Professional Documents
Culture Documents
First Moscow State Medical University
First Moscow State Medical University
Uploaded by
Mardiana KamalOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
First Moscow State Medical University
First Moscow State Medical University
Uploaded by
Mardiana KamalCopyright:
Available Formats
First Moscow State Medical University
MEDICAL FACULTY Division of Foreign Students with Instruction Conducted in English
Department of Infectious Diseases
Hemorrhagic Fevers
By Mardiana Kamal Medical Faculty, English Medium, Group 93
MOSCOW 2013
Viral Hemorrhagic Fevers
The viral hemorrhagic fevers (VHFs) are a diverse group of animal and human illnesses that may be caused by five distinct families of RNA viruses: the families Arenaviridae, Filoviridae, Bunyaviridae, Flaviviridae, and Rhabdoviridae. All types of VHF are characterized by fever and bleeding disorders and all can progress to high fever, shock and death in many cases. Some of the VHF agents cause relatively mild illnesses, such as the Scandinavian nephropathia epidemica, while others, such as the African Ebola virus, can cause severe, life-threatening disease. Acute infection: fever, myalgia, malaise; progression to prostration Small vessel involvement: increased permeability, cellular damage Multisystem compromise (varies with pathogen) Hemorrhage may be small in volume : (indicates small vessel involvement, thrombocytopenia) Poor prognosis associated with: shock, encephalopathy, extensive hemorrhage
VHF : Potential for aerosol dissemination, with human infection via respiratory route (except dengue) Target organ: vascular bed Mortality 0.5 - 90%, depending on agent
Differential Diagnosis Febrile tropical illnesses: Malaria Typhoid fever Bacterial gastro-enteritis Rickettsial diseases
Etiologic agents Five families of RNA viruses have been recognised as being able to cause this syndrome. They share certain clinical and pathogenic features. The family Arenaviridae include the viruses responsible for o Lassa fever, o Lujo virus o Argentine, Bolivian, Brazilian and Venezuelan hemorrhagic fevers. The family Bunyaviridae include o Hemorrhagic fever with renal syndrome (HFRS) by members of the Hantavirus genus o Crimean-Congo hemorrhagic fever (CCHF) virus from the Nairovirus genus o Garissa virus from the Orthobunyavirus o Rift Valley fever (RVF) virus from the Phlebovirus genus. The family Filoviridae include o Ebola virus o Marburg virus. The family Flaviviridae include
o o o
dengue yellow fever two viruses in the tick-borne encephalitis group that cause VHF: Omsk hemorrhagic fever virus Kyasanur Forest diseasevirus.
Category A agents Filoviruses Arenaviruses
Category C agents Hantaviruses Tick-borne hemorrhagic fever viruses Yellow fever
Transmission Zoonotic diseases Rodents and arthropods main reservoir Humans infected via bite of infected arthropod, inhalation of rodent excreta, or contact with infected animal carcasses Person-to-person transmission possible with several agents Primarily via blood or bodily fluid exposure Rare instances of airborne transmission with arenaviruses and filoviruses Rift Valley fever has potential to infect domestic animals following a biological attack
Summary of Agents
Virus Family
Virus/Syndrome
Geographic occurrence
Reservoir or Vector Rodents
Human-human transmission? Lassa Fever yes, via body fluids; others not usually
Arenaviridae
Junin (Argentine HF) Machupo (Bolivian HF) Guanarito (Brazilian HF) Sabia (Venezuelan HF) Lassa (Lassa Fever)
S.America S.America S.America S.America West Africa Tropical Africa,Latin America Tropical areas India Siberia Geographic occurrence
Flaviridae
Yellow Fever
Mosquitoes
Dengue Fever Kyanasur Forest Disease Omsk HF Virus Family Virus/Syndrome
Yellow Fever blood infective up to 5d of illness; Others - No
Ticks
Reservoir or Vector Ticks Mosquitoes
Human-human transmission?
Congo-Crimean HF
Crimea, parts of Africa, Europe & Asia Africa Diverse
Rift Valley Fever Bunyaviridae Hantaviruses (Hemorrhagic Renal Syndrome/ Hantavirus Pulmonary Syndrome) Ebola HF Filoviridae Marburg HF
Rodents
Congo-Crimean Hemorrhagic Fever yes, through body fluids; Rift Valley Fever, Hantaviruses no
Africa Unknown Africa
Yes, body fluid transmission
Clinical Presentation Clinical manifestations nonspecific, vary by agent Incubation period 2-21 days, depending on agent Onset typically abrupt with filoviruses, flaviviruses, and Rift Valley fever Onset more insidious with arenaviruses
Not all infected persons develop a classic hemorrhagic fever syndrome, and specific signs and symptoms vary according to the specific type of VHF. Initial signs and symptoms may include marked fever, fatigue, dizziness, muscle aches, weakness, and exhaustion. Severe cases may show bleeding manifestations ranging from petechiae to spontaneous bleeding. Infection control measures for protection of health care workers should be implemented for suspected VHF cases. The different VHF agents produce a spectrum of symptoms and clinical manifestations, complicating diagnosis. The incubation period for the viral hemorrhagic fevers ranges from 2-21 days, depending on the agent, and is followed by a prodromal illness lasting less than a week. Initial symptoms (slide 25) may include high fever, headache, malaise, joint or muscle aches, weakness, exhaustion, dizziness, nausea, abdominal pain, and non-bloody diarrhea. Illness onset is typically abrupt for the filoviruses, flaviviruses and Rift Valley fever; and more insidious with the arenaviruses. Incubation periods for specific agents: South American hemorrhagic fevers (arenaviruses): Lassa Fever: Ebola viral disease: Marburg viral disease: Hemorrhagic Fever with Renal Syndrome (hantavirus): Hantavirus Pulmonary Syndrome: Yellow Fever: Congo-Crimean Hemorrhagic Fever: Dengue Fever: Rift Valley Fever:
7-16 days 6-21 days 2-21 days 3-9 days usually 2-4 weeks (range=few days 2 months) ~2 weeks (range=few days 6 weeks) 3-6 days 1-12 days 3-14 days 3-12 days
Initial Symptoms Prodromal illness lasting < 1 week may include: High fever Headache Malaise Weakness Exhaustion Dizziness Muscle aches Joint pain Nausea Non-bloody diarrhea
Clinical Signs Flushing, conjunctival injection (red eye) Pharyngitis Rash
Edema Hypotension Shock Mucous membrane bleeding
Clinical Identification of Suspected Cases (Adapted from WHO) Clinical criteria: Temperature 101 F(38.3 C) for <3 weeks Severe illness and no predisposing factors for hemorrhagic manifestations 2 or more of the following: Hemorrhagic or purple Blood in stools rash Other hemorrhagic Epistaxis symptoms Hematemesis No established Hemoptysis alternative diagnosis
Laboratory Diagnosis Malaria smears Blood cultures (closed system) CBC, especially platelet count Transaminases (prognostic value) Treatment Supportive care Rule out or treat febrile illnesses: malaria, rickettsia, leptospirosis, typhoid, dysentery Early hospitalization Distant medical evacuation associated with high mortality Cautious sedation and analgesia Careful hydration Pressors, cardiotonic drugs Support of coagulation system Correct coagulopathies as needed No antiplatelet drugs or IM injections Investigational treatments, available under protocol: Ribavirin x 10 days for arenaviridae and bunyaviridae Convalescent plasma w/in 8d of onset for AHF
Management of Exposed Persons Patients convalescing should refrain from sexual activity for 3 months post-recovery (arenavirus or filovirus infection) Only licensed vaccine: Yellow Fever Investigational vaccines: AHF, RV, HV Possible use of ribavirin to high-risk contacts of CCHF and LF patients Some VHF viruses may continue to be present in body fluids for long periods following recovery. Patients recovering from an arenavirus or filovirus infection should therefore refrain from sexual activity for three months after clinical recovery. Yellow fever is the only VHF with a licensed vaccine. Yellow fever antibodies take longer than the three- to six-day incubation period to appear, and thus this vaccine would not be useful for prophylaxis during a biological attack. There is limited experimental evidence that postexposure prophylaxis with ribavirin will delay onset of disease from arenaviruses, but not prevent it. The Department of Defense has a compassionate use protocol for prophylactic administration of oral ribavirin to high risk contacts of Congo-Crimean hemorrhagic fever patients, and CDC guidelines recommend ribavirin to high-risk contacts of Lassa fever patients. The latter recommendations will be undergoing a review shortly, and may be revised. The Civilian Working Group for Biodefense does not recommend the administration of ribavirin to exposed individuals in the absence of signs or symptoms.
Infection Control Airborne & contact precautions for health care, environmental, and laboratory workers Negative pressure room, if available 6-12 air changes/hour Exhausted outdoors or through HEPA filter Personal protective equipment Double gloves Impermeable gowns, leg and shoe coverings Face shields and eye protection N-95 mask or PAPR Dedicated medical equipment for patients If available, point-of-care analyzers for routine laboratory analyses If unavailable, pretreat serum w/Triton X-100 Lab samples double-bagged & hand-carried to lab Prompt burial or cremation of deceased with minimal handling Autopsies performed only by trained personnel with PPE
VHFs are transmitted via contact with blood and bodily fluids. Hantaviruses are an exception: infectious virus is not present in blood or excreta at the time of clinical presentation. Health care workers should wash their hands prior to donning, and after removing, personal protective equipment (PPE). Hands should be cleaned prior to the removal of facial protective equipment, and after the removal of all PPE. Care should be taken to avoid touching mucous membranes during patient care and before washing hands. PPE should be changed between patients. An adjoining anteroom is useful as a site for changing into and removal of protective clothing, supply storage, and decontamination of specimen containers. Airborne precautions require that the patient be placed in a room with negative air pressure, 6 to 12 air changes per hour, air exhausted directly to the outdoors or passed through a high-efficiency particulate air (HEPA) filter before recirculation, and doors kept closed. In mass casualty and other situations in which the use of negative air pressure rooms may not be feasible, all other infection control precautions (as outlined in slides 26-27) should be followed. Available evidence suggests that in the great preponderance of historical cases, these measures were sufficient to prevent transmission of disease to health care workers, family members, and other patients. The decision to use an N-95 mask versus a powered air purifying respirator (PAPR) should be made after considering the benefits and risks of each option in the specific situation. Disadvantages of the N-95 masks include the difficulty in ensuring a reliable face-mask seal with each use and impossibility of effective use by bearded individuals. PAPRs, on the other hand, are more expensive, bulky, impair voice communication, and may increase the risk of needlestick injuries. Dedicated medical equipment (e.g., stethoscopes) should be used for VHF patients, to decrease the risk of transferring infection to other patients. Point of care analyzers are small, portable devices that can be used at the bedside for routine laboratory tests; they should be used, if available, to minimize exposure of laboratory personnel to infectious specimens. If point of care analyzers are unavailable, specimens should be double-bagged, hand-carried to the laboratory, and pre-treated with Triton X-100, as this may decrease viral titers. Pretreatment with Triton X-100 does not significantly alter serum electrolytes, urea nitrogen, creatinine, and glucose or liver function test results. Embalming of deceased VHF patients should not be done. Autopsies should be performed only by specially trained persons using VHF-specific barrier precautions, HEPA-filtered respirators (N-95 masks or PAPRs), and negative-pressure rooms.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (347)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Compensation and Benefits SyllabusDocument3 pagesCompensation and Benefits SyllabusPratik LembheNo ratings yet
- Guia Del Examen de Ingles.Document11 pagesGuia Del Examen de Ingles.Anonymous E5UqPWhkimNo ratings yet
- Bone DensityDocument18 pagesBone Densitydhwanit31100% (1)
- West Coast Baptist College: Syllabus For BI 102 - New Testament SurveyDocument4 pagesWest Coast Baptist College: Syllabus For BI 102 - New Testament SurveyJakmensar Dewantara SiagianNo ratings yet
- An Invitation To CuriosityDocument12 pagesAn Invitation To CuriosityMax Marioneti100% (1)
- Management Interview QuestionsDocument3 pagesManagement Interview Questionsjoshua sacadasNo ratings yet
- BSW 2605 Portfolio Made EasyDocument4 pagesBSW 2605 Portfolio Made EasyMtshali NthusengNo ratings yet
- The Annotated Art of WarDocument4 pagesThe Annotated Art of WarLuisNo ratings yet
- Modeling and Simulation of Complex Communication NetworksDocument435 pagesModeling and Simulation of Complex Communication Networkssomeuser287No ratings yet
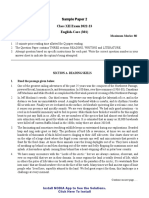
- EN Sample Paper 2 UnsolvedDocument12 pagesEN Sample Paper 2 UnsolvedYokesh BalajiNo ratings yet
- ID Act, 1947Document22 pagesID Act, 1947Abubakar MokarimNo ratings yet
- 13th Age - Bestiary Preview - OrcDocument7 pages13th Age - Bestiary Preview - OrcDasmatarixNo ratings yet
- KH Coder Tutorial Using Anne of Green Gables:: A Two-Step Approach To Quantitative Content Analysis Koichi HiguchiDocument35 pagesKH Coder Tutorial Using Anne of Green Gables:: A Two-Step Approach To Quantitative Content Analysis Koichi HiguchiAlbertNo ratings yet
- UCSP Module Week 11-20Document14 pagesUCSP Module Week 11-20Maricel BumanglagNo ratings yet
- Summit TV Video Program and Activity WorksheetsDocument4 pagesSummit TV Video Program and Activity WorksheetsAbdullahNo ratings yet
- AD9852Document42 pagesAD9852cbernal73No ratings yet
- Anna Cosio BioDocument1 pageAnna Cosio BioBandril MonNo ratings yet
- RLC Moot MumbaiDocument26 pagesRLC Moot MumbaiMudit GuptaNo ratings yet
- Session 14 CII Beniesh ModelDocument22 pagesSession 14 CII Beniesh ModelKumar PrashantNo ratings yet
- High Frequency Oscillatory Ventilation (HFOV) تغريدDocument16 pagesHigh Frequency Oscillatory Ventilation (HFOV) تغريدtaghreednurseNo ratings yet
- Valena Scientific Corporation - Case StudyDocument4 pagesValena Scientific Corporation - Case Studyaaashu770% (1)
- The Tales of Manhood What A Biblical Man Shows Final ThoughtsDocument1 pageThe Tales of Manhood What A Biblical Man Shows Final ThoughtsAugustus NiikondoNo ratings yet
- Equivalent Lateral Force ProcedureDocument2 pagesEquivalent Lateral Force ProceduremojeebmashalNo ratings yet
- Amir + Lev-Wiesel - 2007 - Dissociation As Depicted in Traumatic DrawingsDocument10 pagesAmir + Lev-Wiesel - 2007 - Dissociation As Depicted in Traumatic DrawingsAlejandra IsabelNo ratings yet
- How To Create Default RADDocument3 pagesHow To Create Default RADnikhil_805No ratings yet
- Psychology of Sport & ExerciseDocument11 pagesPsychology of Sport & ExerciseEzequiel KatzNo ratings yet
- Multivariable CalculusDocument158 pagesMultivariable CalculusJulian Cordero Arroyo100% (1)
- Destroy Lonely - If Looks Could Kill Lyrics Ge PDFDocument1 pageDestroy Lonely - If Looks Could Kill Lyrics Ge PDFMoodboy snNo ratings yet
- Read The Text and Complete It With The Simple Present of The Verbs in BracketsDocument2 pagesRead The Text and Complete It With The Simple Present of The Verbs in BracketsLaura VillamizarNo ratings yet
- Church Expansion Through Church - Emmanuel Louis NterfulDocument212 pagesChurch Expansion Through Church - Emmanuel Louis NterfulSP-Pitshou NdundaNo ratings yet