Professional Documents
Culture Documents
Operatif Delivery
Uploaded by
Pepo AryabarjaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Operatif Delivery
Uploaded by
Pepo AryabarjaCopyright:
Available Formats
OPERATIVE DELIVERIES
Presented by Dr NANA Philippe
PLAN
DEFINITION ROUTES -VAGINAL -ABDOMINAL
A- ABDOMINAL= CAESAREAN SECTION
1. HISTORY 2. TYPES OF CAESAREAN SECTION 3. INDICATIONS 4. COMPLICATIONS 5. SPECIAL SITUATIONS
B- VAGINAL
1. FORCEPS DELIVERY 2. BREECH DELIVERY 3. DESTRUCTIVE OPERATIONS 4. SYMPHYSIOTOMY 5. EPISIOTOMY
DEFINITION Operative delivery denotes any obstetric procedure in which active measures are taken to accomplish delivery. The success of such a procedure depends on the skill and /or experience of the Operator. The timing of such an intervention must be in the interest of both the mother and the baby.
ABDOMINAL ROUTE - CAESAREAN SECTION Definition: This is delivery through an abdominal route by an incision on the abdominal wall and the uterus after 28 weeks of gestation. This definition excludes vaginal caesarean section, laparotomy for uterine rupture or abdominal pregnancy. HISTORICAL NOTES It is generally said that the operation originated from the decree lex Caesarea under the rule of the Caesars which stipulated that before burial of the mother, the child be
removed from the uterus of any woman dying in late pregnancy. Others think it originated from the Latin word caedere meaning to cut. The first caesarean section was carried out in 1610 and the first successful one in 1794 in the USA. Early caesarean sections were associated high maternal and foetal mortality because of haemorrhage and sepsis. LEBAS (1769), first to introduce the use of sutures. PORRO, ITALY (1876) introduced a modification in the surgery that consisted of amputating the corpus of the uterus (sub-total hysterectomy). This was followed by a marked reduction in maternal mortality (70-80% in 1870 to about 50%). KEHRER, 1881 intrduced the lower segment caesarean section. SANGER, 1882 introduced the classical caesarean section. TYPES OF INCISION AT CAESAREAN SECTIONS Classical Caesarean Section Lower Segment Caesarean Section Caesarean Hysterectomy Extra-peritoneal Caesarean Section (Abandoned). General consideration: The caesarean section rate has steadily been on the increase and varies between 5% and 30% in most reported series. The rate varies between 8 and 10% in our major hospitals in Yaounde. This change in the rate of caesarean section is due to the following: Abandoning of high forceps and reduction in the number of mid forceps, increased intra-partum surveillance, a decreasing number of vaginal breech delivery and an increasing elective and primary caesarean section rate. Materno-foetal mortality has also improved due widening of indications, improved surgical techniques, blood transfusion, infection prevention measures and anaesthetic methods. Caesarean section is not a risk free operation and this must be taken into consideration before deciding to operate. Maternal mortality associated with caesarean section varies in different series from 4 in 10.000 to 8 in 10.000 operations. Caesarean section is preferable to a difficult vaginal delivery. There are no conclusive proofs that the liberal use of caesarean section improves the mental performance or reduce the incidence of neurological deficits of children or adults. Classical Caesarean Section. Advantages: It is easy to perform. Today it has very limited indications (conjoint twins, post-mortem, varicose veins and adhesion over the lower segment, impacted neglected shoulder presentation). However, it has several 2
disadvantages: associated with increased bleeding, increased risk of rupture in subsequent pregnancy and increased risk of intestinal obstruction. Lower Segment Caesarean Section. Three types of incision can be done on the lower segment. A- Transverse incision: Most practised type Advantages Muscle under less tension thus undisturbed healing. Decreased risk of peritoneal contamination because incision is behind the bladder and covered by peritoneum so infected material cannot escape into the peritoneal cavity. Lies in the line of the predominating muscle fibres and any stretch occur in the desired transverse direction. It contains more fibrous tissue than the body proper of the uterus. Convalescence is better than for classical scar. Decrease risk of uterine rupture in subsequent pregnancy. Rupture when it occurs is usually not catastrophic because most often it is a dehiscence of the scar. The uterine wall of the lower segment is thin especially when labour has progressed. It is also less vascularised thus better stitching. B Vertical Incision: Advantages Easy extension to the corpus of the uterus (indicated for shoulder presentation, monstrosity, macrosomia, contraction ring, varices etc). It has the disadvantage that it easily extends to the corpus (classical) or the bladder or vagina. C- L incision or inverted T: seldom used. Caesarean Hysterectomy. This is infrequently practised. However, it may be carried out in situations of an operable cancer of the cervix, uterine rupture and uncontrollable post-partum haemorrhage (Placenta accreta). Extra-peritoneal Caesarean Section. Technique that has been abandoned in present practiced of Obstetrics and Gynaecology.
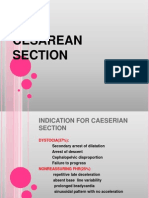
INDICATIONS Caesarean section is indicated when vaginal delivery is not feasible or would impose undue risk on the mother or baby or both. Caesarean section can be carried out as an ELECTIVE PROCEDURE or an EMERGENCY PROCEDURE. The indications can be divided into two groups: A- ABSOLUTE OR RECURRENT INDICATIONS (obvious cephalo-pelvis disproportion = contracted pelvis). B- RELATIVE OR NON RECCURENT INDICATIONS. The dictum once a caesarean section always a caesarean section has been changed to once a caesarean section always hospital delivery. Vaginal delivery or trial of scar can be carried out under the following conditions: Indication for previous caesarean section was non recurrent. Previous caesarean section was a lower segment caesarean section. Presentation is cephalic, with a good BISHOP SCORE. Onset of labour before the expected date of delivery. Foetal weight less than 3500gms. No other risk factor identified (two risk factors is an indication for C/S). Caesarean section is not risk free operation. It is usually complicated by haemorrhage, infection and embolism. The obstetrical history of the mother may be prejudiced by the scar. INDICATION PROPER Cephalo-pelvic Disproportion. This may occur at the inlet, mid-cavity or at the outlet. It may be due to an absolute contracted pelvis or it is relative due to a malposition malpresentation or foetal macrosomia (>4000gms). Major type Placenta praevia. Placenta abruption with foetal activity. Malpresentation and or malposition. Decision is guided by a number of factors such as condition of the pelvis, foetal weight, parity, age, lie etc. Preeclampsia/eclampsia: Except conditions are not favourable for vaginal delivery, induction is the method of choice. Foetal distress Cord prolapse Mass praevia 4
Previous uterine scar Cervical dystocia Cancer of the cervix X factor such as poor obstetrical history, repair of vesico-vaginal fistula, vaginoplasty etc. CONTRAINDICATIONS *Absence of an appropriate indication. *Pyogenic infection of the abdominal wall. COMPLICATIONS AND PROGNOSIS The following factors may affect healing of the uterine incision: Haemostasis Accuracy of apposition Quality and amount of suture material Avoidance of infection and tissue strangulation. The major complications of caesarean section are: A-Uterine Rupture in subsequent pregnancy: The incidence varies from 1-2% for classical scars and 0.5-1% for lower segment caesarean section scars. Pain in the area of the scar may suggest dehiscence and 20% of all ruptured uterine scars occur before the onset of labour especially with classical scars. Rupture of classical scar is usually catastrophic, sudden total with partial or complete extrusion of the foetus into the abdominal cavity. Haemorrhage and shock are prominent. The rupture of a lower segment caesarean section scar is more subtle characterised by pain and slower internal bleeding. However, in wound dehiscence the rupture is silent and caesarean section scar or myometrial fenestration is covered by the visceral peritoneum. B-Post-operative infection: Endometritis, wound sepsis, peritonitis, eventrations and secondarily pelvic adhesions, intestinal obstruction. C- Injury to the urinary system: Bladder, ureters, and secondarily vesico-vaginal fistula D- Injury to the uterine vessels with massive haemorrhage. E- Embolism: Pulmonary, thrombophlebitis and deep venous thrombosis.
SPECIAL SITUATIONS A-GENERAL MEASURES 1- Before surgery: Confirm the gestational age (LMP, Physical examination, ultrasound). 2- Time the procedure: Elective procedures carried out at 37 completed weeks. Emergency procedures are done immediately for maternal or foetal interest. 3- When applicable always type and cross-match at least two units of blood. 4- Prophylaxis antibiotics are used for elective operations and therapeutic antibiotics for emergency operations. 5- Always adopt a left lateral tilting position with slight TREDENLEBURG to prevent supine caval compression syndrome. 6- The median or Para-median sub-umbilical incision is preferable if an expeditious delivery is anticipated or if there is a suspected uterine rupture. 7- The Pfannenstiel incision is cosmetic and less liable to wound dehiscence or incisional hernia. 8- Resorbable suture materials are preferred, non resorbable sutures are associated with increased risk of pelvic adhesions and may predispose to fistula formation especially for lower segment caesarean sections. B-ANAESTHESIA IN CAESAREAN SECTION *General anaesthesia in emergency situations may complicate with inhalation aspiration or MENDELSON syndrome in the mother and respiratory depression in the baby. *Loco-regional anaesthesia: Epidural, Spinal: Good method of anaesthesia for caesarean sections especially emergency operation. However, supine hypotension syndrome usually complicates this type of anaesthesia. *Local anaesthesia(xylocaine(lignocaine) 0.5%. It has action duration of 45 minutes. It has the following advantages: It is safe, associated with quick recovery, post-op vomiting is avoided, there is decreased haemorrhage and the foetus is born
in good condition. However, this type of anaesthesia is contraindicated when the parturient has a poor temperament or other intra abdominal surgery is anticipated. C-OTHER SURGICAL PROCEDURES Appendectomy: When ever the diagnosis is made, irrespective of the gestation age. However, prophylactic appendectomy should be performed only if there are no risk factors such as prolonged operation time, prior transfusion, preeclampsia/eclampsia, potential or actual infection. Myomectomy: Usually it is not advisable to perform myomectomy at caesarean section except pedunculated tumours, subserous myomas with a small base or the myoma occupies the zone of incision. Hysterectomy: Indicated when there is uncontrollable haemorrhage, uterine rupture severe enough to hinder a conservative approach, placenta accreta and exceptionally with very huge uterine myomas. Post-mortem caesarean section. Perinatal mortality associated to it is very high if not 100%. The probability of the child surviving is increased if surgery is done when death is imminent. Tubal Ligation: The uterus is still abdominal and the procedure is easy to perform. D-FRANK INFECTION AND CAESAREAN SECTION The risk of local infection or generalised infection is increased. The following procedures should be carried out to minimize the spread of infection: Adequate control of bleeding, no devitalisation of tissues. Use of therapeutic Antibiotics. Reverse TRENDELENBURG POSITION. Shutting of the general peritoneal cavity before opening into the lower segment. Peritoneal lavage.
Former techniques such as extra peritoneal caesarean section and hysterectomy are today abandoned.
FORCEPS OPERATIONS Definition: The Obstetric Forceps is an instrument designed to extract the babys head. It has three functions: APREHENSION, ROTATION AND TRACTION. The objectives of the forceps operation is to expedite delivery i.e. shorten second stage of labour, overcome or correct certain abnormalities e.g. malposition, and is a life saving procedure to the mother or the baby. PARTS OF A FORCEPS It consists of two matched parts that articulate or lock. Each part is composed of a blade, shank, lock and handle. The blade possesses two curves: the cephalic and pelvic curves. There are two groups of forceps, the classic e.g. SIMPSONS and the special forceps such as the KEILLANDS AND TARNIER for transverse arrest or OP positions, the WRIGGLERS FOR LIFT OUT and the PIPERS for the after coming head in breech delivery. INDICATION AND CONDITIONS FOR FORCEPS DELIVERY Forceps operation is indicated when there is a fault at one of the following levels: Fault in the Forces: When there is uterine inertia or poor uterine contraction and the second stage has gone pass two hours. In this case the perineum and the coccyx offer the only resistance. Fault in the child: When an unfavourable diameter of the head presents to the pelvis e.g. OA in a flat pelvis, OP position, Face presentation and after coming head. Fault in the passage such as in transverse arrest, relative cephalopelvic disproportion. Maternal indications: Situations in which continuation of the second stage of labour would constitute a significant threat to the life of the mother, thus second stage of labour most be shortened e.g. Cardiac and pulmonary disorders, sicklers, severe pre-eclampsia/eclampsia ,maternal exhaustion and other debilitating disease or illness. Foetal indications: Dangers threatening the foetal well-being such as Foetal distress ( Foetal heart tone <100 or>160/minute), late deceleration pattern or gross irregularity, excessive foetal movement, passage of meconium stained liquor in cephalic presentation.
CONDITIONS FOR FORCEPS DELIVERY Full Dilatation. Cephalic presentation (face with chin anterior). Membranes must be ruptured. The head must be engaged (+2). Pelvis must be adequate (no significant CPD). Empty the bladder. CLASSIFICATION AND DEFINITION OF FORCEPS DELIVERIES No classification of forceps delivery is acceptable to all obstetricians. Never the less a workable classification is essential to permit comparison of results and difficulties encountered with the procedure. One of such classification is that proposed by DANFORTH; Outlet or Lift out Forceps: The scalp is visible at the introitus without the need to separate the labia, the skull is at the pelvic floor and the sagittal suture in the antero-posterior diameter of the pelvis. Here only the perineum and the coccyx offer resistance to delivery. Low Forceps: The station is at +3 and the sagittal suture in the anteroposterior diameter of the pelvis or oblique diameter. Mid Forceps: Here the head is engaged and the station is at O. It is associated with an increased morbidity such as low APGAR rating, increased neurological defects thus is rarely indicated. Caesarean section should be preferred except in situations of intra-uterine death, severe foetal distress and abruptio placenta. High Forceps: Before engagement of the foetal head. This procedure has been abandoned because it is associated with injury to both mother and the baby. SPECIAL CIRCUMSTANCES o PROPHYLACTIC FORCEPS: Another name for liftout forceps and carried out to prevent severe perineal tear. o FAILED FORCEPS: An unsuccessful attempt. o TRIAL FORCEPS: Tentative procedure prior to caesarean section. DANGERS AND COMPLICATIONS OF FORCEPS DELIVERY MATERNAL: Extension of episiotomy, uterine rupture, vesico-vaginal fistula. FOETAL: Transient facial paralysis, irreparable intracranial damage; 9
.These complications are usually due to errors in the judgement or lack of the technical skill.
VACUUM EXTRACTOR OR VENTOUSE An instrument that applies traction to the foetal head by means of a suction cup attached to the scalp. This is about a substitute to the forceps. It may be used to control bleeding in minor placenta praevia or before full dilatation when indicated. The instrument was designed by MALMSTROM IN 1957. It consist of three suction cups of various sizes, a hose with a chain, a traction bar, a manometer, a bottle and a pump. CONTRAINDICATIONS Delivery of premature. The management of foetal distress. Accelerate labour before full dilatation. Malrotation or malposition. COMPLICATIONS Sloughing of the scalp. Decapitation Cervical tear Cephalhaematoma Intracranial haemorrhage Vesico-vaginal fistula Tentorial tear
BREECH DELIVERIES: TYPES 1. Frank breech (65%). 2. Complete OR Full breech (cross leg sitting)(10%). 3. Incomplete OR Footling breech (25%) = Single or double footling breech. FACTORS PREDISPOSING TO BREECH 1) Accommodation of the large pole of the baby to the more commodious portion of the uterus. The fundal space may be compromised by a septum or may be cornuate. 10
2) Foetal abnormalities: hydrocephalus, large congenital goitre. 3) Extension of the legs of the foetus as in frank breech immobilizes the body hindering spontaneous rotation. 4) Increased uterine tone and relative oligohydramnios. 5) Multiparity, placenta praevia, polyhydramnios, contracted pelvis, pelvic tumour; The incidence of breech presentation correlates directly with foetal weight and consequently with the duration of pregnancy: Birth weight 1000gms (23%), 1500gms (12%), 2000gms (8%), and >3000gms (3%). DANGERS OF BREECH PRESENTATION A- MOTHER: I. Intrapartum and postpartum infection due to premature rupture of membranes. II. Prolonged labour. III. Genital tract lacerations and tears from version manoeuvres ( uterus, cervix, vagina, perineum). B- FOETUS: A. Increased neonatal death (4-5 times higher than for vertex). B. Increased cord prolapse (footling and complete breech). C. Molding is abrupt thus stressful to the after coming head. D. Intracranial haemorrhage. E. Laceration of the tentorium. F. Injuries to nerves (brachial and cervical plexuses). Breech presentation are usually prevented by external cephalic version but this procedure is not common practise today because of associated risk such as abruptio placenta , cord strangulation, rupture of membranes rhesus iso-immunisation, uterine rupture etc. FAVOURABLE FACTORS FOR VAGINAL DELIVERY a) Gestational age>36 <38 weeks. b) Estimated weight >2.5Kgs < 3.5Kgs. c) Presenting part at or below station 1 at the onset of labour. 11
d) Good BISHOPS SCORE (cervix soft, effaced and >3 cm dilated). e) Ample Gynecoid or Anthropoid pelvis. f) Past history of previous vaginal delivery of a breech> 3.5Kgs or babies > 4Kgs. UNFAVOURABLE FACTORS FOR VAGINAL DELIVERY a. Gestational age > 38 weeks. b. Foetal weight > 3.5Kgs, Station < -2. c. Poor BISHOPS SCORE (firm, non effaced cervix, <3 cm dilated). d. Primipara or history of difficult vaginal delivery e. Android or flat pelvis. f. Footling or complete breech ( increased cord prolapse). g. Hyperextension of the foetal head. TECHNIQUES OF BREECH DELIVERY: o Spontaneous breech delivery (premature). o Assisted breech delivery o Breech extraction o DRUHSSENS incision may be require to expedite vaginal delivery in situations such as retention of the after coming head or when vaginal delivery will be more rapid than caesarean section. However, it can only be carried out if there is good effacement of the cervix, the cervix dilated at> 6cm, station at +3 and there is no impediment to delivery except the cervix. Internal podalic versions whose scope has greatly reduced because of the high foetal mortality and the danger to the mother of uterine rupture may be carried out in situation of retention of a second twin. DESTRUCTIVE OPERATIONS Destructive operations a procedure to reduce the bulk of the child in order to permit easy passage through the parturient canal are virtually obsolete and almost never done in the developed countries but it may be an essential part of obstetric practice in some developing countries. No operative operation should be carried out except it has a reduced risk than the caesarean section. An intrauterine death is not a contraindication to caesarean section. The following operations are included among destructive procedures: 12
CRANIOTOMY: Perforation of the skull and evacuation of its content to reduce the size of the head (hydrocephalus). Cranioclasm, is crushing of the cranium. DECAPITATION: indicated for neglected shoulder presentation with intrauterine death, interlocking twins. CLEIDOTOMY: Division of the clavicle (shoulder dystocia). EVISCERATION: It may be thoracic or abdominal when the obstruction is due to abnormal size of the thorax and/ or the abdomen (Tumour or accumulation of fluid). Destructive procedures complicate with tear or laceration of the vagina, cervix and lower segment of the uterus. Always explore therefore for such a complication. Sometimes a catheter must be left in place to prevent vesico-vaginal fistula. If a fistula occurs it is repaired after three months. SYMPHYSIOTOMY HISTORY: Claude de la Couve (1655) first performed the operation on the dead as an alternative to caesarean section. The first successful operation was carried out by Sigault in 1777 but today this procedure is abandoned in favour of the caesarean section. EPISIOTOMY Operation carried out to relieve outlet obstruction and prevent severe perineal tears. The tendency today is to individualise the operation.
13
You might also like
- C-S & VbacDocument54 pagesC-S & VbacDagnachew kasayeNo ratings yet
- Caesarean Section4817080565385082090Document38 pagesCaesarean Section4817080565385082090DoaaNo ratings yet
- Cesarean SectionDocument20 pagesCesarean Sectionjeribob1823No ratings yet
- Cesarean SectionDocument110 pagesCesarean SectionyordiNo ratings yet
- C SectionDocument10 pagesC Sectionshubham kumarNo ratings yet
- Uterine Anomaly, Fibroid Uterus, Ovarian Tumor, Uterine ProlapseDocument30 pagesUterine Anomaly, Fibroid Uterus, Ovarian Tumor, Uterine ProlapseVijith.V.kumar80% (5)
- 15b Ectopicpregnancy 090507104012 Phpapp02 130825152041 Phpapp01Document48 pages15b Ectopicpregnancy 090507104012 Phpapp02 130825152041 Phpapp01Erwynsonsaut SimanjuntakNo ratings yet
- Anaesthesia For Fetal SurgeriesDocument8 pagesAnaesthesia For Fetal SurgeriesrepyNo ratings yet
- Ectopic Pregnancy22Document43 pagesEctopic Pregnancy22Sunil YadavNo ratings yet
- Caesarean SectionDocument48 pagesCaesarean SectionStaen KisNo ratings yet
- By Dr. Malleswar Rao Kasina, MD, Dgo. Hod & CSS, Dept. of Gynobs, Esi Hospital, Sanathnagar, Hyderabad, Ap, IndiaDocument102 pagesBy Dr. Malleswar Rao Kasina, MD, Dgo. Hod & CSS, Dept. of Gynobs, Esi Hospital, Sanathnagar, Hyderabad, Ap, IndiaHerry SasukeNo ratings yet
- Cesarean SectionDocument6 pagesCesarean Sectionmohammed alkananiNo ratings yet
- Cesarean Section: Associate Professor Ph.D. E.A. EinyshDocument33 pagesCesarean Section: Associate Professor Ph.D. E.A. EinyshPrerit Aggarwal100% (1)
- Ectopic Pregnancy: by Amielia Mazwa Rafidah Obstetric and Gynecology DepartmentDocument43 pagesEctopic Pregnancy: by Amielia Mazwa Rafidah Obstetric and Gynecology DepartmentAlrick AsentistaNo ratings yet
- The B-Lynch Surgical Technique PDFDocument4 pagesThe B-Lynch Surgical Technique PDFRobertus HajaiNo ratings yet
- New Options for Managing Adherent PlacentaDocument6 pagesNew Options for Managing Adherent PlacentaAngelique Ramos PascuaNo ratings yet
- Everything You Need to Know About C-SectionsDocument46 pagesEverything You Need to Know About C-SectionsBugingo Julita100% (2)
- Cervical DystociaDocument22 pagesCervical DystociaBaldau TiwariNo ratings yet
- Common Gynecologic Procedures ExplainedDocument55 pagesCommon Gynecologic Procedures ExplainedQurrataini IbanezNo ratings yet
- Cervical IncompetenceDocument28 pagesCervical IncompetenceHoney May Rollan Vicente100% (1)
- Cervical IncompetenceDocument30 pagesCervical IncompetenceSignor ArasNo ratings yet
- Cesarean SectionDocument73 pagesCesarean Sectionkalsoom sahibzadaNo ratings yet
- Gynecological DisordersDocument26 pagesGynecological DisordersVijith.V.kumarNo ratings yet
- C Section 180515193200Document29 pagesC Section 180515193200Raluca HabaNo ratings yet
- Cesarean SectionDocument42 pagesCesarean SectionSyahirul Afifi100% (1)
- Circ LageDocument54 pagesCirc Lagetsega tilahunNo ratings yet
- C-Section Procedure GuideDocument4 pagesC-Section Procedure GuideKeanu ArcillaNo ratings yet
- Caserian SectionDocument100 pagesCaserian SectionsindhujojoNo ratings yet
- Cervical InsufficiecyDocument35 pagesCervical InsufficiecyWilliams Emmanuel AdeyeyeNo ratings yet
- Cesarean SectionDocument16 pagesCesarean SectionAbraham ChiuNo ratings yet
- Understanding miscarriage: causes, types, symptoms, and treatmentDocument38 pagesUnderstanding miscarriage: causes, types, symptoms, and treatmentzianab aliNo ratings yet
- Cesarean Section EditedDocument72 pagesCesarean Section EditedMohammad AlrefaiNo ratings yet
- Midwifery 102 Module 2aDocument18 pagesMidwifery 102 Module 2aWynjoy NebresNo ratings yet
- Caesarean section risks and indicationsDocument7 pagesCaesarean section risks and indicationsmark kennethNo ratings yet
- Dapus 4Document4 pagesDapus 4Ressy IrmaNo ratings yet
- Seminar On Complication of 3rd Stage PPHDocument13 pagesSeminar On Complication of 3rd Stage PPHjuhi labana0% (1)
- Chapter 24: Nursing Care of A Family During A Surgical Intervention For BirthDocument22 pagesChapter 24: Nursing Care of A Family During A Surgical Intervention For BirthAlyssaGrandeMontimorNo ratings yet
- Acute Non-Puerperal Uterine Inversion Case ReportDocument4 pagesAcute Non-Puerperal Uterine Inversion Case ReportALfuNo ratings yet
- Cesarean Delivery Techniques and RisksDocument27 pagesCesarean Delivery Techniques and RisksYared TJNo ratings yet
- Dr. Ahlam Al-Kharabsheh: Assistant Professor, OBS & GYN Department Mu'tah UniversityDocument36 pagesDr. Ahlam Al-Kharabsheh: Assistant Professor, OBS & GYN Department Mu'tah Universityraed faisalNo ratings yet
- Complications of PuerperiumDocument45 pagesComplications of PuerperiumsubashikNo ratings yet
- Caesarean SectionDocument22 pagesCaesarean SectionElsai EsbNo ratings yet
- Cervicval Shortening / Cervical Insufficiency: EtiologyDocument3 pagesCervicval Shortening / Cervical Insufficiency: EtiologyMiska RaihanaNo ratings yet
- Placenta Percreta and UrologistDocument4 pagesPlacenta Percreta and Urologistcb_cristianNo ratings yet
- CESAREAN SECTION BmsDocument25 pagesCESAREAN SECTION BmsAhemigisha JamesNo ratings yet
- Caesarean Section GuideDocument21 pagesCaesarean Section Guideshabir popalNo ratings yet
- Obstetri Dan Ginekologi 9a Partus TerlantarDocument20 pagesObstetri Dan Ginekologi 9a Partus Terlantar90Agva Dwi FatikaNo ratings yet
- Kehamilan Dengan Bekas Sectio Cecar: Disusun Oleh: Heru Maranata Nababan Pembimbing: Dr. Dr. Donel S, Spog (K)Document36 pagesKehamilan Dengan Bekas Sectio Cecar: Disusun Oleh: Heru Maranata Nababan Pembimbing: Dr. Dr. Donel S, Spog (K)Heru Maranata Nababan100% (1)
- Cs ObgDocument44 pagesCs ObghulwanvashaliNo ratings yet
- Complications of Third Stage of LabourDocument7 pagesComplications of Third Stage of LabourDeepaRamani100% (1)
- Cesarean SectionDocument42 pagesCesarean SectionP Kasikrishnaraja100% (1)
- Second Trimester MiscarriageDocument5 pagesSecond Trimester MiscarriageAmmarNo ratings yet
- Cesarean SectionDocument14 pagesCesarean Sectionمؤمن شطناويNo ratings yet
- Cesearean SectionDocument15 pagesCesearean SectionAbdurahman DarahemNo ratings yet
- 2 2017 03 26!08 03 00 PMDocument10 pages2 2017 03 26!08 03 00 PManakayamNo ratings yet
- Cesarean Section & Tubal Ligation SurgeryDocument16 pagesCesarean Section & Tubal Ligation SurgerySteffiNo ratings yet
- Nursing care for reproductive health issuesDocument100 pagesNursing care for reproductive health issuesHassen ZabalaNo ratings yet
- Inversion, Retained Placenta, AfeDocument95 pagesInversion, Retained Placenta, Afesushma sharmaNo ratings yet
- Sign 108Document108 pagesSign 108Pepo AryabarjaNo ratings yet
- 1756 0500 7 281 Libre PDFDocument7 pages1756 0500 7 281 Libre PDFPepo AryabarjaNo ratings yet
- VN-Brochure Aspirin OUSDocument2 pagesVN-Brochure Aspirin OUSPepo AryabarjaNo ratings yet
- Association of Aspirin Resistance With Increased Stroke Severity An..Document2 pagesAssociation of Aspirin Resistance With Increased Stroke Severity An..Pepo AryabarjaNo ratings yet
- 1756 0500 7 281 Libre PDFDocument7 pages1756 0500 7 281 Libre PDFPepo AryabarjaNo ratings yet
- Aspirin Resistance: Is It Real and Does It Matter?: DR - Wai-Hong ChenDocument3 pagesAspirin Resistance: Is It Real and Does It Matter?: DR - Wai-Hong ChenPepo AryabarjaNo ratings yet
- VN Pocketguide UsDocument8 pagesVN Pocketguide UsPepo AryabarjaNo ratings yet
- 14341D-InterpretingResults Aspirin TestDocument2 pages14341D-InterpretingResults Aspirin TestPepo AryabarjaNo ratings yet
- Stroke Prevention Algorithm-LoewenDocument1 pageStroke Prevention Algorithm-LoewenPepo AryabarjaNo ratings yet
- Drug Food InteractionsDocument8 pagesDrug Food InteractionsDecky Aditya ZNo ratings yet
- IELTS Handbook 2007Document22 pagesIELTS Handbook 2007srikwaits4u100% (15)
- Sectio Caesarea, Bedah Caesar, Operasi PersalinanDocument30 pagesSectio Caesarea, Bedah Caesar, Operasi PersalinanPepo AryabarjaNo ratings yet
- Sectio Caesarea, Bedah Caesar, Operasi PersalinanDocument19 pagesSectio Caesarea, Bedah Caesar, Operasi PersalinanPepo AryabarjaNo ratings yet
- Machine Design - LESSON 4. DESIGN FOR COMBINED LOADING & THEORIES OF FAILUREDocument5 pagesMachine Design - LESSON 4. DESIGN FOR COMBINED LOADING & THEORIES OF FAILURE9965399367No ratings yet
- Analysis of Trend Following SystemsDocument52 pagesAnalysis of Trend Following SystemsClement Li100% (1)
- GSM Multi-Mode Feature DescriptionDocument39 pagesGSM Multi-Mode Feature DescriptionDiyas KazhiyevNo ratings yet
- Funded African Tech Startups 2020Document13 pagesFunded African Tech Startups 2020LoNo ratings yet
- Department of Education: Republic of The PhilippinesDocument3 pagesDepartment of Education: Republic of The PhilippinesAdonis BesaNo ratings yet
- CCTV8 PDFDocument2 pagesCCTV8 PDFFelix John NuevaNo ratings yet
- STS Chapter 5Document2 pagesSTS Chapter 5Cristine Laluna92% (38)
- Liability WaiverDocument1 pageLiability WaiverTop Flight FitnessNo ratings yet
- Gigahertz company background and store locationsDocument1 pageGigahertz company background and store locationsjay BearNo ratings yet
- Libros de ConcretoDocument11 pagesLibros de ConcretoOSCAR GABRIEL MOSCOL JIBAJANo ratings yet
- Bolsas Transfer FKDocument7 pagesBolsas Transfer FKBelèn Caridad Nelly Pajuelo YaipènNo ratings yet
- VBScriptDocument120 pagesVBScriptdhanaji jondhaleNo ratings yet
- HSPA+ Compressed ModeDocument10 pagesHSPA+ Compressed ModeAkhtar KhanNo ratings yet
- BC Specialty Foods DirectoryDocument249 pagesBC Specialty Foods Directoryjcl_da_costa6894No ratings yet
- Capran+980 CM en PDFDocument1 pageCapran+980 CM en PDFtino taufiqul hafizhNo ratings yet
- Czar Alexander IIDocument11 pagesCzar Alexander IIMalachy ChinweokwuNo ratings yet
- Amended ComplaintDocument38 pagesAmended ComplaintDeadspinNo ratings yet
- Farmers InterviewDocument5 pagesFarmers Interviewjay jariwalaNo ratings yet
- Hillingdon Health Visiting ServiceDocument12 pagesHillingdon Health Visiting ServiceAnnikaNo ratings yet
- Lenex 3.0 Technical DocumentationDocument31 pagesLenex 3.0 Technical DocumentationGalina DNo ratings yet
- Storage Reservior and Balancing ReservoirDocument19 pagesStorage Reservior and Balancing ReservoirNeel Kurrey0% (1)
- Macdonald v. National City Bank of New YorkDocument6 pagesMacdonald v. National City Bank of New YorkSecret SecretNo ratings yet
- Forms of Business Organization: Sole Proprietorship, Partnership, Corporation, CooperativesDocument17 pagesForms of Business Organization: Sole Proprietorship, Partnership, Corporation, CooperativesSanti BuliachNo ratings yet
- Financial ManagementDocument21 pagesFinancial ManagementsumanNo ratings yet
- StrutsDocument7 pagesStrutsBatrisyialya RusliNo ratings yet
- KL Wellness City LIvewell 360 2023Document32 pagesKL Wellness City LIvewell 360 2023tan sietingNo ratings yet
- Denys Vuika - Electron Projects - Build Over 9 Cross-Platform Desktop Applications From Scratch-Packt Publishing (2019)Document429 pagesDenys Vuika - Electron Projects - Build Over 9 Cross-Platform Desktop Applications From Scratch-Packt Publishing (2019)Sarthak PrakashNo ratings yet
- IBM TS3500 Command Line Interface (CLI) ExamplesDocument6 pagesIBM TS3500 Command Line Interface (CLI) ExamplesMustafa BenmaghaNo ratings yet
- AssemblyinstructionsDocument12 pagesAssemblyinstructionsPriscila AzevedoNo ratings yet
- Safety of High-Rise BuildingsDocument14 pagesSafety of High-Rise BuildingsHananeel Sandhi100% (2)