Professional Documents
Culture Documents
Marker of Steven Johnson Syndrome
Uploaded by
Billy Salvatore SoedirmanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Marker of Steven Johnson Syndrome
Uploaded by
Billy Salvatore SoedirmanCopyright:
Available Formats
The Pharmacogenomics Journal (2006) 6, 265268 & 2006 Nature Publishing Group All rights reserved 1470-269X/06 $30.
00
www.nature.com/tpj
ORIGINAL ARTICLE
A marker for Stevens-Johnson syndrome y: ethnicity matters
C Lonjou1, L Thomas2, N Borot1, N Ledger1, C de Toma3, H LeLouet4, E Graf5, M Schumacher5, A Hovnanian1, M Mockenhaupt6, J-C Roujeau2 (for the RegiSCAR group)
INSERM U563, CHU Purpan, France; Department of Dermatology, Hopital Henri Mondor, Creteil, Cedex, France; 3Fondation Jean 4 Dausset, Paris, France; Department of Pharmacovigilance, Hopital Henri Mondor, Creteil, Cedex, France; 5Institute of Med. Biometry and Informatics, University Hospital of Freiburg, Freiburg, Germany and 6Documentation centre of severe skin reactions (dZh), Department of Dermatology, University Hospital of Freiburg, Freiburg, Germany
2 1
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are rare but severe cutaneous adverse drug reactions, which can be caused by a certain number of specific drugs among which is carbamazepine, an antiepileptic agent. A very strong association of carbamazepine-induced SJS with HLA-B*1502 has recently been described in the Han Chinese population. Here in, we report preliminary results from a European study (RegiSCAR) of 12 carbamazepine-induced SJS/TEN cases (nine French and three German). Among these only four had a HLA-B*1502 allele. Remarkably, these four patients had an Asian ancestry, whereas the others did not as far as we have ascertained. This shows that although the HLA region may contain important genes for SJS, the HLA-B*1502 allele is not a universal marker for this disease and that ethnicity matters. The Pharmacogenomics Journal (2006) 6, 265268. doi:10.1038/sj.tpj.6500356; published online 17 January 2006
Keywords: Stevens-Johnson syndrome-toxic epidermal necrolysis; HLA; carbamazepine
Correspondence: Professor J-C Roujeau, Department of dermatology, Hopital Henri Mondor, F-94010 Creteil cedex France. E-mail: jean-claude.roujeau@ hmn.ap-hop-paris.fr
Introduction Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are severe cutaneous adverse reactions to drugs, which represent two forms of the same disease, TEN being the most severe form. Patients develop an acute exanthema, which progresses towards a widespread (TEN) or more limited (SJS) blistering and erosion of the skin and mucous membranes, resulting from apoptosis of keratinocytes. The incidence of SJS/TEN is estimated to be approximately two cases per million inhabitants per year. Up to now, no ethnic-related difference in overall incidence of SJS/TEN has been suspected. Although rare, these reactions have high morbidity and mortality, often resulting in a severe and definitive handicap. A limited number of drugs are associated with a high risk for SJS and TEN: several antiepileptic agents, especially carbamazepine, phenytoin, phenobarbital and lamotrigine, antibacterial sulfonamides, anti-inflammatory drugs of the oxicam family, allopurinol and the antiretroviral agent nevirapine.1,2 Although the pathophysiology of SJS and TEN remains largely unknown, previous work suggests an immune mechanism involving a drug-dependent cytotoxic cell response against epidermal cells. Cytokines like TNFa and Fas ligand (FasL) may play a role in the final apoptosis of the keratinocytes, but the initial events triggering the adverse reaction remain to be identified.3 An immune reaction directed against drug-reactive metabolites produced in excess or not detoxified has been suggested. This defect could be genetically determined, as suggested by several examples of individual pharmacogenetic variability associated with specific adverse drug reactions.46 More recently,
Received 27 June 2005; revised 25 October 2005; accepted 26 October 2005; published online 17 January 2006
A marker for Stevens-Johnson syndrome
C Lonjou et al
266
several lines of evidence have accumulated to show that the final steps of the adverse drug reaction depend on an immunological process, that seems directed against the parent form of the drug more often than against a metabolite.7 Azukizawa et al.8 generated transgenic mice in which ovalbumin was specifically expressed in keratinocytes. Transfer of ovalbumin-specific CD8 T cells into these transgenic mice resulted in rapid proliferation of these cells in lymph nodes and migration to the skin leading to a degeneration of the epidermis and hair follicles, which was reminiscent of TEN. In a 2004 issue of Nature,9 a Taiwanese study reported a very strong association between carbamazepine-induced SJS in Han Chinese patients and the HLA-B*1502 allele. Chung et al. studied 44 Han Chinese patients with carbamazepineinduced SJS and two groups of controls, 101 tolerant patients, who had taken carbamazepine for at least 3 months and 93 healthy controls without carbamazepine use. All 44 SJS or TEN patients had a HLA-B*1502 allele in contrast with 3% of the carbamazepine tolerant and 8.6% of the unexposed controls, respectively. Previous work on HLA and SJS/TEN in France (not focussing specifically on carbamazepine) found a much weaker association with B44 (split of B12), and different haplotypes associated with intolerance to sulfonamides (A29-B12-DR7, an ancestral haplotype in a population of European origin), or to oxicamnonsteroidal antiinflammatory drug (NSAIDs) (A2-B12).10 Together these results show the importance of this region for SJS/TEN. In Europe, the percentage of cases of SJS and TEN induced by carbamazepine is about 56%,1 compared to 2533% in Taiwan.9 We are currently conducting a European study on SJS and TEN (RegiSCAR). At the time of this study, 12 cases were identified as SJS or TEN patients for which carbamazepine was considered to be the culprit drug. Table 1 shows the clinical characteristics of the patients with carbamazepine-induced SJS/TEN identified in our study.
Results and discussion We determined the HLA-B genotypes of the 12 carbamazepine-induced cases by polymerase chain reaction using sequence specific primers (PCR-SSP, Genovision kit) (see results in Table 2). We found that only four patients had the B*1502 allele (all being heterozygous). Although relatively frequent in the Han Chinese population (8%),11 B*1502 is very rare in Europe. The allele frequency of B*1502 was only 12% in prior studies of European populations.11 The frequency of 16.7% (4/24) observed in our cases suggests an over-representation of this allele in our cases, and a risk associated with its presence. Interestingly, the four individuals with B*1502 were the only four cases with a patent Asian origin among the 12 patients studied. They originated from China, Vietnam, Cambodia and the Reunion Island, respectively.
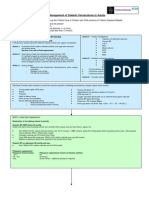
Table 2 HLA-B and supertypes in 12 patients with carbamazepine-induced SJS/TEN
ID 1 2 3 4 5 6 7 8 9 10 11 12 HLA-B alleles B1502 B35 B50 B13 B07 B13 B37 B08 B18 B08 B1502 B08 B38 B44 B51 B1502 B44 B1502 B73 B27 B57 B35 B37 B35 B62 B7 B44 B62 B7 B62 B44 B8 B44 B8 B62 B8 Supertypes B27 B44 B7 B62 B44 B62 B27 B27 B58 B7 B44 B7
Bold characters indicate genotypes or supertypes more often expressed than expected.
Table 1
No. 1 2 3 4 5 6 7 8 9 10 11 12
a
b
Clinical caracteristics of patients with carbamazepine-induced SJS/TEN Age 31 46 52 40 54 39 74 46 57 42 26 37 Sex M M M M M F F M M F F M Phenotype SJS SJS/TEN TEN SJS/TEN SJS SJS/TEN SJS/TEN SJS SJS/TEN TEN SJS SJS Diagnosis Definite Definite Definite Definite Probable Probable Definite Definite Definite Definite Probable Probable %BSAa 5 13 90 26 4 14 17 5 30 70 10 6 Mucosab 2 4 4 2 4 2 3 5 2 4 2 3 Place of birth Vietnamc Germany France Chinac France Cambodiac France Germany France France Reunion Islandc France
overlap overlap overlap overlap overlap
Maximum of skin detachment (% BSA: body surface area). Number of mucosal sites involved. c Patients with Asian ancestry.
The Pharmacogenomics Journal
A marker for Stevens-Johnson syndrome
C Lonjou et al
267
The main biological function of HLA molecules is to bind short peptides derived from the processing of intracellular and extracellular proteins, and to present them on the cell surface to specific T cells.12 The peptide specificity of a given HLA molecule resides in its binding groove, lined with different pockets that engage specific side chains of the peptide ligands.13 HLA genes are extremely polymorphic and they encode proteins which play a crucial role in immunity. However, not all genetically different molecules are functionally different, and it is possible to group them into supertypes on the basis of their functional binding properties.14 The HLA-B*1502 allele is part of the HLA-B62 supertype,14 which was not found in our study among any of the eight carbamazepine-induced cases in patients who do not present the B*1502 allele. These eight patients had different HLA supertypes among which B44 was present in 5/8 patients, which represents a higher phenotypic frequency than that observed in people of European origin14 (62.5% in our cases, compared to 43% in reference14). However, the role of supertypes may not be relevant for immune response to drugs, which are usually very small nonpeptide molecules. In some cases there may be haptenization of self-peptides by a reactive metabolite, but it has been demonstrated that medications are often presented through noncovalent binding with MHC Class I molecules.15 In this context, one may hypothesize that rare and severe reactions to drugs, such as SJS or TEN are dependent on infrequent HLA alleles, each being capable of binding to a specific drug. Our data are preliminary, but anyhow very intriguing. Although obtained on a limited number of patients, our results clearly exclude the hypothesis that the 100% association observed in Taiwan with B*1502 is universal. As the odds ratio for this allele is extremely high in the Taiwanese study (odds ratio 895 for CBZ-SJS/normal with a 95% CI 5015,869), our study with 12 cases was of sufficient size to detect such a strong effect. Since our study included only four patients originating from different Asian countries, it was not able to support or not the conclusion of the Taiwanese study in Han Chinese patients. Furthermore we cannot exclude that a few other French or German patients had some Asian ancestry. However, our data also exclude the hypothesis of another single HLA B allele with a close to 100% association in a western European population. This result has both practical and theoretical implications. Practically, B*1502 cannot be considered as a useful prediction marker of CBZ related SJS in the European population. Theoretically a number of different hypothesis can be considered to explain the results observed. The first being that HLA-B is involved by its capacity to present the drug to T cells and to initiate the immune response to carbamazepine. In this hypothesis, our results show that B*1502 is not the only relevant allele. Different alleles at the same locus could be responsible for increased disease risk in different populations and our results are too preliminary to exclude this hypothesis. However, they do not suggest the existence of an alternative single HLA-B allele with a very strong association in Europe. The second hypothesis is linkage disequilibrium (LD), which varies in different populations, the same high-risk
allele may have a different pattern of association with marker alleles and haplotypes. The association reported in the literature in the Han Chinese sample with B*1502, might be explained by a causal variant which is in strong LD with B*1502 in the Han Chinese population, but not in a European population. Therefore, other genes closely located to HLA-B could be the cause of the observed association, due to strong linkage disequilibrium in the HLA region. SJS is a rare condition with a probable complex inheritance, the list of candidate genes could include genes encoding metabolic enzymes, transport proteins, involved in the immune response, the regulation of apoptosisy. It is possible that a combination of genes is necessary to create this rare phenotype and methods allowing the study of genegene interactions (epistasis) on a much larger sample will be needed. Another important implication of the present preliminary study is that ethnicity matters more than was originally suspected in the pharmacogenomics of severe cutaneous adverse reactions to drugs. This is a key point for advancing further the research in this field: it will be essential to collect more information on ethnicity of the patients and/or to study well-defined ethnic groups. Recently, the same Taiwanese group reported a strong association between HLA-B*5801 and severe cutaneous reactions to allopurinol in Han Chinese patients.16 This new finding sustains a possible drug-specific gene effect in these severe cutaneous adverse drug reactions. It will be interesting to see if this new association will be replicated in our European population.
Materials and methods For each patient, written informed consent approved by the ethical committee of each participating country was obtained. A standardized clinical assessment was used and each case was confirmed after review by the international expert committee of the study. Only patients with a final score corresponding to a definite or probable diagnosis were included in the study (possible cases being excluded). SJS is defined when skin detachment is o10% of body-surface area, TEN by a skin detachment 430%, intermediate detachment correspond to SJS/TEN overlap. The same case definitions were used by the Taiwanese group.8 In about 50% of SJS/TEN cases, it is possible to identify clearly which drug is responsible for the adverse event. To identify those individuals for which carbamazepine induced the adverse event, a decisional algorithm was used and the cases were reviewed by an expert in order to take into account parallel comedication, causality and multiple episodes. Information related to ethnicity was limited to skin phenotype, place of birth of the patient and his/her parents. Peripheral blood was taken from all study participants for DNA extraction. We determined the HLA-B genotypes by polymerase chain reaction using sequence specific primers (PCR-SSP, Genovision kit).
The Pharmacogenomics Journal
A marker for Stevens-Johnson syndrome
C Lonjou et al
268
Abbreviations
SJS TEN NSAID Stevens-Johnson syndrome Toxic epidermal necrolysis Nonsteroidal anti-inflammatory drug
Acknowledgments
We thank all SCAR-patients and their physicians as well as the French patients association, Amalyste, for their important contribution. This study was funded by grants from the European Commission (QLRT-2001-01738), ORPHANET and INSERM ATC Pharmacogenetique. NL is funded by a SIDACTION grant.
Duality of Interest None declared. References
1 Roujeau JC, Kelly JP, Naldi L, Rzany B, Stern RS, Anderson T et al. Medication use and risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. New Engl J Med 1995; 333: 16001607. 2 Fagot JP, Mockenhaupt M, Bouwes-Bavinck JN, Naldi L, Viboud C, Roujeau J-C. Nevirapine and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis: preliminary results of a case-control study. AIDS 2001; 15: 16. 3 Viard I, Wehrli P, Bullani R, Schneider P, Holler N, Salomon D et al. Inhibition of toxic epidermal necrolysis by blockade of CD95 with human intravenous immunoglobin. Science 1998; 282: 490493.
4 Nebert DW. Pharmacogenetics and pharmacogenomics: why is this relevant to the clinical geneticist? Clin Genet 1999; 56: 247258. 5 Mallal S, Nolan D, Witt C, Mosel G, Martin AM, Moore C et al. Association between presence of HLA-B*5701, HLA-DR7, and HLA-DQ3 and hypersensitivity to HIV1 reverse-transcriptase inhibitor abacavir. Lancet 2002; 359: 727732. 6 Hetherington S, Hughes AR, Mosteller M, Shortino D, Baker KL, Spreen W et al. Genetic variation in HLA-B region and hypersensitivity reactions to abacavir. Lancet 2002; 359: 11211122. 7 Nassif A, Bensussan A, Boumsell L, Deniaud A, Moslehi H, Wolkenstein P et al. Toxic epidermal necrolysis: effector cells are drug specific cytotoxic T cells. J Allergy Clin Immunol 2004; 114: 12091215. 8 Azukizawa H, Kasaka H, Sano S, Heath WR, Takahashi I, Gao X et al. Induction of T-Cell mediated skin disease specific for antigen transgenically expressed in keratinocytes. Eur J Immunol 2003; 33: 18791888. 9 Chung WH, Hung SI, Hong HS, Hsih MS, Yang LC, Ho HC et al. A marker for Stevens-Johnson syndrome. Nature 2004; 428: 486. 10 Roujeau JC, Huynh TN, Bracq C, Guillaume JC, Revuz J, Touraine R. Genetic susceptibility to toxic epidermal necrolysis. Arch Dermatol 1987; 123: 11711173. 11 Geer L, Terasaki PI, Gjertson DJ. HLA frequency. HLA. In: Gjertson DW, Terasaki PI (eds). HLA 1998. Lenexa: American Society for Histrocompatibility and Immunogenetics: 1998, pp. 327363. 12 Germain RN. MHC-dependent antigen processing and peptide presentation: providing ligands for T lymphocyte activation. Cell 1994; 76: 287299. 13 Madden DR. The three dimensional structure of peptide-MHC complexes. Ann Rev Immunol 1995; 13: 587622. 14 Sette A, Sidney J. Nine major HLA class I supertypes account for the vast preponderance of HLA-A and -B polymorphism. Immunogenetics 1999; 50: 201212. 15 Schnyder B, Burkhart C, Schnyder-Frutig K, von Greyerz S, Naisbitt DJ, Pirmohamed M et al. Recognition of sulfomethoxazole and its reactive metabolites by Drug-Specific CD4+ T cells from allergic Individuals. J Immunol 2000; 164: 66476654. 16 Hung SH, Chung WH, Liou LB, Chu CC, Lin M, Huang HP et al. HLAB*5801 allele as a genetic marker for severe cutaneous adverse reactions caused by allopurinol. Proc Natl Acad Sci USA 2005; 102: 41344139.
The Pharmacogenomics Journal
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Who TRMDocument250 pagesWho TRMDaniel Giraldo Toro100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 7 - Speaker Notes - 08333 - STN-Spinal Column - Spinal Cord InjuriesDocument75 pages7 - Speaker Notes - 08333 - STN-Spinal Column - Spinal Cord InjuriesBilly Salvatore SoedirmanNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Chapter 2Document9 pagesChapter 2Monissa ArrianiNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Treatment For AutismDocument22 pagesTreatment For Autismbig fourNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Diagnosis Treatment Malaria 2013Document20 pagesDiagnosis Treatment Malaria 2013leo randa sebaztian simangunsongNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Dopamine - CNS Pathways and Neurophysiology 549Document7 pagesDopamine - CNS Pathways and Neurophysiology 549Borzoo TajdinNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Dopamine PDFDocument9 pagesDopamine PDFBilly Salvatore SoedirmanNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Should The New Hypertension Guidelines Affect Your Practice - PetersonDocument24 pagesShould The New Hypertension Guidelines Affect Your Practice - PetersonRendha Fatima RystaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Lepromin TestDocument4 pagesLepromin TestBilly Salvatore SoedirmanNo ratings yet
- Pemberian Zat BesiDocument8 pagesPemberian Zat BesiBilly Salvatore SoedirmanNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Dka Guidelines - 2012Document4 pagesDka Guidelines - 2012djizhieeNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Marker of Steven Johnson SyndromeDocument4 pagesMarker of Steven Johnson SyndromeBilly Salvatore SoedirmanNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)