0% found this document useful (0 votes)
1K views40 pagesMedical Law and Ethics: The Physician-Patient Relationship
LAW AND ETHICS
Uploaded by
박태용Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
1K views40 pagesMedical Law and Ethics: The Physician-Patient Relationship
LAW AND ETHICS
Uploaded by
박태용Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
- Introduction: Cover page introducing Chapter 5 of Medical Law and Ethics focusing on the Physician-Patient Relationship.
- Learning Objectives: Outlines the key learning objectives for understanding the physician-patient relationship and related ethical principles.
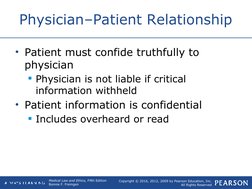
- Physician–Patient Relationship: Details the agreement and confidentiality necessary between physicians and patients in forming a therapeutic relationship.
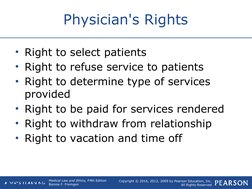
- Physician's Rights: Describes the rights of physicians regarding patient selection, service fees, and professional boundaries.
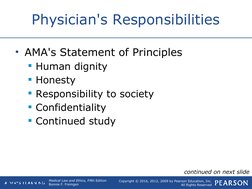
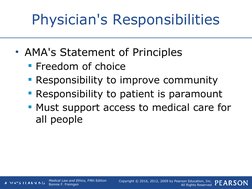
- Physician's Responsibilities: Explains the obligations physicians have towards dignity, honesty, society, and continuous learning.
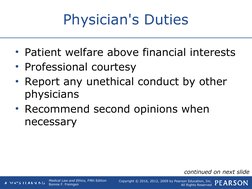
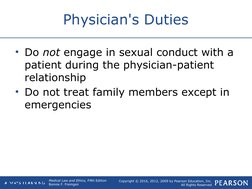
- Physician's Duties: Outlines duties concerning patient welfare, professional conduct, and recommendations for second opinions.
- Professional Practice Responsibilities: Covers responsibilities during emergencies and the treatment of indigent or uninsured patients.
- Duty Not to Abandon a Patient: Discusses the importance of not improperly terminating care once it has been initiated with a patient.
- Noncompliant and Incompetent Patients: Defines and differentiates between noncompliant and incompetent patients, addressing legal aspects.
- Duty to Treat Patients with AIDS: Explores the ethical and legal obligations for treating patients with HIV/AIDS and handling related disclosures.
- Exposure of Health Care Workers to Patient's Blood: Details the risks and allowable practices related to healthcare worker exposure to blood-borne pathogens.
- Restrictions on HIV-Infected Healthcare Workers: Discusses guidelines and recommendations for the practice restrictions placed on HIV-infected healthcare workers.
- Duty to Properly Identify Patients: Focuses on protocols for accurately identifying patients to ensure proper care and confidentiality.
- Duty to Respect Confidentiality: Emphasizes measures to maintain patient confidentiality in communication and record management.
- Duty to Tell the Truth: Discusses the ethical obligation of truth-telling in medical practice and its impact on patient care.
- Patient's Rights: Outlines the various rights patients have regarding confidentiality, consent, and treatment information.
- Confidentiality: Explains the importance of maintaining confidentiality of patient information and legal implications for breaches.
- Patient Self-Determination Acts: Introduces legal documents related to self-determination like living wills and powers of attorney.
- Definition of Minors: Defines minors in the context of healthcare, including mature and emancipated minor considerations.
- The Patient's Responsibilities: Describes responsibilities patients have in the context of adhering to treatment plans and payment obligations.
- Consent: Discusses different types of consent in medical treatment, including informed and implied consent.
- Doctrine of Informed Consent: Detailed exploration of the informed consent doctrine, focusing on patient understanding and rights.
- Implied Consent: Elaborates on scenarios where implied consent is applicable, particularly in emergencies.
- Exceptions to Consent: Addresses situations where exceptions to informed consent are legally recognized.
- Refusal to Grant Consent: Discusses the rights of patients to refuse medical treatment and the legal implications.
- Role of Health Care Consumer: Focuses on the engagement of health care consumers in preventing medical errors and ensuring quality care.