hibiscus Rosa-SinensisDocument32 pagesHibiscus Rosa-SinensisShanthi_KVNo ratings yet
- Gmo FinalDocument9 pagesGmo Finalapi-237602825No ratings yet