Professional Documents
Culture Documents
7 - Rheumatoid Arthritis
Uploaded by
Abdullah Al Arifi0 ratings0% found this document useful (0 votes)
2 views17 pagesrheumatoid
Original Title
7- Rheumatoid Arthritis
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentrheumatoid
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
2 views17 pages7 - Rheumatoid Arthritis
Uploaded by
Abdullah Al Arifirheumatoid
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 17
Rheumatoid Arthritis (RA)
Rheumatoid Arthritis (RA)
• RA is a chronic inflammatory disorder of autoimmune
origin principally attacks the joints, producing a
nonsuppurative proliferative and inflammatory synovitis,
that progresses to joint destruction and ankylosis
• Extraarticular lesions may occur in the skin, heart, blood
vessels, and lungs.
• It is three times more common in women than in men.
• The peak incidence is in the 3rd - 5th decades of life.
• Pathogenesis:
• RA results from exposure of a genetically susceptible host to
environmental factors.
• Genetic susceptibility:
• Association with HLA-DR alleles (DR4, DR1, DRE10, DR14)
• Environmental factors:
• Infectious agents (EBV, retroviruses, mycobacteria, Borrelia,
and Mycoplasma), and smoking.
• Infection and smoking may promote citrullination of self-
proteins that trigger autoimmune reactions.
• The pathologic changes are mediated by antibodies against
self-antigens and inflammation caused by cytokines
secreted by CD4+ T cells.
• CD4+ T helper (TH) cells initiate the autoimmune response
by reacting with an arthritogen, (microbial or a chemically
modified self-antigen).
• The T cells produce cytokines that stimulate other
inflammatory cells to effect tissue injury:
1. IFN-γ from TH1 cells activates macrophages and synovial
cells.
2. IL-17 from TH17 cells recruits neutrophils and monocytes.
3. RANKL expressed on activated T cells stimulates osteoclasts
and bone resorption.
4. TNF and IL-1 from macrophages stimulate resident synovial
cells to secrete proteases that destroy hyaline cartilage.
• Antibodies are produced against self antigens (citrullinated
peptides).
• In RA, complexes of antibodies with citrullinated peptides
deposit in the joints.
• About 80% of patients have serum IgM or IgA
autoantibodies that bind to the Fc portions of their own
IgG.
• These autoantibodies are called rheumatoid factor.
• Morphology:
• Grossly, the synovium becomes edematous, thickened, and
hyperplastic.
• Hallmark is synovitis leading to formation of a pannus (a
mass of edematous synovium, inflammatory cells,
granulation tissue, and fibroblasts
• The pannus can bridge apposing bones to form a fibrous
ankylosis that will eventually ossify.
• The characteristic histologic features include:
1. Synovial cell hyperplasia and proliferation.
2. Dense inflammatory infiltrates of CD4+ helper T cells, B
cells, plasma cells, dendritic cells, and macrophages.
3. Increased vascularity resulting from angiogenesis.
4. Neutrophils and aggregates of organizing fibrin on the
synovial and joint surfaces.
5. Osteoclastic activity in underlying bone causing
periarticular erosions and subchondral cysts.
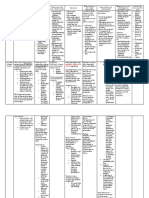
Rheumatoid arthritis.
(A) Schematic view of the joint lesion. (B) Low magnification shows
marked synovial hypertrophy with formation of villi.
(C) At higher magnification, subsynovial tissue containing a dense
lymphoid aggregate.
• Rheumatoid nodules are an infrequent manifestation of RA
and typically occur in subcutaneous tissue including the
forearm, elbows, occiput, and lumbosacral area.
• Microscopically, they resemble necrotizing granulomas.
• Rarely, RA can involve the lungs (rheumatoid nodules,
interstitial lung disease).
Rheumatoid Nodule
• Clinical Course:
• Non-specific malaise, fatigue, and generalized
musculoskeletal pain.
• Arthritis with morning stiffness that improves with activity.
• Symmetric involvement of PIP joints of the fingers (swan-
neck deformity), wrists (ulnar deviation), elbows, ankles,
and knees is characteristic.
• DIP is usually spared (unlike osteoarthritis).
• Affected joints are swollen, warm, and painful.
• Atlanto-axial joint subluxation may threaten the spinal cord
• Laboratory findings:
• Positive Rheumatoid factor.
• Anticyclic citrullinated peptide antibodies (ACPA/anti-CCP)
are highly specific (~98%) for RA.
• There is often anaemia of chronic disease.
• Inflammation causes ↑platelets, ↑ESR, ↑CRP.
• Neutrophils and high protein in synovial fluid.
• X-rays show soft tissue swelling, joint effusions, juxta-
articular osteopenia and ↓joint space.
• Later there may be bony erosions, subluxation or complete
carpal destruction.
• Ultrasound and MRI can identify synovitis more accurately,
and have greater sensitivity in detecting bone erosions
than conventional X-rays.
• Complications:
• Anemia of chronic disease
• Secondary amyloidosis.
• Management:
• Corticosteroids, methotrexate, and TNF antagonists.
• NSAIDS
• Physiotherapy
• Surgery may relieve pain, improve function and prevent
deformity.
You might also like
- Rheumatic FeverDocument26 pagesRheumatic FeverAhmed Ben Bella100% (2)
- Rheumatoid Arthritis: By: Claudio Wangta Oky CahyantoDocument18 pagesRheumatoid Arthritis: By: Claudio Wangta Oky CahyantoEditya AprilianiNo ratings yet
- Rheumatoid Arthritis PresentationDocument36 pagesRheumatoid Arthritis PresentationAsyaari ArifNo ratings yet
- Rheumatoid Arthritis 1Document63 pagesRheumatoid Arthritis 1ycg9n6wq4rNo ratings yet
- Annie Rheumatoid ArthritisDocument65 pagesAnnie Rheumatoid Arthritissaroj yadavNo ratings yet
- Rheumatoid Arthritis and Acute Rheumatic FeverDocument76 pagesRheumatoid Arthritis and Acute Rheumatic FeverM. O. PHC HOLAVANAHALLYNo ratings yet
- Faculty of MedicineDocument28 pagesFaculty of MedicineRana AtefNo ratings yet
- 21 Diseases of The Joints 2 - 2021Document50 pages21 Diseases of The Joints 2 - 2021Ahmed YTNo ratings yet
- PROF: 2017-2018 - Subject: Surgery - DATE-16/04/2020 - DATE - 16/04/2020 - Faculty Name: DR Sunanda (PT)Document18 pagesPROF: 2017-2018 - Subject: Surgery - DATE-16/04/2020 - DATE - 16/04/2020 - Faculty Name: DR Sunanda (PT)amjad khanNo ratings yet
- Poliartr - Reumatoida EnglezaDocument104 pagesPoliartr - Reumatoida EnglezaGermanyNo ratings yet
- Rheumatoid ArthritisDocument19 pagesRheumatoid ArthritisLiya AnjelinaNo ratings yet
- VasculitidesDocument44 pagesVasculitidesNikki LumidaoNo ratings yet
- Medicine Exam NotesDocument211 pagesMedicine Exam Notesjf65ky8f8tNo ratings yet
- Diseases of Immune System Part 2Document47 pagesDiseases of Immune System Part 2KundaNo ratings yet
- Rheumatoid Arthritis (Medi)Document3 pagesRheumatoid Arthritis (Medi)sapa hayoNo ratings yet
- Acute Rheumatic Fever: Prof - Univ.Dr. Corina ZorilăDocument40 pagesAcute Rheumatic Fever: Prof - Univ.Dr. Corina ZorilăGermanyNo ratings yet
- JointsDocument68 pagesJointsLaine ZeeNo ratings yet
- MCTD, Ra, Jia - Hiba Irfan, Group 2Document41 pagesMCTD, Ra, Jia - Hiba Irfan, Group 2hibaNo ratings yet
- Ra 2Document50 pagesRa 2Amira AhmedNo ratings yet
- Autoimmune DiseasesDocument28 pagesAutoimmune Diseasesekwelipraise7No ratings yet
- Systemic Lupus ErythematosusDocument60 pagesSystemic Lupus ErythematosusJulian FsyGaNo ratings yet
- Rheumatic Valvular DiseaseDocument28 pagesRheumatic Valvular DiseaseBenallouaminaNo ratings yet
- باطنة تمريض rheumatologyDocument6 pagesباطنة تمريض rheumatologyAbdullmlik AlfurasNo ratings yet
- 2-Autoimmune DiseasesDocument29 pages2-Autoimmune DiseasessoniaNo ratings yet
- Diseases of The Immune System (II)Document73 pagesDiseases of The Immune System (II)Visca ZerlindaNo ratings yet
- Immune Complex DiseasesDocument11 pagesImmune Complex DiseasesBryan AmataNo ratings yet
- Classification of Disorders of Musculoskeletal System (MSK) : Presented By: Siti Sarah Maha Dewi Bong Jen NeeDocument69 pagesClassification of Disorders of Musculoskeletal System (MSK) : Presented By: Siti Sarah Maha Dewi Bong Jen NeeBONG AIKCHINGNo ratings yet
- Rangkuman Week 3 (PBL) - RADocument27 pagesRangkuman Week 3 (PBL) - RAMaria Dini AdmiratiNo ratings yet
- Rheumatoid Arthritis: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 2/ 11/ 2020Document54 pagesRheumatoid Arthritis: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 2/ 11/ 2020Alan K Mhamad100% (1)
- 10 AutoimmunityDocument11 pages10 AutoimmunityangelNo ratings yet
- Rheumatoid ArthritisDocument52 pagesRheumatoid ArthritisArun NingarajappaNo ratings yet
- Rheumatoid ArthritisDocument66 pagesRheumatoid ArthritisSaeda AhmedNo ratings yet
- Rheumatoid Arthritis: Anthony SafiDocument9 pagesRheumatoid Arthritis: Anthony SafiAnthony safiNo ratings yet
- WBC DisorderDocument24 pagesWBC DisorderNirav SharmaNo ratings yet
- Connective Tissue Disorders: DR Josephine Ojoo MBCHB FRCP CCST (Resp) Dip Hiv Med Senior Lecturer Maseno UniversityDocument70 pagesConnective Tissue Disorders: DR Josephine Ojoo MBCHB FRCP CCST (Resp) Dip Hiv Med Senior Lecturer Maseno UniversityMalueth AnguiNo ratings yet
- Immunity 1Document6 pagesImmunity 1Tori RolandNo ratings yet
- BY Balakrishna.p ArthritisDocument38 pagesBY Balakrishna.p ArthritissandypolapalaNo ratings yet
- Dr. Tehreem Nasir MBBS, RMPDocument27 pagesDr. Tehreem Nasir MBBS, RMPAhmed SaeedNo ratings yet
- Rheumatic Heart Disease: Dr.K.Sathish Kumar, MD (Hom) .Document14 pagesRheumatic Heart Disease: Dr.K.Sathish Kumar, MD (Hom) .mnr hmcNo ratings yet
- InjuryDocument50 pagesInjuryRenaldas AugulisNo ratings yet
- Infectious Arthritis: Marshell Tendean, MD Department of Internal Medicine UKRIDA Faculty of Medicine Jakarta IndonesiaDocument56 pagesInfectious Arthritis: Marshell Tendean, MD Department of Internal Medicine UKRIDA Faculty of Medicine Jakarta Indonesiakintan utamiNo ratings yet
- Dr. Lamia El Wakeel, PhD. Lecturer of Clinical Pharmacy Ain Shams UniversityDocument19 pagesDr. Lamia El Wakeel, PhD. Lecturer of Clinical Pharmacy Ain Shams UniversitysamvetNo ratings yet
- Rheumatoid Arthritis: Classification of RaDocument22 pagesRheumatoid Arthritis: Classification of RaBlanchette ChNo ratings yet
- Rheumatoid Arthritis by DR Bashir Ahmed Dar Associate Professor Medicine Sopore KashmirDocument220 pagesRheumatoid Arthritis by DR Bashir Ahmed Dar Associate Professor Medicine Sopore KashmirProf Dr Bashir Ahmed Dar Chinki Pora Sopore KashmirNo ratings yet
- Rheumatoid Arthritis: Muh. Nur Ikhsan Liwang FK Untad 2019Document38 pagesRheumatoid Arthritis: Muh. Nur Ikhsan Liwang FK Untad 2019Canis MajorisNo ratings yet
- Rheumatology Year 4Document90 pagesRheumatology Year 4Abdalla SamatarNo ratings yet
- RheumatoidDocument35 pagesRheumatoidDeva LekshmiNo ratings yet
- Chapter 3. Inflammatory Rheumatic DisorderDocument37 pagesChapter 3. Inflammatory Rheumatic DisorderMika KresnaNo ratings yet
- Immuno Lec 1&2&3Document33 pagesImmuno Lec 1&2&3Ali AlhamdaniNo ratings yet
- ArthritisDocument11 pagesArthritisHemant GargNo ratings yet
- Rheumatology Saif 2013 Wesmosis PDFDocument30 pagesRheumatology Saif 2013 Wesmosis PDFMohamed A SalehNo ratings yet
- Rheumatoid ArthritisDocument16 pagesRheumatoid Arthritisbudak46No ratings yet
- Borrel Ios IsDocument20 pagesBorrel Ios IsRohan TejaNo ratings yet
- Rheumatoid ArthritisDocument29 pagesRheumatoid ArthritisTamim IshtiaqueNo ratings yet
- Reh ImmunlogyDocument18 pagesReh Immunlogygavallapalli ramyaNo ratings yet
- Rheumatoid HandsDocument144 pagesRheumatoid HandsSushil VijayNo ratings yet
- Transverse Myelitis, A Simple Guide To The Condition, Treatment And Related DiseasesFrom EverandTransverse Myelitis, A Simple Guide To The Condition, Treatment And Related DiseasesRating: 5 out of 5 stars5/5 (1)
- Carpal Tunnel Syndrome, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandCarpal Tunnel Syndrome, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Lemone/Burke/Bauldoff/Gubrud, Medical-Surgical Nursing 6Th Edition Test BankDocument44 pagesLemone/Burke/Bauldoff/Gubrud, Medical-Surgical Nursing 6Th Edition Test Banknurse homeNo ratings yet
- Type of GaitsDocument4 pagesType of GaitsSyimah UmarNo ratings yet
- Viii. Medications: Generic Name: Actions: AssessmentDocument4 pagesViii. Medications: Generic Name: Actions: AssessmentJohn Alex Maramba MelencioNo ratings yet
- PGI MANIMTIM - Reaction Paper - Family Medicine - COVID-19Document1 pagePGI MANIMTIM - Reaction Paper - Family Medicine - COVID-19Kim Adarem Joy ManimtimNo ratings yet
- Case Study Interview QuestionsDocument10 pagesCase Study Interview QuestionsJzelNo ratings yet
- 2022 HRS - Aggressive B-Cell Lymphomas FINALDocument80 pages2022 HRS - Aggressive B-Cell Lymphomas FINALИван НегарэNo ratings yet
- Binge Eating Disorder PDFDocument4 pagesBinge Eating Disorder PDFIsidora KesićNo ratings yet
- Human Physiology PRACTICE SCENERIO QUESTIONDocument8 pagesHuman Physiology PRACTICE SCENERIO QUESTIONThao NguyenNo ratings yet
- Test Bank For Medical Terminology A Word Building Approach 7th Edition RiceDocument24 pagesTest Bank For Medical Terminology A Word Building Approach 7th Edition RiceMaryJohnsonafrz100% (37)
- Villa vs. GSIS DigestDocument2 pagesVilla vs. GSIS DigestChristopher AdvinculaNo ratings yet
- Drug Study 6th FloorDocument4 pagesDrug Study 6th Floorjulesubayubay5428No ratings yet
- Hematology L5Document22 pagesHematology L5Haibat Sultan StationeryNo ratings yet
- Alprazolam BiperidinDocument6 pagesAlprazolam BiperidinFionah RetuyaNo ratings yet
- CO-VANCE (Metformin + Glibenclamide) Product PresentationDocument25 pagesCO-VANCE (Metformin + Glibenclamide) Product Presentationashe64h74No ratings yet
- Little Child Jesus Christian Academy Cabiao, Nueva Ecija, IncDocument5 pagesLittle Child Jesus Christian Academy Cabiao, Nueva Ecija, IncEuniceNo ratings yet
- Ramesh Vasudeva Rao InsuranceDocument7 pagesRamesh Vasudeva Rao InsuranceNasr MegahedNo ratings yet
- Pathology of Parathyrid Gland FinalDocument63 pagesPathology of Parathyrid Gland FinalGurpreet Kaur SagooNo ratings yet
- Diarrhea Care PlanDocument2 pagesDiarrhea Care Planbobbyr4100% (2)
- Ortho Case StudyDocument17 pagesOrtho Case StudyAndrea Sibayan SorianoNo ratings yet
- Pharma - Updated Topical Past Papers 2007-23Document53 pagesPharma - Updated Topical Past Papers 2007-23Tayyab AfzalNo ratings yet
- An Assessment of Microbial Contamination of Bush Meat Sold at Different Locations Along WarriBenin Express Way in NigeriaDocument4 pagesAn Assessment of Microbial Contamination of Bush Meat Sold at Different Locations Along WarriBenin Express Way in NigeriaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Space InfectionsDocument79 pagesSpace Infectionssridevi sivaramakrishnanNo ratings yet
- GlutenDocument4 pagesGlutenAnsharah SameenNo ratings yet
- Grp. 11 ManuscriptDocument98 pagesGrp. 11 ManuscriptJosiah VillacampaNo ratings yet
- Module 1: Care For Clients With Cognitive and Perceptual Disorder 1Document93 pagesModule 1: Care For Clients With Cognitive and Perceptual Disorder 1Woot RootNo ratings yet
- A. Photoorganotrophs: MCU-FDT Medical Foundation Department of Microbiology and Parasitology College of MedicineDocument14 pagesA. Photoorganotrophs: MCU-FDT Medical Foundation Department of Microbiology and Parasitology College of MedicineFernandez-De Ala NicaNo ratings yet
- Cga - 1Document19 pagesCga - 1Kenji Tolero100% (1)
- Census August 14 - August 15, 2020Document6 pagesCensus August 14 - August 15, 2020Patrick JohnNo ratings yet
- C Auris Lab Workers FactSheet HDocument2 pagesC Auris Lab Workers FactSheet HYi ChanNo ratings yet
- Asthma Thesis StatementDocument4 pagesAsthma Thesis Statementfjnev0hc100% (2)