Professional Documents
Culture Documents
Bazetol
Uploaded by
pabitra0 ratings0% found this document useful (0 votes)
6 views18 pagesEpilepsy is a brain disorder involving recurrent seizures caused by abnormal electrical excitation in the brain. Seizure disorders affect about 0.5% of the population. Risk factors include family history, head injury, or other brain damage. Symptoms vary from simple staring spells to violent convulsions and loss of consciousness. Seizures are classified as either generalized, affecting all of the brain, or partial, affecting only a portion. Bazetol XR is a specially formulated carbamazepine that maintains therapeutic levels for 12 hours with twice daily dosing to minimize side effects.
Original Description:
Carbamazepine
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentEpilepsy is a brain disorder involving recurrent seizures caused by abnormal electrical excitation in the brain. Seizure disorders affect about 0.5% of the population. Risk factors include family history, head injury, or other brain damage. Symptoms vary from simple staring spells to violent convulsions and loss of consciousness. Seizures are classified as either generalized, affecting all of the brain, or partial, affecting only a portion. Bazetol XR is a specially formulated carbamazepine that maintains therapeutic levels for 12 hours with twice daily dosing to minimize side effects.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views18 pagesBazetol
Uploaded by
pabitraEpilepsy is a brain disorder involving recurrent seizures caused by abnormal electrical excitation in the brain. Seizure disorders affect about 0.5% of the population. Risk factors include family history, head injury, or other brain damage. Symptoms vary from simple staring spells to violent convulsions and loss of consciousness. Seizures are classified as either generalized, affecting all of the brain, or partial, affecting only a portion. Bazetol XR is a specially formulated carbamazepine that maintains therapeutic levels for 12 hours with twice daily dosing to minimize side effects.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 18
Epilepsy
Seizure disorder
Epilepsy is a brain disorder involving
recurrent seizures
Epilepsy is a disorder involving repeated
seizures of any type. Seizures ("fits") are
episodes of disturbed brain function that
cause changes in attention and/or
behavior. They are caused by abnormal
electrical excitation in the brain.
Seizure disorders affect about 0.5% of the
population. Approximately 1.5 to 5.0% of
the population may have a seizure in their
lifetime. Epilepsy can affect people of any
age.
Risk factors include a family history of
epilepsy, head injury, or other condition
that causes damage to the brain.
The following factors may present a risk for
worsening of seizures in a person with a
previously well-controlled seizure disorder:
Pregnancy
Lack of sleep
Skipping doses of epilepsy medications
Use of alcohol or other recreational drugs
Certain prescribed medications
Illness
Symptoms
The severity of symptoms can vary greatly
from simple staring spells to loss of
consciousness and violent convulsions. For
many patients, the event is stereotyped (the
same thing over and over) while some
patients have many different types of
seizures that cause different symptoms each
time.
The type of seizure a person experiences
depends on a variety of factors, such as the
part of the brain affected, the cause, and
individual response
SYMPTOMS OF GENERALIZED
SEIZURES
Generalized seizures affect all or most of the brain.
They include petit mal and grand mal seizures.
Petit mal seizures:
Minimal or no movements (usually, except for "eye
blinking") -- may appear like a blank stare
Brief sudden loss of awareness or conscious
activity -- may only last seconds
Recurs many times
Occurs most often during childhood
Decreased learning (child often thought to be day-
dreaming)
Tonic-clonic (grand mal) seizures:
Whole body, violent muscle contractions
Rigid and stiff
Affects a major portion of the body
Loss of consciousness
Breathing stops temporarily, then "sighing"
Incontinence of urine
Tongue or cheek biting
Confusion following the seizure
Weakness following the seizure (Todd's
paralysis)
SYMPTOMS OF PARTIAL
SEIZURES
Partial seizures affect only a portion of the brain.
Simple partial (focal) seizures:
Muscle contractions of a specific body part
Abnormal sensations
May have nausea, sweating, skin flushing and
dilated pupils
May have other focal (localized) symptoms
Partial complex seizures:
Automatism (automatic performance of complex
behaviors without conscious awareness)
Abnormal sensations
May have nausea, sweating, skin flushing and dilated
pupils
May have other focal (localized) symptoms
Recalled or inappropriate emotions
Changes in personality or alertness
May or may not lose consciousness
Olfactory (smell) or gustatory (taste) hallucinations or
impairments -- if the epilepsy is focused in the temporal
lobe of the brain.
Bazetol XR is a specially designed
formulation that minimizes the sudden rise
in peak concentration (cmax), maintains it
within the therapeutic range, avoiding the
peak concentration – related troublesome
side –defects. It also offers convenient BID
dosage schedule because of sustained
action. Thus Bazetol XR is a major
breakthrough in carbamazepine therapy.
Mode of Action:
Exact mechanism of action is not clearly
understood. It is believed that carbamazepine
produces differential inhibition of high frequency
discharges in and around epileptic foci with
minimal disruption of normal neuronal traffic by
inhibiting voltage –sensitive sodium channels.
Carbamazepine also alters most of the classical
neurotransmitters such as dopamine,
noradrenalin, serotonin and noradrenalin
explains its usefulness in a complex disorder
known as manic depressive or depression
(swinging between two extreme poles of mania
and depression).
PHARMACOKINETICS
Absorption:
Bazetol-XR is slowly absorbed from the gastrointestinal
tract, in such a manner that the peak levels achieved are
within therapeutic range and are maintained for 12
hours. Consequently, the side effects due to high plasma
levels are reduced.
Metabolism:
Bazetol XR is metabolized in the liver and it induces its
own metabolism. As a result the half life which is long
(50 to 60 hours) after the first dose is reduced to 5 to 24
hours at steady state levels .The metabolite of Bazetol
XR is active.
Distribution:
Bazetol XR is distribution rapidly in all tissues.
Excretion:
Mainly by kidney (72%) and also in the faeces (28%).
INDICATIONS
All types of epilepsy except absence seizures
Trigeminal neuralgia (Pain in the trigeminal
nerve, which sends intense pain shooting across
the face)
Manic depressive psychosis (Bipolar
depression)
Diabetic Neuropathy (Degeneration of tissues
of the nervous system due to diabetes).
Schizophrenia, in combination with other anti-
psychotics
Alcohol withdrawal syndrome.
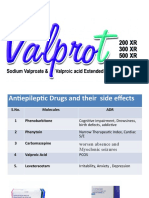
ADVERSE EFFECTS
Adverse effects are much less as compared to
plain carbamazepine formulation. However side
effects may occur in the initial period of starting
the treatment and they disappear spontaneously
within 7 to 14 days or following a temporary
reduction in dosage. The following adverse
effects are considered to be dangerous and
requires stoppage of treatment. These are
aplastic anemia, agranulocytosis, bone marrow
depression, and thrombocytopenia.
CONTRAINDICATION
Hypersensitivity to Carbamazepine, AV block,
Severe Cardiovascular, Hepatic and renal
disorders are the contraindications to the use of
Bazetol XR.
USE IN PREGNANCY AND LACTATION
Bazetol XR is not administered routinely in
pregnant women as well as lactating women. If
need arise, Carbamazepine is considered to be
the safest anti- epileptic drug in pregnant or
lactating women.
OVER DOSAGE
Over dosage may produce tremor, excitation
convulsion changes in blood pressure and
coma. Over dosage is seen after ingestion of 30
to 60 gm of carbamazepine . There is no specific
antidote and the patient is treated with
supportive treatment consisting of gastric
lavage, activated charcoal and if necessary
administration of benzodiazepine.
DRUG INTERACTION
Combination with phenytoin, phenobarbitone or
primidone causes lowering of blood levels of
carbamazepine resulting in relapse of the disease unless
the dose of carbamazepine is increased. (These drugs
induce the liver enzymes which result in more
metabolism of carbamazepine).
Carbamazepine increase the metabolism of warfarin,
doxycycline, and theophylline. (This is so because it
induces the liver enzyme which is involved in metabolism
of these drugs).
Blood levels of co administered haloperidol are reduced.
Concomitant administration of carbamazepine with
erythromycin, cimetidine, propoxyphen and isoniazide
cause elevated plasma levels of carbamazepine and its
side effects. ( Since these drugs inhibit the metabolizing
enzyme).
THANK YOU
You might also like
- Psychiatry Pharmacology J. Psychiatry' AntidepressantsDocument9 pagesPsychiatry Pharmacology J. Psychiatry' AntidepressantssumithjalyNo ratings yet
- Drug List PsychopharmDocument23 pagesDrug List PsychopharmGeorge HananiaNo ratings yet
- Psychopharmacology in PsychiatryDocument94 pagesPsychopharmacology in PsychiatryOslo SaputraNo ratings yet
- Basic Medial Science of The Kidney: The Scientific Basis of Clinical Disease, Marc Imhotep Cray, M.D.Document193 pagesBasic Medial Science of The Kidney: The Scientific Basis of Clinical Disease, Marc Imhotep Cray, M.D.Marc Imhotep Cray, M.D.100% (3)
- Get Rid of Lipomas Naturally With These 3 Home Remedies!Document10 pagesGet Rid of Lipomas Naturally With These 3 Home Remedies!XICMENNo ratings yet
- The World of Darkness - Merit's Compendium 3Document200 pagesThe World of Darkness - Merit's Compendium 3Sam Thornton100% (1)
- Luo Circumcision Rites: © Dan Omondi K'Aoko 1986Document17 pagesLuo Circumcision Rites: © Dan Omondi K'Aoko 1986Prince AliNo ratings yet
- Oils of MetalsDocument9 pagesOils of Metalsmichael777No ratings yet
- Antiepileptic FullDocument60 pagesAntiepileptic FullBurning DesireNo ratings yet
- A Simple Guide to Hand Tremors, Related Diseases and Use in Disease DiagnosisFrom EverandA Simple Guide to Hand Tremors, Related Diseases and Use in Disease DiagnosisRating: 3.5 out of 5 stars3.5/5 (3)
- Antiepileptics (Autosaved)Document57 pagesAntiepileptics (Autosaved)vishal singhNo ratings yet
- Australian Medicines Handbook Pty LTDDocument5 pagesAustralian Medicines Handbook Pty LTDDia Sb67% (3)
- 10 Herbal Plants (Halamang Gamot) Approved by The DOH.: Name (Tagalog & English) Scientific Name Description Uses FiguresDocument2 pages10 Herbal Plants (Halamang Gamot) Approved by The DOH.: Name (Tagalog & English) Scientific Name Description Uses FiguresSha Zaenudin100% (2)
- Guidelines of Arterial Duplex ScanDocument23 pagesGuidelines of Arterial Duplex ScanMohamed Omar Elfarok100% (1)
- Drug PresentationDocument32 pagesDrug PresentationManisha ShakyaNo ratings yet
- DiazepamDocument2 pagesDiazepamgoyaNo ratings yet
- Assignment On PrionsDocument22 pagesAssignment On PrionsRinta Moon100% (3)
- COPDDocument55 pagesCOPDRetno Lies SetiyowatiNo ratings yet
- IVT Checklist For StudentsDocument9 pagesIVT Checklist For StudentsNoorwashila100% (1)
- Pharmacology. Sedative HypnoticDocument16 pagesPharmacology. Sedative HypnoticJean FlorencondiaNo ratings yet
- AnxiolyticsDocument23 pagesAnxiolyticsNalafNo ratings yet
- Anti-Epileptics: Awale YusufDocument42 pagesAnti-Epileptics: Awale Yusufahmed mahamedNo ratings yet
- TabletsDocument6 pagesTabletsRupesh Kumar DuttaNo ratings yet
- Antiepileptic DrugsDocument24 pagesAntiepileptic Drugsjanemwanza003No ratings yet
- Anti-Convulsants/Antiepileptic Drugs: Prepared By: DR Sana FaheemDocument23 pagesAnti-Convulsants/Antiepileptic Drugs: Prepared By: DR Sana Faheemaziz aliNo ratings yet
- Anti-Epilepsy Agents: Prepared By: Gerald R. Oriña BSN-2B Mrs. Jessica SabasDocument32 pagesAnti-Epilepsy Agents: Prepared By: Gerald R. Oriña BSN-2B Mrs. Jessica SabasGerald Resubal OriñaNo ratings yet
- Anticonvulsants NotesDocument19 pagesAnticonvulsants NotesPIRENANo ratings yet
- Movement DisordersDocument28 pagesMovement DisordersAhmad WaliNo ratings yet
- Antiepileptic Drug: Presented by Prerna Surana Yukta Mehta Sarfa MalickDocument65 pagesAntiepileptic Drug: Presented by Prerna Surana Yukta Mehta Sarfa Malick33 Momin SarahNo ratings yet
- Anti Psychotic DrugsDocument6 pagesAnti Psychotic DrugsJoseph NyirongoNo ratings yet
- Antipsychotics 27042022 103124am 21102022 020159pm 23062023 020410pmDocument27 pagesAntipsychotics 27042022 103124am 21102022 020159pm 23062023 020410pmMuhammad ZubairNo ratings yet
- CNS 2022Document8 pagesCNS 2022Kathleen Kate MonsalveNo ratings yet
- Is A Group of Chronic Syndromes Characterized by Recurrent Seizures With Periods of ConsciousnessDocument29 pagesIs A Group of Chronic Syndromes Characterized by Recurrent Seizures With Periods of ConsciousnessJulius MendozaNo ratings yet
- Sedative - HypnoticsDocument62 pagesSedative - HypnoticsvijayNo ratings yet
- Randa Al-Harizy Prof of Internal MedicineDocument40 pagesRanda Al-Harizy Prof of Internal MedicinerafikaNo ratings yet
- PrognosisDocument8 pagesPrognosisallkhusairy6tuansiNo ratings yet
- AmbroxolDocument4 pagesAmbroxoldiannuryandaNo ratings yet
- Medications For The ElderlyDocument8 pagesMedications For The ElderlyShawn TaylorNo ratings yet
- Anti Parkinson Disease - PDF - Pharmacology - AssignmentDocument11 pagesAnti Parkinson Disease - PDF - Pharmacology - AssignmentMr HotmasterNo ratings yet
- MNS Care For MO - Neurological DisordersDocument42 pagesMNS Care For MO - Neurological DisordersfatehmaanNo ratings yet
- Sedative - HypnoticsDocument60 pagesSedative - HypnoticsNurul AinNo ratings yet
- LEXOTANIL Bromazepam MeppoDocument4 pagesLEXOTANIL Bromazepam MeppoTkt Sheik AbdullahNo ratings yet
- 7) 13 AntiepilepticsDocument27 pages7) 13 AntiepilepticsKhushboo IkramNo ratings yet
- EpilepsyDocument28 pagesEpilepsybabon3No ratings yet
- AnticonvulsantDocument37 pagesAnticonvulsantPamela MendozaNo ratings yet
- Notes For Diazepam and Other DrugsDocument1 pageNotes For Diazepam and Other DrugsVanessa HabajabNo ratings yet
- Antiseizure age-WPS OfficeDocument15 pagesAntiseizure age-WPS Officermconvidhya sri2015No ratings yet
- Drugs Affecting The Central Nervous SystemDocument16 pagesDrugs Affecting The Central Nervous SystemShafaqNo ratings yet
- Sedative & Hypnotics: Prof. Hanan Hagar Pharmacology Department Medical College King Saud UniversityDocument51 pagesSedative & Hypnotics: Prof. Hanan Hagar Pharmacology Department Medical College King Saud UniversityRose Ann Raquiza-PeranteNo ratings yet
- Anti Parkinson DrugsDocument33 pagesAnti Parkinson Drugsraina3546No ratings yet
- Disease Spotlight: Neuromuscular AbnormalitiesDocument6 pagesDisease Spotlight: Neuromuscular AbnormalitiesLorie Yvonne Quibin AgullanaNo ratings yet
- Pharma Nervous Day 2Document76 pagesPharma Nervous Day 2Nhelia Santos BañagaNo ratings yet
- Drugs That Affect The Neuromuscular SystemDocument12 pagesDrugs That Affect The Neuromuscular SystemARNOLITO LUCENANo ratings yet
- Anti Epileptic AgentsDocument78 pagesAnti Epileptic AgentsPrincess VanquirayNo ratings yet
- ICU PharmacologyDocument18 pagesICU PharmacologyIrsani FeniliaNo ratings yet
- Epilepsy: Neurovascular DisordersDocument30 pagesEpilepsy: Neurovascular DisordersNdoo NdooNo ratings yet
- Pertimbangan Pemilihan Obat Anti Epilepsi DR Nelly Edit 23 JanDocument53 pagesPertimbangan Pemilihan Obat Anti Epilepsi DR Nelly Edit 23 Janvenus002No ratings yet
- Anti Epileptic AgentsDocument64 pagesAnti Epileptic AgentsPrincess VanquirayNo ratings yet
- ICU Pharmacology: Sean Forsythe M.D. Assistant Professor of MedicineDocument52 pagesICU Pharmacology: Sean Forsythe M.D. Assistant Professor of Medicinecoolboy1990No ratings yet
- ReghDocument9 pagesReghreghpineda28No ratings yet
- Pharmacology of The Central Nervous System-1Document163 pagesPharmacology of The Central Nervous System-1Gølà Sèèñàà–baale irraaNo ratings yet
- DrugsDocument13 pagesDrugsChristine UdhayNo ratings yet
- Movement DisordersDocument28 pagesMovement DisordersSheron MathewNo ratings yet
- Exam 6 Study GuideDocument27 pagesExam 6 Study GuideBrandi WeaverNo ratings yet
- DiazepamDocument6 pagesDiazepamF - TOMELDAN, CERESNo ratings yet
- Anxiolytic & Hypnotics Part 2Document24 pagesAnxiolytic & Hypnotics Part 2Sarah ArkanNo ratings yet
- Pharm 2 TESTDocument26 pagesPharm 2 TESTRachel MackeyNo ratings yet
- Dr. Rahul Trivedi B.R.Nahata College of Pharmacy, Department of Pharmacy, Mandsaur UniversityDocument16 pagesDr. Rahul Trivedi B.R.Nahata College of Pharmacy, Department of Pharmacy, Mandsaur UniversityVampire VampireNo ratings yet
- Antiepileptic Drugs.Document32 pagesAntiepileptic Drugs.pabitraNo ratings yet
- Mania HypomaniaDocument2 pagesMania HypomaniapabitraNo ratings yet
- ValprotDocument35 pagesValprotpabitraNo ratings yet
- 18aantiepileptic Drugs With ClobazamDocument29 pages18aantiepileptic Drugs With ClobazampabitraNo ratings yet
- hYPO DRUGDocument17 pageshYPO DRUGpabitraNo ratings yet
- Antipsychotic Present and FutureDocument34 pagesAntipsychotic Present and FuturepabitraNo ratings yet
- Authorization: - , To Use My Blood Donation Card With National BloodDocument1 pageAuthorization: - , To Use My Blood Donation Card With National BloodQC TownhomesNo ratings yet
- Certificate Mini Par OBDocument3 pagesCertificate Mini Par OBEmman TiempoNo ratings yet
- Anterior-Posterior Chest Exam PhotoguideDocument9 pagesAnterior-Posterior Chest Exam PhotoguideMark GuirguisNo ratings yet
- D1. Neurologic Examination PDFDocument33 pagesD1. Neurologic Examination PDFRamona-Stela CzakoNo ratings yet
- Error Recognition: Having Chose (A) The Topics For (B) Their Essays, The Students (C) Were Instructed To Make Either ADocument1 pageError Recognition: Having Chose (A) The Topics For (B) Their Essays, The Students (C) Were Instructed To Make Either AElisabeth Febry LianNo ratings yet
- Stock Pt. Kuda Mas Jms 12 April 2023 (Oot) : Nama Barang Grup Barang Satuan Harga Stock ExpiredDocument1 pageStock Pt. Kuda Mas Jms 12 April 2023 (Oot) : Nama Barang Grup Barang Satuan Harga Stock ExpiredAndre DizzaNo ratings yet
- Information Booklet 1 PDFDocument40 pagesInformation Booklet 1 PDFVandana RanaNo ratings yet
- Bulacan State University College of Nursing: Bulsu-Op-Con-23F15 Revision: 0Document6 pagesBulacan State University College of Nursing: Bulsu-Op-Con-23F15 Revision: 0Richmon SantosNo ratings yet
- Disturbance of Pigment MetabolismDocument37 pagesDisturbance of Pigment MetabolismKaushik BhuvaNo ratings yet
- PriceList En2022239251Document1,396 pagesPriceList En2022239251oliur1988bdNo ratings yet
- Generic Substitution Binu ThapaDocument13 pagesGeneric Substitution Binu ThapabimuNo ratings yet
- JawetzDocument3 pagesJawetzAvissa Fadlika DausawatiNo ratings yet
- The Adventure of Self-Discovery: Stanislav Grof, M.DDocument2 pagesThe Adventure of Self-Discovery: Stanislav Grof, M.DNoxroy PowellNo ratings yet
- AnuriaDocument4 pagesAnuriachoobiNo ratings yet
- Pixl 201101 AHLDocument26 pagesPixl 201101 AHLJuan Camilo MateusNo ratings yet
- P ('t':'3', 'I':'3053926525') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document14 pagesP ('t':'3', 'I':'3053926525') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Ni Wayan Ana PsNo ratings yet
- Terminology and Classification of The Cortical Dysplasias PalminiDocument9 pagesTerminology and Classification of The Cortical Dysplasias PalminiAyhan BölükNo ratings yet
- Intern Preceptor Guild ITP AgreementDocument10 pagesIntern Preceptor Guild ITP AgreementmelancholymelonNo ratings yet
- Verapamil PDFDocument13 pagesVerapamil PDFddandan_2No ratings yet