0% found this document useful (0 votes)
22 views15 pagesPrematurity
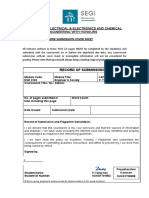
The document outlines the definitions, classifications, and complications associated with prematurity and low birth weight (LBW) in infants. It discusses predisposing factors, management strategies, and the importance of Kangaroo Mother Care (KMC) for improving outcomes in these vulnerable newborns. Additionally, it highlights key danger signs that caregivers should monitor for in preterm and LBW infants.
Uploaded by
Arthur ChibondoCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
22 views15 pagesPrematurity
The document outlines the definitions, classifications, and complications associated with prematurity and low birth weight (LBW) in infants. It discusses predisposing factors, management strategies, and the importance of Kangaroo Mother Care (KMC) for improving outcomes in these vulnerable newborns. Additionally, it highlights key danger signs that caregivers should monitor for in preterm and LBW infants.
Uploaded by
Arthur ChibondoCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd