Professional Documents
Culture Documents
Monkeypox: Introduction and Control by Atif Aziz
Uploaded by
atif aziz0 ratings0% found this document useful (0 votes)
16 views13 pagesOriginal Title
Monkeypox
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
16 views13 pagesMonkeypox: Introduction and Control by Atif Aziz
Uploaded by
atif azizCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 13
Monkeypox
Introduction and Control
By
Atif Aziz
Monkeypox:
Learning
objectives
Understand the emergence of
monkeypox
§ Describe routes of transmission
§ List signs and symptoms
§ Identify monkeypox,
chickenpox, measles
§ Describe laboratory specimens
and tests
§ Discuss prevention and control
strategies
Monkeypox:
illness
§ infectious disease caused by
monkeypox virus and
characterized by a severe rash
§ typically self-limiting, but can
lead to severe illness or death
§ death occurs in up to 11% of
cases, most often in younger age
groups
Zoonotic Transmission:
• Monkeypox occurs primarily around rainforests of
West and Central Africa.
• The natural host of monkeypox is not known.
• Many species of small rodents and non-human
primates are susceptible to monkeypox virus.
• Following the eradication of smallpox, monkeypox
virus emerged as the most significant orthopoxvirus
in humans.
Orthopoxviruses:
• Like cowpox virus and variola virus (which causes
smallpox), the monkeypox virus is a species of the
genus Orthopoxvirus in the family Poxviridae.
• Monkeypox is a zoonosis (transmitted to humans
from animals) with symptoms similar to smallpox,
although less severe.
• Smallpox was eradicated in 1980 and vaccination
ceased.
• Waning immunity may be a factor in the emergence
of monkeypox.Orthopoxviruses
Viral Characteristics:
• Distinct virus subtypes group in two clades:
• The Central African Clade, prevalent in the Central
African Republic, the Democratic Republic of the Congo
and other countries.
• Clinically, virus in this clade causes more severe illness
and case fatality up to 11%
• The West African Clade, found in Nigeria, Côte d’Ivoire,
Liberia and Sierra Leone.
• This monkeypox virus causes less human-to-human
transmission, less severe illness, and death in up to 6% of
cases.
Zoonotic Transmission:
• Human infection has occurred from handling
infected animals: giant poached rats, rope squirrels,
and monkeys.
• Infection results from direct contact with the blood,
bodily fluids, or external lesions of infected animals.
• Eating inadequately cooked meat of infinfect
animals is a possible risk factor.
Continue...
• Human-to-human transmission results from close
contact with infected respiratory droplets, skin
lesions, or contaminated oobjects.
• Healthcare workers and household members of
active cases are at higher risk of infection.
• As human-to-human transmission is limited, most
outbreaks consist of only a few cases within
families.
Incubation Period and Disease
Progression:
• The interval from infection to onset of symptoms is
usually 6 to 13 days, but can range from 5 to 21 days.
• The infection progresses in two phases:
• the invasion period (0-5 days) characterized by fever,
headache, lymphadenopathy (swelling of the lymph
nodes), back pain, myalgia (muscle aches), and fatigue
• A characteristic rash appearing in stages 1-3 days after
the onset of fever, beginning on the face and
spreading to the trunk and limbs.
Continue..
• The rash lesions evolve from macules (lesions with a flat base)
to papules (raised from lesions) to vesicles (filled with clear
fluid) to pustules (filled with yellowish fluid), followed by crusts
• The rash affects
• The face in 95% of cases,
• The palms and soles of the feet (75%),
• Oral mucous membranes (70%),
• Genitalia (30%),
• The conjunctivae and cornea (20%).
• It may take three weeks for crusts to disappear.
Laboratory
Diagnosis:
Monkeypox can be confirmed in the
laboratory.
The bestspecimens are from lesions (fluid,
roof and crust).
The virus can be best identified with nucleic
acid tests by PCR. Antigen and antibody
detection methods are not specific
Specimens from persons and animals should
be handled by trained staff, wearing personal
protective equipment and working in suitably
equipped laboratories.
Procedures for safe storage and transport of
samples must be followed.
Prevention and Control:
• Health care workers caring for patients or handling
specimens must take standard, contact and droplet
precautions:
• Wash hands before and after caring for a patient,
• touching surroundings or handling specimens
• Wear appropriate personal protective equipment
• including gowns, gloves, masks, goggles and boots
• Ensure isolation of the patient in hospital or at home
• Ensure proper waste disposal and environmental
decontamination
Treatment:
• First generation vaccinia vaccines used to prevent
smallpox also largely protected vaccinees from
monkeypox.
• In 2019, a newer vaccinia vaccine for smallpox was
also approved for prevention of monkeypox in
adults.
• Further vaccination and treatment studies are
underway.
You might also like
- Monkey PoxDocument4 pagesMonkey PoxPrince Mark BadilloNo ratings yet
- MPX Prevention and Control at Cipto Mangunkusumo HospitalDocument16 pagesMPX Prevention and Control at Cipto Mangunkusumo Hospitaltatag primiawanNo ratings yet
- What's Monkeypox ?Document10 pagesWhat's Monkeypox ?Fumika VenayaNo ratings yet
- Monkey Pox FinalDocument35 pagesMonkey Pox FinalHiren patelNo ratings yet
- Crimean Congo Hemorrhagic FeverDocument18 pagesCrimean Congo Hemorrhagic FeverAmmar AbbasNo ratings yet
- Monkey PoxDocument29 pagesMonkey PoxMalavika A GNo ratings yet
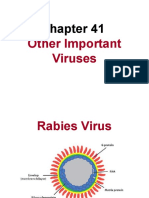
- Rabies: by Zakariya Al-NuaimiDocument16 pagesRabies: by Zakariya Al-Nuaimi123 sasNo ratings yet
- FB4 - 11 - NishanKharel - Dengue and MalariaDocument18 pagesFB4 - 11 - NishanKharel - Dengue and Malariavaskar_karkiNo ratings yet
- Rabies Virus: Structure, Pathogenesis, PreventionDocument22 pagesRabies Virus: Structure, Pathogenesis, PreventionpoojaNo ratings yet
- Is Monkeypox The Next Pandemic ?Document21 pagesIs Monkeypox The Next Pandemic ?Cyril LambayongNo ratings yet
- Ebola Haemorrhagic FeverDocument42 pagesEbola Haemorrhagic FeverDebraj BhattacharjeeNo ratings yet
- Rabies: Clinical FeaturesDocument3 pagesRabies: Clinical FeaturessivaNo ratings yet
- Chapter 13: Infectious Diseases (Week 26, 27 & 28) : Powerpoint Slides by Ms Lina TangDocument70 pagesChapter 13: Infectious Diseases (Week 26, 27 & 28) : Powerpoint Slides by Ms Lina TangHanaOmarNo ratings yet
- MonkeypoxDocument8 pagesMonkeypoxTabarak BhuiyanNo ratings yet
- Malaria 141112210953 Conversion Gate02Document33 pagesMalaria 141112210953 Conversion Gate02shubham vermaNo ratings yet
- Communicable DiseaseDocument32 pagesCommunicable DiseaseRaquel M. MendozaNo ratings yet
- Major Bacteria Infecting The Hematology System 2. Major Parasites Infecting The Hematologic SystemDocument128 pagesMajor Bacteria Infecting The Hematology System 2. Major Parasites Infecting The Hematologic SystemƯớc Của BếttingNo ratings yet
- MALARIA: CAUSES, SYMPTOMS, DIAGNOSIS AND TREATMENTDocument57 pagesMALARIA: CAUSES, SYMPTOMS, DIAGNOSIS AND TREATMENTsemere demissieNo ratings yet
- Communicable DiseasesDocument123 pagesCommunicable DiseasesAndrea Marie T. Artajo-BoheromNo ratings yet
- Zoonotic DiseaseDocument34 pagesZoonotic Diseasebajarangi_chaudhary100% (2)
- Rabies Diagnosis: Detecting Virus in Saliva, Skin and CSFDocument37 pagesRabies Diagnosis: Detecting Virus in Saliva, Skin and CSFjeanne_mbNo ratings yet
- Microbiology and Parasitology of the Hematologic SystemDocument121 pagesMicrobiology and Parasitology of the Hematologic SystemƯớc Của BếttingNo ratings yet
- Infectious Diseases and Rural Health Module Microbiology and ParasitologyDocument65 pagesInfectious Diseases and Rural Health Module Microbiology and ParasitologyDagnachew kasayeNo ratings yet
- Monkey Pox-FinalDocument23 pagesMonkey Pox-FinalnirmalaspandagaleNo ratings yet
- Filariasis: By: Barrantes, Patrick and Garcia, Charina JaneDocument17 pagesFilariasis: By: Barrantes, Patrick and Garcia, Charina Janerhimineecat71No ratings yet
- Crimean-Congo Hemorrhagic Fever Virus Classification and BiologyDocument14 pagesCrimean-Congo Hemorrhagic Fever Virus Classification and BiologyArnold AyebaleNo ratings yet
- RabiesDocument50 pagesRabiesMichael John TahadlangitNo ratings yet
- Eukaryotic Diseases - 06Document33 pagesEukaryotic Diseases - 06Vien WhitlockNo ratings yet
- Understanding Lymphatic FilariasisDocument5 pagesUnderstanding Lymphatic FilariasisawilakNo ratings yet
- Epidemiology Terminology GuideDocument5 pagesEpidemiology Terminology GuideBiratNagar100% (2)
- Basic Microbiology For 2014 Ver1Document27 pagesBasic Microbiology For 2014 Ver1Dr. Mussa QamerNo ratings yet
- Bio ProjDocument12 pagesBio Projsb132086No ratings yet
- Principles of Disease and EpidemiologyR1Document35 pagesPrinciples of Disease and EpidemiologyR1Biancia MckenzieNo ratings yet
- 48 Foot and Mouth DiseaseDocument20 pages48 Foot and Mouth DiseaseUsman Haider BuzdarNo ratings yet
- Viral Diseases - 06Document51 pagesViral Diseases - 06HIMANSHU SINGHNo ratings yet
- Basic Facts About Rabies DiseaseDocument32 pagesBasic Facts About Rabies DiseasedrkhalidfcpsNo ratings yet
- Introduction To Crimean-Congo Haemorrhagic FeverDocument17 pagesIntroduction To Crimean-Congo Haemorrhagic FeverImad Q. KhaleelNo ratings yet
- Presentation 2Document18 pagesPresentation 2Shaafici MahamudNo ratings yet
- Occupational Biohazards: Dr. Tajuddin Bantacut Department of Agroindustrial Technology Bogor Agricultural UniversityDocument29 pagesOccupational Biohazards: Dr. Tajuddin Bantacut Department of Agroindustrial Technology Bogor Agricultural UniversityAbdur RahmanNo ratings yet
- Community Health Nursing - 1 MahirDocument37 pagesCommunity Health Nursing - 1 MahirvhoramahirNo ratings yet
- Viral Diseases of The Cardiovascular and Lympatic SystemDocument50 pagesViral Diseases of The Cardiovascular and Lympatic SystemHeuniceLoisSumabongNo ratings yet
- Dr. Sanjeev GuptaDocument73 pagesDr. Sanjeev Guptadrsanjeev15No ratings yet
- Helminths: Intestinal WormsDocument43 pagesHelminths: Intestinal WormsBatool SherbiniNo ratings yet
- Update MonkeypoxDocument14 pagesUpdate MonkeypoxMary Grace PedrozoNo ratings yet
- Infections of The CVSDocument11 pagesInfections of The CVScleahis cruzNo ratings yet
- Vector Borne DiseasesDocument7 pagesVector Borne DiseasesAbuzar KhanNo ratings yet
- BrucellosisDocument24 pagesBrucellosisdr. snehal patilNo ratings yet
- Monkey Pox2Document7 pagesMonkey Pox2Zeren Joy C. AngelesNo ratings yet
- ZOONOSISDocument53 pagesZOONOSISBiManda Rizki NurhidayatNo ratings yet
- African Swine Fever: A Highly Contagious Hemorrhagic DiseaseDocument11 pagesAfrican Swine Fever: A Highly Contagious Hemorrhagic DiseaseTamiru LegesseNo ratings yet
- Communicable DiseaseDocument32 pagesCommunicable Diseasekimberly shayneNo ratings yet
- Microbialdiseases 160303140348Document42 pagesMicrobialdiseases 160303140348proud.student2023No ratings yet
- Êy Êy Êy Êy ÊyDocument4 pagesÊy Êy Êy Êy ÊyYel CMNo ratings yet
- RabiesDocument81 pagesRabiesSujatha J Jayabal100% (1)
- What Is Anthropod and Vector Borne Disease What Is Anthropod and Vector Borne DiseaseDocument59 pagesWhat Is Anthropod and Vector Borne Disease What Is Anthropod and Vector Borne DiseaseNessa Layos MorilloNo ratings yet
- Mumps - DishaDocument18 pagesMumps - DishaDr Bharat ZinjurkeNo ratings yet
- What Is Rabies? How Do People and Animals Get The Disease?Document14 pagesWhat Is Rabies? How Do People and Animals Get The Disease?lea nicole iglesiasNo ratings yet
- Emerging Diseases: Mers Cov Dan Ebola Virus: Agung Dwi Wahyu WidodoDocument54 pagesEmerging Diseases: Mers Cov Dan Ebola Virus: Agung Dwi Wahyu WidodoElisa Maria WahyuniNo ratings yet
- Chapter-5 Quality Assurance of VaccinesDocument37 pagesChapter-5 Quality Assurance of VaccinesYarfa KhurramNo ratings yet
- Medicine NamesDocument782 pagesMedicine NamesasgbalajiNo ratings yet
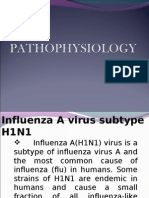
- A h1n1 PathophysiologyDocument11 pagesA h1n1 PathophysiologyJayson RNNo ratings yet
- Mucosal Adjuvants: Charles O. Elson Mark T. DertzbaughDocument1 pageMucosal Adjuvants: Charles O. Elson Mark T. DertzbaughPortobello CadısıNo ratings yet
- FIGO Cancer Report 2018Document2 pagesFIGO Cancer Report 2018Anonymous 2XsadJlrNo ratings yet
- Chickenpox 160531062051 PDFDocument16 pagesChickenpox 160531062051 PDFJu Lie AnnNo ratings yet
- Varicella ZosterDocument6 pagesVaricella Zosterapi-550140983No ratings yet
- Laporan Bulanan Hasil Imunisasi Rutin Bayi Dan Batita Bulan: JanuariDocument9 pagesLaporan Bulanan Hasil Imunisasi Rutin Bayi Dan Batita Bulan: JanuariNUR AFIAHNo ratings yet
- Agota Statement On COVID 19 Vaccination of Pregnant and Lactating - 17-8-21Document5 pagesAgota Statement On COVID 19 Vaccination of Pregnant and Lactating - 17-8-21prisco linusiNo ratings yet
- Transmission Precautions ExplainedDocument8 pagesTransmission Precautions Explainedniraj_sd100% (1)
- Mortality DeclineDocument13 pagesMortality DeclineKathrina GabrielNo ratings yet
- Make the Most of Your Preventive CareDocument5 pagesMake the Most of Your Preventive CarelindytindylindtNo ratings yet
- Dna VaccineDocument2 pagesDna VaccinesauravsarkarNo ratings yet
- CatalogDocument342 pagesCatalognuzufeedNo ratings yet
- David OnyangoDocument16 pagesDavid OnyangoprabhasNo ratings yet
- Balanced Diet and Human Diseases Biology GuideDocument19 pagesBalanced Diet and Human Diseases Biology GuideRameshNo ratings yet
- WHO - The Second Ten Years of The World Health OrganizationDocument456 pagesWHO - The Second Ten Years of The World Health OrganizationFloripondio19No ratings yet
- Animal Science PowerpointDocument104 pagesAnimal Science Powerpointtom2susanNo ratings yet
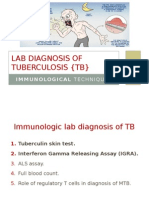
- Immunological Lab Diagnosis of TuberculosisDocument38 pagesImmunological Lab Diagnosis of TuberculosisRasha EmadNo ratings yet
- Rubella: Dr.T.V.Rao MDDocument42 pagesRubella: Dr.T.V.Rao MDtummalapalli venkateswara raoNo ratings yet
- Executive Order No 14FDocument5 pagesExecutive Order No 14FHelen BennettNo ratings yet
- Summary of Key Microbiology TestsDocument45 pagesSummary of Key Microbiology TestsAtiya HajjajNo ratings yet
- RHU Situanional ReportDocument8 pagesRHU Situanional ReportErnest AtonNo ratings yet
- Hepa B TestDocument1 pageHepa B TestsmilingfroggyNo ratings yet
- Drug Study 12Document4 pagesDrug Study 12Nathalie kate petallarNo ratings yet
- English Learning Activity Sheets: Quarter 4 Weeks 1-2Document24 pagesEnglish Learning Activity Sheets: Quarter 4 Weeks 1-2Benyrose Aguilar AsuncionNo ratings yet
- AIIMS Mega Test Series-02 PDFDocument11 pagesAIIMS Mega Test Series-02 PDFRajat KumarNo ratings yet
- A Study To Assess The Knowledge Regarding NationalDocument1 pageA Study To Assess The Knowledge Regarding NationalAnsu MaliyakalNo ratings yet
- Malaria Research in South East AsiaDocument186 pagesMalaria Research in South East AsiaRizal QowiNo ratings yet
- Bordetellabronchiseptica (Kennel Cough)Document5 pagesBordetellabronchiseptica (Kennel Cough)Della HalyoNo ratings yet