Professional Documents
Culture Documents
Cardiovascular Disorders and Pregnancy
Uploaded by
Chari Rivo0 ratings0% found this document useful (0 votes)
10 views31 pagesCopyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
10 views31 pagesCardiovascular Disorders and Pregnancy
Uploaded by
Chari RivoCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 31
Cardiovascul
ar Disorders
and
Pregnancy
Chari V. Rivo, RM, RN
Cardiovascular Disorder and
Pregnancy
• complicates only
approximately 1% of all
pregnancies
• responsible for 5% of
maternal deaths during
pregnancy (Cunningham,
Leveno, Bloom, et al., 2014)
• Infant Mortality Rate - Number of deaths per 1000 live births
occurring at birth or in the first 12 months of life
– 20.9 deaths/1,000 live births (2018 est.)
– male: 23.8 deaths/1,000 live births
– female: 17.9 deaths/1,000 live births
• Maternal Mortality Rate - Number of maternal deaths per
100,000 live births that occur as a direct result of the reproductive
process.
– 121 deaths/100,000 live births (2017 est.)
• Childhood Mortality Rate - Number of deaths per1000
population in children, 1 to 14 years of age.
• Childhood Morbidity Rate
Maternal and Child Health
Nursing
• Primary Goal: Promotion and maintenance of optimal family
health to ensure cycles of optimal child-bearing and childrearing.
• Range of practice includes:
– Preconceptual health care
– Care of women during three trimesters of pregnancy and the
puerperium (the 6 weeks after childbirth, sometimes termed the fourth
trimester of pregnancy)
– Care of infants during the perinatal period (6 weeks be-fore conception
to 6 weeks after birth)
– Care of children from birth through adolescence
– Care in settings as varied as the birthing room, the pediatric intensive
care unit, and the home
Purposes Of Prenatal Care
1. Establish a baseline of present health
2. Determine the gestational age of the fetus
3. Monitor fetal development and maternal well
being
4. Identify women at risk for complications
5. Minimize the risk of possible complications
by anticipating and preventing problems before
they occur
6. Provide time for education about pregnancy,
lactation, and newborn care
Preconceptual Visit
• appointment with a physician or nurse-midwife before
becoming pregnant to obtain accurate reproductive life planning
information, receive reassurance about fertility (as much as can
be given based on a health history and a routine physical
examination), and detect any problems that may need
correction through a thorough health history, and physical and
pelvic examinations(Rojas, Wood, & Blakemore, 2007)
• Hemoglobin level and blood type (including Rh factor)
• Papanicolaou (Pap) test,
• minor vaginal infections such as those arising from Candida or
chlamydia can be corrected to help ensure fertility.
• Counseling on the importance of a good protein diet, adequate
intake of folic acid and other vitamins,
• Early prenatal care if she does become pregnant.
Health Assessment Suring
Prenatal
• Initial Interview
– Establishing rapport
– Gaining information about a woman’s physical and
psychosocial health
– Obtaining a basis for anticipatory guidance for the
pregnancy
– To be accomplished in private, quiet setting
Components of a Health History
• Demographic Data
• Chief Concern
• Family Profile
• History of Past Illnesses
• History of Family Illnesses
• Day History/Social Profile
• Medical History
• Gynecologic History
– Reproductive tract problems/ surgeries
– Women’s health problems such as breast disease
– Menarche
– Use of family planning methods
• Obstetric History
– History of previous pregnancies– baby’s gender,
BW, BL, other significant findings
– Hx of miscarriage
– Rh Immunoglobulin injection
T: Number of full-term
infants born (infants born at
37 weeks or after)
P: Number of preterm
infants born (infants born
before 37 weeks)
A: Number of spontaneous
miscarriages or therapeutic
abortions
L: Number of living
children
M: Multiple pregnancies
TPAL/TPALM
Example:
• A woman who has had two previous
pregnancies, has given birth to two term
children, and is again pregnant.
– gravida 3, para 2002 (GTPAL) or 320020
(GTPALM)
• A woman who had term twins, then one
preterm infant, and is now pregnant again
– gravida 3, para 21031 (GTPALM)
• Review of Systems
– Head to Toe Assessment
• Conclusion
• Physical Examination
– Baseline Height/Weight and Vital Sign
Measurement
– Normal weight gain during pregnancy: 25-35 lbs
– sudden increase of BP and weight:
• HPN
– Sudden increase in pulse and respiration:
• Bleeding
Assessment of Systems
• General Appearance and Mental Status
– Closely inspect for signs such as careless hygiene, un-
washed hair, inappropriate or soiled clothing, and sad
facial expression that may suggest fatigue or depression
about their diagnosis
• Head and Scalp
– chloasma
• Eyes
– Edema of the eyelids combined with a swollen optic disk
(identified on ophthalmoscopic examination)
• Edema of PIH - pregnancy-induced hypertension also usually
report spots before their eyes or diplopia (double vision)
• Nose.
– The increased level of estrogen associated with pregnancy
may cause nasal congestion or the appearance of swollen
nasal membranes.
• Ears
– nasal stuffiness that accompanies pregnancy may lead to
blocked eustachian tubes and therefore a feeling of “fullness”
in the ears or dampening of sound during early pregnancy
• Sinuses
– Sinuses should feel nontender
• Mouth, Teeth, and Throat
– Gingival hypertrophy
– Check for cracked corners of the mouth
• Vitamin A Deficiency
• Neck
– Slight thyroid hypertrophy may occur with pregnancy because
the overall metabolic rate is increased
• Lymph Nodes
– No palpable lymph nodes should be present; however, because
pregnant women may develop an increased number of upper
respiratory infections because of reduced immunologic resistance,
one or two pea-sized cervical lymph nodes may be palpable
• Breast
• Breast changes may be one of the first things women
notice in pregnancy:
– Areolae darken.
– Secondary areolae develop.
– Montgomery tubercles (sebaceous glands in the
areolae)become prominent.
– Overall breast size increases.
– Breast consistency firms.
– Blue streaking of veins becomes prominent
– Colostrum may be expelled as early as the 16th week of
pregnancy.
– Any supernumerary nipple also may become darker and
enlarge in size.
Secondary areola
• Heart
– a woman may develop an innocent
(functional) heart murmur during
pregnancy because of her increased
vascular volume
• Lungs
– Shortness of breath (in late pregnancy)
may occur because diaphragm cannot fully
descend
• Back
– Lumbar curve (lordosis)
• Rectum
– Hemorrhoids
• Extremities and skin
– palmar erythema or itching early in pregnancy from a high
estrogen level and perhaps subclinical jaundice (jaundice that is
not yet apparent by a color change) from reabsorbed bilirubin be-
cause of slowed intestinal peristalsis.
– Varicosities
– Capillary refill (toes)
– Edema
• Blood Studies
– complete blood count- Hgb, Hct, WBC, Plt
– genetic screen
– serologic test for syphilis - VDRL or rapid plasma reagin test
– Blood typing (including Rh factor)
– Maternal serum for alpha-fetoprotein (AFP) - normal value
is 2.5 MOM
– indirect Coombs’ test - determination if Rh antibodies are
present in an Rh-negative woman
– Antibody titers for rubella and hepatitis B(HBsAg)
– HIV screening
– glucose loading/tolerance test – 50-gram oral 1 hour glucose
loading (OGTT)
• plasma glucose level should not exceed 140 mg/dL at 1 hour
• Urinalysis – proteinuria, glycosuria, pyuria
• Tubercolosis Test
• Ultrasonography
Risk Assessment
You might also like
- Preconception & Prenatal ScreeningDocument51 pagesPreconception & Prenatal ScreeningainaNo ratings yet
- Maternal and Fetal Wellbeing AssessmentDocument46 pagesMaternal and Fetal Wellbeing AssessmentmariaNo ratings yet
- Prenatal Care: Dr. Ruby E Robiso, Fpogs Davao Medical School Foundation, IncDocument33 pagesPrenatal Care: Dr. Ruby E Robiso, Fpogs Davao Medical School Foundation, IncISFAHAN MASULOTNo ratings yet
- Antenatal Care During The First, SecondDocument85 pagesAntenatal Care During The First, Secondasmina sihotang100% (1)
- History Taking and Physical ObstetricsDocument42 pagesHistory Taking and Physical ObstetricsCHALIE MEQU100% (1)
- Neonate-Week 1Document38 pagesNeonate-Week 1drnasir31No ratings yet
- NCM 107 Lesson 9Document18 pagesNCM 107 Lesson 9eirelav0902No ratings yet
- 1 AncDocument48 pages1 AncKaruna PrasanthNo ratings yet
- Importance of Prenatal CareDocument12 pagesImportance of Prenatal CarePinkymekala HasanparthyNo ratings yet
- Wa RaDocument17 pagesWa RaRechie RechNo ratings yet
- Identifying Clients at RiskDocument57 pagesIdentifying Clients at Riskcoosa liquors100% (1)
- Antenatal Care - Final - 27 Aug 2021Document88 pagesAntenatal Care - Final - 27 Aug 2021vrunda joshiNo ratings yet
- The High Risk Prenatal ClientDocument46 pagesThe High Risk Prenatal ClientPaul Albert Agunod100% (2)
- Antenatal CareDocument29 pagesAntenatal Careعبدالكريم الاسدNo ratings yet
- Antenatal AssessmentDocument40 pagesAntenatal AssessmentKailash NagarNo ratings yet
- Antenatal Care AssessmentDocument67 pagesAntenatal Care Assessmenthiral mistry100% (2)
- Ante Natal Care (ANC)Document34 pagesAnte Natal Care (ANC)Monazzt AsshagabNo ratings yet
- Antenatal Care During The First, SecondDocument85 pagesAntenatal Care During The First, SecondhemihemaNo ratings yet
- NCM 209 Lesson 1 FinallDocument8 pagesNCM 209 Lesson 1 Finalldanica grace gubaNo ratings yet
- Obstetric History & ExaminationDocument4 pagesObstetric History & ExaminationalifisallahNo ratings yet
- Antenatal Care Unit Two Lesson 192Document192 pagesAntenatal Care Unit Two Lesson 192RidiculouslySweetNo ratings yet
- Gynacology and Obstetrics Format For History & Physical ExaminaitonDocument13 pagesGynacology and Obstetrics Format For History & Physical ExaminaitonBayisa GirmaNo ratings yet
- IUFDDocument29 pagesIUFDfasyanneshaNo ratings yet
- Prenatal ScreeningDocument61 pagesPrenatal Screeningjoycechicago100% (1)
- MCN Quiz 2Document6 pagesMCN Quiz 2Romer RiveraNo ratings yet
- Pregnancylaboranddelivery DeliveryDocument73 pagesPregnancylaboranddelivery DeliveryAdolfo ErlisNo ratings yet
- OBGYN History and Exam EssentialsDocument61 pagesOBGYN History and Exam EssentialsEthiopia TekdemNo ratings yet
- OBGYNE Must-KnowsDocument10 pagesOBGYNE Must-KnowsPigwet KwisNo ratings yet
- Antenatal Care: Dr. Dr. I Nyoman Bayu Mahendra, Spog (K)Document38 pagesAntenatal Care: Dr. Dr. I Nyoman Bayu Mahendra, Spog (K)Anresangsya YasaNo ratings yet
- Anc Inc PNCDocument51 pagesAnc Inc PNCCharudatt ChalisgaonkarNo ratings yet
- Radha Antenatal Fetal Well Being1Document32 pagesRadha Antenatal Fetal Well Being1Shaells JoshiNo ratings yet
- PreconceptionDocument33 pagesPreconceptionGian PagadduNo ratings yet
- MCN Skills Lab 2021Document25 pagesMCN Skills Lab 2021irene mancaoNo ratings yet
- Hand Out For Pregnant Client NCM 109Document8 pagesHand Out For Pregnant Client NCM 109Allaine Royce LibrandoNo ratings yet
- 3 High Risk PregnancyDocument103 pages3 High Risk PregnancyKaguraNo ratings yet
- Antenatal CareDocument30 pagesAntenatal CareSheila WilsonNo ratings yet
- Antenatal Care Guidelines for Pregnancy Screening and Risk FactorsDocument81 pagesAntenatal Care Guidelines for Pregnancy Screening and Risk FactorsDorjee SengeNo ratings yet
- IUDDocument23 pagesIUDAang AkamaNo ratings yet
- Prenatal care guideDocument31 pagesPrenatal care guideNoraNo ratings yet
- Prenatal Care: Muthia MutmainnahDocument77 pagesPrenatal Care: Muthia MutmainnahBima NetNo ratings yet
- Preconception and Prenatal Care GuideDocument17 pagesPreconception and Prenatal Care GuideDenisse Marie SotoNo ratings yet
- Antenatal CareDocument41 pagesAntenatal CareHani NadiahNo ratings yet
- High Risk Prenatal ClientDocument10 pagesHigh Risk Prenatal ClientAudreySalvador100% (1)
- Assesment of Women in LabourDocument103 pagesAssesment of Women in Labourmikegrace02No ratings yet
- Feotal Measure: Presented by Sandhya Gupta M.SC - Nursing Previous YearDocument35 pagesFeotal Measure: Presented by Sandhya Gupta M.SC - Nursing Previous Yearsuman guptaNo ratings yet
- Prenatal Care Lecture Notes and Health TeachingsDocument12 pagesPrenatal Care Lecture Notes and Health Teachingswanda100% (2)
- Factors of Care During Pregnancy, ScreeningsDocument38 pagesFactors of Care During Pregnancy, ScreeningssabhyaNo ratings yet
- Lec 7 Prenatal CareDocument58 pagesLec 7 Prenatal CareCarmel CochingNo ratings yet
- 5 Normal PeurpuriumDocument48 pages5 Normal Peurpuriumdemeke andebetNo ratings yet
- Prenatal Care Visits Obstetrical HistoryDocument18 pagesPrenatal Care Visits Obstetrical HistoryZarlyn Miraflores100% (1)
- Antenatal CareDocument23 pagesAntenatal Caremalaika khanNo ratings yet
- Antenatal Principles of Antenatal Care 2017Document60 pagesAntenatal Principles of Antenatal Care 2017JanielWright100% (3)
- Maternal & Child HealthDocument84 pagesMaternal & Child HealthAnjum AbbasiNo ratings yet
- Prenatal Care Health AssessmentDocument25 pagesPrenatal Care Health AssessmentKatherine Nichole AgultoNo ratings yet
- Obsterics History C-I (Edited)Document14 pagesObsterics History C-I (Edited)Tamam JamalNo ratings yet
- Intra Uterine Growth Restriction (IUGR)Document44 pagesIntra Uterine Growth Restriction (IUGR)Afiqi FikriNo ratings yet
- Ante Natal Care - 2Document43 pagesAnte Natal Care - 2Dina M ElbakaryNo ratings yet
- Pre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- The Respiratory SystemDocument10 pagesThe Respiratory SystemChari RivoNo ratings yet
- NSTP 1 MODULE 4 Environmental ProtectionDocument24 pagesNSTP 1 MODULE 4 Environmental ProtectionChari RivoNo ratings yet
- Leopolds ManeuverDocument14 pagesLeopolds ManeuverChari RivoNo ratings yet
- 2022 Sept 30 DpriDocument51 pages2022 Sept 30 DpriChari RivoNo ratings yet
- Nursing Care for Postpartum Hemorrhage and InfectionDocument85 pagesNursing Care for Postpartum Hemorrhage and InfectionChari Rivo100% (1)
- cOMMON gENETIC dISORDERSDocument11 pagescOMMON gENETIC dISORDERSChari RivoNo ratings yet
- Menstrual CycleDocument45 pagesMenstrual CycleChari RivoNo ratings yet
- Legal Considerations of Maternal and Child PracticeDocument22 pagesLegal Considerations of Maternal and Child PracticeChari RivoNo ratings yet
- Nursing Care of High-Risk NewbornsDocument83 pagesNursing Care of High-Risk NewbornsChari RivoNo ratings yet
- RHD and Maternal and Child Health ConnectionDocument2 pagesRHD and Maternal and Child Health ConnectionChari RivoNo ratings yet
- Stages of Fetal Development and the Changes that OccurDocument24 pagesStages of Fetal Development and the Changes that OccurChari RivoNo ratings yet
- Physiologic SignsDocument59 pagesPhysiologic SignsChari RivoNo ratings yet
- FS1500 Foundations For Accelerated Learning OLDocument17 pagesFS1500 Foundations For Accelerated Learning OLChari RivoNo ratings yet
- Theories and Models Applicable in Maternal and ChildDocument4 pagesTheories and Models Applicable in Maternal and ChildChari RivoNo ratings yet
- COMMON REPRODUCTIVE HEALTH CONCERNS For WOMENDocument10 pagesCOMMON REPRODUCTIVE HEALTH CONCERNS For WOMENChari RivoNo ratings yet
- Fetal Development: From Conception to BirthDocument22 pagesFetal Development: From Conception to BirthChari RivoNo ratings yet
- Foundation for Maternal and Child Nursing PracticeDocument18 pagesFoundation for Maternal and Child Nursing PracticeChari RivoNo ratings yet
- High-Risk Neonate & Neurodevelopmental OutcomeDocument155 pagesHigh-Risk Neonate & Neurodevelopmental OutcomeChari RivoNo ratings yet
- Answers To The Multiple Choice Questions From Volume NumberDocument8 pagesAnswers To The Multiple Choice Questions From Volume NumberVennela Kumari.kNo ratings yet
- Safety and Efficacy of Antipsychotics in Pregnancy and Lactation 2329 6488 1000267Document7 pagesSafety and Efficacy of Antipsychotics in Pregnancy and Lactation 2329 6488 1000267Marzuqi AbdullahNo ratings yet
- Country Profile - PHLDocument8 pagesCountry Profile - PHLAlec AnonNo ratings yet
- LVN Application PDFDocument12 pagesLVN Application PDFChari RivoNo ratings yet
- Application FormDocument1 pageApplication Formsheryl maeNo ratings yet
- Abcde Abcde: Name Class QuizDocument1 pageAbcde Abcde: Name Class QuizChari RivoNo ratings yet
- LVN Application PDFDocument12 pagesLVN Application PDFChari RivoNo ratings yet
- Fluid Resuscitation Regimen For An AdultDocument1 pageFluid Resuscitation Regimen For An AdultChari RivoNo ratings yet
- Fluids, electrolytes, and body water regulation quizDocument3 pagesFluids, electrolytes, and body water regulation quizChari RivoNo ratings yet
- LVN Application PDFDocument12 pagesLVN Application PDFChari RivoNo ratings yet
- Complications of PNDocument19 pagesComplications of PNChari RivoNo ratings yet
- Our Lady of Consolation Orchestra InstrumentsDocument2 pagesOur Lady of Consolation Orchestra InstrumentsCelestian Valensario PaderangaNo ratings yet
- New Monasticism: An Interspiritual Manifesto For Contemplative Life in The 21st CenturyDocument32 pagesNew Monasticism: An Interspiritual Manifesto For Contemplative Life in The 21st CenturyWorking With Oneness100% (8)
- Australian Securities and Investments Commission V KingDocument47 pagesAustralian Securities and Investments Commission V KingCourtni HolderNo ratings yet
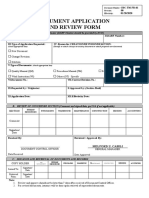
- Document Application and Review FormDocument1 pageDocument Application and Review FormJonnel CatadmanNo ratings yet
- India-An Underdeveloped Economy: (Contd )Document6 pagesIndia-An Underdeveloped Economy: (Contd )Amrita Prashant IyerNo ratings yet
- Written Work 1 Q1 Science 10Document6 pagesWritten Work 1 Q1 Science 10JOEL MONTERDENo ratings yet
- Down Syndrome Research PaperDocument11 pagesDown Syndrome Research Paperapi-299871292100% (1)
- Diesel Pump of The Desmi GroupDocument10 pagesDiesel Pump of The Desmi Groupngocdhxd92No ratings yet
- Macroeconomics QuestionnaireDocument5 pagesMacroeconomics Questionnairevikrant vardhanNo ratings yet
- NBCC Green ViewDocument12 pagesNBCC Green Views_baishyaNo ratings yet
- L.G.B.T. Fiction: Book ReviewDocument4 pagesL.G.B.T. Fiction: Book ReviewDejana KosticNo ratings yet
- On Healing Powers: Asclepius, Caduceus and AntibodiesDocument4 pagesOn Healing Powers: Asclepius, Caduceus and AntibodiesasclepiuspdfsNo ratings yet
- A Case of Haemochromatosis and Diabetes A Missed OpportunityDocument111 pagesA Case of Haemochromatosis and Diabetes A Missed Opportunitymimran1974No ratings yet
- Wiring Diagram Obp 1 v2Document5 pagesWiring Diagram Obp 1 v2Jorge Luis Vera AlmeidaNo ratings yet
- Molar Mass, Moles, Percent Composition ActivityDocument2 pagesMolar Mass, Moles, Percent Composition ActivityANGELYN SANTOSNo ratings yet
- What Is The Time Value of MoneyDocument6 pagesWhat Is The Time Value of MoneySadia JuiNo ratings yet
- Sustainable Farming FPO Promotes Natural AgricultureDocument4 pagesSustainable Farming FPO Promotes Natural AgricultureSHEKHAR SUMITNo ratings yet
- PH.D Scholars UGCDocument25 pagesPH.D Scholars UGCUsha MurthyNo ratings yet
- Surrealismo TriplevDocument13 pagesSurrealismo TriplevVictor LunaNo ratings yet
- Sponsor A Child With E-Tuition 2022Document19 pagesSponsor A Child With E-Tuition 2022nuur xiemaNo ratings yet
- Emerson Field Tools Quick Start GuideDocument48 pagesEmerson Field Tools Quick Start Guidepks_2410No ratings yet
- Thesis Chapter 123Document15 pagesThesis Chapter 123Chesca Mae PenalosaNo ratings yet
- CartridgeDocument26 pagesCartridgeMnavya SaiNo ratings yet
- Row and Cluster Housing Building Codes and Bye LawsDocument1 pageRow and Cluster Housing Building Codes and Bye Lawssadhana illaNo ratings yet
- Teaching As Noble ProfessionDocument1 pageTeaching As Noble ProfessionJeric AcostaNo ratings yet
- MarketNexus Editor: Teri Buhl Character LetterDocument2 pagesMarketNexus Editor: Teri Buhl Character LetterTeri BuhlNo ratings yet
- Bread and Pastry Production NC II 1st Edition 2016Document454 pagesBread and Pastry Production NC II 1st Edition 2016Brian Jade CadizNo ratings yet
- Registration Form Proficiency Testing Program: Name Designation Mob. / Tel. NoDocument4 pagesRegistration Form Proficiency Testing Program: Name Designation Mob. / Tel. NoOwais Manzoor MalikNo ratings yet
- CV HannahDocument3 pagesCV HannahRoxan DosdosNo ratings yet
- FS1-Episode 10Document4 pagesFS1-Episode 10Mark Gerald Lagran82% (11)