Professional Documents
Culture Documents
Bone Is A Mineralized
Uploaded by
Zen Firhan ShahabOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bone Is A Mineralized
Uploaded by
Zen Firhan ShahabCopyright:
Available Formats
BONE IS A MINERALIZED CONNECTIVE TISSUE
Bone contains both organic and inorganic material. The organic matter is mainly protein. The principal proteins of bone are listed in Table 489; type I collagen is the major protein, comprising 9095% of the organic material. Type V collagen is also present in small amounts, as are a number of noncollagen proteins, some of which are relatively specific to bone. The inorganic or mineral component is mainly crystalline hydroxyapatiteCa10(PO4)6(OH)2along with sodium, magnesium, carbonate, and fluoride; approximately 99% of the bodys calcium is contained in bone (Chapter 45). Hydroxyapatite confers on bone the strength and resilience required by its physiologic roles. Bone is a dynamic structure that undergoes continuing cycles of remodeling, consisting of resorption followed by deposition of new bone tissue. This remodeling permits bone to adapt to both physical (eg, increases in weight-bearing) and hormonal signals. The major cell types involved in bone resorption and deposition are osteoclasts and osteoblasts (Figure 4811). The former are associated with resorption and the latter with deposition of bone. Osteocytes are descended from osteoblasts; they also appear to be involved in maintenance of bone matrix but will not be discussed further here. Osteoclasts are multinucleated cells derived from pluripotent hematopoietic stem cells. Osteoclasts possess an apical membrane domain, exhibiting a ruffled border that plays a key role in bone resorption (Figure 4812). A proton-translocating ATPase expels protons across the ruffled border into the resorption area, which is the microenvironment of low pH shown in the figure. This lowers the local pH to 4.0 or less, thus increasing the solubility of hydroxyapatite and allowing demineralization to occur. Lysosomal acid proteases are released that digest the now accessible matrix proteins.
Osteoblastsmononuclear cells derived from pluripotent mesenchymal precursorssynthesize most of the proteins found in bone (Table 489) as well as various growth factors and cytokines. They are responsible for the deposition of new bone matrix (osteoid) and its subsequent mineralization. Osteoblasts control mineralization by regulating the passage of calcium and phosphate ions across their surface membranes. The latter contain alkaline phosphatase, which is used to generate phosphate ions from organic phosphates. The mechanisms involved in mineralization are not fully understood, but several factors have been implicated. Alkaline phosphatase contributes to mineralization but in itself is not sufficient. Small vesicles (matrix vesicles) containing calcium and phosphate have been described at sites of mineralization, but their role is not clear. Type I collagen
appears to be necessary, with mineralization being first evident in the gaps between successive molecules. Recent interest has focused on acidic phosphoproteins, such as bone sialoprotein, acting as sites of nucleation. These proteins contain motifs (eg, poly-Asp and polyGlu stretches) that bind calcium and may provide an initial scaffold for mineralization. Some macromolecules, such as certain proteoglycans and glycoproteins, can also act as inhibitors of nucleation. It is estimated that approximately 4% of compact bone is renewed annually in the typical healthy adult, whereas approximately 20% of trabecular bone is replaced. Many factors are involved in the regulation of bone metabolism, only a few of which will be mentioned here. Some stimulate osteoblasts (eg, parathyroid hormone and 1,25-dihydroxycholecalciferol) and others inhibit them (eg, corticosteroids). Parathyroid hormone and 1,25-dihydroxycholecalciferol also stimulate osteoclasts, whereas calcitonin and estrogens inhibit them.
You might also like
- The Musculoskeletal SystemDocument56 pagesThe Musculoskeletal SystemMaria Dini AdmiratiNo ratings yet
- Physiology of BoneDocument22 pagesPhysiology of BoneKhairaFirselNo ratings yet
- Calcium Homeostasis and Osteoporosis - McMaster Pathophysiology ReviewDocument8 pagesCalcium Homeostasis and Osteoporosis - McMaster Pathophysiology ReviewEzayu AzeraNo ratings yet
- Bone Metabolism: German VersionDocument17 pagesBone Metabolism: German VersionDapot SianiparNo ratings yet
- Physiologic Processes in The Skeletal SystemDocument6 pagesPhysiologic Processes in The Skeletal SystemAry Romeo ShakespeareNo ratings yet
- Bone and Cartilage PDFDocument50 pagesBone and Cartilage PDFalviraNo ratings yet
- Bone and Mineral Metabolism in Health and DiseaseDocument14 pagesBone and Mineral Metabolism in Health and Diseasebiniam MesfinNo ratings yet
- Agents That Affect Bone Mineral Homeostasis: Department of PharmacologyDocument44 pagesAgents That Affect Bone Mineral Homeostasis: Department of Pharmacologymichaelcyl100% (1)
- Musculoskeltal SystemDocument18 pagesMusculoskeltal Systemhy7tnNo ratings yet
- Bone MarkersDocument31 pagesBone MarkersJetGoliath 26No ratings yet
- Kalsifikasi, Deposisi Dan Resorpsi TulangDocument40 pagesKalsifikasi, Deposisi Dan Resorpsi TulangrifkaNo ratings yet
- Bone BiochemistryDocument21 pagesBone BiochemistrySheilasmNo ratings yet
- AN OVERVIEW OF BONE CELLS AND THEIR REGULATING FACTORS OF DIFFERENTIATION, Mohamed 2008Document9 pagesAN OVERVIEW OF BONE CELLS AND THEIR REGULATING FACTORS OF DIFFERENTIATION, Mohamed 2008Faizal Reza PahleviNo ratings yet
- Lec 1516 Bone Tissue and Skeletal SystemDocument28 pagesLec 1516 Bone Tissue and Skeletal SystemonegaonnweNo ratings yet
- Review Article: Mechanisms of Bone Resorption in PeriodontitisDocument11 pagesReview Article: Mechanisms of Bone Resorption in PeriodontitisBetrik Sefyana MangiriNo ratings yet
- Bone ResorptionDocument10 pagesBone ResorptionVibhor PradhanNo ratings yet
- DR Naveed Seminar PPT 2Document60 pagesDR Naveed Seminar PPT 2mohammad abdul naveedNo ratings yet
- Bone Ash Estimation of Content of Bone Ash Project Submitted by PrashanthDocument3 pagesBone Ash Estimation of Content of Bone Ash Project Submitted by PrashanthHarsh Kumar0% (3)
- Alveolar Bone: and It's Associated PathologiesDocument7 pagesAlveolar Bone: and It's Associated Pathologiesمحمد العراقيNo ratings yet
- Disorders Associated With Bone Mineral ImbalanceDocument4 pagesDisorders Associated With Bone Mineral ImbalanceKarla Erika SugimotoNo ratings yet
- Bone Formation: Hypothalamic Hormone, CRH, and The Pituitary Hormone, ACTHDocument3 pagesBone Formation: Hypothalamic Hormone, CRH, and The Pituitary Hormone, ACTHSimon AvilaNo ratings yet
- Bone Remodeling: Prepa Red B Y: Divin E Mac Aran AS 2-8-2 017Document60 pagesBone Remodeling: Prepa Red B Y: Divin E Mac Aran AS 2-8-2 017Divine Macaranas CordovizNo ratings yet
- MSK NotesDocument83 pagesMSK NotesabdulNo ratings yet
- Maxillary Sinus Bone GraftingDocument181 pagesMaxillary Sinus Bone GraftingTuấn Hành TrầnNo ratings yet
- Chemistry Project On Estimation of Content of Bone AshDocument18 pagesChemistry Project On Estimation of Content of Bone AshKim TaesiNo ratings yet
- Chemistry Project On Estimation of Content of Bone AshDocument13 pagesChemistry Project On Estimation of Content of Bone AshShlok Sah50% (2)
- Kenkre Bassett 2018 The Bone Remodelling CycleDocument20 pagesKenkre Bassett 2018 The Bone Remodelling Cyclealealer2708No ratings yet
- Fisiologi Molekuler TulangDocument42 pagesFisiologi Molekuler TulangKhairaFirselNo ratings yet
- Bone FinalDocument25 pagesBone Finalcelestina dawn peterNo ratings yet
- Maxilary Sinus Graft ArunDocument181 pagesMaxilary Sinus Graft ArunJose Fernando Fragozo MendozaNo ratings yet
- We Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsDocument19 pagesWe Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsJade LolongNo ratings yet
- Bone Basic Science: Presenter: DR Nshimiyimana Alexis Orthopedic Resident-UrDocument36 pagesBone Basic Science: Presenter: DR Nshimiyimana Alexis Orthopedic Resident-UrNshimiyimana AlexisNo ratings yet
- Calcium and Phosphate Homeostasis - Endotext - NCBI BookshelfDocument32 pagesCalcium and Phosphate Homeostasis - Endotext - NCBI BookshelfdrvancedNo ratings yet
- Miapoly Calcium in AnimalDocument8 pagesMiapoly Calcium in AnimalDev jibreenNo ratings yet
- Cellular and Molecular Mechanisms of Bone RemodelingDocument9 pagesCellular and Molecular Mechanisms of Bone RemodelingDwi Rizky LestariNo ratings yet
- Basic Avian Bone Growth and HealingDocument8 pagesBasic Avian Bone Growth and HealingIban HernándezNo ratings yet
- Biokimia Tulang Dms Block - Nop.2013Document59 pagesBiokimia Tulang Dms Block - Nop.2013yandaputriNo ratings yet
- Alveolar Bone FFDocument105 pagesAlveolar Bone FFshashi kant chaudharyNo ratings yet
- jkms-25-985 OSTEOCALCININDocument7 pagesjkms-25-985 OSTEOCALCININVerónica Serrato QuezadaNo ratings yet
- Formation: Blood Calcium Level - Calcium HydroxyapatiteDocument13 pagesFormation: Blood Calcium Level - Calcium HydroxyapatiteClarissa IsuriñaNo ratings yet
- Anaphy C7 Oral Rec.Document3 pagesAnaphy C7 Oral Rec.Katrina ParbaNo ratings yet
- Bone Structure: OsteoblastsDocument4 pagesBone Structure: OsteoblastsamlniNo ratings yet
- Osteoblast: osteo-and βλαστάνω, blastanō "germinate") are cells with a singleDocument10 pagesOsteoblast: osteo-and βλαστάνω, blastanō "germinate") are cells with a singleAlan FosterNo ratings yet
- This Article Is About The Skeletal Organ. For Other Uses, See and - For The Tissue, SeeDocument17 pagesThis Article Is About The Skeletal Organ. For Other Uses, See and - For The Tissue, SeeSadaf FatimaNo ratings yet
- Physiology of BoneDocument32 pagesPhysiology of BoneAnandhu GNo ratings yet
- Bone Remodeling: Vitamin A Vitamin C Vitamin D Vitamins K and B The Insulin-Like Growth Factors (Igfs)Document2 pagesBone Remodeling: Vitamin A Vitamin C Vitamin D Vitamins K and B The Insulin-Like Growth Factors (Igfs)Lainie ZefiahNo ratings yet
- Pengaruh Penambahan Platelet-Rich Plasma Pada Cangkok Tulang Terhadap Kadar Osteocalcin Cairan Sulkus Gingiva Pada Terapi Poket InfraboniDocument8 pagesPengaruh Penambahan Platelet-Rich Plasma Pada Cangkok Tulang Terhadap Kadar Osteocalcin Cairan Sulkus Gingiva Pada Terapi Poket InfraboniMogu NobyNo ratings yet
- Role of RANKL-RANK-osteoprotegerinDocument7 pagesRole of RANKL-RANK-osteoprotegerinsebastian BarrigaNo ratings yet
- Bone Cells and Applied AnatomyDocument48 pagesBone Cells and Applied Anatomynams orthoNo ratings yet
- Chapter 23: Osteoporosis of The SpineDocument15 pagesChapter 23: Osteoporosis of The SpineTraian UrsuNo ratings yet
- Nihms-1641529 Mechanisms of Bone Development and RepairDocument41 pagesNihms-1641529 Mechanisms of Bone Development and Repairhennysusanto18No ratings yet
- 7 CalciumDocument83 pages7 Calciumtmqt2fbnzgNo ratings yet
- Department of Periodontics and Implantology: Calcium MetabolismDocument63 pagesDepartment of Periodontics and Implantology: Calcium Metabolismrasagna reddy100% (1)
- Osteocrin, A Novel Bone-Specific Secreted Protein That Modulates The Osteoblast PhenotypeDocument10 pagesOsteocrin, A Novel Bone-Specific Secreted Protein That Modulates The Osteoblast PhenotypeRuth Esperanza RodriguezNo ratings yet
- Bone Changes During Orthodontic TreatmentDocument39 pagesBone Changes During Orthodontic TreatmentDENTALORG.COMNo ratings yet
- OsteoclastsDocument9 pagesOsteoclastszwetzaNo ratings yet
- DN - AJ Metabolisme Tulang Dan SendiDocument46 pagesDN - AJ Metabolisme Tulang Dan SendiJohn Felix SitumorangNo ratings yet
- Bone Grafts and Their SubstitutesDocument4 pagesBone Grafts and Their SubstitutesIndriastuti SoetomoNo ratings yet
- Bone Remodeling Process: Mechanics, Biology, and Numerical ModelingFrom EverandBone Remodeling Process: Mechanics, Biology, and Numerical ModelingNo ratings yet
- Fraktur Collum Femur Dengan AustinDocument3 pagesFraktur Collum Femur Dengan AustinZen Firhan ShahabNo ratings yet
- Data Rekon WordDocument3 pagesData Rekon WordZen Firhan ShahabNo ratings yet
- Blount DiseaseDocument1 pageBlount DiseaseZen Firhan ShahabNo ratings yet
- QuotesDocument48 pagesQuotesParitosh MunotNo ratings yet
- Avery Dennison TemplateDocument1 pageAvery Dennison TemplateZen Firhan ShahabNo ratings yet
- Mayo Wrist Score: Please Answer The Following 12 Multiple Choice QuestionsDocument1 pageMayo Wrist Score: Please Answer The Following 12 Multiple Choice QuestionsZen Firhan ShahabNo ratings yet
- QuotesDocument48 pagesQuotesParitosh MunotNo ratings yet
- Tendon Transfers Are Done To Restore A Function That Has Been LostDocument4 pagesTendon Transfers Are Done To Restore A Function That Has Been LostZen Firhan ShahabNo ratings yet
- Glasgow Coma Scale Zen2Document7 pagesGlasgow Coma Scale Zen2Zen Firhan ShahabNo ratings yet
- Glasgow Coma Scale Zen2Document7 pagesGlasgow Coma Scale Zen2Zen Firhan ShahabNo ratings yet
- Principles of Tendon TransferDocument1 pagePrinciples of Tendon TransferZen Firhan ShahabNo ratings yet
- Bone Is A MineralizedDocument2 pagesBone Is A MineralizedZen Firhan ShahabNo ratings yet
- Collagen Types FullDocument3 pagesCollagen Types FullZen Firhan ShahabNo ratings yet
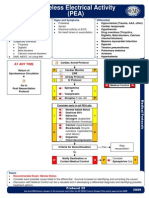
- Pro29 PulselessElectricalActivityDocument1 pagePro29 PulselessElectricalActivityZen Firhan ShahabNo ratings yet
- Bowel RetrainingDocument5 pagesBowel RetrainingZen Firhan ShahabNo ratings yet
- Rna 10 924Document10 pagesRna 10 924Jyoti ChaturvediNo ratings yet
- Fatima Laureano-Maravilla - Unit 3 - Photosynthesis ch8Document6 pagesFatima Laureano-Maravilla - Unit 3 - Photosynthesis ch8api-542684299No ratings yet
- 2 Boore - The Human CellDocument27 pages2 Boore - The Human Cellمحمد العراقيNo ratings yet
- Bio Chapter 1 To 5Document23 pagesBio Chapter 1 To 5QASIM jamilNo ratings yet
- RBT Tissue CultureDocument49 pagesRBT Tissue CultureH.M. AriyanNo ratings yet
- Cell CycleDocument16 pagesCell CycleRose RomeroNo ratings yet
- Sesquiterpene Lactones - Structural Diversity and Their Biological ActivitiesDocument22 pagesSesquiterpene Lactones - Structural Diversity and Their Biological ActivitiesAri Puji AstutiNo ratings yet
- MTT AssayDocument12 pagesMTT AssaySurampalliGuruNo ratings yet
- Cell, Basic Structure of All Living Creatures: Life Science, Human BiologyDocument11 pagesCell, Basic Structure of All Living Creatures: Life Science, Human BiologyAshleigh Jenson WilliamsonNo ratings yet
- HKDSE Biology S5 Exam (2020)Document28 pagesHKDSE Biology S5 Exam (2020)FuchingAuntie100% (1)
- Stem Cells and The Skin - Dahl2012Document10 pagesStem Cells and The Skin - Dahl2012ranasoftNo ratings yet
- Bio 322 Assignment 2Document1 pageBio 322 Assignment 2Gopika SureshNo ratings yet
- Ajpgi 00008 2022Document18 pagesAjpgi 00008 2022Jéssica Thandara GosseNo ratings yet
- Chapter 9 Active Reading Guide The Cell Cycle: Key Role ExampleDocument7 pagesChapter 9 Active Reading Guide The Cell Cycle: Key Role ExampleAulia RahmawatiNo ratings yet
- NMAT Review 2018 Module - BiologyDocument34 pagesNMAT Review 2018 Module - BiologyRaf Lin DrawsNo ratings yet
- F Plasmids PDFDocument2 pagesF Plasmids PDFNickNo ratings yet
- Hasil Praktikum Sds-PageDocument30 pagesHasil Praktikum Sds-Page09680017No ratings yet
- Khan 2014Document11 pagesKhan 2014Hidayat Jamalul INo ratings yet
- CDGM StudentWSDocument4 pagesCDGM StudentWSJana Al-DossariNo ratings yet
- Mark Scheme (FINAL) Summer 2007: GCE Biology SNAB (6131/01)Document11 pagesMark Scheme (FINAL) Summer 2007: GCE Biology SNAB (6131/01)Rayyan BariNo ratings yet
- Pglo Powerpoint 1Document24 pagesPglo Powerpoint 1api-358681703No ratings yet
- PHP2018Document25 pagesPHP2018radu nicolaeNo ratings yet
- Fonc 13 1226289Document19 pagesFonc 13 1226289Shady tantawyNo ratings yet
- Sheet PDFDocument316 pagesSheet PDFMarina WorldNo ratings yet
- Exercise 6. Analysis of Milk Proteins Using SDS-PAGEDocument6 pagesExercise 6. Analysis of Milk Proteins Using SDS-PAGELance LanceNo ratings yet
- Post Lab Fatty AcidsDocument2 pagesPost Lab Fatty AcidsBeverly DatuNo ratings yet
- Protein ExperimentDocument25 pagesProtein ExperimentYulinar Fawanys100% (1)
- Mesotherapy by Institute BCN EnesfrDocument32 pagesMesotherapy by Institute BCN Enesfrmarketing4558No ratings yet
- Cell CrosswordDocument2 pagesCell CrosswordLycanAlfaNo ratings yet
- A TextBook of Inorganic ChemistryDocument510 pagesA TextBook of Inorganic Chemistrytili_secara127No ratings yet