Professional Documents
Culture Documents
Treatment Algorithm of Malaria
Uploaded by
Jen Chan Pui SheonCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Treatment Algorithm of Malaria
Uploaded by
Jen Chan Pui SheonCopyright:
Available Formats
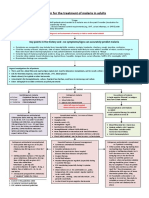
History of travel to malaria-endemic area or clinical suspicion of malaria
Perform thick and thin blood films and read within a few hours
No
Blood film positive?
Yes
Repeat blood films every 12 to 24 h for a total of 3 sets No Blood film positive? Yes
Calculate parasitemia Evaluate clinical status and disease severity
Consider alternate diagnoses
Uncomplicated malaria Determine species
Severe malaria and/or Patient unable to take oral medication
Non-falciparum species
Plasmodium falciparum or
species not yet identified
P. malariae
acquired outside Papua New Guinea or Indonesia
P. ovale or P. vivax
P. vivax acquired in
Papua New Guinea or Indonesia
P. knowlesi
Acquired in chloroquine- Acquired in chloroquine- Acquired in mefloquinesensitive area resistant area resistant area
Chloroquine or Hydroxychloroquine Atovaquone-proguanil or Artemether-lumefantrine or Quinine plus tetracycline or doxycycline or clindamycin or Mefloquine
Chloroquine or Hydroxychloroquine Chloroquine or Hydroxychloroquine
Atovaquone-proguanil or Quinine plus tetracycline or doxycycline or Mefloquine
Atovaquone-proguanil or Artemether-lumefantrine or Quinine plus tetracycline or doxycycline or clindamycin Intravenous quinidine plus tetracycline, or doxycycline, or clindamycin If quinidine is unavailable contact CDC malaria hotline for artesunate Admit to intensive care unit for continuous cardiac monitoring. Prevent and treat complications. Consider exchange transfusion if parasitemia is >10% or if patient has an altered mental status, ARDS, or renal failure Switch to oral medicines to complete the treatment regimen after appropriate clinical response
Plus
Primaquine if not G6PD deficient
Admit to hospital to monitor for progression of disease severity
Repeat blood films if symptoms recur
You might also like
- USMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsFrom EverandUSMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsRating: 5 out of 5 stars5/5 (9)
- Plasmodium Falciparum: or orDocument1 pagePlasmodium Falciparum: or orRaluca LupuNo ratings yet
- P. Malariae and P. Knowlesi: Knowlesi Species Therefore, Chloroquine (Or Hydroxychloroquine) May Still Be Used For BothDocument9 pagesP. Malariae and P. Knowlesi: Knowlesi Species Therefore, Chloroquine (Or Hydroxychloroquine) May Still Be Used For BothAmirul AdilNo ratings yet
- CDC Malaria Hotline: (770) 488-7788 or (855) 856-4713 (Toll-Free) Monday-Friday 9am-5pm EST (770) 488-7100 After Hours, Weekends, and HolidaysDocument1 pageCDC Malaria Hotline: (770) 488-7788 or (855) 856-4713 (Toll-Free) Monday-Friday 9am-5pm EST (770) 488-7100 After Hours, Weekends, and HolidaysRaden febrian Dwi cahyoNo ratings yet
- Algorithm PDFDocument1 pageAlgorithm PDFjosua koirewaNo ratings yet
- Mona Abd El Fattah Ahmed Ain Shams University Egyptking Abdullah Medical City Saudi ArabiaDocument23 pagesMona Abd El Fattah Ahmed Ain Shams University Egyptking Abdullah Medical City Saudi ArabiaVandana GoelNo ratings yet
- Malaria Treatment Protocol: Third EditionDocument32 pagesMalaria Treatment Protocol: Third Editionrizqi_cepiNo ratings yet
- Uncomplicated Malaria: Malaria: Standard Case Definitions: Suspected CaseDocument4 pagesUncomplicated Malaria: Malaria: Standard Case Definitions: Suspected CasejamshaidjiNo ratings yet
- Malaria Managment Algorithm 202208Document1 pageMalaria Managment Algorithm 202208Marianne Joy PontigonNo ratings yet
- Malaria Management AlgorithmDocument1 pageMalaria Management AlgorithmAdriel SebastianNo ratings yet
- Malaria Treatment Bis 07Document11 pagesMalaria Treatment Bis 07braggsNo ratings yet
- MalariaDocument30 pagesMalariaRevan NasirNo ratings yet
- Susceptibility of Plasmodium Falciparum Different of Quinine in Vivo and Quinine Quinidine Relation Chloroquine LiberiaDocument7 pagesSusceptibility of Plasmodium Falciparum Different of Quinine in Vivo and Quinine Quinidine Relation Chloroquine LiberiaderekwwillisNo ratings yet
- SEI - INEP - 0137469 - Projeto BásicoDocument29 pagesSEI - INEP - 0137469 - Projeto BásicoMARLOMbran HERRNo ratings yet
- PARAGONIMIASISDocument21 pagesPARAGONIMIASISaNo ratings yet
- Antiprotozoal Drugs: Halia Wanadiatri, DR., M.SiDocument34 pagesAntiprotozoal Drugs: Halia Wanadiatri, DR., M.SiBaiqLinaAnggrianNo ratings yet
- Septic Shock Update 2020Document41 pagesSeptic Shock Update 2020Dr AhmedNo ratings yet
- Malaria Case Studies: Disclosure of Potential Conflict of InterestDocument30 pagesMalaria Case Studies: Disclosure of Potential Conflict of InterestVandana GoelNo ratings yet
- Exmen P3 TropiDocument14 pagesExmen P3 TropiAndrew AvilaNo ratings yet
- Malaria PocketcardDocument2 pagesMalaria PocketcardYudha fedrian AKNo ratings yet
- Lascano, Joanne Alyssa H. - Parasitology SGDDocument8 pagesLascano, Joanne Alyssa H. - Parasitology SGDJoanne Alyssa Hernandez LascanoNo ratings yet
- Journal Malaria VivaxDocument3 pagesJournal Malaria VivaxPutri PertiwiNo ratings yet
- Diagnosis PreeclampsiaDocument13 pagesDiagnosis Preeclampsiabipbip bipNo ratings yet
- Malaria NotesDocument3 pagesMalaria NotesAbynarh PinaNo ratings yet
- Treatment Table MalariaDocument3 pagesTreatment Table MalariaFauziah Husnu ShofiahNo ratings yet
- Management of MalariaDocument55 pagesManagement of MalariaAnu SinhaNo ratings yet
- MALARIADocument8 pagesMALARIAMohmmadRjab SederNo ratings yet
- Lecture-4 Viral GastroenteritisDocument37 pagesLecture-4 Viral GastroenteritislolitlolatNo ratings yet
- In Vitro Efficacy of Antimalarial Drugs Against Plasmodium VivaxDocument3 pagesIn Vitro Efficacy of Antimalarial Drugs Against Plasmodium VivaxSidharth KhannaNo ratings yet
- Comparison of Clinical Profile Between Plasmodium Vivax andDocument6 pagesComparison of Clinical Profile Between Plasmodium Vivax andellasianturiNo ratings yet
- Uncomplicated Malaria and TreatmentDocument44 pagesUncomplicated Malaria and TreatmentSisilia AlfinaNo ratings yet
- Empyema CPGDocument8 pagesEmpyema CPGLe Vu AnhNo ratings yet
- Community Acquired PneumoniaDocument37 pagesCommunity Acquired PneumoniaJoean CabarlocNo ratings yet
- NACH-1554 UTI Practice Tool - jr6Document2 pagesNACH-1554 UTI Practice Tool - jr6minipredatorNo ratings yet
- Elsye Gunawan: Farmakoterapi Pada Pasien MalariaDocument47 pagesElsye Gunawan: Farmakoterapi Pada Pasien MalariaEnvhy WinaNo ratings yet
- 1 - Uncomplicated Malaria and TreatmentDocument35 pages1 - Uncomplicated Malaria and Treatmentstivana26No ratings yet
- Algorithm For The Treatment of Malaria in AdultsDocument1 pageAlgorithm For The Treatment of Malaria in AdultsRihab IsmaeelNo ratings yet
- Gastro 1Document1 pageGastro 1Adolf HitlerNo ratings yet
- Typhoid GuidelinesDocument3 pagesTyphoid GuidelinesMuthia Rahma AninditaNo ratings yet
- Pediatric Malaria Treatment & Management: Approach Considerations, Intensive Care, Deterrence and PreventionDocument4 pagesPediatric Malaria Treatment & Management: Approach Considerations, Intensive Care, Deterrence and PreventionVivi DeviyanaNo ratings yet
- Protozoans-2 0Document34 pagesProtozoans-2 0ArllrNo ratings yet
- Fever Online SessionDocument51 pagesFever Online SessionPrecious ChaiNo ratings yet
- Medicin Protozoal Diseases (Part 2)Document6 pagesMedicin Protozoal Diseases (Part 2)زين العابدين محمد عويش مشريNo ratings yet
- CDC - Paragonimiasis - Resources For Health ProfessionalsDocument3 pagesCDC - Paragonimiasis - Resources For Health ProfessionalsKevin GarciaNo ratings yet
- Antimalarial DrugsDocument33 pagesAntimalarial DrugsPinakin Dhirajlal Jadav100% (1)
- Infectious QuestionDocument52 pagesInfectious Questionrayooona88No ratings yet
- Fetal Therapy: Hyaline Membrane DiseaseDocument5 pagesFetal Therapy: Hyaline Membrane DiseaseDelphy VargheseNo ratings yet
- Dextrose Saline Compared With Normal Saline.13Document8 pagesDextrose Saline Compared With Normal Saline.13Cynthia Z.No ratings yet
- Study of Clinical Etiological and Radiological Profile of UTI CasesDocument8 pagesStudy of Clinical Etiological and Radiological Profile of UTI CasesDebabrata MohapatraNo ratings yet
- Pulmonary InfectionsDocument16 pagesPulmonary InfectionsFawad AhmedNo ratings yet
- Communicable Diseases: Roberto M. Salvador Jr. R.N.,M.D. Infectious and Tropical Disease SpecialistDocument846 pagesCommunicable Diseases: Roberto M. Salvador Jr. R.N.,M.D. Infectious and Tropical Disease SpecialistGrn Mynjrkxz100% (1)
- The Prevention and Treatment of Plasmodium: Vivax MalariaDocument21 pagesThe Prevention and Treatment of Plasmodium: Vivax MalariaDoaa SaifNo ratings yet
- Pugud Samodro Bag/SMF Ilmu Penyakit Dalam FKIK Unsoed/ RSUD ProfDocument68 pagesPugud Samodro Bag/SMF Ilmu Penyakit Dalam FKIK Unsoed/ RSUD ProfpugudNo ratings yet
- 8 - MalariaDocument21 pages8 - MalariaCAÑADA, JOHANNELYN M.No ratings yet
- Cefdinir Double Dose - PIDJDocument8 pagesCefdinir Double Dose - PIDJAhmad TharwatNo ratings yet
- Fan 2014Document7 pagesFan 2014farisNo ratings yet
- Typhoid FeverDocument23 pagesTyphoid FeverAs ShahirahNo ratings yet
- Paediatric HivDocument8 pagesPaediatric Hivian ismailNo ratings yet