Professional Documents
Culture Documents
Rheumatology 1996 Huskisson 29 34
Uploaded by
Ardi PratamaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Rheumatology 1996 Huskisson 29 34
Uploaded by
Ardi PratamaCopyright:
Available Formats
British Journal of Rheumatology 1996;35(soppl.
l):29-34
A LONG-TERM STUDY TO EVALUATE THE SAFETY AND EFFICACY OF MELOXICAM THERAPY IN PATIENTS WITH RHEUMATOID ARTHRITIS
E. C HUSKISSON,* R. GHOZLAN.t R. KURTHENJ F. L. DEGNER and E. BLUHMKI^
*St Bartholomews Hospital, West Smithfield, London EC1A 7BE, f Service Rhumatologie, Polyclinique de La Roseraie, 93300 Aubervilliers, France, }Karlsgraben 15,52064 Aachen, Germany, Dr Karl Thomae GmbH and \Boehringer Ingelheim GmbH, Birkendorfer Strafie 65,88397 BiberachJRiss, Germany
SUMMARY Meloxicam is a new non-steroidal anti-inflammatory drug (NSAID), which has a higher activity against cyclooxygenase-2 (COX-2) than against cyclooxygenase-1 (COX-1), with potentially high anti-inflammatory and analgesic action. This study was designed to assess the long-term safety and efficacy of meloxicam 15 mg daily. Three hundred and fifty-seven patients (aged 19-84 yr, mean 56 yr) with rheumatoid arthritis (RA) received meloxicam 15 mg orally once dairy, for up to 18 months. Sixty-six per cent of patients remained on therapy for 18 months. Mean global efficacy, assessed by each patient on a visual analogue scale (0 cm = excellent, 10 cm = useless), was 3.32 3.1 cm at the last study visit (all patients included) and 2.33 2.25 cm afteT 18 months. Health status, general condition, morning stiffness, grip strength of right hand, Ritchie joint index, pain in the morning and pain at night all improved significantly. Efficacy was maintained throughout the study. Only 11.4% of patients discontinued prematurely due to lack of efficacy. Mean global tolerance was good. Twenty-eight per cent of patients experienced gastrointestinal (GI) adverse events, 21% musculoskeletal system disorders, 18% skin disorders and 15% respiratory disorders. Only 13.7% of patients discontinued due to adverse events. Severe GI effects, such as perforation, ulcer and bleeding, occurred in only three patients (0.8%). Withdrawals due to GI adverse events occurred in 3.9% of patients. Meloxicam 15 mg once daily was effective and compared favourably with standard NSATDs regarding tolerance when administered to patients with RA over an 18 month period.
KEY WORDS: Meloxicam, NSAID,
Downloaded from http://rheumatology.oxfordjournals.org/ by guest on May 11, 2012
Long-term, Rheumatoid arthritis.
CONTROLLED double-blind
clinical trials over periods of 3 weeks to 6 months have demonstrated that the efficacy of meloxicam 7.5 mg and 15 mg/day in the treatment of patients with rheumatoid arthritis (RA) is comparable to naproxen 750 mg/day [1] and piroxicam 20 mg/day [2]. Meloxicam is a new non-steroidal antiinflammatory drug (NSAID) that has been shown in preclinical studies to have a favourable activity against cyclooxygenase-2 (COX-2) [3]. The safety of meloxicam in these trials of up to 6 months compared favourably with that of the comparator drugs. Therefore this study was designed to assess the long-term safety and efficacy of meloxicam 15 mg daily used where necessary in conjunction with common second-line antirheumatic therapies. PATIENTS AND METHODS In this non-comparative trial, patients were recruited from 31 centres located in France, Germany, the UK, the Netherlands and Croatia. The study was reviewed or approved by the Ethics Committee of each institution taking part and was conducted in accordance with the provisions of the Declaration of Helsinki 1974 (version of Venice 1983) and GCP criteria. All patients gave informed consent to participate in the study. Male and female patients aged 18 yr or older were recruited. All patients suffered from RA as defined by the American College of Rheumatology criteria and required anti-inflammatory therapy.
Correspondence to: E. C Huskixson, 14A Miilford House, 7 Queen Anne's Street, London W1M 9FD.
Exclusion criteria Patients who had taken part in other clinical trials within the last month were excluded from the study, together with those with other rheumatological or non-rheumatological diseases, e.g. collagenosis, dermatomyositis, gout, infectional arthritis, sarcoidosis, psoriasis, ankylosing spondylitis or Still's disease. Patients with active peptic ulceration during the previous 6 months, severe cardiac, hepatic or renal disease, bronchial asthma or known hypersensitivity to analgesics, antipyretics and NSAIDs, were also excluded. If abnormal laboratory values were found at baseline which were not considered to be secondary to RA, but were thought to be clinically relevant by the investigator, the affected patients were not permitted to enter the study. Patients receiving anticoagulants or lithium were excluded. Finally, pregnant or breastfeeding women and women not using adequate contraception were excluded from the study. Treatment medication Meloxicam was supplied by Boehringer Ingelheim as 15 mg capsules, one capsule to be taken each day after breakfast Compliance was assessed by the dispensing record and the number of trial medication capsules taken. Non-compliant patients were withdrawn from the study. Second-line antirheumatic treatments were permitted providing the patient had been stabilized for at least 3 months before the start of the study. Any changes in dose were recorded. A protocol amendment was made during the study allowing changes of second-line treatment, to account for the fact that the severity of
O 19% British Society Tor Rheumatology
29
30
STUDIES ON MELOXICAM (MOBIC) data were handled by carrying forward the last available value for each parameter. Changes from baseline regarding continuous parameters of efficacy and safety and meloxicam plasma concentrations were evaluated by paired /-tests, whereas data on nominal or ordinal scales (number of withdrawals, Stanford health questionnaire, Ritchie joint index) were analysed descriptively. Incidence, time, severity and causal relationship of the adverse events were tabulated by the World Health Organization body system organ class and crude as well as hazard rates were estimated. The evaluation of laboratory values was done by score analysis referring to the normal ranges of the parameters [9]. Furthermore, the values were checked for clinically relevant changes. The sample size estimation was based on the CPMP guidelines for long-term treatment [10], which recommends that at least 200 patients be studied in an open design. A double-blind comparison was deemed to be inappropriate. The selected number of 300 patients was aimed to achieve sufficient long-term safety and efficacy data from 15 mg meloxicam given once daily. RESULTS The 31 centres recruited a total of 357 patients (94 males, 263 females). Their mean age was 56 yr (range 19-84 yr). All patients suffered from RA and required anti-inflammatory therapy. Characteristics of RA at baseline of all enrolled patients are listed in Table I. Fifteen patients were not treated due to abnormal baseline laboratory results (six patients), withdrawal of consent (one patient), concomitant disease regarded as an exclusion criteria (four patients), and withdrawal by the investigator (four patients). Efficacy Global efficacy at the final visit as assessed by the patient on a 10 cm horizontal VAS (mean S.D.) was 3.32 3.1 cm (n = 327). Patients who completed the study rated the global efficacy at the final assessment better (2.33 2.25 cm; n = 229) than patients who discontinued prematurely (5.65 3.43 cm; n = 98). Therapeutic efficacy improved throughout the duration of the trial in the patients who did not discontinue prematurely. The assessment changed from 4.37 2.50 cm on day 14 (n = 330) to 2.54 2.29 cm at month 18 (n = 232). The time course of efficacy reached a plateau ~6 months after start of therapy (Fig. 1). Discontinuation of the trial due to lack of efficacy occurred in 11.4% of the patients. Withdrawals occurred during the whole study period with most of these patients (7.3%) discontinuing within the first 3 months. Concomitant therapy with second-line treatment, intra-articular injections or therapy with corticosteroids, as well as being aged 65 yT or less, were associated with a significantly higher rate of discontinuation due to lack of efficacy (P < 0.05). The secondary variables, health status, general condition, pain in the morning, pain at night, morning stiffness and Ritchie joint index, improved significantly during treatment when comparing baseline values with
RA and the degree of joint destruction in the individual patient may vary considerably during the study period. Originally the use of low-dose oral corticosteroids was acceptable, at a maximum dose of prednisolone 7.5 mg equivalent daily, stabilized for at least 1 month. However, the protocol was amended during the study to allow doses >7.5 mg. The type and daily dose of glucocorticosteroids were chosen at the discretion of the investigator. The use of intra-articular injections of both short- and long-acting steroids was also acceptable. Physiotherapy could be continued during the study. Paracetamol (500 mg tablets) was supplied as rescue medication and a record was kept of its usage. If another rescue analgesic was taken, the same analgesic was used throughout the study and a record kept. Analgesics containing an NSAID were not allowed. Efficacy assessment Patients were assessed before enrolment to the study, on day 0 before the start of treatment, on day 14 and 1, 2, 3, 6, 9, 12, 15 and 18 months after the start of therapy. There were two primary endpoints for assessment of efficacy. At the last visit, global therapeutic efficacy was assessed by the patient on a 10 cm horizontal visual analogue scale (VAS: 0 cm = excellent; 10 cm = useless). The number and timing of withdrawals due to inadequate effect was also recorded. There were eight secondary endpoints for efficacy which were assessed at each visit. Difficulties in performing activities of daily life were assessed using a modified form of the Stanford health questionnaire [4, 5]. The assessment was rated on a four point scale (1 = without any difficulty, 4 = unable to do). General condition was assessed by the patient using a 10 cm VAS (0 cm = best ever, 10 cm = worst ever). Pain at night and in the morning were also assessed on a 10 cm VAS (0 cm = no pain; 10 cm = unbearable pain). Duration of morning stiffness and tenderness of the joints was assessed using the Ritchie joint index [6]. Grip strength of both hands was measured by means of a Martin Vigorimeter [7]. The acute phase reactants, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), were determined. Tolerability assessment Global tolerance was used as the primary endpoint for safety assessment, measured by the patient at the last visit (VAS: 0 cm = excellent; 10 cm = extremely bad). In addition, the occurrence of adverse events and of withdrawals due to poor tolerance were recorded at each visit. The investigator or clinical monitor assessed whether the adverse events were related to drug therapy using the method of Karch and Lasagna [8]. Laboratory assessments of clinical chemistry, haematology and urinalysis were performed together with measurement of meloxicam plasma concentrations. Statistics Data from all enrolled patients were included in an intention-to-treat analysis. Withdrawals and missing
Downloaded from http://rheumatology.oxfordjournals.org/ by guest on May 11, 2012
HUSKISSON ETAL: MELOXICAM IN RHEUMATOID ARTHRITIS
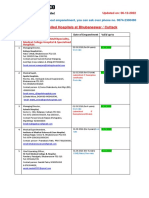
TABLE I Baseline characteristics of rheumatoid arthritis of all enrolled patients (n = 357) Variable Acute inflammatory state Previous treatment with NSAIDi Second-line treatment Organ involvement Physiotherapy (before and during the trial) Duration of morning stiffness of at least 1 h Soft tissue swelling 23 joints Swelling of different joints 26 wccics Symmetric joint swelling 26 weeks Rheumatoid nodules Rheumatoid factor positive Radiological evidence of erosions/osteopenia ESR of at least 30 mm/h Frequency (%) 50 (14.0) 299 (83.7) 229(64.1) 10(2.8) 105 (29.4) 285 (79.8) 338 (94.6) 339 (94.9) 315 (88 2) 108(30.2) 281 (78.7) 280 (78.4) 87 (24.3)
Day 14 1 3 6 9 Month of tratnwnl 12 1B
31
Fio. 1.Mean global efficacy of meloxicam 15 mg daily as assessed by patients on a 10 cm VAS (0 cm = excellent, 10 cm = useless). The numbers on each bar indicate the number of patients under treatment at each time point.
Downloaded from http://rheumatology.oxfordjournals.org/ by guest on May 11, 2012
values obtained at 6, 12 and 18 months, and at the last evaluation (i.e. at the last regular visit or early withdrawal) (Table II). Grip strength of the right hand demonstrated improvement after 6 and 12 months compared with baseline. Grip strength of the left hand improved significantly after 6 and 18 months and at the last evaluation, but not on examination after 12 months of treatment (Table II). ESR and CRP did not change throughout the study period except for the last ESR value, which was slightly higher than the baseline value.
Day 14 1
Safety All 357 patients were included in the safety analysis. Final global tolerance as assessed by the patient on the VAS (mean S.D.) was rated as 0.90 1.25 cm after completion of treatment (18 months) or 1.59 2.3 cm after completion or early withdrawal. Patients who completed treatment assessed tolerance better (0.90 1.25 cm) than those who discontinued treatment (3.20 3.15 cm). The longer the disease had been present the better the global tolerance was rated. Age, weight and sex had no influence on this parameter. Patients being treated with second-line drugs, intra-articular injections and corticosteroids rated global tolerance better than patients not taking these concomitant medications. Assessment of global tolerance improved during the course of the trial in the patients who did not discontinue the trial prematurely. The assessment changed from 1.86 2.19 on day 14 (n = 330) to 1.01 1.40 at month 18 (/ = 232) (Fig. 2). A total of 802 adverse events occurred in 249 (69.7%) patients during the whole treatment period. One hundred and sixty GI adverse events (19.9% of all adverse events) were reported in 99 (27.7%) patients. Three patients (0.8%) were diagnosed to have upper GI ulcers, and experienced nausea and vomiting. The other commonly reported adverse events included skin disorders (17.9% of patients), musculoskeletal system
3 6 8 Month of trsstmont
12
18
Fio. 2.Mean global tolerance of meloxicam 15 mg daily as assessed by patients on a 10 cm VAS (0 cm = excellent, 10 cm = extremely bad). The numbers on each bar indicate the number of patients under treatment at each time point.
disorders (21.0% of patients) and respiratory system disorders (15.4% of patients). Discontinuations due to adverse events occurred in 13.7% patients. Eighteen of these patients (5%) suffered GI disturbances and are described in Table III. The remainder suffered adverse events affecting: liver function (mild to moderate raised enzyme concentrations of the liver function tests; four patients), skin and appendages (five patients), the genitourinary system (three patients, comprising two patients with proteinuria and one patient with haematuria), the cardiovascular/pulmonary system (six patients) and the nervous system (seven patients). A further four patients discontinued following four adverse events not fitting into any of these categories (femur neck fracture, shivers and uneasy feeling, lethargy, and bleeding in the vitreous body with retinal detachment). Serious adverse events occurred in 42 (11.7%)
32
STUDIES ON MELOXICAM (MOBIQ
TABLEn Secondary endpoinu during the course of treatment Baseline
(meanlsjx)
6 months of therapy 12 months of therapy 18 months of therapy (meanlsji) (mean SJX) (mean S.D.) 1.62 0.45*** 2.8212.13*" 3.05 2J7*** 2.65 Z25*** 43 55"* 11 9*** 36 22* 35121" 26119 17122 1.65 0.51** 2.88 2.25*** 3.0612.33*" 2.5512.16*" 45 168"* 11 10*" 36 23* 3422 2823 18 25 1.6110.51"* 2.60 2.13*** 2.6512.14*" 2.36 2.07*** 39 6 1 " * 10 9*** 35124 34 23* 27120 17123
Last value (mean 1 sx>.) 1.6910.54* 3.31 1 2.57"* 3.29 1 Z60*" 193 1 2.53*** 55181** 131 11*** 34124 34124* 29122* 17124
Health status (mean score) General condition (cm) Pain in the morning (cm) Pain at night (cm) Morning stiffness (min) Ritchie index (sum score) Grip strengthrighthand (kPa) Grip strength left hand (kPa) ESR(mm/h) CRP(mg/l)
1.76 0.48 4.1612.30 4.78 2.55 3.71 1 2.58 70 67 1812 33 22 31+22 27 20 16 21
*P < 0.05; */> < 0.01; "/ < 0.001 for difference VJ baseline.
Downloaded from http://rheumatology.oxfordjournals.org/ by guest on May 11, 2012
patients. Seventeen of these serious adverse events were admissions to hospital due to RA for routine examinations or scheduled operations. One serious adverse event, colitis, was judged by the investigator to be probably related to treatment with meloxicam. The investigators considered three adverse events to be possibly related to treatment (ocular haemorrhage, diarrhoea and pyelonephritis). The relationship to the study medication for the remaining 21 serious adverse events was listed as conditional or doubtful by the investigator. Two patients died, one from pneumonia or cardiac failure 3 months after completion of the study. Neither death was considered to be related to meloxicam treatment. Descriptive statistical evaluation of laboratory data revealed no clinically relevant changes except for those already described as adverse events. Meloxicam plasma concentrations Plasma concentrations (mean S.D.) on day 14 were similar to those obtained after 12 and 18 months of treatment (1.34 0.91 ug/ml, n = 130; vs 1.34 0.87 ug/ml, n = 107 and 1.41 0.94 ug/ml, n = 85, respectively). Therefore, no accumulation is to be expected during long-term meloxicam therapy. Plasma levels (mean S.D.) were 26% higher in patients aged >65 yr than in those obtained in patients aged 65 yr or less (1.65 0.59 g/ml, n = 29; vs 1.31 0.70 g/ml, n = 108, respectively; P = 0.0185). No effect on weight adjusted plasma levels was observed with concomitant diuretic therapy (n = 137). DISCUSSION The efficacy of meloxicam at various doses in the short-term treatment of RA has already been demonstrated in a number of clinical trials [1,2, 11, 12]. In one study [12], patients were treated with meloxicam 7.5 mg or 15 mg daily for 3 weeks. The symptoms of RA improved on both doses, but there was a trend towards greater efficacy with the higher dose. The study described in this paper shows that the efficacy of
TABLEm Gastrointestinal adverse events resulting in discontinuation of study Duration of treatment at the time of withdrawal (days) 21 12 449 -35 293 393 42 24 5 32 78 335 206 168 16 230 22 32
Adverse event Nausea/vomiting/ diarrhoea Nausea/bloating/gastric pain Gastric pain Dizziness/nausea Duodenal ulcer Gastric ulcer Nausea/headache Epigastric pain Epigastric pain/ headache/fever Strong stomach pain Pneumoperitoneum/ sigmoiditis Severe diarrhoea Stomach upset Stomatitis and diarrhoea Colostomy atoms burning Dysphagi a/epigastric pain Nausea/vomiting/ epigastric pain Anaemia/borborygmus
Outcome Recovered Recovered Recovered Recovered Recovered Recovered Recovered Recovered Recovered Recovered Recovered Recovered Recovered Recovered Recovered Recovered Recovered Recovered
Causal relationship* Definite Definite Possible Probable Probable Possible Possible Definite Doubtful Probable Probable Conditional Doubtful Probable Possible Probable Probable Probable
* Assessed by investigator.
meloxicam 15 mg daily is maintained in the long-term management of the symptoms of RA. Over the 18 month treatment period there was a statistically significant improvement of signs and symptoms of RA when compared with baseline. Discontinuation due to lack of efficacy occurred in 11.4% of patients. This figure is comparable with data for indomethacin (8.5%), naproxen (13.0%) and diclofenac (11.3%) obtained after 2-3 yr of treatment in a prospective drug survival study [13].
HUSKISSON ETAL: MELOXICAM IN RHEUMATOID ARTHRITIS Patients who were concomitantly treated with other antirheumatic agents such as second-line drugs, intraarticular corticosteroids or oral corticosteroids were more likely to discontinue the study prematurely, possibly due to a more severe disease state. More than half of the patients discontinued within the first 3 months, suggesting that a majority of patients who are satisfied by their therapy by month 3 will continue. Compliance with meloxicam therapy was good, with a high number of patients remaining on therapy at the end of the trial. As expected, patients who completed the study rated efficacy better than those who withdrew before the end. The efficacy of meloxicam was maintained throughout the study period. GI tolerance of meloxicam at a dose of 7.5 mg daily has been reported to be superior to that of naproxen 750 mg daily [1], and at a dose of 15 mg daily to be superior to piroxicam 20 mg daily [2]. As described in Results, ~28% of all patients experienced GI adverse events, the most common being nausea, vomiting and gastric pain. This figure of 28% is expected for an open long-term treatment of 18 months. In the double-blind trials up to 6 months meloxicam 15 mg showed a rate of 18% for GI adverse events. This figure was significantly lower (P < 0.05) than the rate for piroxicam 20 mg, diclofenac 100 mg SR and naproxen 750-1000 mg [14]. Three patients (0.8%) experienced uncomplicated upper GI ulcers that resolved without problems. In one of these patients the diagnosis 'ulceration' was made solely on clinical grounds without performing an endoscopy or X-ray. No perforated or bleeding ulcers were reported. The incidence of severe GI adverse events (ulcer, bleeding, perforation), however, was less than that observed with other NSAIDs [15]. Data from double-blind clinical trials with meloxicam 15 mg showed significantly less perforations, ulcerations and bleeding than diclofenac 100 mg SR, piroxicam 20 mg and naproxen 750-1000 mg. The frequency of severe GI adverse events is dependent on the duration of treatment. For example, in the USA the rate of severe GI adverse events for all NSAIDs except nabumetone is 2-4% for a treatment duration of 1 yr. For nabumetone 1000 mg, which is comparable in efficacy to naproxen 500 mg, a rate of 0.5-0.8% was maintained for a treatment duration of 1-2 yr [16]. Therefore a rate of 0.8% for severe GI adverse events with meloxicam 15 mg over 18 months treatment duration compares favourably with other NSAIDs. During the 18 month study period 13.7% of patients discontinued due to adverse events. In a previous study evaluating diclofenac, indomethacin and naproxen in long-term treatment, 19, 41 and 14% of patients respectively were withdrawn within a year due to adverse events [13]; the most common side-effects leading to withdrawal were of GI origin. The apparently lower risk of serious and non-serious GI adverse events with meloxicam when compared with other NSAIDs may be due to its selective inhibition of COX-2 [3], which is induced by inflammatory mediators under pathological conditions, over COX-1, which is
33
responsible for physiological processes, e.g. protection of the stomach. NSAIDs may affect renal function, especially in patients whose renal function is already impaired [17]. However, meloxicam was well tolerated, except in two patients who reported proteinuria. This was judged to be caused by concomitant gold therapy or chronic pyelonephritis respectively, so no clear causal relationship to meloxicam could be established. In this study the plasma levels of meloxicam were increased by 26% in patients aged >65 yr when compared with younger patients. The magnitude of this effect is not of clinical relevance, as described earlier in more detail [18]. The skin reactions observed in this study may have been caused by meloxicam since skin reactions have been reported with other NSAIDs. NSAIDs are also known to influence liver enzyme laboratory parameters. Four patients had mild to moderate elevations of liver enzyme values. In three of these, however, this adverse event could not be clearly related to meloxicam administration as the patients were taking other potentially liver damaging drugs at the same time (gold, paracetamol, alcohol) or had elevated enzymes recorded at baseline. CONCLUSION In conclusion, the results of this study are consistent with previous experience with meloxicam and confirm that meloxicam 15 mg, administered once daily over a period of up to 18 months, is effective and well tolerated in the treatment of the symptoms of RA. The rate of gastrointestinal adverse events, such as dyspepsia, abdominal pain and perforations, ulcerations and bleedings, compare favourably with standard NSAIDs; this may be explained by the COX-2 selectivity of meloxicam.
ACKNOWLEDGEMENTS
Downloaded from http://rheumatology.oxfordjournals.org/ by guest on May 11, 2012
We would like to thank the following investigators who participated in this study. Germany: Dr E. Ettrich, Gerlingen (three patients); Dr J. Bartl, Miinchen (four patients); Dr J. A. M. Baltus, Vreden (four patients); Dr R D. Krippner, Frankfurt (10 patients); Mr H. Bouzo, Augsburg (36 patients); Dr C. Lembens, Mainz (six patients); Dr U. Droste, Bad Kreuznach (seven patients); Dr R. Sprekeler, Rotenburg-Wumme (one patient); Dr L. Kriegel, Nurnberg (13 patients); Dr G. Kratzsch and Dr Knaupp, Ulm (three patients); Dr U. Oberschelp and Dr E. Hartmut, Hamm (18 patients); Dr G. Bowing, Dixsseldorf (five patients); Dr R. Kurthen, Aachen (12 patients); Dr H. Geidel, Dr R Hrdlicka and Dr L. Unger, Dresden (seven patients); Mr M. Keysser, Rostock (nine patients); Dr R. Schmidt, Falkenstein (21 patients); Dr H. Lang, Plauen (12 patients); Dr H. Kamps and Dr M. Mrochen, Uelzen (four patients); UK: Dr B. L. Hazleman, Addenbrooke's Hospital, Cambridge (19 patients); Dr Beardwell, Barking Hospital, Barking (12 patients); Dr D. N. L. Cox, Royal Hampshire County Hospital, Winchester (24 patients); Dr J. S. Coppock, Coventry and Warwickshire Hospital, Coventry (six patients); Dr
34
STUDIES ON MELOXICAM (MOBIQ ness in patients with rheumatoid arthritis. Q J Med 1968^7:393-406. 7. Jones E, Hanly JG, Mooney R et aL Strength and function in the normal and rheumatoid hand. J Rheumatol 1991;l&1313-8. 8. Karch FE, Lasagna L. Toward the operational identification of adverse drug reactions Clin Pharmacol Ther 1977/21:247-54. 9. Chuang-Stein C. Summarizing laboratory data with different reference ranges in multicentre clinical trials. Drug InfJ 1992;26:77-84. 10. CPMP guidelines on clinical testing requirements for drugs for long-term use. HI/602/81-EN. 11. Lemmel EM, Bolten W, Burgos-Vargas Retal. A doubleblind placebo controlled study of 7.5 mg and 15 mg of meloxicam in patients with rheumatoid arthritis (RA). Scand J Rheumatol 1994;Suppl 98:abstract no. 111. 12. Reginster JY, Distel M, Bluhmki E. A double-blind study to compare the efficacy and safety of meloxicam 7.5 mg and meloxicam 15 mg in patients with rheumatoid arthritis. BrJRheumatol 1996;35(suppl. 1):17-21. 13. Wijnands M, van Riel P, van't Hof M et al. Longterm treatment with nonsteroidal antiinflammatory drugs in rheumatoid arthritis: a prospective drug survival study. J Rheumatol 1991;18:184-7. 14. Distel M, Bluhmki E. Global analysis of safety of meloxicam, a new enolic acid derived non-steroidal antiinflammatory agent. Rheumatol Eur 1995;3:abstract no. E259. 15. Griffin MR, Piper JM, Daugherty JR, Snowden M, Ray WA et aL Nonsteroidal anti-inflammatory drug use and increased risk for peptic ulcer disease in elderly persons. Ann Intern Med 1991;114:257-63. 16. Physicians Desk Reference 1995. Medical Economics Company Inc., Montvale, NJ. 17. Kenny GNC Potential renal, haematological and allergic adverse effects associated with nonsteroidal anti-inflammatory drugs. Drugs 1992;44:31-7. 18. Sander O, Hubner G, Tiirck D et aL Differences in meloxicam pharmacokinetics in patients with chronic polyarthritis depending on sex and age. Z Rheumatol 1994;53:68 abstract no. P.I 13.
R. M. Bernstein, Rheumatism Research Centre, The Royal Infirmary, Manchester (22 patients); Dr J. Belch, Ninewells Hospital and Medical School, Dundee (15 patients); Dr P. G. Davies, Broomfield Hospital, Essex (five patients); Dr J. A. Wojtulewski, Eastbourne District General Hospital, Eastbourne (seven patients); France: Prof. Treves, Limoges (nine patients); Prof. R. Ghozlan, Polyclinique de la Roseraie Rhumatologie, Aubervilliers (four patients); Dr Chariot, Creteil (11 patients); The Netherlands: Dr B. A. Masek, St Maartens Gasthuis Afdeling Reumatologie, Venlo (24 patients); Croatia: Prof. Z. Domljan, Institut Fur Rheumatologie Rebro, Zagreb (24 patients).
REFERENCES
1. Wojtulewski JA, Schattenkircher M, Barccl6 P et aL A six month double-blind trial to compare the efficacy and safety of meloxicam 7.5 mg daily and naproxen 750 mg daily in patients with rheumatoid arthritis. Br J Rheumatol 1996;35(suppl. l):22-28. 2. Huslrisson EC, Narjes H, Bluhmki E. Efficacy and tolerance of meloxicam, a new NSAID, in daily oral doses of 15, 30 and 60 mg in comparison with 20 mg piroxicam in patients with rheumatoid arthritis. Scand J Rheumatol 1994;Suppl 98:abstract no. 115. 3. Engelhardt G. Meloxicam: a potent inhibitor of COX-2. Data presented at the 9th International Conference on Prostaglandins and Related Compounds, Florence, Italy, June 6-10, 1994, p. 82. 4. Pincus TH, Callahan LF, Brooks RH et aL Self-report questionnaire scores in rheumatoid arthritis compared with traditional physical, radiographic and laboratory measures. Ann Intern Med 1989;110:259-66. 5. Lorish CD, Abraham N, Austin J et aL Disease and psychosocial factors related to physical functioning in rheumatoid arthritis. J Rheumatol 1991 ;18:1150-7. 6. Ritchie DM, Boyle JA, Mclnners IM et aL Clinical studies with an articular index for the assessment of joint tender-
Downloaded from http://rheumatology.oxfordjournals.org/ by guest on May 11, 2012
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Turner Syndrome Appraisal-Problem 1Document7 pagesTurner Syndrome Appraisal-Problem 1Ardi PratamaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Literature ReviewDocument31 pagesLiterature ReviewArdi PratamaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Wright 2008Document17 pagesWright 2008Ardi PratamaNo ratings yet
- Bimbel MGDocument78 pagesBimbel MGArdi PratamaNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- 048 VCH Xi GM Amrs 2015Document1 page048 VCH Xi GM Amrs 2015Ardi PratamaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Vitamin D de Ficiency in Critically Ill Children: AuthorsDocument8 pagesVitamin D de Ficiency in Critically Ill Children: AuthorsArdi PratamaNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Tipe-Tipe DiareDocument10 pagesTipe-Tipe DiareArdi PratamaNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Gatot Sugiharto, MD, Internist Faculty of Medicine, UWKS Lecture - 2010Document62 pagesGatot Sugiharto, MD, Internist Faculty of Medicine, UWKS Lecture - 2010Ardi PratamaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Ear Medication: Ear DropsDocument2 pagesEar Medication: Ear DropsArdi PratamaNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Cognitive Behavior Therapy (CBT) For Panic Disorder: Relationship of Anxiety and Depression Comorbidity With Treatment OutcomeDocument2 pagesCognitive Behavior Therapy (CBT) For Panic Disorder: Relationship of Anxiety and Depression Comorbidity With Treatment OutcomeArdi PratamaNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Referat Selulitis: No. Nama NPMDocument2 pagesReferat Selulitis: No. Nama NPMArdi PratamaNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Figure 1.4 Suggested Dengue Case Classification and Levels of SeverityDocument2 pagesFigure 1.4 Suggested Dengue Case Classification and Levels of SeverityArdi PratamaNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- OzaenaDocument4 pagesOzaenaArdi PratamaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- 03-F10 Planned Job ObservationDocument1 page03-F10 Planned Job ObservationSn Ahsan100% (1)
- Micro - Systemic Bacteriology Questions PDFDocument79 pagesMicro - Systemic Bacteriology Questions PDFShashipriya AgressNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 16 Personalities ResultsDocument9 pages16 Personalities Resultsapi-605848036No ratings yet
- Rin Case StudyDocument4 pagesRin Case StudyReha Nayyar100% (1)
- BKNC3 - Activity 1 - Review ExamDocument3 pagesBKNC3 - Activity 1 - Review ExamDhel Cahilig0% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- FDD Spindle Motor Driver: BA6477FSDocument12 pagesFDD Spindle Motor Driver: BA6477FSismyorulmazNo ratings yet
- Heart Rate Variability Threshold As An Alternative.25Document6 pagesHeart Rate Variability Threshold As An Alternative.25Wasly SilvaNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Chunking Chunking Chunking: Stator Service IssuesDocument1 pageChunking Chunking Chunking: Stator Service IssuesGina Vanessa Quintero CruzNo ratings yet
- Heirs of Vinluan Estate in Pangasinan Charged With Tax Evasion For Unsettled Inheritance Tax CaseDocument2 pagesHeirs of Vinluan Estate in Pangasinan Charged With Tax Evasion For Unsettled Inheritance Tax CaseAlvin Dela CruzNo ratings yet
- English 2nd Quarter Week 7 Connotation DenotationDocument28 pagesEnglish 2nd Quarter Week 7 Connotation DenotationEdward Estrella GuceNo ratings yet
- Personal Narrative RevisedDocument3 pagesPersonal Narrative Revisedapi-549224109No ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- June 2014 (v3) QP - Paper 3 CIE Physics IGCSEDocument20 pagesJune 2014 (v3) QP - Paper 3 CIE Physics IGCSECole KhantNo ratings yet
- Autodesk Nastran In-CAD PDFDocument43 pagesAutodesk Nastran In-CAD PDFFernando0% (1)
- Topic 1 - ICT Tools at USP - Theoretical Notes With Google AppsDocument18 pagesTopic 1 - ICT Tools at USP - Theoretical Notes With Google AppsAvantika PrasadNo ratings yet
- ANS145 - Beef Cattle ProductionDocument52 pagesANS145 - Beef Cattle ProductionEgie BulawinNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- National Employment Policy, 2008Document58 pagesNational Employment Policy, 2008Jeremia Mtobesya0% (1)
- Reference by John BatchelorDocument1 pageReference by John Batchelorapi-276994844No ratings yet
- Operational Readiness and Airport TransferDocument2 pagesOperational Readiness and Airport TransferochweriNo ratings yet
- ProbDocument10 pagesProbKashif JawaidNo ratings yet
- Thermodynamic c106Document120 pagesThermodynamic c106Драгослав БјелицаNo ratings yet
- Fluoride - Wide Range of Serious Health Problems"Document29 pagesFluoride - Wide Range of Serious Health Problems"zataullah100% (2)
- Afzal ResumeDocument4 pagesAfzal ResumeASHIQ HUSSAINNo ratings yet
- Model Answer Winter 2015Document38 pagesModel Answer Winter 2015Vivek MalwadeNo ratings yet
- MOS - Steel StructureDocument15 pagesMOS - Steel StructuredennisNo ratings yet
- Empanelled Hospitals List Updated - 06-12-2022 - 1670482933145Document19 pagesEmpanelled Hospitals List Updated - 06-12-2022 - 1670482933145mechmaster4uNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Assignment RoadDocument14 pagesAssignment RoadEsya ImanNo ratings yet
- APA Citation Method For ERLACS: Reference Citations in TextDocument8 pagesAPA Citation Method For ERLACS: Reference Citations in Textdanny_alfaro_8No ratings yet
- Level Swiches Data SheetDocument4 pagesLevel Swiches Data SheetROGELIO QUIJANONo ratings yet
- Cocaine in Blood of Coca ChewersDocument10 pagesCocaine in Blood of Coca ChewersKarl-GeorgNo ratings yet
- Chapter 24 - The Solar SystemDocument36 pagesChapter 24 - The Solar SystemHeather Blackwell100% (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)