Professional Documents
Culture Documents
Intrauterine Growth Restriction: Low Infant Birth Weight
Uploaded by
Louwella Ramos0 ratings0% found this document useful (0 votes)
17 views3 pagesBabies with a birth weight less than 2500g are considered low birth weight. Very low birth weight is defined as 1500g or less, and extremely low birth weight is less than 1000g. Low birth weight can be caused by preterm birth or being small for gestational age. After birth, optimal management includes clearing airways, delayed cord clamping, warmth, monitoring, and gentle stimulation to recreate the in utero environment. Long term care involves careful feeding, nutrition, oxygen therapy if needed, and family support to help the infant thrive.
Original Description:
Original Title
Low-infant-Birth-weight
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentBabies with a birth weight less than 2500g are considered low birth weight. Very low birth weight is defined as 1500g or less, and extremely low birth weight is less than 1000g. Low birth weight can be caused by preterm birth or being small for gestational age. After birth, optimal management includes clearing airways, delayed cord clamping, warmth, monitoring, and gentle stimulation to recreate the in utero environment. Long term care involves careful feeding, nutrition, oxygen therapy if needed, and family support to help the infant thrive.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
17 views3 pagesIntrauterine Growth Restriction: Low Infant Birth Weight
Uploaded by
Louwella RamosBabies with a birth weight less than 2500g are considered low birth weight. Very low birth weight is defined as 1500g or less, and extremely low birth weight is less than 1000g. Low birth weight can be caused by preterm birth or being small for gestational age. After birth, optimal management includes clearing airways, delayed cord clamping, warmth, monitoring, and gentle stimulation to recreate the in utero environment. Long term care involves careful feeding, nutrition, oxygen therapy if needed, and family support to help the infant thrive.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
Low infant Birth weight
Babies with a birth weight less than 2500g, irrespective of the period of their gestation are classified as low infant birth weight.
Very low birth weight is 1500g or less while extremely low birth weight is less than 1000g.
Causes
Preterm: the growth potential is normal and is appropriate for gestational period.
SGA (small for gestational age):
o Constitutionally Small: they are most of the time genetic but the baby is well and healthy.
o IUGR (Intrauterine growth restriction) by pathological process
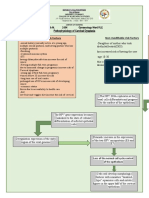
Low Infant birth weight/very low or extremely low birth weigh
Optimal Management at birth
Air passage cleared by mucus
Delayed clamping of cord helps in improving iron store
but lead to hypervolemia and hyperbilirubinemia. So
clamp the cord quickly
Promptly dry, keep effectively covered and warm
Vit K 0.5mg IM
Vital signs monitoring
Activity and behavior Monitoring
Color of the skin: Pink, Pale Grey, Blue, Yellow
Tissue Perfusion pink colour, capillary refill over upper
chest <2sec, warm and pink extremities, normal BP,
Urine output >1.5 ml/kg/hr, absence of metabolic
acidosis, lack of disparity between Pa02 and SPO2
Monitor ABG and Electrolyte (needs doctors order)
Tolerance of feeds: vomiting, gastric residuals and
abdominal girth
Look for development of apnoeic attack (absent of
breath), sepsis
After Birth
Provide in uterus milieu by
Create soft comfortable nestled and cushioned bed
Avoid excessive light, sound, rough
handling and painful procedures. Use effective
sedation and analgesia for procedures
Provide warmth and ensure asepsis
Prevent evaporative skin losses by effectively covering
the baby, application of oil or liquid paraffin
Provide effective and safe oxygenation
Provide parenteral nutrition partially and give trophic
feeds with EBM (expressed breast milk)
Provide tactile and kinetic stimulation- skin to skin
contact, interaction, music caressing and cuddling
Most love to lie in a prone position, cry less and feels
more comfortable
Relieves abdominal discomfort by passage of flatus
and reduce risk of aspiration.
Increase ventilation and increase dynamic lung compliance
and enhance arterial oxygenation
Unsupervised prone position beyond neonatal period
recognized as a risk factor for SIDS (sudden Infant Death
Syndrome)
Provide thermal comfort
Pre warmed open care system or incubator should be
available
Care in a thermoneutral environment with servo
sensor geared to maintain skin temperature of mid
epigastric region at 36.5 degrees Celsius
Application of oil or liquid paraffin reduce convective
heat loss and evaporative water loss
Extremely low babies covered with cellophane or thin
transparent plastic sheet to prevent convective and
evaporative losses from skin
As soon as condition stabilises effectively clothe the
baby
Partial kangaroo care to prevent hypothermia
Oxygen therapy
Oxygen should be administered with a head box when
saturation is less than 85% and withdrawn gradually
when >90%
Phototherapy
Jaundice is common due to immaturity, hypoxia,
hypoglycaemia, infections and hypothermia Normal
jaundice is within first 24 hours after birth, if exceeded
can be consider pathologic Jaundice.
Due to immaturity of blood brain barrier,
hyperproteinaemia and perinatal distress factors
bilirubin brain damage may occur at relatively lower
level
Initiate phototherapy early
Prevention of nosocomial infection
Handling should be reduced to minimum
Vigilance maintained on all procedures
Feeding and Nutrition (Collaborative)
Babies with weight < 1200g or gestational age < 30
weeks and sick baby should be started on IV dextrose
solution. Wt.> 1000g: 10% dextrose while Wt. <1000g:
5% dextrose
Trophic Feeds with EBM (1-2Ml 4 times a day,
Through NG tube can be started in all babies
irrespective of birth weight
When stabilized enteral feeds are begun with EBM
starting with a volume of 30 ml/kg/day on day1
Depending on tolerance feeds increased by 10-20
ml/kg/day every day and IVF are reduced
Nutritional Supplements (Collaborative)
When baby is stable, EBM can be fortified with human
milk fortifier (HMF) for additional calories and protein.
Multivitamin drop containing folic acid started at 2
weeks of age
Iron Supplements after 2-3 weeks
Vitamin E which prevents powerful antioxidant and
prevent haemolytic anaemia and enema
Gentle Rhythmic Stimulation
Gentle touch, massage, cuddling, stroke and flexing by
the nurse or preferably by mother
Soothing auditory stimuli can be given to preterm
baby in the form of family voices or music
Visual input provided with the help of coloured object,
diffuse light and eye to eye contact
Utility of Corticosteroids (Collaborative)
In infants who did not receive antenatal steroids a
single dose of dexamethasone 0.2 mg/kg iv at 4 hours
of age is recommended in very LBW babies.
Weight Record
Accurate weighing is a sensitive index of well being
Most LBW babies’ loss weight during 1st 3 to 4days of
life up to 10 to 15% of birth weight
The weight remains stationary for next 4 to 5 days
then starts to gain at a rate of 1.0 to 1.5% of body
weight per day and regain birth weight by the end of
2nd week.
Immunization
The dose is not reduced in preterm babies
Administer 0-day vaccine on the day of discharge
Family Support
The frightened seen of NICU should be demystified
Family should be constantly informed and involved in
care of baby
Mother should be encouraging to touch and talk with
her baby and provide routine care under guidance of
nurses
Assist to provide kangaroo care
Transfer From to Cot
Baby who is feeding well, reasonably active with a
stable body temperature irrespective of weight
qualified for transfer to open cot
The baby should be observed for another 12 hours
after putting incubator off
You might also like
- Care of Iugr and Low Birth Weight BabiesDocument30 pagesCare of Iugr and Low Birth Weight BabiesjessyNo ratings yet
- Review UNIT XI High Risk NewbornDocument20 pagesReview UNIT XI High Risk NewbornShehana ShihabNo ratings yet
- Low Birth Weight NoteDocument9 pagesLow Birth Weight Notesushma shrestha100% (1)
- High Risk NewbornDocument19 pagesHigh Risk Newbornsantosh s u100% (1)
- Anthropometric MeasurementsDocument3 pagesAnthropometric Measurementssabao kizuiteNo ratings yet
- MCN FinalsDocument40 pagesMCN Finalsmolderoirish600No ratings yet
- MCNDocument12 pagesMCNIan CarodanNo ratings yet
- High Risk Newborn 1Document101 pagesHigh Risk Newborn 1f8kcznbdqjNo ratings yet
- 5 Idol Ko Si Nanay Module 5Document48 pages5 Idol Ko Si Nanay Module 5Mash JumahariNo ratings yet
- Breast FeedingDocument33 pagesBreast Feedingjulie kisku100% (1)
- Unciano Colleges Inc. Sta. Mesa ManilaDocument14 pagesUnciano Colleges Inc. Sta. Mesa Manilanaman24No ratings yet
- WelcomeDocument103 pagesWelcomeLyka BernalNo ratings yet
- Baby at Risk - Koros E.k-1-1-1-1Document132 pagesBaby at Risk - Koros E.k-1-1-1-1victorNo ratings yet
- Post Mature Newborn: Gervacio, Jonah Micah NDocument20 pagesPost Mature Newborn: Gervacio, Jonah Micah NJessa BorreNo ratings yet
- PrematurityDocument66 pagesPrematurityJolmajas JoharNo ratings yet
- Hesi Review For MaternityDocument29 pagesHesi Review For MaternitySteam Lc86% (21)
- MCN LECTURE Final Coaching 2223Document37 pagesMCN LECTURE Final Coaching 22239tfvnv4ghzNo ratings yet
- High-Risk Newborn: Complications Associated With Gestational Age and DevelopmentDocument97 pagesHigh-Risk Newborn: Complications Associated With Gestational Age and DevelopmentALYSSA NICOLE GINESNo ratings yet
- My Paediatric NotesDocument14 pagesMy Paediatric NotesTicky TomNo ratings yet
- Nursing Care of Low Birth Weight BabiesDocument10 pagesNursing Care of Low Birth Weight BabiesAnnisa Yusuf80% (5)
- EincDocument14 pagesEincmendoza jhamNo ratings yet
- Week 9 NCM 109 LectureDocument63 pagesWeek 9 NCM 109 LecturePolicarpio AprilNo ratings yet
- Essential Newborn CareDocument14 pagesEssential Newborn CareJam Corros100% (1)
- Maternity and Newborn Nursing ReviewerDocument20 pagesMaternity and Newborn Nursing ReviewerNick RealinoNo ratings yet
- NICU Protocol 100Document76 pagesNICU Protocol 100Catherine Lee100% (1)
- PCBF KpjrawangDocument48 pagesPCBF KpjrawangDr Puteri Nur Sabrina Binti Mohd HanapiNo ratings yet
- MCN Reviewer: Basic ConceptsDocument22 pagesMCN Reviewer: Basic ConceptsPanJan BalNo ratings yet
- BreastfeedingDocument26 pagesBreastfeedingDee SarajanNo ratings yet
- Preterm Infant: Case StudyDocument39 pagesPreterm Infant: Case StudyRey De LunaNo ratings yet
- Assessment Scientific Basis Plan of Care Intervention With Rationale Evaluation Subjective: IndependentDocument16 pagesAssessment Scientific Basis Plan of Care Intervention With Rationale Evaluation Subjective: IndependentAbdullah Mascardo BarabagNo ratings yet
- Maternity and Newborn Nursing ReviewerDocument40 pagesMaternity and Newborn Nursing Reviewerrahkel08No ratings yet
- Pengelolaan Bayi Baru LahirDocument19 pagesPengelolaan Bayi Baru LahirekaNo ratings yet
- Baby at Risk (NBU) NotesDocument131 pagesBaby at Risk (NBU) NotesMercy KeruboNo ratings yet
- Immediate Newborn Care. BlanksDocument11 pagesImmediate Newborn Care. BlanksMay Princes Torregosa Abucejo100% (1)
- Activity 4 NCM 109Document10 pagesActivity 4 NCM 109Angelica BernalesNo ratings yet
- Maternal and Child Health Nursing.Document32 pagesMaternal and Child Health Nursing.Ace FabrigasNo ratings yet
- Pengelolaan Bayi Baru LahirDocument19 pagesPengelolaan Bayi Baru LahirekaNo ratings yet
- Post Partum PeriodDocument31 pagesPost Partum PeriodMay CaballeroNo ratings yet
- High-Risk Newborns and Child During Illness and Hospitalization - Pediatric NursingDocument200 pagesHigh-Risk Newborns and Child During Illness and Hospitalization - Pediatric Nursingjaggermeister20100% (8)
- General Guides To Daily Nicu Practice: Birth Weight (GM) Age To Start Feeding (Day)Document75 pagesGeneral Guides To Daily Nicu Practice: Birth Weight (GM) Age To Start Feeding (Day)Humayun NasserNo ratings yet
- Care of New BornDocument14 pagesCare of New Bornshubham vermaNo ratings yet
- Newborn1Document68 pagesNewborn1Michelle FactoNo ratings yet
- Nursing Care of Newborn and FamilyDocument38 pagesNursing Care of Newborn and FamilyLady Jane CaguladaNo ratings yet
- Case Study (Summer)Document30 pagesCase Study (Summer)dave del rosarioNo ratings yet
- Postpartum Physical AssessmentDocument60 pagesPostpartum Physical AssessmentJhgrace Mary Pacaña Gallo100% (1)
- 2020 Immediate Care of The Newborn 3Document56 pages2020 Immediate Care of The Newborn 3Ellah PerenioNo ratings yet
- Care of Preterm Babies: Chinchu.MDocument59 pagesCare of Preterm Babies: Chinchu.MChinchu MohanNo ratings yet
- Nicu Case StudyDocument4 pagesNicu Case Studyapi-508102663No ratings yet
- NewbornDocument193 pagesNewbornKenneth Myro Garcia100% (1)
- Phototherapy: Presented byDocument49 pagesPhototherapy: Presented byKevin RaiyaniNo ratings yet
- Maternal Nursing BulletDocument37 pagesMaternal Nursing BulletShane ArroyoNo ratings yet
- PEDIAPrelims - 2. Care of The Newborn 1 (First 24 Hours To Vital Signs)Document7 pagesPEDIAPrelims - 2. Care of The Newborn 1 (First 24 Hours To Vital Signs)RenatoCosmeGalvanJuniorNo ratings yet
- Postpartum Physical AssessmentDocument60 pagesPostpartum Physical Assessmentalmyr_rimandoNo ratings yet
- Pedia 2Document30 pagesPedia 2regNo ratings yet
- A. Cardiovascular System: Physiological Effects of Labor On A MotherDocument4 pagesA. Cardiovascular System: Physiological Effects of Labor On A MotherStudent NurseNo ratings yet
- LBWDocument39 pagesLBWJOSLINNo ratings yet
- The Care and Feeding of Children A Catechism for the Use of Mothers and Children's NursesFrom EverandThe Care and Feeding of Children A Catechism for the Use of Mothers and Children's NursesNo ratings yet
- "Nurturing Beginnings: A Comprehensive Guide to Breastfeeding Success"From Everand"Nurturing Beginnings: A Comprehensive Guide to Breastfeeding Success"No ratings yet
- Standing Order SheetDocument1 pageStanding Order SheetLouwella RamosNo ratings yet
- Ramos, LF - 2BN - LFDDocument1 pageRamos, LF - 2BN - LFDLouwella RamosNo ratings yet
- Bryan Beran: Barangay Captain, RizalDocument1 pageBryan Beran: Barangay Captain, RizalLouwella RamosNo ratings yet
- Project ProposalDocument5 pagesProject ProposalLouwella RamosNo ratings yet
- RAMOS, LOUWELLA 2 BN International Health Information Regulatory BodiesDocument2 pagesRAMOS, LOUWELLA 2 BN International Health Information Regulatory BodiesLouwella RamosNo ratings yet
- Program Proposal FinalDocument5 pagesProgram Proposal FinalLouwella RamosNo ratings yet
- Survey Questionnaire Pacheckk 4444Document11 pagesSurvey Questionnaire Pacheckk 4444Louwella RamosNo ratings yet
- COPAR Chapter 10Document2 pagesCOPAR Chapter 10Louwella RamosNo ratings yet
- Ramos - Cervical-DysplasiaDocument1 pageRamos - Cervical-DysplasiaLouwella RamosNo ratings yet
- Ramos - Pathophysiology PCOSDocument1 pageRamos - Pathophysiology PCOSLouwella RamosNo ratings yet
- Coahs Medical Center: Date/Tim E Focus Data, Action, ResponseDocument4 pagesCoahs Medical Center: Date/Tim E Focus Data, Action, ResponseLouwella RamosNo ratings yet
- Copar Ii BN Survey 2Document4 pagesCopar Ii BN Survey 2Louwella RamosNo ratings yet
- Coahs Medical Center: Date/Time Focus Data, Action, ResponseDocument4 pagesCoahs Medical Center: Date/Time Focus Data, Action, ResponseLouwella RamosNo ratings yet
- Adequate InadequateDocument6 pagesAdequate InadequateLouwella RamosNo ratings yet
- Cycling: Ramos, Louwella Faith M. 2-BNDocument7 pagesCycling: Ramos, Louwella Faith M. 2-BNLouwella RamosNo ratings yet
- Copar Ii BN SurveyDocument4 pagesCopar Ii BN SurveyLouwella RamosNo ratings yet
- Drug Name Mechanism of Action Indication Side Effects/ Adverse Reaction Contraindication Nursing ConsiderationsDocument2 pagesDrug Name Mechanism of Action Indication Side Effects/ Adverse Reaction Contraindication Nursing ConsiderationsLouwella RamosNo ratings yet
- Cues/Data Nursing Diagnosis Interference Planning Intervention Rationale EvaluationDocument3 pagesCues/Data Nursing Diagnosis Interference Planning Intervention Rationale EvaluationLouwella RamosNo ratings yet
- Coahs Medical Center: Date/Time Focus Data, Action, ResponseDocument2 pagesCoahs Medical Center: Date/Time Focus Data, Action, ResponseLouwella RamosNo ratings yet
- Medical ManagementDocument2 pagesMedical ManagementLouwella RamosNo ratings yet
- Medical ManagementDocument2 pagesMedical ManagementLouwella RamosNo ratings yet
- LOUWELLA FAITH RAMOS - FIRST QUIZ MARCH 12 MCN QuestionnareDocument3 pagesLOUWELLA FAITH RAMOS - FIRST QUIZ MARCH 12 MCN QuestionnareLouwella RamosNo ratings yet
- Melo, Moinca T. Case Reading Vaginal Bleeding Causes Patient Dysfunctional Uterine BleedingDocument2 pagesMelo, Moinca T. Case Reading Vaginal Bleeding Causes Patient Dysfunctional Uterine BleedingMonica Melo HernandezNo ratings yet
- Theriogenology: S. Fierro, C. Vi Noles, J. Olivera-MuzanteDocument5 pagesTheriogenology: S. Fierro, C. Vi Noles, J. Olivera-MuzanteViviana CarrilloNo ratings yet
- Neonatal and Pediatric Patient Assessment (Study Guide)Document17 pagesNeonatal and Pediatric Patient Assessment (Study Guide)Fatima Sherrisa SaliNo ratings yet
- Small Group Discussion #4: A Case of A 22-Yr Old Nullipara Who Consulted For Left Lower Quadrant PainDocument36 pagesSmall Group Discussion #4: A Case of A 22-Yr Old Nullipara Who Consulted For Left Lower Quadrant PainRose Ann RaquizaNo ratings yet
- Introduction To Educational PyschologyDocument38 pagesIntroduction To Educational PyschologyCarabNo ratings yet
- Health Teaching During PergnancyDocument4 pagesHealth Teaching During PergnancyAnuradha MauryaNo ratings yet
- Lab Report 24 HormonesDocument3 pagesLab Report 24 HormonesLyka ElenaNo ratings yet
- Flink TeenagePregancyDocument1 pageFlink TeenagePregancyAnabel BaticanNo ratings yet
- Kea-Med Medical College 22 Campus: Title: Family Planning Project Work Surgical Contraceptive Individual AssignmentDocument13 pagesKea-Med Medical College 22 Campus: Title: Family Planning Project Work Surgical Contraceptive Individual AssignmentlahmetoNo ratings yet
- Science 5 DLP 1 - Human Reproductive SystemDocument12 pagesScience 5 DLP 1 - Human Reproductive SystemMark Cua89% (35)
- The Sympto-Thermal Method - Ten Years of Change PDFDocument18 pagesThe Sympto-Thermal Method - Ten Years of Change PDFFabian GuardaNo ratings yet
- Ectopic Pregnancy - PathophysiologyDocument1 pageEctopic Pregnancy - PathophysiologyMarimiel PagulayanNo ratings yet
- Science Paper Sec 2Document37 pagesScience Paper Sec 2JOSHI ARNAV ALANKAR Student2020No ratings yet
- Concept of Ovulation in AyurvedaDocument6 pagesConcept of Ovulation in Ayurvedasan MunNo ratings yet
- Clinical Notes 2 ETT-Ped Taping Pre-TermDocument3 pagesClinical Notes 2 ETT-Ped Taping Pre-TermchristinaNo ratings yet
- Fiqh Al Mustajiddaat (Modern Medicine)Document22 pagesFiqh Al Mustajiddaat (Modern Medicine)tisuchiNo ratings yet
- Topographic Anatomy of The Pelvis PDFDocument23 pagesTopographic Anatomy of The Pelvis PDFEl SpinnerNo ratings yet
- Epilepsy and Oral Hormonal Contraception-Indian Perspective: Review ArticleDocument6 pagesEpilepsy and Oral Hormonal Contraception-Indian Perspective: Review ArticleKirubakaranNo ratings yet
- Prime TechDocument32 pagesPrime Techmohd_ikrayemNo ratings yet
- Celulares y Efectos Motirces en El EmbarazoDocument12 pagesCelulares y Efectos Motirces en El EmbarazoNataly GantierNo ratings yet
- Assessment of Knowledge Attitude and Practice On Emergency Contraceptive Among Goba Female High School and Preparatory StudentsDocument9 pagesAssessment of Knowledge Attitude and Practice On Emergency Contraceptive Among Goba Female High School and Preparatory StudentsLawrence MungaNo ratings yet
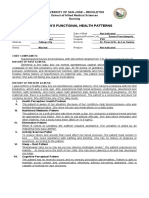
- Gordon'S Functional Health Patterns: University of San Jose - Recoletos School of Allied Medical Sciences NursingDocument2 pagesGordon'S Functional Health Patterns: University of San Jose - Recoletos School of Allied Medical Sciences NursingIvan A. EleginoNo ratings yet
- Case Study Presentation: Group 2Document12 pagesCase Study Presentation: Group 2Anna Marie Donaire0% (1)
- Surrogacy in IndiaDocument40 pagesSurrogacy in IndiaAnkita ThakurNo ratings yet
- Integrated Process - CaringDocument23 pagesIntegrated Process - CaringDonaJeanNo ratings yet
- Breast Cancer Case StudyDocument29 pagesBreast Cancer Case StudyAbdelmar Susulan100% (1)
- J Paediatrics Child Health - 2017 - Halliday - The Fascinating Story of SurfactantDocument6 pagesJ Paediatrics Child Health - 2017 - Halliday - The Fascinating Story of SurfactantTin TomašićNo ratings yet
- EBook - ICSE - 10 - MockPaper - 9 Subjects 2023 PDFDocument37 pagesEBook - ICSE - 10 - MockPaper - 9 Subjects 2023 PDFSiddhesh SrikantNo ratings yet
- The First Omen - ScribdDocument1 pageThe First Omen - ScribdazelikoNo ratings yet
- The Nursing Health History (NHH) : NCM 101-A: Health AssessmentDocument7 pagesThe Nursing Health History (NHH) : NCM 101-A: Health Assessmentthe someoneNo ratings yet