Professional Documents
Culture Documents
Cheatsheet 3
Cheatsheet 3
Uploaded by
Klins Tristan OliverOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cheatsheet 3
Cheatsheet 3
Uploaded by
Klins Tristan OliverCopyright:
Available Formats
Guidelines for setting up a Neonatal Ventilator: 1. Pt range: Neonate (Maximum VT = 40cc) 2.
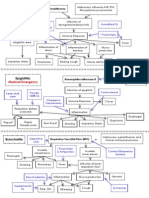
Mode: Pressure Control (works best for un-cuffed ETT) 3. VT: a. <33 weeks gestation 4 6 cc/kg b. >33 weeks gestation or chronic 5 7 cc/kg 4. PIP: a. Maximum PIP settings: - <27 weeks gestation 24 CWP - 27 32 weeks gestation 26 CWP - 33 40 weeks gestation 28 CWP b. Start low (best to err on low side to prevent barotraumas.) c. Increase to obtain target VT and adequate chest rise d. Frequently monitor & adjust PIP to accommodate changes in lung compliance altering tidal volume. 5. PEEP: a. Start at minimum 4 5 CWP b. Increase to 6 7 CWP if FiO2 needs > 60% c. Adjust to maintain acceptable PaO2 and SpO2 d. 8 10 CWP PEEP if directed by physician e. Remember that PC setting is above PEEP 6. FiO2: a. Start low at 40% b. Adjust to maintain target SpO2 c. If SaO2 < target range, FiO2 may be increased by 25, & then allowing 4 minutes for stabilization after each change. (consider adjustment of PIP and PEEP also.) d. Continue assuring AW patent, HR>100 & baby not apneic. e. If SaO2 > target range, FiO2 may be decreased by 2 5, allowing 4 minutes for stabilization after each change. f. Consider increasing PEEP prior to FiO2 g. Maintain neonate on ROOM AIR whenever possible. 7. Rate: a. 50 60 if < 34 weeks gestation or < 3 kg b. 40 50 if >34 weeks gestation or > 3 kg c. 30 40 if 40 weeks gestation; slightly higher if indicated. d. Watch for air trapping at rates > 40 (adjust I-time). 8. I-time: a. Start at 0.3 plus or minus 0.5 (post-term may need more.) b. Neonatal initial I-time setting - <1kg 0.25 0.30 sec minimum 0.20 seconds - 1-2kg 0.30 0.40 sec minimum 0.20 seconds - 2-3kg 0.35 0.45 sec minimum 0.25 seconds - 3-4kg 0.40 0.60 sec minimum 0.30 seconds c. Ideally set using Flow-time graphics d. This alters I-time and I:E ratio e. Increase & decrease to reach target settings as appropriate f. Watch for air trapping at rates >40 in neonates >3kg; they may need I-time >0.40 to complete inspiration & prevent air trapping. g. If neonate using expiratory muscles, try decreasing I-time slightly (increasing flow). h. If I-time gets too short, consider switch to PRVC. 9. I-Rise time: a. 10 if < 33 weeks gestational age b. >5 if >33 weeks gestational age c. Basically, the smaller the ETT the higher this should be to create laminar flow and a pseudo sign wave. d. Increase for bronchospasm (slow rise time, longer e-time) 10. PIP limit: 2 3 > PIP (all other alarms as appropriate.)
Indications to intubating neo 1. PaO2 < 45mmHg while breathing 80 100% FiO2 2. PaCO2 > 65mmHg 3. Intractable metabolic acidosis(B.E. < -10 meq.) 4. Marked retractions on CPAP 5. Frequent episodes of apnea and bradycardia on CPAP.
Normal Neo ABGs & Vitals: 1. Target ABG: PH 7.25 7.40 PCO2 = 45 59 PaO2 = 50 70 BE = 0 -4 2. SpO2: 8292% if <27 wks 8593% if <33 wk 88 95% if >33 wks 2. RR: Term = 3050 Premie = 40 - 70 3. HR: Term =120 160 4. BP: 50 90 systolic 25 60 diastolic
Ideal Tidal Volume for neonates <33 weeks gestation (Based on 4-6 ml/kg IBW) Weight Min VT Max VT (kg) 0.5 2 3 1 4 6 1.5 6 9 2 8 12 2.5 10 15 3 12 18 Ideal tidal volume for neonates > 33 weeks gestation (Based on 5-7ml/kg IBW) Weight Minimum Maximum (kg) VT VT 1 5 7 2 10 14 3 15 21 4 20 28 5 25 35 6 30 42 7 35 49
Respiratorytherapycave.blogspot.com
You might also like
- Critical Care Intravenous DrugsDocument1 pageCritical Care Intravenous DrugsMarynel Dixie Izon Brao91% (11)
- Ventilator Graphics Cheat Sheet (Part 1)Document1 pageVentilator Graphics Cheat Sheet (Part 1)Rick Frea100% (2)
- Ventilator Graphics Cheatsheet (Part 2)Document1 pageVentilator Graphics Cheatsheet (Part 2)Rick Frea100% (2)
- Emergency Department Resuscitation of the Critically Ill, 2nd Edition: A Crash Course in Critical CareFrom EverandEmergency Department Resuscitation of the Critically Ill, 2nd Edition: A Crash Course in Critical CareNo ratings yet
- Capnography Cheat SheetDocument1 pageCapnography Cheat SheetRick Frea100% (1)
- Cheat Sheet 1Document1 pageCheat Sheet 1Rick Frea100% (10)
- Cheetsheet 6Document1 pageCheetsheet 6Rick Frea92% (12)
- ABG Made EasyDocument10 pagesABG Made EasyMayer Rosenberg100% (38)
- Cheetsheet 6Document1 pageCheetsheet 6Rick Frea92% (12)
- Lab CheatsheetDocument1 pageLab CheatsheetRick Frea86% (7)
- Vent Modes ChartDocument1 pageVent Modes Chartladyhavocinc100% (1)
- Lab CheatsheetDocument1 pageLab CheatsheetRick Frea86% (7)
- Lab CheatsheetDocument1 pageLab CheatsheetRick Frea86% (7)
- Haemodynamic Pocket GuideDocument2 pagesHaemodynamic Pocket GuideDarryl Betts85% (13)
- Icu GuidebookDocument43 pagesIcu Guidebookdrimran570100% (5)
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsFrom EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsNo ratings yet
- Cheatsheet 2Document1 pageCheatsheet 2Rick Frea86% (7)
- Acid-Base WorksheetDocument2 pagesAcid-Base WorksheetMayer Rosenberg100% (18)
- Cardiac Med ChartsDocument6 pagesCardiac Med ChartsNursingSchoolNotes100% (15)
- Control of Mechanical VentilationDocument6 pagesControl of Mechanical VentilationMichael Levit100% (1)
- Cheatsheet 4Document1 pageCheatsheet 4Rick FreaNo ratings yet
- Cheatsheet 5Document1 pageCheatsheet 5Rick Frea80% (5)
- Risk For Diseases Cheat SheetDocument1 pageRisk For Diseases Cheat SheetRick Frea100% (5)
- (SVR) Measures Systemic Resistance and Reflects Afterload of Left Ventricle Average Perfusion of A Cardiac CycleDocument1 page(SVR) Measures Systemic Resistance and Reflects Afterload of Left Ventricle Average Perfusion of A Cardiac Cyclesarah_stover_1100% (4)
- RT ConsultDocument5 pagesRT ConsultRick Frea100% (2)
- Ventilation Cheat SheetDocument1 pageVentilation Cheat Sheetlizzy59683% (6)
- Types of Assisted VentilationDocument1 pageTypes of Assisted VentilationJerry G100% (3)
- Respiratory DysfunctionDocument1 pageRespiratory Dysfunctionoxidalaj100% (3)
- Ventilation For DummiesDocument39 pagesVentilation For Dummiessuyalamit100% (6)
- RT Consult Form Side #2Document1 pageRT Consult Form Side #2Rick Frea100% (1)
- Cardiac Study GuideDocument11 pagesCardiac Study Guidejenwiley318096% (74)
- Emergency Room Aerosolized Medication ProtocolDocument3 pagesEmergency Room Aerosolized Medication ProtocolRick Frea67% (3)
- Neo-Peds Intubation Cheat SheetDocument1 pageNeo-Peds Intubation Cheat SheetRick FreaNo ratings yet
- RT Consult Form Side #1Document2 pagesRT Consult Form Side #1Rick Frea100% (2)
- ACLS EKG Rhythms and InterpretationDocument10 pagesACLS EKG Rhythms and Interpretationdonheyzz_02No ratings yet
- Settings and Management Tip Sheet For Providers: Isp Elevated?Document1 pageSettings and Management Tip Sheet For Providers: Isp Elevated?mohamedkorieshNo ratings yet
- Critical Care NotesDocument18 pagesCritical Care NotesjulieNo ratings yet
- Ekg PracticeDocument7 pagesEkg PracticeMichelle Cobb Matthews100% (1)
- Critical Care Calculations Study GuideDocument6 pagesCritical Care Calculations Study GuideAja Blue100% (2)
- Risk For Diseases Cheat SheetDocument1 pageRisk For Diseases Cheat SheetRick Frea100% (5)
- Emergency Room Aerosolized Medication ProtocolDocument3 pagesEmergency Room Aerosolized Medication ProtocolRick Frea67% (3)
- RT Consult Form Side #1Document2 pagesRT Consult Form Side #1Rick Frea100% (2)
- Cheatsheet 5Document1 pageCheatsheet 5Rick Frea80% (5)
- RT Consult Form Side #2Document1 pageRT Consult Form Side #2Rick Frea100% (1)
- RT ConsultDocument5 pagesRT ConsultRick Frea100% (2)
- Neo-Peds Intubation Cheat SheetDocument1 pageNeo-Peds Intubation Cheat SheetRick FreaNo ratings yet
- Normal Pediatric RR and HRDocument1 pageNormal Pediatric RR and HRRick FreaNo ratings yet
- Nautilus Strength Catalog RevisedDocument51 pagesNautilus Strength Catalog RevisedMario Lamberti100% (1)
- Prepgenie Sample Full Test Answers PDFDocument16 pagesPrepgenie Sample Full Test Answers PDFjimNo ratings yet
- MM2KDocument10 pagesMM2KSean Fern100% (1)
- Vibrio CholeraeDocument15 pagesVibrio Choleraetaimoor100% (1)
- Dimensional Analysis For Nursing StudentsFrom EverandDimensional Analysis For Nursing StudentsNo ratings yet
- Tidal Volumes Cheat SheetDocument1 pageTidal Volumes Cheat SheetRick Frea100% (1)
- CO2 Pocket GuideDocument2 pagesCO2 Pocket GuideDarryl Betts100% (7)
- Static Compliance & RSBI CheatsheetDocument1 pageStatic Compliance & RSBI CheatsheetRick FreaNo ratings yet
- Critical Care Survival GuideDocument2 pagesCritical Care Survival Guidetringalama100% (4)
- ABG InterpretationDocument1 pageABG Interpretationnulall100% (18)
- Mechanical Ventilator Management ProtocolDocument3 pagesMechanical Ventilator Management ProtocolRick Frea100% (2)
- Respiratory PathophysDocument1 pageRespiratory PathophysTori IkeharaNo ratings yet
- Inhaler LexiconDocument4 pagesInhaler LexiconRick Frea100% (2)
- Pediatric Respiratory Distress GuidelinesDocument1 pagePediatric Respiratory Distress GuidelinesRick FreaNo ratings yet
- Hemodynamic Assessment ParametersDocument2 pagesHemodynamic Assessment ParametersalexNo ratings yet
- FLASH CardsDocument3 pagesFLASH Cardsclarheena100% (2)
- Pediatric Mechanical VentilationDocument36 pagesPediatric Mechanical VentilationrizalNo ratings yet
- Electrolyte CompleteDocument6 pagesElectrolyte CompleteTofan Ana100% (2)
- Common Cardiac MedicationsDocument1 pageCommon Cardiac MedicationsPaige HardekopfNo ratings yet
- Respiratory Therapy Pocket Reference: Ifnopt TriggerDocument2 pagesRespiratory Therapy Pocket Reference: Ifnopt TriggermohamedkorieshNo ratings yet
- Boot Camp Hemodynamic MonitoringDocument37 pagesBoot Camp Hemodynamic MonitoringTinaHo100% (8)
- A Simplified ECG GuideDocument4 pagesA Simplified ECG Guidejalan_z96% (27)
- Basic EKG Interpretation Exam AnswersDocument3 pagesBasic EKG Interpretation Exam AnswerstwdroppointNo ratings yet
- Adjusting Ventilator SettingsDocument7 pagesAdjusting Ventilator SettingsSiva RamanNo ratings yet
- RT!: Reflections on a Career in Respiratory TherapyFrom EverandRT!: Reflections on a Career in Respiratory TherapyRating: 3 out of 5 stars3/5 (1)
- EKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!From EverandEKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!No ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Inhaler LexiconDocument4 pagesInhaler LexiconRick Frea100% (2)
- Pulmonary Function TestsDocument9 pagesPulmonary Function TestsRick Frea0% (1)
- RsbiDocument1 pageRsbiRick FreaNo ratings yet
- Mechanical Ventilator Management ProtocolDocument3 pagesMechanical Ventilator Management ProtocolRick Frea100% (2)
- Static Compliance & RSBI CheatsheetDocument1 pageStatic Compliance & RSBI CheatsheetRick FreaNo ratings yet
- Neonatal Ventilator Vent Set-Up CheatsheetDocument1 pageNeonatal Ventilator Vent Set-Up CheatsheetRick Frea50% (2)
- Pediatric Respiratory Distress GuidelinesDocument1 pagePediatric Respiratory Distress GuidelinesRick FreaNo ratings yet
- Neonatal Resuscitation ProgramDocument6 pagesNeonatal Resuscitation ProgramRick Frea100% (5)
- Neonatal Ventilator Vent Set-Up CheatsheetDocument1 pageNeonatal Ventilator Vent Set-Up CheatsheetRick Frea50% (2)
- Tidal Volumes Cheat SheetDocument1 pageTidal Volumes Cheat SheetRick Frea100% (1)
- MBBS Scheme Feb2014Document23 pagesMBBS Scheme Feb2014Sasikala MohanNo ratings yet
- Yoga FaceliftDocument164 pagesYoga Faceliftneca11neca100% (2)
- AQA Homeostasis and Response Knowledge OrganiserDocument6 pagesAQA Homeostasis and Response Knowledge OrganiserDan LiNo ratings yet
- Hit Ags10Document8 pagesHit Ags10George OstNo ratings yet
- 2 Treatment of Pulpitis With Biological, Vital Amputational and Extirpation Methods-1Document107 pages2 Treatment of Pulpitis With Biological, Vital Amputational and Extirpation Methods-1Bikku Negi100% (1)
- Appendix I - Plant TissuesDocument24 pagesAppendix I - Plant TissuesAmeera ChaitramNo ratings yet
- Vet. Internal Medicine Text BookDocument674 pagesVet. Internal Medicine Text Bookuhgl hgluvtm100% (5)
- LeukemiaDocument8 pagesLeukemiapriscillaNo ratings yet
- Eeg EogDocument19 pagesEeg EogpranoyrajNo ratings yet
- 22 Lecture PresentationDocument88 pages22 Lecture PresentationLeilaNo ratings yet
- Gas Exchange in PlantsDocument6 pagesGas Exchange in PlantsMaria Theresa HerreroNo ratings yet
- Where To Learn What in PaPhDocument1 pageWhere To Learn What in PaPhSydNo ratings yet
- Erythrosomes: Pinank V. Pandya Babaria Institute of Pharmacy, VadodaraDocument21 pagesErythrosomes: Pinank V. Pandya Babaria Institute of Pharmacy, VadodaraSagar Patel0% (2)
- Ineffective Airway ClearanceDocument6 pagesIneffective Airway Clearanceapi-253288732No ratings yet
- Diabetic Emergencies PDFDocument11 pagesDiabetic Emergencies PDFJuan C. Salazar PajaresNo ratings yet
- Bee Stings Immunology Allergy and Treatment Marterre PDFDocument9 pagesBee Stings Immunology Allergy and Treatment Marterre PDFOktaviana Sari DewiNo ratings yet
- Form Inte FinalDocument14 pagesForm Inte FinalCHRISTOPHER SCALENo ratings yet
- Biology Form 3 December Holiday AssignmentDocument38 pagesBiology Form 3 December Holiday Assignmenterastuskamunya1No ratings yet
- Advance 1 Term 3 ExamDocument6 pagesAdvance 1 Term 3 ExamMeenah KumariNo ratings yet
- Biology Mcqs PDFDocument58 pagesBiology Mcqs PDFMuhammad Mohsin RazaNo ratings yet
- Human Anatomy Study Guide: Chapter 10: Muscle Tissue and OrganizationDocument5 pagesHuman Anatomy Study Guide: Chapter 10: Muscle Tissue and OrganizationSuperjunior8No ratings yet
- Orthodontic Camouflage in Skeletal Class III Malocclusion A Contemporary ReviewDocument5 pagesOrthodontic Camouflage in Skeletal Class III Malocclusion A Contemporary ReviewNatasha Ank100% (1)
- Cambridge IGCSE: Biology 0610/21Document20 pagesCambridge IGCSE: Biology 0610/21Eain ThuNo ratings yet
- Structure and Function of DNADocument29 pagesStructure and Function of DNAMatthew Justin Villanueva GozoNo ratings yet
- Critical Review On Trends in Hydrotherapy ResearchDocument27 pagesCritical Review On Trends in Hydrotherapy ResearchPuneeth RaghavendraNo ratings yet
- BIOD 151 Essential Human Anatomy & Physiology I W/ Lab: 4 CreditsDocument10 pagesBIOD 151 Essential Human Anatomy & Physiology I W/ Lab: 4 CreditsFAHAD KHAN NIAZINo ratings yet