Professional Documents
Culture Documents
Hemodynamic Monitoring
Hemodynamic Monitoring
Uploaded by
Ahmad Adityawarman0 ratings0% found this document useful (0 votes)
18 views27 pagesCopyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
18 views27 pagesHemodynamic Monitoring
Hemodynamic Monitoring
Uploaded by
Ahmad AdityawarmanCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 27
Hemodynamic Monitoring
Vital Signs & Urine Output
Noninvasive Arterial Blood Pressure (BP)
Monitoring
• The level of the sampling site
relative to the heart affects the
measurement of BP because of
the effect of gravity
• In patients with severe
peripheral vascular disease,
there may be significant
differences in BP measurements
among the extremities. The
greater value should be used in
these patients.
Invasive Arterial Blood Pressure Monitoring
• Indications
• Current or anticipated hypotension
or wide blood pressure deviations,
• Contraindications
• end-organ disease necessitating
precise beat-to-beat blood • Smaller end arteries lacking
pressure regulation, collateral blood flow
• the need for multiple arterial blood • In extremities where there is a
gas or other blood analyses. suspicion of preexisting vascular
insufficiency.
Interpreting an Arterial Waveform
EKG
Systemic arterial waveform is
characterized by:
1. A rapid upstroke & downslope
(systolic ejection)
2. A dicrotic notch (closure of the
aortic valve)
3. Smooth progressive runoff
(diastole)
Jugular venous pressure (JVP)
• Cardinal aspect of the cardiovascular examination in the assessment
of volume status in patients in general, & in those with ADHF in
particular.
• Abnormally elevated JVP: > 5 cmH2O
• Patient is sitting at a 45 degree angle to the bed, there should be no
visible pulsations above the angle of Louis.
• JVP reflects right atrial (RA) pressure. It is often used as a surrogate
for LV filling pressure; however right heart failure is often absent in
patients with left-sided heart failure
Hepatojugular reflux (HJR)
• Jugular venous distension induced by firm pressure over the liver.
• An increase in JVP >3 cm by this maneuver is a positive HJR, which is a
sign of right-sided volume overload.
The third heart sound (S3)
• Occurs in early diastole due to abrupt cessation of rapid early diastolic
left ventricular inflow as a consequence of increased LV filling
pressures and an abnormally stiff, non-compliant left ventricle
• It is a fairly specific marker for LV dysfunction and correlates with BNP
levels.
Echocardiography
• Intracardiac pressures, cardiac output, vascular resistance, shunt
fractions, & valve lesions can be assessed by using a combination of
two-imensional imaging, color Doppler, pulse & continuous wave
Doppler, and tissue Doppler.
• Measuring of CO with echo:
VTI (velocity time integral)
• A VTI variation of > 12% predicts fluid
responsiveness (defined as an increase
in CO by at least 15% in response to a
standard fluid bolus) sensitivity of
100% & specificity of 89%.
• The maximum and minimum peak
velocities (Vmax) is an alternative to
tracing the VTI. This is quicker and
easier, and again. > 12% variation
suggests fluid responsiveness
Collapsibility index ≈ fluid status
(Dmax-Dmin) In spontaneous breathing:
• IVC < 2 cm with > 50% collapse ≈ CVP < 10
Dmax x 100% • IVC > 2 cm with > 50% collapse ≈ CVP > 10
Central venous catheter (CVC)
• Indications • V. femoralis
• CVP monitoring
• Central access caustic agent, rapid
hydration, TPN • Relative contraindications:
• Aspiration of air emboli, insertion of • Tumors, clots, or tricuspid valve
transcutaneous pacing leads, gaining
venous access in patients with poor vegetations that could be
peripheral veins dislodged/embolized during
cannulation.
• Access • Relate to the cannulation site. Ex:
• V. subclavian subclavian vein cannulation relatively
• V. jugularis interna/externa contraindicated in patients receiving
anticoagulants (if bleeding occurs
inability to direct compression).
Clinical Importance of CVC
• Monitoring of CVP & be an
additional parameter for
volume status
• In normal cardiac compliance
CVP approximates RA
pressure
• With specialized catheters, CVC
can be used for continuous
monitoring of central venous
oxygen saturation (Scvo2 )
Jugular venous pressure waveforms
Consists of 2 distinct positive waves (a & v wave) & 2 negative waves (x & y
descent).
• a wave occurs with RA systole & follows the P wave on EKG, precedes the S1.
• x descent occurs as RA pressure falls after the a wave & ventricular systole pulls
the tricuspid valve & the RA downward.
• c wave interrupts the x descent during early ventricular systole as the tricuspid
valve is briefly pushed in to the RA as the ventricle begins contracting, thereby
elevating RA pressure briefly.
• v wave occurs with RA filling at the end of ventricular systole, just after the S2.
• y descent follows the v wave & occurs with fall in RA pressure after the tricuspid
valve opens and fills the RV in diastole
Factors that make up SVO2
• Cardiac output
• SaO2
• VO2 (oxygen consumption)
• Hemoglobin
Normal values: 60-75%
Decreased values indicate:
• ↓ oxygen delivery
• ↑ oxygen demands
Causative Factors Clinical Conditions
O2 Delivery - Anemia
Hb concentration - Hemorrhage
Oxygen saturation - Hypoxemia
(SaO2) - Lung disease
- Low FIO2
Cardiac Output - LV dysfunction (cardiac disease, drugs)
- Shock – cardiac/septic (late)
- Hypovolemia
- Cardiac Dysrhythmias
Oxygen consumption - Fever, infection
- Seizures, agitation
- Shivering
- Work of Breathing
- Suctioning, bathing, repositioning
PA Catheter
• Functions:
• Measure CO (thermodilution) & pulmonary artery occlusive pressure (PAOP)
• Measure LVEDP & ventricular volume
• Predict SV
• Measure SVR
Find out the specific cause of
the patient's hemodynamic
instability
Other functions of PA Catheter
• Vascular tone, myocardial
contractility, & fluid balance can
be correctly assessed and
managed
• Measures CVP & allows for
hemodynamic calculated values.
• SvO2 monitoring (Fiber optic).
• Transvenous pacing.
• Fluid administration
PA Catheter
RED
KEEP
COVERED KEEP LOCKED
BLUE
Clear
YELLOW Markings on catheter.
1. Each thin line= 10 cm.
2. Each thick line= 50 cm.
Relative
Indications for PA catheter
contraindications
In patients whose cardiopulmonary
pressures, flows, and circulating
volume require precise, intensive
management • LBBB (because of the concern about
complete heart block)
MI – cardiogenic shock - CHF
Shock - all types • Conditions associated with a greatly
increased risk of arrhythmias
Valvular dysfunction (consider a catheter with pacing
Preoperative, Intraoperative, and capability)
Postoperative Monitoring • A PA catheter may serve as a nidus of
ARDS, Burns, Trauma, Renal Failure infection in bacteremic patients or
thrombus formation in patients prone
to hypercoagulation
Other methods of measuring cardiac output
• PA catheter: associated with worse outcome
• Less invasive methods
• Thermodilution
• Dye dilution
• Pulse contour device
• Esophageal doppler
• Thoracic bioimpendance
• Echocardiography
Thank you
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Nursing Care PlanDocument4 pagesNursing Care Planmanu_gutierrez0891% (11)
- 2007, Vol.87, Issues 5, Vascular Surgery - New Concepts and Practice For The General SurgeonDocument320 pages2007, Vol.87, Issues 5, Vascular Surgery - New Concepts and Practice For The General SurgeonCitlalli Ortiz100% (1)
- Mizuho Vascular (Transcranial) DopplerDocument4 pagesMizuho Vascular (Transcranial) DopplersigmakarsaNo ratings yet
- The Endovascular Management of Ruptured Abdominal Aortic AneurysmsDocument12 pagesThe Endovascular Management of Ruptured Abdominal Aortic AneurysmsDiilNo ratings yet
- Case Study HypertensionDocument7 pagesCase Study Hypertensionsanthyakunjumon75% (4)
- Hemodynamic MonitoringDocument34 pagesHemodynamic Monitoringkurt94764No ratings yet
- Termodiluicao PulmonarDocument7 pagesTermodiluicao PulmonarKarina ResendeNo ratings yet
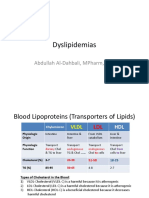
- Dyslipidemias: Abdullah Al-Dahbali, Mpharm, PHDDocument15 pagesDyslipidemias: Abdullah Al-Dahbali, Mpharm, PHDعزالدين الطيارNo ratings yet
- Cardiovascular WorksheetDocument4 pagesCardiovascular WorksheetAnonymous V7A9OKNo ratings yet
- A Study to Assess the Effectiveness of Video Assisted Teaching Module on Knowledge Regarding Myocardial Infarction and its Prevention among the Patients Attending Diabetic Clinic at BVV Sangha’s HSK Hospital and Research Centre, BagalkotDocument3 pagesA Study to Assess the Effectiveness of Video Assisted Teaching Module on Knowledge Regarding Myocardial Infarction and its Prevention among the Patients Attending Diabetic Clinic at BVV Sangha’s HSK Hospital and Research Centre, BagalkotInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Nursing Care Plan For Pulmonary Edema PDFDocument2 pagesNursing Care Plan For Pulmonary Edema PDFAsmaa100% (1)
- Cardiac Musclet PDFDocument1 pageCardiac Musclet PDFمؤمل كامل عبد العالي هريسNo ratings yet
- Cartlidge Timothy Role of Percutaneous CoronaryDocument7 pagesCartlidge Timothy Role of Percutaneous Coronarybruno baileyNo ratings yet
- Circulatory System REVIEWERDocument6 pagesCirculatory System REVIEWERClyde BaltazarNo ratings yet
- Insufisiensi Vena Kronik: Akina Maulidhany Tahir, M.DDocument12 pagesInsufisiensi Vena Kronik: Akina Maulidhany Tahir, M.Dummu yayaNo ratings yet
- Worksheets-Respiratory and Circulatory SystemsDocument8 pagesWorksheets-Respiratory and Circulatory SystemsCarlos GuardadoNo ratings yet
- Principles of HemodynamicDocument48 pagesPrinciples of HemodynamicdevdsantoshNo ratings yet
- Patent Ductus ArteriosusDocument37 pagesPatent Ductus Arteriosuschiitoxin0% (1)
- Pathology of Renal Artery StenosisDocument24 pagesPathology of Renal Artery Stenosishamed8181No ratings yet
- 40-Article Text-54-1-10-20200920Document5 pages40-Article Text-54-1-10-20200920Alif Ibnu QoyyimNo ratings yet
- Anatomy of Esophagus and StomachDocument65 pagesAnatomy of Esophagus and Stomachmackiecc100% (2)
- Functions of The Muscular System IncludeDocument8 pagesFunctions of The Muscular System IncludeDanesh CamachoNo ratings yet
- Intracardiac PressuresDocument41 pagesIntracardiac Pressureswaleed315No ratings yet
- CALDOBDocument2 pagesCALDOBSatyendra Pandey50% (2)
- Duplex Ultrasound in The Diagnosis of Lower-Extremity DVTDocument5 pagesDuplex Ultrasound in The Diagnosis of Lower-Extremity DVTastraeax panda100% (1)
- Hemoptysis Revealing Intracardiac Thrombosis: A Case Report of Behcets DiseaseDocument5 pagesHemoptysis Revealing Intracardiac Thrombosis: A Case Report of Behcets DiseaseIJAR JOURNALNo ratings yet
- Blood Pressure ChartDocument4 pagesBlood Pressure ChartMelvyn Chavez MauricoNo ratings yet
- NNS Tutorial NotesDocument7 pagesNNS Tutorial NotesGio AmadorNo ratings yet
- Vascular AnastamosisDocument6 pagesVascular AnastamosissahandNo ratings yet
- Vitalsigns 180617200506Document34 pagesVitalsigns 180617200506Maricris Tac-an Calising-PallarNo ratings yet