Professional Documents
Culture Documents
OHT Study - Factors Predicting Onset of POAG
Uploaded by
mmpipi21Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
OHT Study - Factors Predicting Onset of POAG
Uploaded by
mmpipi21Copyright:
Available Formats
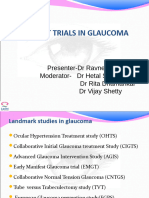
OHT Study Factors Predicting Onset of POAG -OHTS designed to evaluate safety and efficacy of topical meds in delaying/preventing
POAG -1636 pts w OHT and IOP 24-32 w/no evidence of glc damage; randomized to tx or observation -goal of tx was to achieve IOP <24 and 20% reduction from baseline IOP (IOP <18 not required) -60% reduced risk of POAG w topical meds -at 60 months risk of POAG was ~4.4% in txd group vs 9.5% in untxd group -CCT measurements obtained at F/U visitis, not during randomization; inverse relationship between CCT and development of POAG; 3 fold risk incr if CCT <555um -key risk factors: age, large vertical CD ratio, incr IOP, incr PSD on at least 2 VFs, thin CCT (<555um) -Hx of DM seemed to be a protective factor from onset of POAG (6/191 developed POAG)
Early Manifest Glaucoma Trial (1992-2001) -compared the effect of immediate IOP lowering vs not treating on progression of newly detected OAG -255 pt (129 tx/126 controls) aged 50-80 (median 68) w/early glc, repeatable VF defects w/ONL on GHT, and median IOP of 20 -txd group received 360 trabeculoplasty plus betxolol drops bid -pts remained in untxd unless progression occurred F/u every 3 months, with stereo photos every 6 months -Tx reduced IOP by ~5mmHg (~25%); progression less frequent and occurred much later than untxd group -mean IOP reduced in tx group from 20.6 to 15.5 (25%) -larger progression in control group; mean time to progression=48 months for control; 66 months for txd group -Each mmHg decrease correlates to ~10% lower risk of progression -nuclear lens opacitites incr in txd group -study showed that reducing IOP can slow progression of glaucoma; also showed value of repeated reliable visual fields -no rigid target IOP was set in the EMGT -considerations: almost all participants were white with very early glaucoma and IOP <30
You might also like
- The Penis Enlargement BibleDocument12 pagesThe Penis Enlargement BibleDPEYIZA72% (18)
- Penis Enlargement Exercises-The Natural Penis Elargment Guide-EducationalDocument30 pagesPenis Enlargement Exercises-The Natural Penis Elargment Guide-Educationalmesagerdivin17No ratings yet
- Knockout Craps StrategyDocument158 pagesKnockout Craps Strategymmpipi21100% (2)
- Texas Commercial Real Estate Purchase Agreement: I. THE PARTIES. This CommercialDocument14 pagesTexas Commercial Real Estate Purchase Agreement: I. THE PARTIES. This Commercialmmpipi21No ratings yet
- TMOD StudyGuideDocument302 pagesTMOD StudyGuidemmpipi2175% (4)
- Forget Book Sales : Here's How You REALLY Make Money Self-PublishingDocument16 pagesForget Book Sales : Here's How You REALLY Make Money Self-Publishingmmpipi21No ratings yet
- Texas Real Estate Purchase Agreement TemplateDocument10 pagesTexas Real Estate Purchase Agreement Templatemmpipi21No ratings yet
- Texas Real Estate Purchase Agreement TemplateDocument10 pagesTexas Real Estate Purchase Agreement Templatemmpipi21No ratings yet
- Complementary and Alternative Medical Lab Testing Part 8: UrologyFrom EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyRating: 3 out of 5 stars3/5 (1)
- Cushing's DiseaseDocument56 pagesCushing's DiseaseDrasmNo ratings yet
- Imp Landmark Glauc StudiesDocument100 pagesImp Landmark Glauc StudiesASHOK KUMAR SINGHNo ratings yet
- The Effect of Prostaglandin Analogs On The Biomechanical Properties and Central Thickness of The Cornea of Patients With OpenDocument4 pagesThe Effect of Prostaglandin Analogs On The Biomechanical Properties and Central Thickness of The Cornea of Patients With OpenHawania IINo ratings yet
- Papers: Treatment of Ocular Hypertension and Open Angle Glaucoma: Meta-Analysis of Randomised Controlled TrialsDocument3 pagesPapers: Treatment of Ocular Hypertension and Open Angle Glaucoma: Meta-Analysis of Randomised Controlled TrialsDanil Anugrah JayaNo ratings yet
- Latanoprostene Bunod 0.024% Versus Timolol Maleate 0.5% in Subjects With Open-Angle Glaucoma or Ocular Hypertension The APOLLO StudyDocument11 pagesLatanoprostene Bunod 0.024% Versus Timolol Maleate 0.5% in Subjects With Open-Angle Glaucoma or Ocular Hypertension The APOLLO StudybungagladysNo ratings yet
- The Effect of Prostaglandin Analogues On Central Corneal Thickness in Patients With GlaucomaDocument4 pagesThe Effect of Prostaglandin Analogues On Central Corneal Thickness in Patients With GlaucomarandyhermawanNo ratings yet
- Impetigo Due To Staphylococcus Aureus (Methicillin - Susceptible Isolates Only) or Streptococcus PyogenesDocument18 pagesImpetigo Due To Staphylococcus Aureus (Methicillin - Susceptible Isolates Only) or Streptococcus PyogenesjoelrequenaNo ratings yet
- Evolve Study Journal Club PresentationDocument62 pagesEvolve Study Journal Club PresentationsantoshvelloreNo ratings yet
- Palmberg 2004Document14 pagesPalmberg 2004nishtha singhNo ratings yet
- Clinical Executive Summary: Treatment of Bipolar I DisorderDocument9 pagesClinical Executive Summary: Treatment of Bipolar I DisorderjoelrequenaNo ratings yet
- Chap 4 Summary - Steroid Resistant Nephrotic Syndrome - Final - V2Document3 pagesChap 4 Summary - Steroid Resistant Nephrotic Syndrome - Final - V2betaNo ratings yet
- Poems Enero 2021Document22 pagesPoems Enero 2021Gabriela Santin GuzmanNo ratings yet
- Long-Term Effectiveness and Tolerability of Topiramate in Children With Epilepsy Under The Age of 2 Years: 4-Year Follow-UpDocument7 pagesLong-Term Effectiveness and Tolerability of Topiramate in Children With Epilepsy Under The Age of 2 Years: 4-Year Follow-Uppkarina_3No ratings yet
- Lerner SFDocument9 pagesLerner SFAdriana FallaNo ratings yet
- Jurnal Mata 3Document4 pagesJurnal Mata 3Ami AntariksawatiNo ratings yet
- The Glymphatic System and New Etiopathogenic Hypotheses Concerning Glaucoma Based On Pilot Study On Glaucoma Patients Who Underwent Osteopathic Manipulative Treatment (OMT)Document7 pagesThe Glymphatic System and New Etiopathogenic Hypotheses Concerning Glaucoma Based On Pilot Study On Glaucoma Patients Who Underwent Osteopathic Manipulative Treatment (OMT)BOHR International Journal of Current Research in Optometry and Ophthalmology (BIJCROO)No ratings yet
- Review and Evaluation of Clinical Data: 2.1 BackgroundDocument21 pagesReview and Evaluation of Clinical Data: 2.1 BackgroundjoelrequenaNo ratings yet
- 260-Main Manuscript-1507-1-10-20220620Document5 pages260-Main Manuscript-1507-1-10-20220620hilman lesmanaNo ratings yet
- Blood Pressure and Cholesterol Lowering in Persons Without Cardiovascular DiseaseDocument46 pagesBlood Pressure and Cholesterol Lowering in Persons Without Cardiovascular DiseaseJirran CabatinganNo ratings yet
- Biophysical Properties in Glaucoma: Diagnostic TechnologiesFrom EverandBiophysical Properties in Glaucoma: Diagnostic TechnologiesIngrida JanulevicieneNo ratings yet
- PrintDocument8 pagesPrintannarchyNo ratings yet
- EBM ReviewDocument6 pagesEBM ReviewdavidperdanaNo ratings yet
- Perhitungan RRDocument5 pagesPerhitungan RRMuh Witly FairussaflyNo ratings yet
- Risk Factors For Steroid Response Among Cataract PatientsDocument7 pagesRisk Factors For Steroid Response Among Cataract PatientsRodrigoBarreraNo ratings yet
- The Use of Procalcitonin As A Marker of Sepsis in Children: Abst TDocument3 pagesThe Use of Procalcitonin As A Marker of Sepsis in Children: Abst TAsri RachmawatiNo ratings yet
- Pegasus TIMI 54 TrialDocument13 pagesPegasus TIMI 54 TrialIsaac Aaron Enriquez MonsalvoNo ratings yet
- 10 1007@BF02549523Document11 pages10 1007@BF02549523rachel0301No ratings yet
- Journal 4 - Management of Traumatic Brain Injury A Narrative Review of Current EvidenceDocument11 pagesJournal 4 - Management of Traumatic Brain Injury A Narrative Review of Current EvidenceNatalindah Jokiem Woecandra T. D.No ratings yet
- Kring JournalDocument3 pagesKring JournalcbanguisNo ratings yet
- FluidDocument190 pagesFluidAndrias OzNo ratings yet
- Evidence-Based Medicine Studi KasusDocument27 pagesEvidence-Based Medicine Studi KasusIntan Dewi SaputriNo ratings yet
- TPL2 Makes Sure RASinduced Inflammatory Signaling Which Is Initialized Simply by Level VariationsrzbyqDocument1 pageTPL2 Makes Sure RASinduced Inflammatory Signaling Which Is Initialized Simply by Level Variationsrzbyqcupwitch78No ratings yet
- Cardiogenic Shock: Nick Tehrani, MD Saharman Leman Int - CardilogistDocument54 pagesCardiogenic Shock: Nick Tehrani, MD Saharman Leman Int - CardilogistSigit_RokhmadiNo ratings yet
- Role of Flicker Perimetry in Predicting Onset of Late-Stage Age-Related Macular DegenerationDocument10 pagesRole of Flicker Perimetry in Predicting Onset of Late-Stage Age-Related Macular DegenerationHarold Estiven MarinNo ratings yet
- Abstracts - How To Critically Appraise From An AbstractDocument3 pagesAbstracts - How To Critically Appraise From An AbstractآكوجويNo ratings yet
- Long-Term Surveillance For Adverse Effects of Antihypertensive DrugsDocument10 pagesLong-Term Surveillance For Adverse Effects of Antihypertensive Drugsahmad kholiqNo ratings yet
- 2098JCEN - Jcen 15 214Document7 pages2098JCEN - Jcen 15 214SriUtari MasyitahNo ratings yet
- Otolaryngology Head and Neck Surgery 2011 Abadie P176Document2 pagesOtolaryngology Head and Neck Surgery 2011 Abadie P176Gus JanantaraNo ratings yet
- Hypertension Landmark Trials 2015: A European Perspective of The Practicing ClinicianDocument3 pagesHypertension Landmark Trials 2015: A European Perspective of The Practicing ClinicianFiqih VidiantoroNo ratings yet
- tmp1617 TMPDocument7 pagestmp1617 TMPFrontiersNo ratings yet
- Lutfi-Full Paper-Pit 2024Document6 pagesLutfi-Full Paper-Pit 2024Lutfi MaulanaNo ratings yet
- Clinical Study: Detection of Glaucoma in A Cohort of Chinese Subjects With Systemic HypertensionDocument6 pagesClinical Study: Detection of Glaucoma in A Cohort of Chinese Subjects With Systemic HypertensionFebi RahmadinNo ratings yet
- IL 6 Dan QolDocument4 pagesIL 6 Dan Qolbryan ruditaNo ratings yet
- Artig For OrtortisticDocument7 pagesArtig For OrtortisticVitor LopesNo ratings yet
- Atorvastatina y HuesosDocument6 pagesAtorvastatina y HuesosdrasabrinavNo ratings yet
- Latagliata Et Al-2015-American Journal of HematologyDocument4 pagesLatagliata Et Al-2015-American Journal of HematologyRina HarliantiNo ratings yet
- Normal Tension GlaucomaDocument6 pagesNormal Tension GlaucomaAlya Batami PrimasariNo ratings yet
- TOR SEMNAS KARAkTER 4 2018Document6 pagesTOR SEMNAS KARAkTER 4 2018Rosyid PrasetyoNo ratings yet
- Akromegali 4Document7 pagesAkromegali 42018.02.029 Nabila Nareswari AzariaNo ratings yet
- Kol Ditz 2016Document3 pagesKol Ditz 2016Lanna HarumiyaNo ratings yet
- Emergent Management of Acute Ischemic Stroke PDF VersionDocument73 pagesEmergent Management of Acute Ischemic Stroke PDF VersionElizar JarNo ratings yet
- 1 s2.0 S000649712061936X MainDocument11 pages1 s2.0 S000649712061936X Mainalhattab tempNo ratings yet
- 319 FullDocument3 pages319 FullNegreanu AncaNo ratings yet
- Assessment of Patient's Knowledge, Attitude and Practice Regarding HypertensionDocument6 pagesAssessment of Patient's Knowledge, Attitude and Practice Regarding HypertensionScintya NasutionNo ratings yet
- Kontras StatinDocument10 pagesKontras Statinale_rhdNo ratings yet
- 4-Key Findings From CaprieDocument30 pages4-Key Findings From CaprieMuhammad Yolandi SumadioNo ratings yet
- Prevalence and Risk Factors of Thyroid-Associated Ophthalmopathy Among IndiansDocument4 pagesPrevalence and Risk Factors of Thyroid-Associated Ophthalmopathy Among IndiansLastry WardaniNo ratings yet
- What Happens in A 5-Year Follow-Up of Benign Thyroid NodulesDocument4 pagesWhat Happens in A 5-Year Follow-Up of Benign Thyroid NodulesT.A.BNo ratings yet
- Prevalence of Depression and Anxiety Among ParticiDocument10 pagesPrevalence of Depression and Anxiety Among ParticiAishah FarihaNo ratings yet
- 2018-2019 Calendar 2018-2019 Calendar 2018-2019 Calendar 2018-2019 Calendar 2018-2019 CalendarDocument1 page2018-2019 Calendar 2018-2019 Calendar 2018-2019 Calendar 2018-2019 Calendar 2018-2019 Calendarmmpipi21No ratings yet
- Early Voting Calendar Oct 13 - 202009201254208536Document2 pagesEarly Voting Calendar Oct 13 - 202009201254208536mmpipi21No ratings yet
- Pending Cataract Surgery: Name DOB AGE Payment EYE NeedsDocument2 pagesPending Cataract Surgery: Name DOB AGE Payment EYE Needsmmpipi21No ratings yet
- COVID-19 (Fillable) - Employer Verification FormDocument1 pageCOVID-19 (Fillable) - Employer Verification Formmmpipi21No ratings yet
- Shoppers Guide To LTCi - 2019Document76 pagesShoppers Guide To LTCi - 2019mmpipi21No ratings yet
- The Guide To Riding The B-Line Accessible Formats Available: Americans With Disabilities Act (ADA) GuidelinesDocument7 pagesThe Guide To Riding The B-Line Accessible Formats Available: Americans With Disabilities Act (ADA) Guidelinesmmpipi21No ratings yet
- Common Optometric CodesDocument1 pageCommon Optometric Codesmmpipi21No ratings yet
- A Fridge That Takes Only 0.1 KWH A Day?Document6 pagesA Fridge That Takes Only 0.1 KWH A Day?mmpipi21No ratings yet
- Optics ReviewDocument11 pagesOptics Reviewmmpipi21No ratings yet
- DiabetesDocument2 pagesDiabetesmmpipi21No ratings yet
- Bush Chicken CouponsDocument1 pageBush Chicken Couponsmmpipi21No ratings yet
- VisualAid PictureExcerptDocument24 pagesVisualAid PictureExcerptmmpipi21No ratings yet
- P90 XSchedDocument1 pageP90 XSchedmmpipi21No ratings yet