Professional Documents
Culture Documents
March Case Study Edited
Uploaded by
api-174496267Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
March Case Study Edited
Uploaded by
api-174496267Copyright:
Available Formats
1
Amanuel Negussie Clinical Practicum I March 25, 2013 Non-Small Cell Lung Cancer/Superior Vena Cava Syndrome History of Present Illness: SP is a 59-year-old female with a right para-hilar mass compressing the pulmonary artery and completely occluding the superior vena cava (SVC). She was on vacation when she experienced her first symptom. She initially noticed a swollen left breast, and started experiencing hemoptysis few days later. Therefore, she went to the local hospital. After few examinations, she was diagnosed with mastitis and got an antibiotic prescription. She also had a chest radiograph that showed a mass in her lung. Three weeks later, SP visited our hospital. During her first visit, she complained of symptoms that included shortness of breath, fatigue, and poor appetite. SP had a varicose vein that appeared on her chest a few months before her visit. Patients with early SVC symptoms and less respiratory distress can undergo an appropriate workups including chest radiograph, computed tomography (CT) scans, bronchoscopy, and biopsy of tumor.1 However in patients with severe SVC syndrome and respiratory distress, immediate emergency therapy must be initiated without tissue diagnosis.1 Since SPs symptoms did not categorized her as an emergency patient, she had a number of examinations done. A CT scan presented a right hilar and subhilar mass compressing the right pulmonary artery and SVC. It also presented a suspicious neoplastic process. A bronchoscopy procedure was also performed. Given the patients smoking history and weight loss, the mass that pressed the SVC represented a primary lung cancer. She also had two additional metastatic nodules in her right upper lung. A biopsy of all masses was taken during this procedure. Her primary mass measured 3.9x3.6x3.7 centimeter (cm). The other two nodules measured 10.6x8.7 cm, and 1.6 and 1.4 cm. Patient Medical History: SP had a right breast tumor that was removed surgically. She also had a past medical history of coronary artery disease (CAD), insomnia, adjustment disorder with mixed anxiety and depression, hyperlipidemia, coronary artery disease, osteopenia, clavicular fracture, and gastroesophageal reflux disease (GERD). Diagnostic Imaging Studies: A chest x-ray taken on 6/1/10 showed that both lungs were clear. No infiltration, pleural effusions, nodules, and mass lesions were seen. Pulmonary vasculature was normal, and cardiomediastinal silhouette was unremarkable. However, her recent chest x-ray and CT scan presented SVC obstruction and lung masses.
Family History: SPs father died of prostate cancer and her mother had a mayocardial infraction (MI) in her late 70s. Social History: SP is a veteran who lives alone. She has a son and two grand children who live a few miles from her. Her husband is deceased. SP has 60 packs per year smoking history, and still smokes. Medication: SP takes acetaminophen, Aspirin, Buspirone, Calcin, Cyclobenzaprine Hydrochloride, Ezetimibe, Ferrous Sulfate, Metoprolol, Niacin, Omeprazole, Rosuvastatine, Sertraline, Tramadol, and Trazodone. Recommendations: A completely obstructed SVC with a rich collateral vein circulation and abdominal walls of proximal veins which cannot be treated with surgery. For patients diagnosed with non-small cell lung cancer (NSCLC) that presses the SVC, both radiation and chemotherapy treatments are recommended.1 However, SP refused chemotherapy and decided to be treated with radiation alone. She was then scheduled for radiation therapy treatment consultation. The radiation oncologist discussed the treatment process and possible side effects. Informed consent was obtained, and SP was scheduled for simulation. The Plan (Prescription): After reviewing SPs chart and diagnostic studies, the radiation oncologist decided to proceed with three dimensional conformal radiation therapy (3DCRT). The treatment was prescribed to 4200 centigray (cGy) at 200 cGy per fraction to the 98% isodose line for the initial treatment followed by 1800 cGy off cord boost at 200cGy per fraction to the 97% isodose line. Patient Setup/ Immobilization: SP was simulated in a supine position. She was aligned straight on a wing board. Her arms were raised above her head holding the wing board bar (Figure 1). A large wedge sponge was placed under her knees for comfort (Figure 1). Hundred milliliter (ml) Visipaque contrast was administered intravascularly by a nurse. A respiratory sensor was placed on SPs chest prior to the scan, and she was instructed to breathe normally. A Philips large bore 16-slice CT machine was used for the simulation. Two sets of scan were acquired at 0.3 cm slices. The second scan was taken using an integrated respiratory gating system. Using this technology, the patient respiratory signal was recorded in conjunction with the scan. Anatomic Contouring: After the simulation was completed, the two scans were imported and fused in the Pinnacle3 9.0 radiation treatment planning system (TPS). The radiation oncologist contoured the gross tumor volume (GTV) and planning target volume (PTV) using the fused
images. The dosimetrist also contoured the left lung, right lung, heart, esophagus, carina, and spinal cord. The purpose of these contours was to assess and monitor the dose to organs at risk (OR) in the planning, quality assurance, and plan approval process. Beam Isocenter/ Arrangement: A Varian 21 IX 3501 linear accelerator (Linac) machine was used to treat the patient. During the simulation process, the radiation oncologist placed the isocenter in the tumor. A two field anterior/posterior (AP) and posterior/anterior (PA) field was used for the initial treatment. The gantry was set at 0o for the AP and at 180o for the PA. A left anterior oblique (LAO) and right posterior oblique (RPO) off cord beam arrangement was used for the boost field. The LAO was set at 60o and the RPO was set at 235o. The collimator and couch angle were set at 0o for all fields. Treatment Planning: The non-gated CT scans were used for the treatment plan. The dosimetrist picked a new calculation point 1cm medial from the isocenter, because the isocenter was 1cm away from the lateral border of the constructed field. The treatment was initially prescribed to 6000cGy for 200cGy per fraction. The plan was started with three fields of AP, PA, and right lateral. However, due to poor PTV coverage, a fourth left lateral field was added. The weighting of the beams was adjusted for an adequate PTV coverage. The fourth field helped reduce the spinal cord dose, but increased the total lung dose. The dose to all OR meets radiation therapy oncology group (RTOG) 617 protocol with a very close margin.1 Different angles were attempted on the two lateral fields, but the first attempt was better in all aspects. After reviewing the plan, the radiation oncologist was not satisfied with the plan due to the spinal cord dose. After a discussion with the dosimetrist and physicist, he decided to fractionate the treatment to an initial treatment of 4200cGy and off cord boost of 1800 cGy. As a result, an AP and PA field were used for the initial treatment. A multileaf collimator (MLC) blocking pattern was constructed with 1.5 cm margin around the PTV to define the treatment field (Figure 2). A 6 megavolt (MV) beam was primarily used for each field, but the PTV coverage was not sufficient. Therefore, mixed beam energy of 6MV and 18MV was used to achieve a better coverage. A weighting of 35% for the 6MV AP field, 25% for the 18MV AP field, 25% for the 6MV PA field, and 15% for the 18MV PA field was used. The boost was planned with a MLC blocking pattern of 0.7cm margin around the PTV that blocked the spinal cord (Figure 3). An 18MV energy and 54% weighting was used for the LAO field, and 6MV and 44% weighting was used for the RPO. The RTOG 617 protocol dose table was filled out and used to evaluate the dose to all contoured
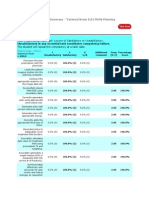
structures. The plan was finalized with a total monitor unit (MU) of 493, maximum dose of 6802cGy, and hot spot of 13% located anteriorly. In addition, the 100% isodose line adequately covered the PTV and the dose to all OR were below their tolerance level (Figure 4 and 5). After the plan was completed to the dosimetrists satisfaction, it was saved for the physician to evaluate. The radiation oncologist approved the plan after reviewing the RTOG 617 data sheet and evaluating the dose coverage to the PTV and OR. Quality Assurance Checks: MU check was performed using the MuCheck 8.2.0. software. At our clinical site, a 3% deviation in MU is the tolerance for any 3DCRT plans. Anything outside this range needs to be recalculated and fixed by the dosimetrists or physicists prior to treatment. The plan was approved with -2.35 % for the 6MV AP field, -2.1% for the 18 MV AP field, -2.99% for the 6MV PA field, -2.69% for the 18MV PA field, -1.91% for the LAO field, and 2.87% for the RPO field (Figure 6 and 7). The treatment plan was then reviewed and evaluated by the medical physicist before the patient began her treatment. Conclusions: Many attempts were made to improve this plan. We especially struggled to minimize the dose to spinal cord and total lung below RTOGs constraints. Although the dose to the lung was very low with the AP and PA field, adding the laterals made it challenging to meet these limits. However, fractionating the treatment allowed us achieve a much better treatment with minimal dose to OR. From this treatment, I learned the treatment regimens and protocols required for SVC syndrome. Before this plan, I considered SVC syndrome as an emergency case that will be treated with high dose and low fractions. However, I now know that SVC patients are only treated as emergency case if they have severe symptoms. I also learned that emergency cases are treated with higher dose of 400cGy per fraction for the first 2-3 treatments followed by additional daily dose of 180 to 200cGy.2
Figures
Figure 1: SPs set up position
Figure 2: Beams eye view (BEV) of the digitally reconstructed radiograph (DRR) demonstrating the field shape of the initial AP and PA field.
Figure 3: BEV of the DRR demonstrating the field shape of the boost LAO and RPO field.
Figure 4: Sagittal, axial, and coronal view of dose distribution
Figure 5: Dose volume histogram (DVH) of the treatment plan
Figure 6: MuCheck of the initial treatment
10
Figure 7: MuCheck of the boost treatment
11
References 1. Bradley, J. RTOG 617. A Randomized Phase III Comparison of Standard- Dose (60 Gy) Versus Highdose (74 Gy) Conformal Radiotherapy with Concurrent and Consolidation Carboplatin/Paclitaxel +/- Cetuximab (IND #103444) in Patients with Stage IIIA/IIIB Non-Small Cell Lung Cancer. http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=0617. Accessed March 17, 2013. 2. Perez CA, Halperin EC, Brady LW. Principle & Practice of Radiation Oncology. 4th ed. U.S.A. Lippincott Williams & Wilkins; 2004: 1226.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Amanuel Negussie: Certificate of AttendanceDocument1 pageAmanuel Negussie: Certificate of Attendanceapi-174496267No ratings yet
- V 13 RtsummaryonsitetrainingworkshopfamanuelnegussieDocument1 pageV 13 Rtsummaryonsitetrainingworkshopfamanuelnegussieapi-174496267No ratings yet
- ImrtDocument3 pagesImrtapi-174496267No ratings yet
- For E-PortfolioDocument14 pagesFor E-Portfolioapi-174496267No ratings yet
- ElectronDocument2 pagesElectronapi-174496267No ratings yet
- Conference LogsDocument1 pageConference Logsapi-174496267No ratings yet
- WK VII WikiDocument6 pagesWK VII Wikiapi-174496267No ratings yet
- WK II WikiDocument4 pagesWK II Wikiapi-174496267No ratings yet
- WK VI WikiDocument4 pagesWK VI Wikiapi-174496267No ratings yet
- Esophagus and ProstateDocument3 pagesEsophagus and Prostateapi-174496267No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Baseline Test in Science 9Document8 pagesBaseline Test in Science 9KRISTA MAE BALANAYNo ratings yet
- ThehumanbodypackDocument11 pagesThehumanbodypackLuciana ArandaNo ratings yet
- 2 1 E28093 Structure and Function of The Ventilation SystemDocument10 pages2 1 E28093 Structure and Function of The Ventilation Systemapi-343368893No ratings yet
- Pulmonary Nodules and Masses After Lung and Heart-Lung TransplantationDocument7 pagesPulmonary Nodules and Masses After Lung and Heart-Lung TransplantationManisha UppalNo ratings yet
- Pharmaceutical Inhalation Aerosol TechnologyDocument152 pagesPharmaceutical Inhalation Aerosol TechnologySyed Shabbir Haider100% (1)
- Human Physiology in An Aquatic EnvironmentDocument47 pagesHuman Physiology in An Aquatic EnvironmentMARIA CAMILA RENGIFO CAICEDONo ratings yet
- Pulmonary TuberculosisDocument5 pagesPulmonary TuberculosisRhelina MinNo ratings yet
- Physiology of Mechanical VentilationDocument12 pagesPhysiology of Mechanical VentilationCarlos ZepedaNo ratings yet
- Sci9 q1 Mod1 Respiratory and Circulatory Systems Working With Other Organ SystemsDocument37 pagesSci9 q1 Mod1 Respiratory and Circulatory Systems Working With Other Organ SystemsArbea John BaguioNo ratings yet
- Acute Respiratory Distress Syndrome (Ards)Document14 pagesAcute Respiratory Distress Syndrome (Ards)salma wangie fNo ratings yet
- Praktikum 1 Patologi ThoraxDocument61 pagesPraktikum 1 Patologi ThoraxFarizky DwitiaNo ratings yet
- Cooperative Activity 3-4 Through 3-8Document7 pagesCooperative Activity 3-4 Through 3-8Thalia Sanders0% (1)
- Physio Assesment 3 MBBSDocument14 pagesPhysio Assesment 3 MBBSAfaq RazaNo ratings yet
- Test Bank For Respiratory Disease A Case Study Approach To Patient Care 3rd Edition WilkinsDocument36 pagesTest Bank For Respiratory Disease A Case Study Approach To Patient Care 3rd Edition Wilkinscreutzerpilement1x24a100% (36)
- EmbryologyDocument26 pagesEmbryologyMeer BabanNo ratings yet
- Hal 1-50Document109 pagesHal 1-50Anonymous xh699eTd8I100% (2)
- Unit 6 Human Biology Biology Lecture NotesDocument6 pagesUnit 6 Human Biology Biology Lecture NotesGrace Melissa ChoiNo ratings yet
- Mallet AnatomyDocument277 pagesMallet AnatomyJethro Rola SiguaNo ratings yet
- Case Presentation On Chest PainDocument36 pagesCase Presentation On Chest PainpayumoNo ratings yet
- Respiratory PhysiologyDocument30 pagesRespiratory PhysiologyBarbara Sakura RiawanNo ratings yet
- 1B Chapter 7 (Gas Exchange) Exercise SolutionDocument3 pages1B Chapter 7 (Gas Exchange) Exercise SolutionSarahHung100% (1)
- Asthma and Lung MassDocument4 pagesAsthma and Lung MassAzmachamberAzmacareNo ratings yet
- Neet - Combined Test - 6 (P, C, B) - 06.08.2017Document19 pagesNeet - Combined Test - 6 (P, C, B) - 06.08.2017Sankar KumarasamyNo ratings yet
- Patient Assessment and Electrocardiogram: Clinical Case PresentationDocument7 pagesPatient Assessment and Electrocardiogram: Clinical Case PresentationLezahnor CasibangNo ratings yet
- Case Study PneumoniaDocument12 pagesCase Study PneumoniaFretzie Mae RamasNo ratings yet
- P&T Chapter Wise 300 MCQDocument13 pagesP&T Chapter Wise 300 MCQsudeep kulkarni100% (1)
- Occupational Health PSMDocument48 pagesOccupational Health PSMKabilesh Selvaraj100% (1)
- LungDocument5 pagesLungMoatasem AhmedNo ratings yet
- Acute Hypercapnic Respiratory Failure Associated With HemodialysisDocument3 pagesAcute Hypercapnic Respiratory Failure Associated With HemodialysisMahmoud DiaaNo ratings yet
- Basic Concepts in Nursing (Report)Document101 pagesBasic Concepts in Nursing (Report)NDJNo ratings yet