Professional Documents
Culture Documents
Human Physiology in An Aquatic Environment
Uploaded by
MARIA CAMILA RENGIFO CAICEDOOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Human Physiology in An Aquatic Environment
Uploaded by
MARIA CAMILA RENGIFO CAICEDOCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/282362173
Human Physiology in an Aquatic Environment
Article in Comprehensive Physiology · October 2015
DOI: 10.1002/cphy.c140018
CITATIONS READS
68 2,958
5 authors, including:
David Robert Pendergast Richard Moon
University at Buffalo, The State University of New York Duke University Medical Center
223 PUBLICATIONS 7,572 CITATIONS 261 PUBLICATIONS 5,595 CITATIONS
SEE PROFILE SEE PROFILE
Paola Zamparo
University of Verona
116 PUBLICATIONS 3,371 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Pathophysiology of Immersion Pulmonary Edema View project
Decompression Illness Treatment View project
All content following this page was uploaded by Paola Zamparo on 18 November 2015.
The user has requested enhancement of the downloaded file.
Human Physiology in an Aquatic Environment
David R. Pendergast,*1,2 Richard E. Moon,3 John J. Krasney,2 Heather E. Held,4 and Paola Zamparo5
ABSTRACT
Water covers over 70% of the earth, has varying depths and temperatures and contains much
of the earth’s resources. Head-out water immersion (HOWI) or submersion at various depths (div-
ing) in water of thermoneutral (TN) temperature elicits profound cardiorespiratory, endocrine, and
renal responses. The translocation of blood into the thorax and elevation of plasma volume by
autotransfusion of fluid from cells to the vascular compartment lead to increased cardiac stroke
volume and output and there is a hyperperfusion of some tissues. Pulmonary artery and capillary
hydrostatic pressures increase causing a decline in vital capacity with the potential for pulmonary
edema. Atrial stretch and increased arterial pressure cause reflex autonomic responses which re-
sult in endocrine changes that return plasma volume and arterial pressure to preimmersion levels.
Plasma volume is regulated via a reflex diuresis and natriuresis. Hydrostatic pressure also leads
to elastic loading of the chest, increasing work of breathing, energy cost, and thus blood flow to
respiratory muscles. Decreases in water temperature in HOWI do not affect the cardiac output
compared to TN; however, they influence heart rate and the distribution of muscle and fat blood
flow. The reduced muscle blood flow results in a reduced maximal oxygen consumption. The prop-
erties of water determine the mechanical load and the physiological responses during exercise
in water (e.g. swimming and water based activities). Increased hydrostatic pressure caused by
submersion does not affect stroke volume; however, progressive bradycardia decreases cardiac
output. During submersion, compressed gas must be breathed which introduces the potential for
oxygen toxicity, narcosis due to nitrogen, and tissue and vascular gas bubbles during decompres-
sion and after may cause pain in joints and the nervous system. © 2015 American Physiological
Society. Compr Physiol 5:1705-1750, 2015.
Introduction HOWI in thermoneutral (TN) water (34 or 35◦ C for 3-
6 h) results in a translocation of blood from the depen-
Water covers ∼70% of earth’s surface. The aquatic environ- dent limbs to the chest, as well as increased plasma vol-
ment is unique. While it is an environment with spectacular ume (PV) due to transcapillary autotransfusion of fluid from
flora and fauna, geology, and vast resources, the physical char- the cells (201, 204). These responses augment intrathoracic
acteristics of water impose profound physiological stresses on blood volume (11, 109, 203) which in turn increases cardiac
humans and animals. The underwater world is far less under- end-diastolic volume, stroke volume (SV) and cardiac output
stood than space or high altitude where extensive exploration (CO) due to increased end-diastolic cardiac fiber length (237).
has been carried out for many years. This review offers an Atrial stretch and elevated arterial pulse pressure (PP) elicit
overview of how the major environmental challenges, that baroreflex neuroendocrine responses that increase urine flow.
is, increased hydrostatic pressure, cold or warm water tem-
peratures, the unbreathable ambient medium and pressure of
the “Silent World” affect breathing, circulation, fluid and * Correspondence to dpenderg@buffalo.edu
electrolyte balance, locomotion, and thermal regulation in 1 Center for Research and Education in Special Environments,
humans. In addition, the effects of the depth and time of div- University at Buffalo, Buffalo, New York, USA
ing can cause deleterious pharmacological and toxic effects. 2 Department of Physiology and Biophysics, University at Buffalo,
As humans are terrestrial, exposure to the aquatic envi- Buffalo, New York, USA
3 Center for Hyperbaric Medicine and Environmental Physiology,
ronment is often viewed negatively and being problematic for
Duke University, Durham, North Carolina, USA
man. While this is partly true, it must be emphasized that life 4 Biomedical Hyperbarics Research Laboratory, Molecular
evolved in the oceans and aquatic organisms leaving the seas
Pharmacology and Physiology, College of Medicine, University of
had to adapt to new terrestrial habitats. Coming out of the sea South Florida, Tampa, Florida, USA
required profound circulatory and musculoskeletal adapta- 5 Department of Neurological and Movement Sciences, University of
tions to gravity, marked alterations in the capacity to maintain Verona, Verona, Italy
fluid and electrolyte balance and of course a switch to lung Published online, October 2015 (comprehensivephysiology.com)
versus gill respiration. Failure to maintain homeostasis in the DOI: 10.1002/cphy.c140018
aquatic environment can result in injury or death. Copyright © American Physiological Society.
Volume 5, October 2015 1705
The Aquatic Environment Comprehensive Physiology
Autotransfusion may persist for as long as 24 h (depending periods (TN = 35◦ at rest and 28-30◦ C during exercise), and,
on the level of volume repletion). as water has high thermal conductance and capacity, there is
As the baseline characteristics of cardio-renal regulation danger of hypothermia when diving in these waters without
are altered compared to terrestrial exercise, the CO, SV, and adequate thermal protective gear. HOWI or diving in cold
blood flow to nonmuscle tissues are greater, and HR and total water temperatures below TN results in greater translocation
peripheral resistance (TPR) are lower. However, mean arterial of blood into the chest relative to the increase in TN immer-
blood pressure (MAP) responses are similar to those observed sion and reductions in intracellular fluid, although there is less
in air (297). In spite of this different baseline cardiovascular autotransfusion and PV is not increased as much (358) such
and renal status in water, increased metabolism during exer- that there is a similar increase in CO in both cold and TN
cise results in similar adjustments in TN water and air, at immersion (297). Although there is increased sympathetic
oxygen consumption (VO2 ) above 1.0 L min−1 , and as high activity, arterial blood pressure is not increased in HOWI
as 80% of maximal aerobic power (VO2 max ) (297, 309). The in cold water as the skin, subcutaneous tissues, and muscle
potential for pulmonary edema increases during exercise in reduced blood flow and increased resistances are likely off-
water (352), particularly in cold water (196). set by increased blood flow in other areas and TPR remains
Breath-holding for a short time is possible for air breath- unchanged (297). The effects of HOWI in warmer or hot
ing mammals, including man. For longer submersions, the water, particularly during exercise, are not extensively inves-
diver has to use pressure compensating equipment to provide tigated and present great challenges to adjustment.
free access to suitable gas. At shallow depths, a snorkel can be Due to body size and physiological differences there
used; however, its effective depth is limited to just under the may be gender differences in the responses to HOWI in TN
surface due to the inability of the respiratory muscles to over- (408), cold, and warm water. Age may also affect physio-
come the hydrostatic pressure on the chest wall and of course logical responses to HOWI, as the increase in CO reported
water entering the snorkel (23). At greater depths, gear called for younger subjects in HOWI is not as great in older sub-
Self-Contained Underwater Breathing Apparatus (SCUBA), jects (302). In addition, there may be different physiological
or a closed-circuit rebreathing system [using special gas mix- responses to body cooling or warming in the elderly, specifi-
tures or pure oxygen (O2 ) in combination with a carbon diox- cally regulation of metabolism and vascular control (147).
ide (CO2 ) scrubber] control gas flow from a high pressure The stresses and strains resulting from the aquatic envi-
tank via a regulator (172). Breathing underwater is also influ- ronment may pose dangers to humans’ exposure to them. On
enced by the depth-induced hydrostatic pressure differences the other hand, HOWI has potential therapeutic benefits and
across the chest wall (static lung loading, SLL) (368), gas this area requires further exploration. The wide variety of
density and composition, and by exercise hyperpnoea, which aquatic environments will be further developed in the sec-
in combination cause increased power of breathing (POB) and tions below. The understanding of the aquatic environment
fatigue of the respiratory muscles (14, 321, 322, 425). starts with its physical properties. HOWI is not only a com-
Alveolar ventilation in normal conditions is regulated to mon aquatic environment, but also a tool to understanding the
maintain arterial PCO2 (PaCO2 ) at ∼40 mmHg with little interactions between the cardio-renal systems and thus is a
variation in normal healthy subjects (167), while matching major part of this paper. As most of the waters of the world
O2 delivery to metabolic demands. The translocation of blood are relatively cold, its effect on physiological systems has to
from the periphery to the chest in HOWI results in reduction be explored. The aquatic environment involves being on the
in air in the lungs, and thus alters ventilation both at rest and water in a water craft, at the water’s surface swimming, as well
during exercise. In addition, diving may promote hypercap- as being submersed in the water during diving. Each of these
nia (CO2 retention) due to a routine practice by divers of different aquatic environments has specific requirements.
hypoventilating to conserve gas and extend dive time and/or
the increased respiratory work which cannot be performed
due to weak or fatigued respiratory muscles. Physical Properties of Water
When compared to altitude, hypoxia is not an issue in the
The properties of the aquatic environment (69) both individu-
aquatic environment as at the surface air is breathed and during
ally and collectively impose critical challenges to physiologi-
submersion breathing with SCUBA gear increases total pres-
cal adjustment. Some of these challenges cannot be compen-
sure and also increases PO2 . However, hyperoxia can damage
sated for physiologically, and thus devices or equipment have
pulmonary (25, 76) and neural (84) tissues. Human adap-
to be used for humans to function in the aquatic environment.
tive responses to hyperoxia appear limited since man is not
normally exposed to high ambient PO2 . In addition to O2 ,
pressures of other gases such as N2 may be increased during Density
submersion at depth such that the gas is absorbed by tissue The density of water is about 1 g cm−3 ; however, it is also
compression to the point of saturation; the unloading of which influenced by temperature (69). The density of liquid water
during decompression imposes further stress on the diver. increases with temperature and maximal density is at approx-
Most swimming and diving occurs where water is colder imately 4◦ C (39◦ F), which is the water temperature of arctic
than the temperature to which subjects can adjust for long water. In addition, there are thermoclines in water, the colder
1706 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
the temperature the deeper the water. In fresh water at 4◦ C, the human function in the aquatic environment. Water is in liq-
water closer to the surface and cold air lose heat energy such uid form at normal temperatures, and holds 80% to 90% of
that the water at the surface is less than 4◦ C. These thermo- the earth’s heat. Water has the capacity to cool the human
clines in water have an impact on thermal stress in humans. body nominally 20 times greater than air. Therefore, hypother-
Floating in water is made possible because of the den- mia or hyperthermia are significant risks in cold and warm
sity of water (69). Density of water is also dependent on the water, respectively. Although the effects of cold water are
salt content which is high in some bodies of water. However, most common and well-studied, exposure to warm/hot water
the high density of water reduces the ability to function in (hyperthermia) is understudied.
water, i.e. there is an increase in the energy cost of locomo-
tion. Dynamic viscosity determines how easily bodies move
through water. Dynamic viscosity divided by density is kine- Head-Out Water Immersion in
matic viscosity. It is easier to float in saltwater as it is denser
Thermoneutral Water
than fresh water. It costs less energy to swim in warm water
even though it is harder to float. The body is about 75% Humans can be in the aquatic environment either immersed
water, but body fat contains less than 75% water so humans with the HOWI or head in the water (swimming) or sub-
with higher fat may float better and have greater resistance to mersed underwater at various depths (diving). Body posture
heat loss. during immersion is significant. One may be immersed either
Compressibility of water is influenced by both pres- in the head-out vertical posture or supine in the water so that
sure and temperature (69) and impacts performance in the the profile of external hydrostatic pressure forces on depen-
aquatic environment. Water compressibility ranges from dent regions differs between vertical and supine. Erect HOWI
5.1 × 10−10 to 4.4×10−10 Pa−1 and is dependent on water has been used as a simple, noninvasive maneuver to increase
temperature (0-45◦ C, respectively). The low compressibility central blood volume and has provided useful insights into
of water often leads to the erroneous conclusion that water is the regulation of blood volume. Increased body buoyancy
incompressible. in HOWI minimizes the influence of gravity and therefore
HOWI has provided important insights into the physiology
of microgravity. In addition to its utility for understanding
Pressure effects of microgravity and volume regulation, HOWI is an
Sea level pressure is 1 atmosphere absolute (ATA) and ambi- obvious useful tool for the study of the physiology of the
ent pressure increases by 1 ATA for every additional 10 m of aquatic environment. Lastly, HOWI can be a useful nonphar-
depth. Air in gas-containing spaces contributes to buoyancy in macological therapeutic modality for the treatment of fluid
water, however since air is compressed with increasing depths retention disorders. An overview of the physiological status
of submersion, buoyancy decreases as depth increases. Gas- during immersion is shown in Figure 1, and will be described
containing spaces in the body are compressed underwater, and in the section on immersion below.
then the volume reexpands when returning to the surface. On As stated above, since there is a hydrostatic pressure gra-
returning to the surface from submersion the increase in vol- dient acting upon the body surface, an erect versus supine
ume may cause problems in air-containing tissues/organs, par- posture in water influences the character of the physiological
ticularly during uncontrolled ascents. Other pressure-related responses as shown in Figure 2. In this article, the focus will
effects during diving include the concomitant increase in gas be primarily upon upright HOWI, unless noted otherwise. In
partial pressures (e.g., O2 and N2 ), and the higher breathing addition, the TN temperature for humans is considered to be
gas density. 34 to 35◦ C for water immersions of 3 to 6 h and we will first
At depths beyond 100-150 m, there are effects of pres- discuss responses to TN HOWI, followed by a description
sure per se, which include tremors and “microsleep.” This is of how varying water temperatures influence the basic TN
termed the high pressure nervous syndrome (HPNS) (22). response. The physiological responses to HOWI are not sim-
Convulsions have been observed in monkeys (22). Other ply due to the removal of gravity because during immersion
effects include partial reversal of sedation or general anes- there is a unique set of stimuli that are not present in true
thesia (382, 383). It is believed that these phenomena occur microgravity.
due to pressure-related changes in macromolecule conforma- The overall physiological responses during water immer-
tion and altered neurotransmitter release (331). Narcotic gases sion appear to be directed toward the homeostatic main-
such as nitrogen can partially offset the effects of HPNS (24). tenance of central cardiopulmonary blood volume via car-
diopulmonary and arterial baroreflexes. Normally, there is a
tight coupling between oxygen delivery and metabolic rate
Heat capacity via autoregulation of blood flow (151). By contrast, in water
The specific heat capacity of water is high (pure liquid water = immersion, there appears to be a unique resetting of vascular
4.182 J K−1 g−1 ) and conducts heat effectively based on autoregulatory control such that the ratio of oxygen delivery
temperature gradients (69). The high heat capacity and high to metabolism increases in the systemic circuit and in some
heat conductivity of water can have significant influences on regional vascular circuits.
Volume 5, October 2015 1707
The Aquatic Environment Comprehensive Physiology
Head-out immersion:
thermoneutral water
Hydrostatic compression
of immersed tissues
Cell Venous
volume capacity
Autotransfusion,
potassium, amino acids Blood flow/oxygen
shift uptake
Natriuresis
Diuresis Hypervolaemia Venous return Cardiac output
Diuresis
Major effect
Renal Cardiac volume Stroke volume
sympathetic
nerve activity
Activation of
cardiac receptors
Vasopressin Aortic pulse pressure
secretion
Release of atrial
natriuretic peptide
Renin
aldosterone Activation of
secretion arterial baroreceptors
(?)
(?) Redundancy:
Renal atrial
natriuretic Time-dependent effects
peptide Bipeds versus quadrupeds
sensitivity Resetting of reflexes
Hydration state
Physical training
Adaptation
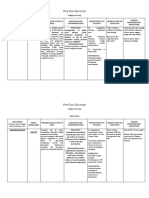
Figure 1 Summary of the circulatory, renal hormonal and neuro responses to thermoneutral HOWI. Central volume expansion and
elevated CO are caused by compression of the dependent veins and autotransfusion. The rise in CO exceeds the metabolic demand
at rest and during exercise. Activation of cardiovascular mechanoreceptors and increased atrial natriuretic peptide secretion sets into
motion neural and hormonal mechanism that promote sodium and fluid loss, thus minimizing hypervolemia and theoretically readjusting
blood flow to the prevailing oxygen uptake. The most powerful efferent mechanism affecting the kidney appears to be sympathetic nerves.
The associated hormonal responses appear to modulate the primary renal response, with many additional factors modulating the basic
renal neurohumoral responses to immersion. Redrawn from Krasney (201) and reproduced with permission from Elsevier Limited, Oxford,
United Kingdom (204).
Circulatory responses and fluid shifts pressure (184). The major role of the kidney in HOWI is to
blunt the expansion of PV and prevent a further increase in PV
Hydrostatic pressure during HOWI translocates blood
(see Fig. 4) and CO as seen in Figure 5 (201,256,257). Early in
to the thorax by compressing the venous compartment.
immersion PV increases about 7% (Fig. 4). There is a signif-
The translocation of blood to the thorax is shown in Figures 2
icant increase in tissue pressure compared to capillary hydro-
and 3 (186). The fluid translocated into the vascular compart-
static pressure promoting capillary reabsorption. Tissue pres-
ment is derived from the intracellular compartment (see Fig.
sure, capillary pressure and central venous pressure (CVP)
2). This autotransfusion into the plasma compartment origi-
are coupled in a linear fashion. Stepwise levels of immersion
nates primarily from the capillaries of the dependent limbs and
from dependent limbs to abdomen, to mid-thorax and to mid-
both expands PV (see Fig. 4) and decreases plasma oncotic
cervical level cause CVP to increase progressively. Plasma
1708 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
Upright in air Upright water immersion
Right atrial Right atrial
pressure: Aorta pressure: Aorta
0 kPa (mmHg) 2 kPa (15 mmHg)
Cardiac
output
Central
Venous return
Venous return
volume
expansion
Autotransfusion Hydrostatic
Filtration pressure:
16 kPa (120 mmHg)
Venous
compartment Hydrostatic
compression
of dependent
tissues
Systemic hypervolaemia
due to autotransfusion
Figure 2 While standing in air (A), right atrial pressure is low and gravity-dependent veins are distended
resulting in increased net plasma filtration in the limb capillaries. During HOWI (B), central volume expansion
occurs with increased right atrial pressure and cardiac output. These result from hydrostatic compression of
the dependent tissues and capillary reabsorption, or an autotransfusion in the dependent limbs. Redrawn
from Krasney (201) and reproduced with permission from Elsevier Limited, Oxford, United Kingdom (204).
Lymphatic oncotic pressure is decreased in HOWI resulting in hemodi-
lution, whereas plasma osmolarity is unchanged. Amino acids
Plasma Interstitial Intracellular
and potassium are increased in the plasma suggesting that the
Renal
volume fluid fluid majority of the fluid shifted is out of the intracellular compart-
Capillary Cellular ment (83, 201, 358). In spite of this, interstitial fluid volume
Immersion and lymph flow do not change in HOWI. PV, SV, and CO are
elevated and sustained throughout 6 to 12 h immersions com-
pared to erect in air (348). These data support the contention
that the intracellular reservoir of fluid is not diminished sig-
Fluid change (mL·kg–1 · min–1)
0
nificantly during HOWI (185). CO is increased in HOWI and
Rest Water immersion
–0.05 110
105
PV(% Δc)
–0.10
Lymphatic 100
Renal
–0.15 Cellular
95
Capillary
–40 0 40 80 120 0
Time (min) 0 1 2 3 4 5
Time (h)
Figure 3 There are three major fluid shifts that occur during HOWI
(upper flow diagram): across capillary, across the cell wall and across Figure 4 Human plasma volume (PV) expressed as a percentage
the kidney. The lymphatic fluid shift is minor. These compartmental fluid change during HOWI in TN water (35◦ C) (squares) and sitting in
changes are then illustrated (graph) for the 120-min upright, thermoneu- thermoneutral air (22◦ C) (circles) from their respective control values.
tral HOWI. Redrawn from Krasney (201) and reproduced with permis- The ∗ indicate that HOWI values are significantly higher than the air
sion from Elsevier Limited, Oxford, United Kingdom (204). counterparts.
Volume 5, October 2015 1709
The Aquatic Environment Comprehensive Physiology
12 Rest Water immersion the cerebellum. HOWI in TN or warmer water results in
increased temperature of the integument causing significantly
11
increased blood flows to skin and subcutaneous fat. Urine out-
Q (1 · min–1)
10 put increases, in spite of the absence of increased blood flow
9 during HOWI. By comparison there are immediate, although
temporary, increases in blood flows (and O2 delivery) to the
8
gastrointestinal tract, liver, pancreas, and spleen. As HOWI
·
7 continues, blood flow to visceral tissues decline to pre-HOWI
6 levels. At this point, the increased CO is redistributed to non-
respiratory skeletal muscles. The elevated blood flow to some
5
0 1 2 3 4 5
tissues may counterbalance fluid shifts out of cells in some
tissues. The increase in CO and tissue blood flows promote
Time (h)
total-body nitrogen elimination during oxygen breathing dur-
Figure 5 Resting cardiac output (Q, L/m) is plotted as a function ing HOWI in TN water compared to nonimmersion (15).
of time for humans resting HOWI in TN water (35◦ C) (squares) and Circulatory and renal responses to HOWI are elicited by
sitting in TN air (22◦ C)(circles). The ∗ indicate that HOWI values are
significantly higher than the air counterparts.
reflex activation due to mechanical loading of cardiovascular
stretch receptors. As stated above in humans, HOWI to the
mid-cervical level is estimated to increase CO from 32% to
its level is greater for the erect posture, increasing from leg 62% which is shown in Figure 5. The magnitude of the esti-
only immersion to mid-cervical HOWI. The increased CO is mated increases in CO depends upon the method and subjects
maintained for many hours. CO is increased 32% to 62% dur- used (201). The increased CO is due to a significant increase
ing HOWI (Fig. 5) due to an increased SV, even though HR is in SV since HR decreases. MAP reported by most studies is
decreased. The relative increase in SV exceeds the observed not shown to change in HOWI, in spite of the increased CO,
decline of HR such that there is a net increase in CO as as TPR is proportionally decreased. Arterial PP is increased
shown in Figure 5. MAP is not effected by HOWI and there- in HOWI, due to the increase in SV (281). The magnitude
fore TPR must be decreased (11, 201, 281). VO2 is unchanged of the increase in CO is coupled to the depth of immersion.
during HOWI in TN water, thus it is apparent that systemic CO increases in a graded fashion from leg (only) immer-
O2 delivery quickly exceeds systemic O2 demands in HOWI. sion through mid-thorax to mid-cervical immersion and the
Blood flow to specific tissues is autoregulated to meet their increase in CO is sustained for several hours (18, 113). The
metabolic demands (151); however, it is blunted in HOWI as elevated CO in immersion is a result of increased cardiopul-
shown in Figure 6 for limb blood flow. The expected autoregu- monary blood volume which in turn increases cardiac filling
latory readjustment of systemic blood flows to match tissue O2 pressures and preload (11).
demands does not occur in HOWI but rather sustained hyper- Pulmonary artery pressure and pulmonary vascular vol-
emia occurs in some tissues (see Fig. 6) (59, 154, 297). Blood ume increase in water immersion and there is a decline of vital
flows to respiratory muscles and cardiac muscle increase as capacity (VC) (364). External water pressure compresses the
expected in response to their increased metabolism, secondary chest which in-turn increases elastic loading of the chest wall
to increased respiratory and cardiac work (154). HOWI- and results in negative pressure breathing (171). The resul-
induced changes in vestibular and proprioceptive inputs tant increase in energy cost of ventilation, secondary to the
caused by buoyancy-microgravity result in hyperemia of increased POB causes an increases in blood flow to the respi-
ratory muscles (154, 314, 366). Prefaut et al. (314) observed
mild hypoxemia in humans with increased lung closing vol-
6 Rest Water immersion Recovery ume (CV). While the apical portions of the lung are less
perfused when upright in air, HOWI causes their flow to
LBF (ml · min–1 · cm–1)
5 increase (314). The overall effect of immersion on ventilation-
4 perfusion (VA /Q) relationships depends on the relationship of
CV to expiratory reserve volume (ERV). When CV is less than
3
ERV (usually in young individuals), during immersion VA /Q
2 relationships are preserved. Arterial PO2 is usually increased
due to an increase in the ventilation to oxygen consumption
1
ratio (VE /VO2 ) ratio (87). When CV exceeds ERV (common in
0 older individuals), immersion is associated with an increase in
0 1 2 3 4 5 right-to-left shunt (87) and a widening of the alveolar-arterial
Time (h) PO2 difference (86).
Figure 6 Resting lower limb blood flow measured by plethysmogra-
Von Diringshofen (400) was the first to postulate that fluid
phy is plotted as function to time of HOWI. The ∗ indicates a significant shifts into the plasma compartment during water immersion
increase above air control. (see Fig. 3). This hypothesis was validated in dog studies
1710 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
(83, 254-257, 260), with increases of PV on the order of ∼7% for regulation of neurohumoral activity and circulatory func-
following 100 min of immersion. Interstitial pressure during tion in HOWI. The volume of fluid expanding the plasma
HOWI is above the capillary hydrostatic pressure, promot- compartment via the transcapillary fluid shift appears to inde-
ing capillary absorption. There is a linear coupling of tissue pendently influence the magnitude of suppression of the renin-
pressure, capillary pressure and CVP and the depth of HOWI. angiotensin system (127, 128).
Plasma osmolarity is not affected by HOWI; however, plasma There are several possible mechanisms for the dramatic
oncotic pressure is decreased and leads to hemodilution. Inter- fluid shift out of the cellular compartment during immer-
stitial fluid volume and lymph flow are not effected by HOWI; sion (See Figs. 1 and 3). First, a primary movement of iso-
however, there is an increase in both amino acids and potas- tonic fluid out of the interstitium into the capillaries leaves
sium concentration in plasma. These changes suggest that the behind osmotically active proteins that could in-turn draw
fluid is shifted out of the intracellular compartment (83, 201). water out of the cells. Second, relative differences in compli-
The kidneys act to minimize the rise in PV, since evidence ances between cells, the interstitial compartment and capil-
from immersed, anaesthetized and nephrectomized dogs has laries could promote a decrease of cell volume more than the
shown PV to increase by 40% instead of the 7% increase interstitial fluid, thus increasing interstitial pressure that could
observed in dogs with intact kidneys. Figure 3 indicates the in turn increase capillary reabsorption. Third, if cells per-
transcellular, transcapillary, and renal fluid shifts that occur ceive hydrostatic compression as an increase in cell volume,
during water immersion. then this could activate cellular volume regulatory decreases
Graded immersion studies indicate that blood is shifted via solute efflux as cells sense and react to volume changes
from the legs to the abdomen, then from abdomen to chest as of 3% or more. The rise in plasma potassium content dur-
shown in Figures 2 and 3. The abdominal splanchnic veins ing water immersion is compatible with cellular regulatory
are an important volume reservoir (186). The increase in CO volume decreases due to loss of potassium chloride perhaps
is graded depending on the depth of HOWI in the erect posi- caused by activation of separate cell membrane potassium
tion (113). The initial increase in cardiac preload increases and chloride channels, and potassium-chloride cotransporters
the change in cardiac chambers and inferior vena cava diam- (360). It has been suggested that the fluid shift occurs mainly
eter, but this is followed by the excretion of nominally 1.5 L from the lower extremities (186). In addition to the increase in
(range 1.0-2.0 L, 202) of urine that in turn decreases intratho- blood flow to the respiratory muscles (diaphragm and inter-
racic blood volume, cardiac preload, SV, and CO (see Fig. 5). costals), coronary blood flow increases commensurate with
The initial HOWI-induced increase in CO is associated with the increase in cardiac work during immersion (153, 154).
peripheral vasodilatation, which is followed later by periph- Secondary to changes in vestibular and proprioceptive inputs
eral vasoconstriction so that lower limb blood flow decreases due to buoyancy and the microgravity state, blood flow to the
over time as CO falls toward control levels (35). HOWI to cerebellum is also increased. However, total cerebral blood
the mid-cervical level results in greater increases in left atrial flow is not changed, implying vasoconstriction in some brain
diameter; however, MAP remains unchanged and arterial PP regions. While core temperature is unchanged, HOWI in TN
does not change any further. Although there was a greater water heats up the integument, since there is an 8◦ C to 10◦ C
increase of CVP during mid-cervical HOWI, plasma nore- difference between the temperature of TN air and warmer TN
pinephrine (NE) declined to levels observed during shallower water. Accordingly, blood flow to skin and subcutaneous fat
immersions. The decline of plasma NE reflects attenuation rises in the order of several hundred percent. Increased cuta-
of sympathetic nerve activity (SNA). Subcutaneous vascular neous blood flow could account for the common observation
resistance in the forearm decreased similarly during HOWI that the cutaneous veins on the dorsum of the feet and hands
both to the xiphoid level and mid-cervical level, whereas remain distended while standing in water.
forearm vascular resistance in muscle declined only during The mechanisms for other regional flow adjustments
mid-cervical HOWI. This observation implies that cutaneous during water immersion are less certain. While blood flow
vasodilation in the forearm reaches maximal levels at shal- to the kidney is unchanged, there are early increases in
lower immersion depths compared to vasodilation in skeletal flows to the gastrointestinal tract, liver, pancreas, and spleen
muscle (127, 128). CVP increases about 5 mmHg along with (154). These increases are proportional to the change in CO.
an increase of left atrial diameter during mid-cervical HOWI After about 30 min of immersion, the increased visceral
and the expansion of cardiac volume is related to decreases of flow declines to preimmersion levels, and the increased CO
plasma renin activity (PRA), as well as plasma protein con- is redistributed to nonrespiratory skeletal muscles. These
centration. By comparison, when the central translocation of regional hyperemias suggest that HOWI has the potential
blood out of the lower limbs during HOWI was prevented by to be a treatment of decompression sickness (DCS) and
placing pressure cuffs on the thighs, the increases of atrial muscle injury and to increase drug delivery to specific
dimensions were similar to those observed in the uncuffed organs, such as the liver. Perhaps these regional hyperemias
situation, whereas the degree of plasma hemodilution was elicit local elevations of capillary hydrostatic pressures that
less and the level of suppression of PRA was attenuated. This counterbalance fluid shifts from the cells in selected tissues.
observation suggests that mechanisms in addition to input In humans, HOWI in either 8◦ C or 22◦ C water results
from low- and high-pressure baroreceptors are responsible in a reductions of femoral artery and cutaneous vascular
Volume 5, October 2015 1711
The Aquatic Environment Comprehensive Physiology
(.10) _ 28
1.6 (a-v)O 1·1–1 (.05) (.10)
2
(.15) 24
1.2 20 H 2O (.20)
Q (1 · min–1)
Qm (1 · min–1)
(.20)
16
0.8
12 Rest Temp Max
·
Air A
·
30° 8 35
0.4
25° 30
20° 4 25
20
0 0
0 0.5 1.0 1.5 2.0 0 1 2 3 4
· –1 ·
VO2 M’ (1 · min ) VO2 (1 · min–1)
Figure 7 Muscle blood flow measured by 133 Xe washout from Figure 8 Cardiac output (Q, L/min) is plotted as a function of oxygen
quadriceps muscle at rest and during cycling exercise is plotted as a consumption (L/min) for air and HOWI in 20◦ C to 35◦ C water at rest
function of VO2 for air and HOWI in 20◦ C, 25◦ C, and 30◦ C water. (VO2 < 1.0 L/min) and exercise (VO2 > 1.0 L/min).
The dashed lines represent a constant (a-v)O2 as a function of VO2 .
diuresis-induced hypovolemia does impair orthostatic adjust-
conductance immediately upon immersion (30-40%). By ment (173)
comparison cutaneous vasoconstriction was less in 8◦ C water The physiological responses to HOWI are temperature
than 22◦ C water (150). Other studies have demonstrated that dependent and this is shown in Figures 7 and 8 (297) and,
cutaneous (394) and muscle (see Fig. 7) (297) blood flows therefore, the study of water immersion requires the elimina-
decrease in cold water. Blood flow to skin and subcutaneous tion of thermal stress. In humans, this is achieved by using
tissues reach minimum levels in cool water (≤30◦ C), whereas water temperatures of 34 to 35◦ C for exposures up to 6 h. For
there is a graded temperature-dependent blunting of resting measurements of hemodynamics, it is important to determine
and exercise hyperemia as seen in Figure 7 (297). the hydrostatic indifference point which is the location in the
During TN water HOWI in humans, cardiopulmonary vol- vasculature at which pressure is independent of posture. This
ume is increased (109, 199), which augments CO via the is a transition zone at which intravascular pressure remains
length-tension response. Since by definition systemic VO2 constant and as such represents a center of gravity for the
does not change during TN immersion, an unusual situation cardiovascular system (132, 332, 333). In humans, this point
develops where systemic oxygen delivery exceeds systemic is usually considered to be at the level of the right atrium
tissue requirements more than usual at rest for sustained peri- (332, 333). However, during HOWI it is very likely to shift;
ods. Autoregulation typically matches metabolic demands of therefore, it is inappropriate in immersion to reference mea-
peripheral tissues to blood flow (150). However, this relation- sured physiological pressures to the surface level of the water.
ship is modified during immersion (Figs. 1, 4, 6) to allow It is better to insert a reference catheter in the esophagus for
for increased systemic blood flow (60, 153, 154). Gauer and estimation of pleural and transmural pressures across the heart
Henry (131) postulated that the diuresis by the kidneys during and great vessels (11, 256, 258).
HOWI results in a net reduction of PV. However, this view was HOWI is a noninvasive maneuver and therefore it has been
later modified when it was shown that PV is expanded during considered to be the investigative tool of choice for studying
HOWI as a result of the transcapillary fluid shift (see Fig. physiological mechanisms of PV regulation (131). Never-
3). Therefore, the increased urine flow and sodium excretion theless, HOWI cannot be strictly compared to true volume
during immersion does not reduce PV below preimmersion expansion, microgravity or head-down tilt, since there are
levels, at least during short-term immersions, as previously unique characteristics associated with each maneuver. Com-
postulated (131). Instead, the kidneys act to off-set the PV pared to true volume expansion, the magnitude of the diuresis
expansion due to HOWI, which if not compensated for would and natriuresis caused by HOWI is equivalent to the infusion
cause a 40% increase in PV (201, 254, 256). The elevation of of 2 L of 0.9% saline (sodium chloride) solution (109). In
PV is sustained during HOWI lasting at least 6 to 12 h (185). terms of the coupling of the cardiac and renal responses, the
In fact, if the renal response did produce a net reduction in induction of hypovolemia as a result of the removal of 15% of
PV as previously postulated (131) the hypovolemia would the total blood volume does not affect the 22% increase in CO
be expected to impair orthostatic adjustments upon emerging in HOWI; however, the diuresis and sodium excretion were
from the water. In fact, a previous study demonstrate that this previously reported to be significantly decreased suggesting
1712 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
Vagal
afferent
activity
Neural lobe
of hypophysis
Atrial
volume
Central
blood
Vassopressin
volume
(antidiuretic hormone)
secretion
Water
Blood reabsorption
volume
Free-water
clearance
Figure 9 An early version of the Gauer-Henry hypothesis. Arrows indicate an increase or stimu-
lation of the variable, darkened arrows indicate a decrease or inhibition of the variable. Redrawn
from Krasney (201) and reproduced with permission from Elsevier Limited, Oxford, United Kingdom
(204).
that the renal responses are quantitatively not well-coupled to is increased (19). The level of physical fitness also affects the
the cardiac response (350). nature of the HOWI renal responses. It has been shown that
HOWI has been shown by many authors to reduce HR, the diuresis and natriuresis due to HOWI were significantly
and more so in cold water. Both apnea and immersion of the blunted in runners and swimmers compared to control
face in cold water have demonstrated a biphasic decrease in subjects in spite of larger and more persistent increases in CO
HR, with a rapid initial decrease and a later slow phase. These (65). Kidney responses to water immersion are primarily due
bradycardia responses are exaggerated in adolescent subjects to alterations in renal tubular functions because glomerular
and they are associated with a high probability of arrhythmias filtration rate (GFR) does not change. In spite of the lack of
(412). The apnea-face immersion bradycardia is partly due increase in plasma osmolarity during HOWI, plasma vaso-
to reduced cardiac SNA and increased vagal tone. Muscle pressin (antidiuretic hormone) level was decreased and asso-
SNA decreases in TN HOWI (262, 263). The decreased HR ciated with the observed increase in CH2 O (26,110,128,282).
and increased SV are associated with an unchanged MAP The primary mechanoreceptors regulating vasopressin secre-
in HOWI. This observation is compatible with the view that tion appear to be the high-pressure arterial baroreceptors
SNA to systemic resistance vessels and heart are suppressed and cardiac volume receptors since plasma osmolarity does
during HOWI while cardiac vagal activity is enhanced. (263). not change (127, 128, 201, 333). It can be concluded that the
In contrast to the suppression of cardiac and vascular SNA depression of PRA and aldosterone levels are more consistent
in TN immersion cold water immersion (26-27◦ C) increased than changes in plasma vasopressin, and in addition seem to
vascular SNA (277). be less associated with the degree of hydration (111, 201).
It is unlikely that the diuretic and natriuretic responses to
HOWI are caused by suppression of aldosterone secretion as
Renal responses to intrathoracic volume expansion they appear after 20 min and thus too rapid in onset. It has
HOWI in a euhydrated subject causes a diuresis, natriuresis, been reported that renal responses to immersion were poorly
kaliuresis, and an increased free water clearance (CH2 O) correlated with right atrial pressure in awake dogs (153, 354).
(108, 109, 319). In nonvolume replete subjects, the renal It is clear that the primary increases in cardiopulmonary
responses gradually return to control levels over a 4 h and PV elicited by HOWI are wholly or partly compensated
period while in subjects that have fluid replacement the for by the renal responses. As seen in Figure 9, Gauer and
renal responses are sustained for the duration of immersion, Henry (130) were the first to demonstrate that stretching the
although at somewhat lower level. In subjects that are not cardiac atria causes a reflex diuresis (increased renal water
euhydrated the diuresis is reduced and thus osmolar clearance loss). In anesthetized dogs obstruction of the mitral valve
Volume 5, October 2015 1713
The Aquatic Environment Comprehensive Physiology
with a balloon catheter in the left atrium, resulted in reduced homeostasis. Jimenez et al. (183) immersed unprotected Navy
vasopressin secretion and elevated CH2 O. These responses swimmers for 6 h periods in 34◦ C, 18◦ C, and 10◦ C. In this
were abolished by cutting the cervical vagus nerves, indicating study, immersion in 34◦ C decreased PV by ∼7% after 6 h. Pro-
that PV is controlled by intrathoracic stretch receptors by way longed immersion at both colder water temperatures resulted
of cardiac reflex neurohumoral control of the kidneys as seen in a more rapid and greater reductions in PV (14.3%-16.3%).
in Figure 9. Plasma osmolarity did not change in TN water whereas
After 20 to 40 min of TN HOWI in euhydrated humans plasma osmolarity increased during the cold water immer-
the diuresis, natriuresis, kaliuresis, and increased renal free- sions. While GFR did not change at 34◦ C (consistent with
water clearance commence (108). As pointed out above, both other observations) the plasma hyperosmolar responses in
the hydration state and physical training have major quantita- cold water were associated with increases of GFR corre-
tive influences on the renal response to HOWI. The kaliuresis lated with significant renal losses of 1.6-1.7 L of water and
reflects tubular washout of potassium secondary to high urine sodium (6-8 g) and increases of osmolar and free water clear-
flow. In subjects who are well hydrated prior to immersion ances (185). PRA and vasopressin levels were unchanged
but then are not allowed to drink, the renal responses persist while aldosterone decreased similarly at all three temper-
for 2 to 4 h. Euhydrated subjects, on the other hand, maintain atures. Jimenez et al. (183) studied trained swimmers. As
a diuresis for the duration of the HOWI (4 h), although at a described above, training can influence the renal responses to
blunted rate. Dehydrated subjects, have less diuresis, but an immersion. Nevertheless, comparing studies of one hour vs
increase of osmolar clearance (19). Similar observations have six hour immersions suggests that progressive hypovolemia
been made in volume repleted and nonrepleted awake dogs develops with longer immersions in both TN and cold water
(354). There have been many studies of the renal response to secondary to increasing renal losses of water and sodium. It
HOWI in dogs; however, many of these animals were anes- might be expected that both hypovolemia and cold exposure
thetized which reduces their natriuretic response, so conclu- would lead to increases in SNA to peripheral vessels and the
sions about kidney regulatory mechanisms from anaesthetized kidneys causing salt and water retention. In this regard, it
studies are not valid (201). is surprising that GFR increased along with a diuresis and
Studies in humans confirm that PV increases in TN immer- natriuresis in the Jimenez (183) study. Perhaps prolonged
sion as reported from conscious animal studies. However, cold HOWI and/or cold water alters neurohumoral regulation of
water dramatically changes the pattern of body fluid shifts. renal function. Sramek et al. (357) studied subjects during 1 h
Stocks et al. (358) found that immersions limited to one hour immersions at 32, 20, and 14◦ C. In this study, subjects in 32◦ C
in 33◦ C versus 18◦ C water both caused reductions of intracel- had lower PRA, cortisol, and aldosterone, and the urine flow
lular volume of similar magnitude in humans. PV increased was increased by 107%. In the same study (357), in colder
in 33◦ C water accompanied by hemodilution. By contrast PV water the cortisol was decreased less, but the aldosterone lev-
decreased in 18◦ C water. Total body water remained constant els were greater. Metabolic rate increased by 350% at 14◦ C
whereas intracellular volume decreased by similar amounts in in this study (357) and it was associated with 530% increase
both TN and cold immersion. This indicates that, compared in NE and 250% for dopamine concentrations. Thus at colder
to TN immersion, movement of fluid out of the intracellular temperatures, there was an uncoupling of the relation between
compartment increases interstitial fluid volume during cold PRA and aldosterone, and SNA. Again it is surprising that
water immersion whereas PV decreases. Therefore, it is likely urine flow increased significantly more at 14◦ C than at 32◦ C
that microcirculatory dynamics during one hour periods of (163% vs. 107%) despite increases in antinatriuretic influ-
cold water immersion impair the entry of fluid from an ele- ences from aldosterone and sympathetic activity. Although
vated interstitial volume into the plasma compartment (358). strict comparisons of the Sramek (357) and Jimenez (183)
Atrial natriuretic peptide (ANP) is increased during cold water studies are not possible, the data suggest that altered neuro-
immersion. Since ANP reduces transcapillary fluid exchange humoral control of renal function may be more affected by
(201, 202), it is possible that ANP contributed to the reduc- water temperature than the duration of immersion. Although
tion in PV in cold water. This study indicated that changes renal responses to immersion are clearly altered by cold water
in PV were not associated with changes in total extracellular and vary among studies, the data from basic TN immersion
fluid volume at least in immersion (358). A further study by studies are consistent in demonstrating a diuresis and a natri-
Stocks et al. (358) established that acclimation to 14 days of uresis and that these responses are related to a decrease of
cold water immersion does not qualitatively or quantitatively PRA, aldosterone, and renal SNA.
alter the fluid shifts during 1 h HOWIs. Intracellular and PVs
were reduced by 5% to 6% while intercellular volume was
Vasopressin
increased by ∼ 5% before and after cold acclimation. Thus
during 1 h immersions in cold water intracellular fluid is dis- Vasopressin mediates the regulation of the total body fluid and
placed into the interstitium even after cold acclimation (358). plasma osmolarity. Since plasma osmolarity is not affected by
By contrast to observations of TN versus cold water HOWI, the control of vasopressin secretion likely depends
immersions for 1 hour periods immersions for longer peri- upon stimulation of volume receptors. Norsk and Epstein
ods appear to elicit more pronounced changes in body fluid (282) have indicated that a reduction in plasma vasopressin
1714 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
concentration causes increased CH2 O in humans during II (ANGII) levels declined also. The authors then infused
immersion. However, vasopressin levels are quite low in ANGII to keep plasma ANGII levels unchanged from control
euhydrated subjects and it has been difficult to detect reduc- levels during immersion. Infusion of ANGII markedly attenu-
tions in circulating vasopressin, although recent studies with ated the immersion natriuresis and reduced lithium clearance
improved vasopressin assays report consistently small but implying increased fractional distal reabsorption of sodium.
significant reductions in such subjects (128). By contrast, Thus reduced formation of ANGII is an important natriuretic
vasopressin concentrations are high in dehydrated subjects mechanism in humans immersed in water and the natriuresis
and decrease during immersion, but CH2 O does not increase. is in part due to decreased fractional distal tubular sodium
However, the kidney is quite sensitive to small changes in reabsorption.
plasma vasopressin (26), and the CH2 O response is abol- However, as emphasized above, the rapid onset of diuretic
ished when subjects are pretreated with vasopressin (110). and natriuretic responses suggest that they are not due to
Hammerum et al. (155) investigated plasma vasopressin in suppression of ANGII formation and aldosterone secretion.
hydrated subjects immersed in TN water with controlled Indeed, Hajduczok et al. (153) and Sondeen et al. (354)
sodium intake. In this study (155) vasopressin and CH2 O reported that renal responses of immersed awake dogs were
declined. Plasma vasopressin remained suppressed while poorly correlated with PRA.
CH2 O rose later in immersion. Collectively, the data indi-
cate that in humans the immersion diuresis can be related
Atrial natriuretic peptide
to suppression of vasopressin secretion. The level of hydra-
tion appears to determine whether an increase in CH2 O is Distension of the atria stimulates ANP release, eliciting
manifest. diuresis, natriuresis, and vasodilatation and fluid shifts from
In animal studies, Hajduczok et al. (153) found a diure- the vascular to extravascular compartment (301). HOWI
sis and natriuresis in awake dogs during water immersion increases ANP in plasma without delay in humans, dogs,
but no change in either vasopressin or CH2 O, despite large and rats (201). However, the relative time courses of the
increments in atrial pressure. By contrast, after total cardiac ANP and renal responses during immersion differ. For exam-
denervation, immersion led to a decline of vasopressin con- ple, although circulating ANP concentration rises rapidly, the
centration, with the diuresis due to an increased CH2 O. The diuresis and natriuresis are evident at 20 to 40 min. In fact,
Bainbridge reflex increases HR and CO in the intact dog it is uncertain whether these renal responses can actually be
during water immersion due to increased venous return and elicited by the levels of ANP that are attained during water
stimulation of the low-pressure baroreceptors, while arterial immersion (149), and the renal responses are poorly corre-
PP does not change. However, after cardiac denervation, the lated with plasma ANP concentrations (254, 354). The renal
increase in HR is abolished, since it was driven autonomically, responses to ANP were greatly augmented in hypervolemic
but CO increased the same as the preload-induced elevation in (but not hemodiluted) awake dogs (253). Subsequently, it
SV was similar, and arterial PP was increased. These observa- was demonstrated that the renal sensitivity to two doses of
tions indicate that, in the dog, the decline in circulating vaso- ANP was greatly augmented in conscious dogs during volume
pressin was due to increased high-pressure arterial barorecep- replete water immersion (202). These observations indicate
tor loading, unmasked by cardiac denervation. Furthermore, that the renal response to ANP is greatly potentiated when the
the natriuresis was dependent upon intact cardiac nerves. It is, PV is expanded. ANP reduces PV and increases hematocrit
therefore, evident that considerable redundancy exists within by causing a transcapillary shift of fluid out of the plasma
the control systems for body fluid regulation, as is evident compartment (334). In awake dogs, it has been shown that
for other regulatory systems. In awake dogs, monkeys, and ANP infusion caused a hemoconcentration in air (202). Dur-
humans, the major mechanoreceptors regulating vasopressin ing water immersion, there was an expected hemodilution.
secretion are likely arterial baroreceptors (201,333), although However, the immersion hemodilution was attenuated in a
graded distension of central cardiac receptors modulates vaso- graded fashion by increasing doses of ANP. Thus, ANP mod-
pressin secretion in humans (128). ulates and opposes the autotransfusion during water immer-
sion, possibly by raising capillary hydrostatic pressure (201).
Renin-angiotensin II-aldosterone system
The renin-angiotensin-aldosterone system and the renal sym-
pathetic nerves are antinatriuretic, and interact with ANP to
Nitric Oxide
regulate extracellular fluid volume and plasma sodium con- Nitric oxide (NO) is synthesized in the kidney and is natri-
tent. In immersed humans, the decrease in PRA and aldos- uretic. Djikhorst-Oei et al. (91) reported that there is inhibi-
terone concentrations are more consistent than changes in tion of renal NO synthesis on renal hemodynamics and renal
plasma vasopressin, and are less associated with the sub- function during 7 h of TN HOWI. During the timed con-
jects’ hydration (109, 201). Schou et al. (340) demonstrated trol immersion with infusion of placebo, arterial pressure and
using lithium clearance that fractional distal tubular reabsorp- renal vascular resistance declined while there was a natriuresis
tion of sodium is reduced during TN immersion. Angiotensin and diuresis.
Volume 5, October 2015 1715
The Aquatic Environment Comprehensive Physiology
A second immersion study was carried out with infusion of that the roles of vasopressin, aldosterone, and ANP are less
l-NMMA (N(G)-monomethyl-l-arginine) to inhibit NO syn- important. Neurohumoral control of renal function in water
thesis. Prior to immersion l-NMMA decreased the [(15)N- immersion is mediated by low-pressure cardiopulmonary and
arginine to [(15)N]-citrulline conversion rate with profound the high-pressure arterial baroreceptors. Since vasopressin
elevations in arterial pressure and reduction of sodium excre- only declines during immersion in awake dogs after cardiac
tion and urine flow. When the subjects were then immersed denervation there may be a shift in neurohumoral regulation
during l-NMMA infusion, there were relative reductions in of renal function from the cardiopulmonary baroreceptors and
arterial pressure and renal vascular resistance and increases in arterial baroreceptors. Indeed, it has been demonstrated that
sodium excretion and urine flow that did not differ from those in awake dogs water immersion selectively increased central
induced prior to NO inhibition. The authors concluded that input from the cardiopulmonary baroreceptors that acts to
although NO synthesis was estimated to be reduced to one- simultaneously inhibit arterial baroreceptor control of renal
third of control levels, the kidney continues to be sensitive to SNA (260). This indicates that the major reflex input that regu-
volume expansion from HOWI resulting in renal vasodilation lates renal function during TN water immersion in the neurally
and natriuresis and diuresis. These data support the view that intact state is from the low-pressure cardiopulmonary barore-
multiple redundant mechanisms are available to bring about ceptors. The potential contribution from the arterial barore-
the renal response to the volume expansion of immersion. ceptors is unmasked by cardiac denervation. These conclu-
sions are derived from studies in quadruped dogs. Additional
effort is essential to fully understand the relative contributions
Renal sympathetic nerves
of low vs high pressure baroreceptors in biped humans.
DiBona and Kopp (90) and others have shown that renal SNA
can elicit important modulation of kidney function even with-
Circadian influences and intrarenal starling forces
out renal hemodynamic changes. For example, renal sympa-
thetic activation at intensities that have no effect on renal In addition to the denervation and neural recording studies
blood flow or glomerular filtration causes antinatriuresis, in animals, the differential effects of neural versus hormonal
whereas suppression of renal neural activity evokes a natri- control were clarified further by experiments showing a dra-
uresis. Mechanical stretch of atrial or arterial baroreceptors matic circadian influence on the renal response to immer-
results in significantly decreased renal SNA, increasing urine sion in humans. The renal responses to TN HOWI have been
flow, as well as sodium excretion. In addition to this suppres- reported to be attenuated at night (205). Subsequently, these
sion, it has been shown that plasma NE concentration declines observations were confirmed and further showed that the ele-
by as much as 50% during water immersion (111, 281). Haj- vation of CO and the reduction in PRA, aldosterone, and vaso-
duczok et al. (153) found in dogs with denervated hearts pressin were similar during the day and night was confirmed
that the natriuresis of water immersion was entirely due to (344). Later, it was reported that elevations of ANP during
the presence of the cardiac nerves, although a water diuresis HOWI at night were similar to those during the day, despite
persisted in the cardiac-denervated dogs, due to a decline of nocturnal suppression of the diuretic and natriuretic responses
vasopressin levels. Thus, the reflex suppression of adrenergic (259). Since the day versus night hormonal responses were
systems in water immersion is dependent upon the stimula- similar, by exclusion, these circadian studies imply that a
tion of cardiac afferent nerves, and major alterations in vaso- reduced reflex suppression of renal SNA at night is respon-
pressin do not occur in neurally intact animals. The decline sible for the attenuated diuresis and natriuresis during water
in PRA usually observed in HOWI is, therefore, likely to be immersion.
related to a decline in renal SNA. Recording of renal SNA It has been well documented that the kidneys respond
activity in awake dogs, provided the first direct evidence that to increased arterial pressure with a rise in interstitial pres-
SNA is suppressed during water immersion (257). The magni- sure, and this causes pressure-induced diuresis and natriuresis
tude of this neural activity suppression was about 50% below (72). However, it has been demonstrated that the immersion-
preimmersion levels, and the renal response in these dogs induced natriuresis was abolished after cardiac denervation,
consisted of diuresis and natriuresis, with no change in renal despite similar elevations in MAP (153), and that abolition
CH2 O. After chronic bilateral renal denervation, the diure- of the natriuresis and diuresis following renal denervation
sis and natriuresis in HOWI were eliminated. Subsequently, occurred despite similar elevations in MAP (257). Thus,
strong evidence was reported that immersion elicits a car- increased renal arterial pressure does not appear to contribute
diac reflex neurogenic natriuresis, since this natriuresis was in a major way to the water immersion natriuresis. Auto-
also abolished by denervation of the heart (257). Later, it was transfusion during upright immersion causes a hypervolemic
demonstrated that the decline in renal SNA and increased hemodilution and a decline of plasma colloid oncotic pressure.
sodium excretion during water immersion were greatly atten- The latter would diminish the tubular reabsorptive capacity for
uated in cardiac-denervated awake dogs (258). The dramatic sodium, contributing to natriuresis. Using graded immersions
consequences of renal and cardiac denervation emphasize the in humans when thigh cuffs were inflated to reduce fluid shifts
important role of reflex suppression of renal sympathetic acti- from the legs, it has been postulated that the decline in plasma
vation in the renal responses to water immersion, and imply colloid oncotic pressure could be responsible for a significant
1716 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
amount of the elevated sodium excretion observed during from studies in air where CO is increased (328). The regula-
water immersion (187). On the other hand, as indicated above, tion of blood flow in the lung is likely due to active vascular
the hemodilution response in humans during HOWI revealed responses to HOWI, and not as dependent on gravity as previ-
minimal circadian influences, yet the natriuretic responses are ously reported. It can be concluded that higher blood flow to
suppressed at night, reinforcing the primary impact of renal pulmonary capillaries is responsible for increased lung blood
sympathetic nerves in mediating immersion-induced natriure- volume, as recruiting additional capillaries does not appear to
sis and diuresis. occur (114,298,328). The high levels of pulmonary blood flow
and pressure in HOWI may lead to failure of the capillary wall
and, in some cases, result in pulmonary edema and sometimes
Effects of exercise during immersion on renal
hemorrhage, particularly during exercise (see below, under
function
“Immersion Pulmonary Edema”). During HOWI hydrostatic
It is well documented that exercise carried out on land results pressure compresses the body’s fluid and gas containing com-
in vasoconstriction of blood flow to the kidney and thus blunts partments, thus breath-hold dives can lead to “lung-squeeze”
the diuresis and increases sodium reabsorption (333). Dur- with hemorrhage and edema due to the compression of the
ing HOWI where at rest there are diuretic and natriuretic gas containing compartments (220).
responses, exercise attenuates these response and potentiates As opposed to the depressing effects of a gradual immer-
the kaliuretic response (326). These exercise-associated alter- sion on HR, a rapid immersion in 0◦ C water results in an
ations are likely the effect of increased SNA blunting the sudden increase in HR, respiratory rate and tidal volume with
mechanoreceptor-mediated suppression of renal SNA during an associated decrease in end-tidal CO2 (237). However, pro-
HOWI. In addition, plasma renin and aldosterone remained longed exposure to cold water results in decreased ventilation
unchanged while vasopressin was significantly increased and breathing frequency (Bf ), and this was the case even if
(326). torso or legs were protected (379). HOWI has been shown to
increase CVs in TN water. On the other hand, ERV decreased
in immersion and the alveolar plateau (Phase III) slope was
Pulmonary adjustments less steep (86).
The HOWI-induced CO induces an increase in pulmonary HOWI increases the demands on the respiratory system
blood flow, causing elevation of pulmonary artery blood vol- due to the hydrostatic pressure differential between the feet
ume and pressure. The changes in blood volume result in and chest and the translocation of blood to the chest discussed
increased residual volume and decreased VC (171, 227). The above. If the person is breathing with a snorkel, or SCUBA,
compression of the chest wall causes elastic loading and nega- there is likely an increase in breathing resistance. In addition to
tive pressure breathing (171, 227, 368). The negative pressure the increased SLL described above, the effects of HOWI cause
breathing has an effect on pulmonary mechanics, causing ele- increased WOB at both rest and during exercise (162,322). In
vated pressure difference between the outside of the chest addition, during HOWI, there is a translocation of blood from
and the alveolar air pressure (SLL) (227). Increased SLL the dependent limbs to the chest (11, 201, 368), resulting in a
results if the source of breathing gas (breathing regulator) decrease in total lung capacity, residual volume (171,228,363)
is at a different hydrostatic pressure than the lung centroid and lung compliance (227, 228). The sum total of the HOWI-
(228, 366, 369). SLL is typically negative during immersion induced changes in lung volume increase the elastic WOB.
and submersion due to the negative body attitude, even dur- HOWI causes increased airway resistance (Raw) (162).
ing exercise (228), when the mouth is at lower pressure than The increases in resistance would demand a concurrent
the chest which increases the force required by the inspira- increase in alveolar pressure (PA ) to maintain VE . Airway
tory muscles, while assisting expiration. The elevated SLL resistance has been shown to be modulated by NO (4). It
has been reported to increase ERV (227, 364, 365), resulting has been reported that synthesis of, or administration of NO
in the respiratory muscles being stretched to a less functional results in a decreased airway resistance in a dose-dependent
length resulting in a reduced force development and mainte- manner (103, 166) and due to the increased airway resistance
nance (39,247). The inadequate force may not be sufficient to in HOWI NO production is blunted during HOWI. Ventilation
accomplish the increased total work of breathing (WOB) and in water is also dependent on the water temperature on the face
may lead to respiratory muscle fatigue. The increased total (82). A recent study proposed that the increased inspiratory
WOB demands more O2 increasing the demand for blood force needed to overcome negative SLL during immersion
flow to the respiratory muscles (154, 162), which may also resulted in increased breathing cycle, that is, increased Bf
reduce blood flow and O2 delivery to other skeletal muscles (162).
(158). Immersion results in a decrease in WOB for each breath
HOWI has been reported to increase lung CV in humans, that is a result of the decrease in resistance for that individ-
and may lead to slight hypoxemia (314). It is widely accepted ual breath, and thus WOB ̇ per breath was less. The expira-
that there is increased blood flow to apical regions of the lung ̇
tory WOB per breath was unaffected by immersion. Negative
(11). Its effect on VA /Q depends on the relationship between SLL increases the inspiratory effort to overcome the nega-
CV and ERV as discussed earlier (114,298) and can be implied tive pressure and likely explains the total WOB ̇ changes due
Volume 5, October 2015 1717
The Aquatic Environment Comprehensive Physiology
Regional blood distribution in the lung to decreases in ETCO2 and cerebral vasoconstriction reflected
400 at various levels of water immersion by a decline of middle cerebral artery velocity and is sufficient
to cause disorientation and loss of consciousness (236).
Regional lung volume (counts/pixel)
350 Cooling and heating during HOWI can affect contractile
properties (force generation) of muscle. However, HOWI does
300 not result in changes in muscle fascicle, tendon, and aponeu-
Region 1
Region 2 rosis were during passive stretch, and in addition there was no
250 Region 3
Region 4 change in contractile performance of muscles (206). Another
Region 5 study found that HOWI was associated with a decrease in
200 Region 6
Region 7 maximal voluntary contraction of plantar flexors and the elec-
Region 8
150 Region 9 tromyography amplitude, as well as the Hofman and Achilles
tendon reflexes and these data imply that there is a triggering
100 of inhibitory mechanisms (313).
0
0 Air Knee Hip Xyphoid ss Modulating factors
Water immersion level
Hydration
Figure 10 Regional lung volume determined by radioactive labeling Various fluid supplementation protocols have been applied
of red blood cells is plotted as a function of the depth of water immersion
(progressive increasing pulmonary blood flow). The lung was divided
during extended water immersion, with the idea of helping
into nine equal layers from the apex to the top of the lung. The slopes of to sustain the blood volume and are based on the assump-
the increase in lung volume as a function of increasing cardiac output tion that the PV declines in HOWI (131). Protocols have
for the nine layers were not significantly different from each other. In
parallel measurements diffusion capacity (DLCO) was measured and
included hourly boluses of water and replacement of fluid
confirmed the increase in pulmonary blood volume was a result of cap- losses with saline, resulting in a water diuresis. However, due
illary enlargement, and not capillary recruitment (data not shown). to immersion-induced autotransfusion, the assumption that
there is reduced PV is incorrect, and the rationale for partic-
to immersion where negative SLL is increased (162). Dur- ular hydration protocols has never been entirely clear (201).
ing immersion, the energy cost of breathing is increased as a
result of the increased total WOB and a decrease in the net
Egress from water immersion
mechanical efficiency of the respiratory muscles (162, 351).
HOWI results in decreased PaO2 and alveolar-arterial O2 Upon exiting the water, the fluid shifts experienced during
difference and increased CO-transfer factor, due to the redis- immersion are reversed, causing reductions of PV and thus
tribution of lung perfusion to the apical lung (223). How- CO, and favoring orthostatic intolerance (35). Although CO
ever, VE in relation to functional residual volume does not is elevated during diving at rest and low exercise levels (209)
change in immersion (223). HOWI in 35◦ C water has been due to immersion, a decrease in CO due to reduced SV has
shown to increase VE while shunt, VA /Q, and the perfusion been shown after a dive (29, 102). It is unclear how long this
distribution were unaffected (88). More recent studies using depressed cardiac function lasts, or if it is persistent until the
nuclear techniques and diffusion capacity data have shown next dives or accumulates with repeat dives.
that the increased pulmonary blood flow due to HOWI results A recent study has shown that both decreased SNA and
in increased volume of blood in the capillaries (capillary increased para-SNA followed 6 h in-water immersion when
engorgement), as opposed to the opening of more pulmonary PV was significantly reduced (117). By contrast, they reported
capillaries at the top of the lung (capillary recruitment) as seen that aldosterone, ANP, AVP, and NE were unchanged postim-
in Figure 10 (114, 298, 328). Increases in lung blood volume mersion. Importantly, they also showed that cardiovascular
during HOWI is shown in Figure 10. The capillary engorge- and autonomic control are not sufficient to prevent orthostatic
ment, when combined with increased MAP due to exercise intolerance postimmersion (117).
and the vasoconstrictor effects of cold water may predispose
subjects to pulmonary edema. These studies also show that
the capillary engorgement is sustained for 6 h of HOWI. Gender
Cutaneous cold-induced vasodilation has been reported to not
be different between men and women during HOWI (30 min
Cortical and neuromuscular responses at 9◦ C) of the hand (148, 378). Cutaneous cold immersion
Sustained HOWI (34◦ C) increases the activity of both sen- resulted in increased SNA of the hand and reduced blood flow
sory and motor areas of the cortex (339), influencing cortical in both females and males (176) with equal time courses and
processing of somatosensory inputs (337). Rapid immersion magnitude. In addition, the rates of decreases in deep Ts was
in cold (0◦ C) water results in an immediate increase in HR, similar between the genders (234). When differences in body
respiratory rate, and tidal volume. The hyperventilation leads size are considered, the cardiovascular or renal responses to
1718 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
TN HOWI are likely similar (408). While short-term ventila- sympathetic suppression induced by TN HOWI (262). Older
tion with immersion have not been reported to be different in subjects have a blunted increase in SV and CO in TN HOWI
men and women, during cold, HOWI females were shown to to both the shoulder and neck (302). SBP and TPR decrease
have a greater increase in ventilation than males (176). During in response to HOWI, however less so in the elderly. Ectopic
HOWI in water below TN temperature, no gender differences arrhythmias occurred regularly in elderly, but not in young
have been reported after correction for body fatness and sur- subjects. In elderly subjects, blood pressure is elevated in
face area in either the physiological or metabolic responses HOWI, in spite of the blunted increase in SV and constant
(378). Thus, the above description of responses to water HR suggesting that vasoregulatory mechanisms dependent
immersion can most likely be applied to both men and women on the baroreceptor reflex diminish with age (361).
(148). However, one study reported that in water of 20◦ C, the No difference in thermosensitivity, mean Ts , metabolic
drop in Tc was greater in women than men, but only after cor- heat production, Tc and slope of Tc and heat production were
rection of body fat content at rest and low levels of exercise, observed between old and young during HOWI for 40 min
while no differences were seen at higher exercise levels (230). in 20◦ C (147). Sensory perception determined by cold hand
Still another study showed that the time course of changes in immersion detection threshold was higher in older subjects
deep Ts are not different between men and women (176). and required a greater noxious stimulation to reach the thresh-
In TN HOWI, the increases in CO and SV and unchanged old for pain (407).
HR and BP, and a decrease in TPR, at rest were not different Older subjects have been reported to have more shunt
in adult men and women (428). No significant difference in blood flow in the lungs than younger subjects resulting in
atrial diameter, HR, BP, urine volume, osmolality, endothe- lower perfusion areas and perfusion distributions showing
lium, urodilatin, sodium, and potassium excretion were found more inequality in VA /Q (88). No temporal changes were
between men and women (408). However, in females urodi- seen in old or young subjects over 30 min. In young subjects,
latin excretion per kilogram was reported to be higher and CV increased 77%; however, it was below the tidal breath-
there was a delay in the kaliuretic response, while men had a ing range upper limit. However, in older subjects, CV only
greater potassium excretion, presumably due to greater body increased 34% and was not different from the tidal breathing
mass (408). range. While the absolute volume change during HOWI is not
Thermosensitivity, as judged by limb blood flow, was dependent on age, ERV was decreased both groups but was
shown to not be significantly different between genders lower in older.
immersed in cold water (20◦ C), and the phase of the men- In spite of a lesser elevation of CO in older subjects, their
strual cycle of the females did not affect limb blood flow natriuretic response to HOWI was augmented, with increased
(148). This is supported by the data of a study that reported GFR (361) in spite of a decline in pressure-dependent sodium
in women of high versus low body fat the Ts or total body and water excretion in older subjects (395). Nocturnal urine
insulation were not different; however, the fatter group main- production increases with age after 50 years, with increased
tained a higher Tc than the thinner group, presumably due to urination frequency being reported during supine position dur-
increased body insulation (315). ing sleep when CO is increased (28). Similarly, the renal
Responses of BP, HR, and CO and TPR were similar responses to HOWI are attenuated at night in young subjects;
during exercise, and there was no significant effect of age this may not be the case in elderly subjects (205, 344).
or acclimation (428). In 28◦ C, the drop in Tc was inversely
related to exercise VO2 ; however, this was not the case in 20◦ C
water in either men or women (230). It has been shown that no Exercise in Head-Out Water Immersion
gender adjustments are necessary for the metabolic pathways
during shivering or prediction models of cold exposure, as The modes of exercise in the aquatic environment are man-
long as percentage of body fat and the ratio of body surface ifold and so are their respective physiological responses. In
area to size are taken into account (378). this section, this topic will be covered by dividing the modes
of exercise in water into two main categories.
Age
1. Water locomotion. The energy requirements of cyclic type
It has been reported that the well documented increase in activities such as swimming, rowing, and kayaking can be
CO in young subjects during HOWI is blunted in older appropriately described by measuring their “cost of trans-
subjects (302). In TN HOWI, older subjects had less sensitive port” (C). It will be shown how this parameter depends
spontaneous baroreflex sensitivity than younger subjects on the speed and the mode of locomotion and how C is
based on the variation of HR (390). This may be due, in part affected by “biomechanical” factors such as hydrodynamic
to older subjects having less carotid arterial compliance than resistance and propelling efficiency; the former is larger,
young, and increased systolic blood pressure (SBP) (390). the higher the speed, and the wetted area of the immersed
SNA is depressed in all subjects during TN HOWI; however, body/boat, the latter is larger, the greater the distance cov-
there is much less suppression in the older subjects (262). ered per cycle. These forms of exercise in water could
In fact, there is an inverse relationship between age and the also be defined as “competitive aquatic sports” even if this
Volume 5, October 2015 1719
The Aquatic Environment Comprehensive Physiology
definition includes other activities (such as water polo and 2.5
synchronized swimming) that will not be considered here.
2. Water-based activities. These are performed in HOWI 2.0
(e.g., water walking, water running, and water fitness).
The main difference between these activities and the other
competitive aquatic sports is in their aim: while the former 1.5
E (kw)
are mainly performed to improve an athlete’s performance,
water-based activities are mainly performed to maintain L
·
and improve health in the general population, and/or as a 1.0 UWF
rehabilitation mode for athletes and patients. These activ- AL
ities can be carried out with or without specific equipment K
and their energy demands depend essentially on two “water 0.5
R
characteristics”: buoyancy and drag. The former is larger
the deeper the immersion level of the body/body parts, the
latter is larger the greater the frequency and the amplitude 0
of the movement of the submerged body parts. 0 1 2 3 4 5 6
υ (m · s–1)
Water Locomotion: Energetic and Figure 11 Net energy expenditure (E′ , kW) is plotted as a function
of the speed (v, m . s−1 ) for different forms of aquatic locomotion (orig-
Mechanical Determinants inal data were interpolated over the aerobic speed range, see text for
details). L: swimming by using the leg kick at the surface; UWF: under-
As is the case for land locomotion, locomotion in the aquatic water swimming with SCUBA diving equipment; AL: swimming the front
environment can be sustained with or without locomotory crawl; K: kayaking; R: rowing. Taken from Pendergast et al. (308) with
permission.
tools; these tools do not supply additional energy but provide
effective compensation for the limitations in our anatomical
design and for inadequacy in muscle performance (2, 261); where E′ is metabolic power expenditure and v is the speed
their effects on the energetics and mechanics of water loco- of progression. Expressing the velocity as m . s−1 and E′ in
motion allow to better understand the general principles that kJ . s−1 , C results in kJ . m−1 (94): (it represents the energy
determine the physiological responses in this environment; expended to cover a specific distance at a given velocity).
for this reason, data referring to some of these tools (i.e., fins, Equation 1 indicates that, for a given metabolic power, the
kayak, and rowing shell) will be presented in the following locomotion speed will depend on the differences in C among
paragraphs, along with data referring to the swimming strokes locomotion modes. This is shown in Figure 12 where the
(the “unaided” cyclic modes of water locomotion). energy cost of the forms of locomotion considered above is
In Figure 11 (adapted from 308) the metabolic power reported. The solid lines are the iso-metabolic power hyper-
expenditure (E′ , kW) of different forms of aquatic locomo- bolae of 0.5, 1.0, 1.5, and 2 kW. For the same metabolic
tion is reported as a function of the locomotion speed (v, power (e.g., 0.5 kW), the locomotion speed will be larger in
m . s−1 ): surface swimming with leg kick (barefoot) (E′ = the forms of locomotion with the lower C, that is, from about
0.91 . v1.75 ), fin swimming below the surface with SCUBA 0.6 m . s−1 in SCUBA diving to about 2.4 m . s−1 in rowing.
diving equipment (E′ = 1.08 . v1.39 ), front crawl swimming For a swimmer, or a boat, to progress in calm water at a
(E′ = 0.60 . v1.87 ), kayaking (E′ = 0.098 . v2.76 ), and rowing specific, constant, velocity, the propulsive force must be equal
(E′ = 0.088 . v2.05 ). The equations listed above are determined to the sum of the resistances opposing locomotion. Thus, the
from reanalyzing the original data (92,299,338,431,438) with increase in E′ with the speed mirrors the increase in (total)
power functions over the aerobic speed range. As indicated mechanical power output (Wtot ′ , kW) that the swimmer has
by Figure 11, metabolic power increases sharply as a function to supply to maintain that velocity (261). Figures 11 and 12
of speed and, at similar velocities, it is greater for leg kicking indicate, therefore, that the speed of locomotion is a “mea-
(both underwater and at the surface), slightly lower for the sure” of the intensity of exercise and that, for a given form of
front crawl and lower by a significant amount in kayaking aquatic locomotion, the physiological responses to exercise
and rowing. depend on (could be graded based on) the locomotion speed.
The energy expenditure of cyclic forms of locomotion As for land locomotion, the total mechanical power of
such as those indicated above, can be expressed not only as aquatic locomotion (Wtot ′ ) is the sum of two terms (e.g., 50):
a function of time (e.g., L O2 . min−1 or kJ . s−1 ) but also as the power required to move the limbs with respect to the centre
a function of the distance covered, by calculating the energy of mass (the internal power, Wint ′ ) and the power required to
cost per unit distance (C) as: compensate for external forces (the external power, Wext ′ ):
C = E′ v−1 (1) ′
Wtot ′
= Wext ′
+ Wint (2)
1720 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
1.5 ηP . Propelling and Froude efficiency refer to the mechanical
partitioning only, whereas the performance and the overall
L
efficiency take into account also the energy expenditure. The
UWF
efficiency with which metabolic power input (E′ ) is trans-
AL
formed into useful mechanical power output (Wd′ ) is termed
1.0 K performance (or drag) efficiency (ηd ) and is given by:
R
C(kJ · m–1)
ηd = Wd′ ∕E′ (6)
The efficiency with which metabolic power input (E′ ) is
0.5 transformed into mechanical power output (Wtot ′ ) is termed
overall (or gross or mechanical) efficiency (ηO ) and is given
by:
′
ηO = Wtot ∕E′ (7)
0
0 1 2 3 4 5 6 It follows that: ηO = ηd /ηP . Combining Eqs. (5) to (7) one
υ (m · s–1) obtains:
Figure 12 Net energy cost (C, kJ . m−1 ) is plotted as a function of the E′ = Wd′ ∕(ηP ηO ) (8)
speed (v, m . s−1 ) for different forms of aquatic locomotion (original data
were interpolated over the aerobic speed range, see text for details).
The continuous lines represent iso-metabolic power hyperbolae of 0.5, that relates the metabolic power input (E′ ) with the power
1.0, 1.5, and 2 kW (from bottom to top). L: swimming by using the leg needed to overcome hydrodynamic resistance (Wd′ ) and with
kick at the surface; UWF: underwater swimming with SCUBA diving
equipment; AL: swimming the front crawl; K: kayaking; R: rowing. Taken
propelling (ηP ) and overall (ηO ) efficiency, at a specific veloc-
from Pendergast et al. (308) with permission. ity.
Since, for any given speed, C = E′ /v and Wd′ = Wd . v:
For aquatic locomotion Wext ′ is comprised of two factors:
C = Wd ∕(ηP ηO ) (9)
the power to overcome drag, generating thrust (Wd′ ), and that
that does not add to the thrust (Wk′ ): that relates the energy cost of locomotion with the work, per
unit distance, that is necessary to overcome hydrodynamic
′
Wext = Wd′ + Wk′ (3) resistance (Wd ) and with propelling (ηP ) and overall (ηO ) effi-
ciency, at a specific velocity. For further details, see Zamparo
Both Wd′ and Wk′ accelerate water giving it kinetic energy et al. (433).
but only Wd′ contributes to propulsion (e.g., 8, 80). The Equations (8) and (9) show that differences in E′ (or in
efficiency with which the external mechanical power pro- C) among locomotion modes in water, at any given speed and
duced the swimmer/kayaker/rower is transformed into “use- for a specific ηO , depend on differences in ηP and/or in Wd′
ful” mechanical power (thrust) is termed Froude (theoretical) (or Wd ); it also indicates that, for a given locomotion mode,
efficiency (ηF ) and is given by: increasing ηP and/or decreasing Wd′ (or Wd ) would result in
decreased E′ (or in C). The justification for this postulate is
ηF = Wd′ ∕Wext
′
(4) discussed in the following paragraphs.
All cyclic forms of locomotion involve the intermittent
The efficiency with which the overall mechanical power application of forces: the mean velocity (v, m . s−1 ) is indeed
produced by the swimmer/kayaker/rower is transformed into the product of the cycle frequency (f, cycle . s−1 , Hz) and of
“useful” mechanical power (thrust) is termed propelling effi- the distance covered per cycle (dc , m . cycle−1 ) (e.g., 75). As
ciency (ηP ) and is given by: shown by Figure 13 (which reports the f vs. v relationship
in the forms of locomotion in water taken as an example)
ηP = Wd′ ∕Wtot
′
(5) each mode of locomotion is almost univocally defined by its
dc : surface leg kicking = about 0.5 m . cycle−1 ; underwater
This parameter (ηP ) is of utmost importance in water fin swimming with SCUBA diving equipment = about 1 m
locomotion since it indicates the capability of the swim- . cycle−1 ; front crawl swimming = about 2.5 m . cycle−1 ;
mer/kayaker/rower to transform at best his or her muscular kayaking = about 4 m . cycle−1 ; and rowing = about 8 m .
power into power useful for propulsion. Propelling efficiency cycle−1 . These differences have to be attributed (at least in
could vary from 0 (none of the power provided by the muscles part) to the length of the “propelling tool” (i.e., arms, legs,
is useful for propulsion) to 1 (all power is utilized for propul- paddles, or oars) but essentially indicate the capability of the
sion); if the internal power (Wint′ ) is nil or negligible η = swimmer/rower/kayaker to exert useful forces in water: the
F
Volume 5, October 2015 1721
The Aquatic Environment Comprehensive Physiology
150 150
L
UWF
100 100
AL
ƒ(cycles · min–1)
D (N)
R
L
50 50 UWF
AL
K
R
0 0
0 1 2 3 4 5 6 0 1 2 3 4 5 6
υ (m · s–1) υ (m · s–1)
Figure 13 Cycle frequency (f, cycles . min−1 ) is plotted as a func- Figure 14 Active/passive drag (D, N) is plotted as a function of
tion of the speed (v, m . s−1 ) for different forms of aquatic locomotion the speed (v, m . s−1 ) for different forms of aquatic locomotion (origi-
(original data were interpolated over the aerobic speed range, see text nal data were interpolated over the aerobic speed range, see text for
for details). The average distance the body/boat travels per cycle (dc , details). L: swimming by using the leg kick at the surface; UWF: under-
m . cycle−1 ) is indicated by the continuous lines irradiating from the water swimming with SCUBA diving equipment; AL: swimming the front
origin. L: swimming by using the leg kick at the surface; UWF: under- crawl; K: kayaking; R: rowing. Taken from Pendergast et al. (308) with
water swimming with SCUBA diving equipment; AL: swimming the front permission.
crawl; K: kayaking; R: rowing. Taken from Pendergast et al. (308) with
permission.
To understand the physiological demands of cyclic forms
of aquatic locomotion, it is therefore sufficient to measure the
power available for propulsion (Wd′ ) is indeed responsible locomotion speed and to know the E′ versus v (the C vs. v)
for the distance the body/boat travels per cycle, as originally relationship of that locomotion mode. A deeper understand-
indicated by Craig and Pendergast (75); dc is thus an index of ing of the energetics of aquatic locomotion can be obtained
propelling efficiency and these two parameters were indeed by assessing the hydrodynamic resistance and the propelling
found to be related: ηP = 0.46 . dc 0.21 (R = 0.78), as shown by (and overall) efficiency of the locomotion at stake. These are
Pendergast et al. (308) for these forms of water locomotion. not easy tasks in this environment and in the following sec-
The power to overcome drag (Wd′ , W) is given by: tions a survey of the techniques mostly used to assess these
Wd . v, where v is velocity (m . s−1 ) and Wd is the work parameters are reviewed.
to overcome drag in the unit distance (J . m−1 = N), Wd has
thus the same units and significance of hydrodynamic resis-
tance (D, N). Hydrodynamic resistance increases as a function Measurement of E ′ , W ′ d , and ηP in the water
of velocity in a similar fashion as E′ and C as seen in Figure environment
14; at comparable (paired) speeds D is larger in underwater
Metabolic power (E ′ )
fin swimming (SCUBA diving, D = 115.7 . v1.57 ), slightly
lower for kicking at the surface (D = 42.9 . v1.55 ) and the The large majority of aquatic locomotion studies report data of
front crawl (D = 49.8 . v1.03 ) and significantly reduced for submaximal energy expenditure after steady state conditions
boats locomotion A rowing shell (D = 12.8 . v1.33 ) offers a are attained, a condition for which is not necessary to esti-
lower resistance to motion than a kayak (D = 14.5 . v201 ) (see mate the role of anaerobic energy sources, the determination
308). of which, as indicated below, is based on several (and some-
Taken together, the differences in ηP (or dc ) and D can times debated) assumptions. Metabolic power (E′ ) at constant,
thus explain the differences in E′ (and C): as an example: (i) submaximal (aerobic) speeds can be calculated by measuring
in SCUBA diving ηP (dc ) is larger than when leg kicking at the the oxygen consumption after a steady VO2 is obtained (VO2 ss )
surface but the former demands more energy than the latter using standard open-circuit techniques. Under this condition,
because its D is larger; (ii) the similar values of D between leg energy expenditure is based only on “aerobic energy sources”
′
(E′ = EAer = VO2 ss ) (93). Douglas bags, balloons, or portable
kicking and front crawl swimming indicate that the primary
difference in the metabolic power (E′ ) or in the energy cost metabolimeters can be utilized to measure continuously VO2
(C) between these two forms of locomotion must be in their during exercise but often this is a challenging task in the water
relative propelling efficiencies (in their dc ). environment. An alternative way to assess VO2 ss is to use the
1722 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
“back extrapolation technique” where breath by breath oxy- Table 1 Percentage contribution of aerobic (EAer ), anaerobic lactic
gen consumption is taken during the first 30 to 45 s immedi- (EAl ), and anaerobic alactic (EAnAl ) energy sources to overall energy
expenditure during maximal swimming trials (average for the four
ately postexercise (e.g., 327, 431). From the linear regression strokes) over three distances (adapted from 46) and during maximal
of the logarithm of the VO2 values as a function of recovery trials on the Olympic kayak over four distances (adapted, with permis-
time, VO2 can be backward extrapolated “at time zero” and sion, from 434).
the VO2 ss can be estimated (e.g., 71, 269, 270).
Since VO2 reaches a steady state value (at muscular level) Distance Time Speed EAer EAl EAnAl
with a time constant (τ) of about 30 s (330), the methods (m) (s) (m/s) (%) (%) (%)
indicated above could also be applied to measure the aerobic
contribution to metabolic power (Eaer ′ ) in maximal trials last-
Swimming 45.7 25.9 1.76 19.2 54.8 26.0
ing at least 2 to 3 min (e.g., more than 4-5 τ). In these cases,
Swimming 91.4 57.5 1.59 37.4 44.2 19.4
the anaerobic lactic energy contribution to metabolic power
′ ) plays a significant role, the more so the shorter the exer-
(EAnl Swimming 182.9 126.6 1.45 62.4 25.3 12.3
cise time; in these conditions: E′ = Eaer ′ + E′ . The lactate Kayaking 250 61.9 4.04 40.5 37.3 22.2
Anl
′
contribution to E can be calculated from the net increase of Kayaking 500 134.8 3.71 60.4 26.9 13.4
blood lactate concentration (ΔLab ) determined after exercise: Kayaking 1000 289.0 3.46 83.3 8.8 7.9
′
EAnl = b ΔLab . t−1 , where t is the exercise time and b is
Kayaking 2000 568.2 3.52 89.5 6.1 4.4
the energy equivalent of lactate (e.g., 3 mLO2 . mmol/L−1 .
kg−1 , as proposed by di Prampero (93). As can be evaluated
from the above equation, the role of EAnl′ is reduced for longer
exercise durations, regardless the absolute peak lactate con-
centration in blood. This approach has been validated and as the exercise time gets longer, regardless the absolute PCr
used to determine the energy cost of maximal swimming and concentration at rest.
kayaking trials by several authors (e.g., 47, 431, 432). This approach to estimate E′ [by means of Eq. (10)] is
During all-out tests of shorter duration (less than 2-3 min), discussed in detail by di Prampero (95) and Capelli et al.
metabolic power (E′ ) can be estimated as the sum of three (47) and is only applicable to “square wave” exercises at
terms, as proposed by Wilkie (414) and later applied to land intensities at or above maximal aerobic power where oxygen
locomotion (94), to swimming (115,432,437) and to kayaking uptake does not achieve a steady state, and where other energy
(42, 431): sources play a major role.
The percentage contribution of the aerobic (Eaer ′ ) and
′ ′
anaerobic (EAnl and EAnAl ) energy sources to total metabolic
E′ = EAnS t−1 + α VO2 max − αVO2 max τ ⋅ (1 − e−(t∕τ) )t−1 (10) power is shown in Table 1. The percentage contribution of
′ , E′ , and E′
Eaer is almost independent of gender, skill
Anl AnAl
and mode of aquatic locomotion, but is dependent on the dura-
where α is the energy equivalent of O2 (e.g., 20.9 kJ . lO2 −1 tion of the exercise (t). As an example, for all out efforts of
consumed, for a QR of 0.96), τ is the time constant (s) where- the same duration (about 1 min, e.g., over a distance of 100 m
with VO2 max is attained at the onset of exercise at the muscular in swimming and 250 m in kayaking) the aerobic and anaero-
level (about 30 s, 328), EAnS is the amount of energy derived bic lactic energy sources supply about 40% and the anaerobic
from anaerobic energy utilization, t is the time of performance alactic energy source about 20% of total power expenditure
(s), and VO2 max is the net maximal oxygen uptake (above rest- (47, 432).
ing values). The third term of Eq. (10) is an estimate of the
oxygen debt incurred at the onset of exercise and, therefore,
the aerobic contribution to metabolic power (EAer ′ ) can be esti- Passive and active drag
mated as the sum of the second and third term of Eq. (10). EAer ′
The hydrodynamic resistance (D) determined by towing a
thus increases with the duration of exercise becoming equal “passive” subject (or a boat) through the water (when the
to α VO2 max in maximal exercises of 2 to 3 min or more (e.g., subject is not providing propulsion) and is defined as passive
more than 4-5 τ). EAnS′ (EAnS . t−1 ) is equal to the sum of the drag (Dp , N). When this resistive force is measured (e.g., by
′ ,
metabolic power derived from lactic acid production (EAnl means of a force transducer) at constant speed (v, m . s−1 ),
see above) plus that derived from phosphocreatine splitting: the power to overcome drag (Wd′ , W) is simply calculated as:
′ = PCr (1 − e −t/τ) . t −1 , where PCr is the phosphocre-
EAnAl Dp . v. By repeating these experiments at different speeds,
atine concentration at rest (in the contracting muscles), t is the Dp versus v relationship can be determined. Data of Dp
the exercise duration, and τ is the time constant of PCr split- reported in the literature are fairly consistent (for a review, see
ting at work onset (about 30 s). This analysis assumes that 159, 160). Females and children are characterized by lower
the time constant of PCr breakdown at the start of exercise values of Dp compared to adult male swimmer due to their
is equal to the time constant of the VO2 -on response at the smaller body dimensions and better floating characteristics
muscle level (330). As was the case for EAnl ′ , E′ decreases (e.g., 52, 64, 195).
AnAl
Volume 5, October 2015 1723
The Aquatic Environment Comprehensive Physiology
In “passive conditions,” no propulsion is provided by determinants of Da that are more easily calculated than Da
the swimmer/rower/kayaker whereas, in actual swimming (or itself on energy expenditure.
paddling) conditions, the arms/paddle/oars movements create Hydrodynamic resistance can be considered as the sum of
propulsion but also create additional resistance; thus, active three simultaneously created drag components: (i) form (pres-
drag (Da ) is expected to be significantly larger than passive sure) drag, that depends on the wetted area of the immersed
drag (Dp ) (159, 417, 433, 436). body/boat [see Eq. (11) below]; this component of drag
The Da versus v relationship in swimming has been inves- increases with the speed of movement and prevails at low
tigated with a specially designed Measuring Active Drag sys- to moderate speeds (up to about 1.2 m . s−1 ); (ii) friction drag,
tem which measures the push off forces (F) exerted by the that depends on the surface characteristics of the body/boat
swimmer using only arm strokes at a constant speed. The F is and that is determined by viscosity effects between the water
measured by pads fixed to a solid rod positioned underwater particles that are carried away in the vicinity of the body/boat;
under the swimmer. Under this condition, for the action reac- this component of drag is rather unaffected by the speed of
tion principle, it is assumed that Da = F (e.g., 387). According movement; and (iii) wave drag, that derives from displac-
to these authors Da ≈ Dp , this unexpected finding could be ing and rising water masses against gravity and thus from
explained by the fact that it is required that the swimmer does creating waves at the water surface; this component of drag
not use the legs, they are floated by a pull buoy, thus reducing increases as the speed of movement increases and is prevail-
the swimmer’s wetted area (as discussed below). Therefore, ing at the highest speeds attained in swimming competitions
with this method, the values of Da are probably underesti- (1.8-2.0 m ⋅ s−1 ) and in boat locomotion. For more details,
mated. Active drag has also been estimated by the difference see (268, 306, 307).
in swimming speed caused by free swimming with various Form, or pressure, drag can be calculated as:
hydrodynamic bodies attached that create a known additional
Dpr = 1∕2 ρCd Av2 (11)
resistance (197). This method, however, can be applied only
at maximal speed and thus does not allow to determine the Da where ρ is water density, v is the velocity, Cd is the drag coef-
versus v relationship. ficient, and A is the projected frontal area (in the direction
Active drag can be inferred from metabolic measures as of movement). Cd is a coefficient that takes into account the
originally proposed by di Prampero et al. (96): the hydro- shape of the body in motion; smaller values of Cd are asso-
dynamic resistance of a swimmer/boat moving in water at ciated with elongated shapes oriented in the direction of flow
constant speed, could be increased or decreased by attaching (streamlined objects) (397). For partially submerged bodies,
to the swimmer/boat known forces (e.g., an added drag, AD) A is the “wetted” area: the surface exposed to the water, since
acting in the direction of progression. Using this method, the that exposed to air has a negligible resistance (ρ of air is about
relationship between steady state VO2 and added/subtracted 800 times lower than that of water).
drag is linear for any given speed. The extrapolation of this Kayaks and rowing shells float on the surface and have
relationship to resting VO2 yields a value of AD that is in abso- lower values of Cd compared to human swimming; these
lute terms (and opposite in sign) equal to the average active boats are long and narrow (a single scull is about 8 m long
drag (Da ), that is, to the propelling force that the person has to and 0.3 m wide) and their design keeps pressure and wave
provide to proceed at that velocity (see also 94,300,432,438). drag low. In boat locomotion, the weight of the boat (about
With this method, the active drag of front crawl swimming 10-15 kg for a single sculls) is the major determinant of the
and kayaking was investigated; these studies have shown that: wetted surface area: an increase in weight has been reported
(i) in front crawl swimming active drag is almost twice than to increase hydrodynamic resistance by 10% for rowing and
passive drag: Da = 44 . v1.60 and Dp = 24 . v1.99 (in elite 20% for kayaking for a 20% increase in weight (299, 343).
male swimmers) (436), and (ii) not only active drag is larger As for boat locomotion, the wetted area of the swimmer
than passive drag but the former depends on the technical depends on the dimensions of the body (e.g., it is larger in
skill of the subjects; as an example in kayaking: Dp = 0.90 . heavier and taller swimmers) and on the fraction of the body
v1.63 whereas Da (elite men) = 1.48 . v2.01 and Da (unskilled that is submerged (which is larger the larger the “underwater
man) = 2.32. v1.75 : the lower the technical skill the larger the weight” of the swimmer) but in swimmers A depends also on
additional resistance to motion “created” by the subject while the body incline. Indeed, whereas the “underwater weight”
moving in water at a given speed (299). of the swimmer is determined by Archimedes’ principle as is
These data indicate that Da > Dp , as expected; they also the case for boats, in swimmers the “wetted area” depends not
indicate that, to understand the effects of hydrodynamic resis- only on the balance between weight (W) and buoyant force
tance on the physiological responses of exercise in the aquatic (B) but also on the distance between the points of application
environment Da and Dp are not interchangeable and that of these two forces. In the human body, these do not coincide
Da should be assessed/estimated instead of Dp . However, and this induces the body to rotate, the entity of this rotation
whereas measurements of Dp have been made for a long time (the angular momentum) depending on the values of W and B
using many methods, the measure of Da is still a controver- and on their lever arms. Particularly at low speeds, swimmers
sial issue (e.g., 160, 387, 416, 436). The difficulty measuring are not horizontal to the surface of the water and this
Da prompted some authors to investigate the effects of some increases their projected (wetted) frontal area. As the velocity
1724 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
of progression increases, the body becomes more horizontal in kayaks and rowing shells (e.g., 307, 434). Drag efficiency
to the surface and the wetted area decreases (436); in this increases with increasing velocity in both swimming and boat
condition, the major determinant of D is the underwater locomotion, as is the case for ηO (e.g., 308).
weight of the swimmers, as is the case for boat locomotion. Even more controversial than ηd are the methods utilized
Due to its importance in determining wetted area, and due to estimate overall and propelling efficiency, and the range of
to the difficulties of measuring Da , body incline was inves- their values. The values of ηO reported in the literature, for
tigated in static or dynamic “conditions” by several authors. swimming, range from 0.1 to 0.2 (387, 438) and the values of
The effect of the underwater static position on the energet- ηP range from 0.2 to 0.8 (115, 243, 386, 429, 438). As previ-
ics of swimming can be described quantitatively by measuring ously indicated (441), ηp can be calculated based on values
(with an underwater balance) the underwater torque (T) which of drag efficiency provided that overall (gross) efficiency is
is a quantitative measure of “the tendency of the legs to sink”: known (ηO = ηd /ηp ). In cycling, where Wtot ′ can easily be
the greater T the higher the wetted area (and thus D) and the measured with proper ergometers: ηO = 0.25-0.30. Overall
greater the C is for a given speed. As men have greater T, they efficiency in all cyclic forms of locomotion should theoreti-
expend more energy per unit distance than women; at low cally have the same value, as long as elastic energy does not
swimming speeds (0.9-1.1 m . s−1 ) about 70% of the variabil- play a role. In addition, the total power output must be pre-
ity of C is explained by the variability of T, regardless of the cisely measured to have a valid calculation. This proposal is
gender, age and skill of the swimmer (e.g., 96, 300, 431). At supported by a study (152) that demonstrated that ηO can be
higher swimming velocities (> 1.2-1.4 m . s−1 ) the hydrody- as high as 0.24 (in elite oarsman during a simulated 2000 m
namic lift counteracts the T, so that the body is horizontal to race on a rowing ergometer) and the same value was reported
the water surface,; at these speeds no relationship between T for “simulated swimming” on a laboratory based ergometer
and C could be observed anymore (431), at least in the front (441). The values of v, C, Wd′ , and ηp for various forms of
crawl. aquatic locomotion are shown in Table 2. Thus, the lower ηO
In “dynamic conditions” (during actual swimming), the values for swimming are likely due to the failure to account
wetted area depends on the body incline of the swimmer’s for all forms of work or lost energy during free swimming. It
body in respect to the waterline and the latter can be measured necessarily follows that, for ηO values of about 0.20 to 0.25,
by means of underwater cameras (e.g., 268, 435, 436). The and since ηd = 0.03-0.09, ηp could be as high as 0.36 to 0.45:
relationship between the static and dynamic position in water for example, only 50% of total power output results in propul-
depends thus on the speed and, at high swimming speeds, A sion (useful thrust) in subjects while swimming (441). These
is essentially determined by body surface and by the fraction estimates appear valid as humans are not ideally designed
of body that is submerged (the body incline being negligible). physically for locomotion in water, as compared to cetaceans
As shown by Zamparo et al. (436) at speeds from 1 to 1.6 that have ηp values ranging from 0.75 to 0.90 (116).
m . s−1 the average body incline during (front crawl) swim- In the last decade, a novel approach to determine pro-
ming is about twice that measured when the same swimmer pelling efficiency was put forward (243, 429, 435, 437, 441):
is passively towed in water (about 10◦ and 5◦ , respectively); instead of attempting to assess ηP based on measures of
this supports the hypothesis that Da > Dp and actually these
authors calculated that Da is indeed about twice than Dp (see
above), as previously reported also by other authors (e.g., Table 2 Values of speed (v) energy cost (C), power to overcome drag
96, 300). (W′ d ) and propelling efficiency (ηp ) at metabolically equivalent speeds
(E′ tot = 0.5 kW) in different modes of aquatic locomotion. Adapted,
with permission, from Pendergast et al. (308) and from Zamparo et al.
(434).
Drag, propelling, and overall efficiency
The determination of ηP and ηO requires the measure of the Mode of Speed range v C W′
d
total mechanical work (or work rate) of aquatic locomotion locomotion (m/s) (m/s) (kJ/m) (W) ηp
[Wtot or Wtot′ , see Eqs. (5) and (7)]. Given the difficulties in
just assessing Da it is not a surprise that only few papers UWF 0.4-0.8 0.6 0.88 31 0.58
attempted to estimate these two parameters. Drag efficiency
LK 0.6-1.0 0.7 0.70 17 0.36
(ηd ) only requires measures of drag and energy expenditure
[Eq. (6)] which are easily made and thus ηd values are likely FC 0.9-1.4 0.9 0.55 40 0.45
valid. This is the case even if the methods currently used to PW 1.1-1.3 1.3 0.36 44 0.39
estimate drag (active and/or passive) are controversial, they K 1.0-3.0 1.8 0.28 85 0.70
reliably show that less than 10% of the subject’s metabolic
WB 1.2-2.9 2.3 0.23 73 0.57
power can be transformed into mechanical power output
(ηd = 0.03-0.09) in the aquatic environment (e.g., 169, 300, R 2-5 2.4 0.22 99 0.70
387, 438).
UWF: underwater SCUBA diving with fins; LK: swimming with the leg
In boat locomotion, the values of drag efficiency are higher kick only; FC; front crawl swimming; PW: paddle-wheel boat; K: kayak-
than reported for swimming: for example, about 0.15 to 0.20 ing (slalom kayak); WB: water-bike: R: rowing shell.
Volume 5, October 2015 1725
The Aquatic Environment Comprehensive Physiology
force/power (which is quite difficult in the aquatic environ- differences in C should be accompanied for by differences in
ment, as indicated above) the efficiency of leg kicking and arm maximal swimming speed (vmax ) among strokes. Indeed, this
stroking were determined by methods designed for analysis was reported for male swimmers (US Olympic trials, 1976)
of animal locomotion. In swimmers using the leg kick (with over the 100 m distance, the corresponding vmax are: 1.92,
and without fins), ηp has been determined from values of for- 1.70, 1.78, and 1.48 m . s−1 , respectively (75). Moreover, the
ward speed and of the speed of the backward wave traveling differences in C among strokes should depend on differences
along the body (439, 440) as previously applied to the study in Da and ηP . Active drag or ηP have not been studied for
of undulating fish (e.g., 8, 80, 217). The technique for the arm swimming strokes other than the front crawl but, as indicated
stroke in front crawl swimming is comparable to the tech- above, the distance covered per stroke (dc ) is an index of pro-
nique used for animals using a “rowing” motion that move pelling efficiency. As reported by the same authors for the
water by producing power strokes, due to the backward move- same swimmers in the same conditions, dc is of 2.03, 2.24,
ment of their appendages, with the recovery strokes returning 1.99, and 1.46 m . cycle−1 for the front crawl, backstroke,
the appendages back to their starting position, moving for- butterfly, and breaststroke, respectively. Thus, as indicated by
ward (8, 80). In the front crawl, as a first approximation, the Eq. (9), the greater the distance the body travels per stroke
body can be assumed to move forward at constant velocity (an index of ηP ) the lower the C; this general rule seems not
(v) while the upper limbs (the appendages) move forward and to hold for the backstroke which is characterized by a larger
backward with a velocity u relative to the body. The ratio v/u dc than the front crawl but also by a larger C. This state of
is proportional to the Froude efficiency in animal locomotion affairs is probably due to differences in active drag between
(8) as well as in fluid machines (pumps, turbines, propellers, these two strokes.
fans, water wheels, and paddle wheels) as it is dependent on Compared to other forms of locomotion (e.g., cycling
the velocity of the components of the fluid and rotor at the or running) where minimal differences in C are observed
inlets and outlets (122). The velocity of the appendages (u, the among subjects with different technical skills (5-10%), tech-
hand speed for the arm stroke) can be directly measured by nical ability in swimming has a significant influence on C,
means of underwater kinematic analysis (115) or estimated, thus improving skill significantly reduces the C. As previ-
by modeling the upper arms motion as the motion of a pad- ously indicated, a recreational swimmer can spend as much
dle wheel (438); the values of ηp calculated in this way were as twice the energy a good swimmer uses for proceeding in
about 0.45 (in male elite swimmers). This value was expected water at the same speed (its C is 200% larger) and the latter
on theoretical grounds (441), and was not different between consumes about 20% to 30% more energy than an elite swim-
the two methods (115). mer at comparable speeds (169, 170). Training is expected
Propelling efficiency in boat locomotion is larger than in to improve technical skills and thus would lead to improved
swimming (in the 0.65-0.75 range [e.g., 51,308)], and overall ηP and reduced C. It has been shown that 4 years of high
efficiency was reported to be of about 0.20 to 0.22 (e.g., 92, velocity training caused a 20% decrease in energy expendi-
308) as previously found for exercise on a rowing ergometer ture (E′ ) and a 16% improvement in dc (propelling efficiency
(where mechanical work can be accurately assessed) (e.g., was not calculated in this study) (367). In addition improved
152, see above). skill would decrease Da by 15% to 35% (308); as shown by
Eq. (9) the reduction of Da is an important factor in reducing
C rafter training.
The determinants of the energy cost of locomotion Both ηP and Da are influenced by the anthropometric char-
(C)
acteristics of the swimmer that change with growth, and are
Data reported in Figures 1-4 refer to selected aquatic loco- also influenced by concurrent development and training. C
motion modes and to elite male athletes. Differences in E′ , C, is thus expected to differ between children and adults and
D, and ηP are however reported in the literature as a function between males and females. Women have indeed a lower C
of age, gender, and skill level; these parameters also differ (10-30%) than men (e.g., 52, 53, 269, 300, 431). The lower C
among strokes (in swimming) and depend on the specific has been reported to be due to lower hydrodynamic resistance
locomotor tool utilized to move in water. In the following secondary to smaller body size, and higher body fat (thus
sections, more detailed information regarding the energetics they assume a more horizontal attitude in the water) (e.g.,
of water locomotion is reported. 300, 430). A few studies have investigated the determinants
The energy cost of swimming, for a given speed, is the of C in children and adolescents. These studies indicate that,
lowest for the front crawl, then backstroke and butterfly, with at similar velocities, C is lower (10-50%) in children than in
breaststroke having the greatest cost (47, 170). For young adults (195, 312, 320, 437), the more so the younger the sub-
elite swimmers, the relationships between C and v for the four jects (437). Master swimmers are characterized by a higher C
strokes are well described by the following equations (adapted compared to younger swimmers and, at comparable speeds,
from Capelli et al. 47): front crawl: C = 0.670 . v1.614 , Back- C increases as a function of age (435); the decrease in maxi-
stroke: C = 0.799 . v1.624 , Butterfly: C = 0.784 . v1.809 , breast- mal metabolic power (Emax ′ ) that occurs with age forces these
stroke: C = 1.275 . v0,878 . Since elite athletes are characterized swimmers to reduce their speed; this, in turn, is related to an
by similar values of maximal metabolic power (Emax ′ ) these unfavorable alignment of the body (and thus with an increase
1726 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
in Wd ). More importantly, though, with age a deterioration in (a combination of water based activities to improve the
propelling efficiency occurs so that C increases due both to athletes’ physical performance); and (iii) “aquatic rehabilita-
an increase in Wd and to a decrease in ηP (435). tion” (a combination of water based activities aimed to total
These examples indicate that differences in C (E′ ) should or partial orthopedic and neurological rehabilitation). These
be expected based on differences in Wd , ηP , and ηO among activities can be performed without specific equipment (i.e.,
swimmers. The ACSM guideline tables (9) emphasize this water walking and running, aqua gym, and aqua aerobics),
relationship by warning readers that physical activity energy can utilize small tools to increase water resistance (e.g.,
expenditure (PAEE) “can vary substantially from person to hand paddles) or to improve buoyancy (e.g., pull buoys and
person during swimming as a result of different strokes and buoyant jackets) or can be performed with specific equipment
skill levels.” Thus, whereas it is true that in aquatic locomo- (such as water steps, treadmills, and bikes). The physiological
tion an increase in speed corresponds to an increase in exercise responses to these forms of exercise (the energy expenditure
intensity, care should be taken in selecting the appropriate C of WA) are greatly influenced by: (i) buoyancy and (ii)
versus v (or E′ vs. v) relationship to estimate the actual values hydrodynamic resistance.
of C (E′ ) in this environment. This is at variance with land
locomotion where in “healthy young adults” interindividual
Buoyancy
differences in C for walking, running, and cycling are negli-
gible allowing for a proper and simpler prescription of PAEE Archimedes’ principle is a law of physics stating that an
in “standardized conditions” (e.g., on flat and firm terrain, at immersed body is buoyed up by a force (B) equal to the
sea level and in the absence of wind). weight of the fluid it actually displaces. According to this
Compared with swimming, boat locomotion is charac- principle, the submerged weight of a body in water (UW =
terized by far lower values of drag and far larger values of body weight − B) is reduced in proportion to the immersion
propelling efficiency; this means that, according to Eq. (9), level; as a rule of thumb it allows for a 35% reduction in body
C is much lower than in swimming. As is the case for swim- weight when the body is submerged up to the thigh, 50% up to
ming, however, the energy cost of boat locomotion increases the navel, 75% up to the chest, and 90% up to the neck. In full
(nonlinearly) as a function of the speed and is determined by immersion, a human body thus weights only few Newtons. A
the design of the boat and the skill level of the athlete. As an larger “unloading effect” could be obtained with immersion
example, for sprint flat-water kayaking (K1 scull) C = 0.020 in seawater (which has a larger density than fresh water).
v2.26 (441) and for rowing C = 0.088 v1.05 (92). Body volume (Vb ), mass (M), and density (Vb ) are related
By analogy to swimming studies, in kayaking C was found as: Vb = M/ρb and thus, for a given immersion level, the
to be up to 30% to 50% lower (at paired speeds) in elite than in buoyant force will be larger the smaller the body density and
less experienced paddlers (42, 299). These differences were the larger the body mass. The density of muscle is about 1
attributed to differences in propelling efficiency. As is the g . cm−3 , of fat about 0.8 g . cm−3 and of bone about 3 g .
case for swimming, for the same skill level, male kayakers cm−3 ; this means that different buoyant forces will charac-
were found to be less economical than females (299): a 5% terize subjects with different anthropometric characteristics
to 12% difference in C, increasing with increasing speed. In (e.g., lean muscular subjects are less buoyant than subjects
this case, the difference was attributed to differences in Wd (a with a large percentage of body fat due to their different
lower body mass in female kayakers and hence a lower wetted values of ρb ; hence differences should be expected between
area). males and females and between young and elderly people).
As previously indicated for swimming, training decreases Moreover, when the lungs are also submerged, body density
the energy cost of boat locomotion (of about 25-33% in rowing will change with the changes in lung volume since air density
and 6-10% in kayaking), due to an increase in dc (an index of is about 800 times lower than that of water.
ηP ) and a decrease in Da (e.g., after 4 years of training active Thus, the “unloading effect of water” depends on the
drag can be reduced by 18-50% in kayaking) (307). level of immersion, on the density of water, on the volume
of the immersed body, on its density and on the volume of
air filling the lungs (when these are submerged). Therefore,
Water based activities for a given water depth, different “unloading effects” can be
Water-based activities (WA) are modes of physical exercise elicited in different subjects resulting in different physiologi-
performed in water and in HOWI. This general definition is cal responses.
useful to distinguish these exercise modes from the cyclic The buoyant force has also a deep impact on the “static
modes of aquatic locomotion (e.g., swimming, kayaking, and equilibrium” (e.g., on the “static position” the body assumes
rowing) and from other sport activities performed in water in water) as well as on the “dynamic equilibrium” (e.g., dur-
(e.g., diving, synchronized swimming, or water polo). ing body movements). Let us consider, as an example, the
WA (besides the recreational purposes) could be divided condition of a subject standing still (upright) in water up to
into three major categories: (i) “aquatic fitness” (activities to the neck: since the points of application of the buoyant force
maintain and improve physical fitness carried out in water (B) and body weight (W) do not coincide (the former is more
using different techniques and methods); (ii) “aqua training” cranial and closer to the lungs than the latter) if they are not
Volume 5, October 2015 1727
The Aquatic Environment Comprehensive Physiology
aligned on the vertical line (a condition in which the lever reducing the overall energy requirements of exercise, the more
arms of these two forces are nil) the body will rotate. so the larger the level of immersion; but (ii) the larger den-
In dynamic conditions (e.g., while raising an arm) the sity of water (compared to air) provides “loading” during
body’s centre of gravity changes and, if the arm is raised out all movements so that hydrodynamic resistance works as a
of the water, the value of B will also change. Furthermore, “confounding factor” increasing the energy requirements of
inspirations and expirations will change the position of the WA compared to the same movements performed on land,
centre of buoyancy (and also the value of B); this means that, the more so the larger the speed (frequency) of movement
in water, energy has to be expended to maintain the desired and the larger the submerged area of the body/body segments
body position (e.g., vertical during head out water activities) in motion. As an example, in water walking, the “favorable”
and to avoid unwanted (and unbalancing) rotations, the more effect of buoyancy seems to be offset by the added resistance
so the larger the amplitude of the movements. of water when the level of water approaches/exceeds waist
Buoyancy helps a body/body part to move toward the level (145).
water surface but resists a body/body part moving from the Since there is no means to assess with accuracy the
water surface; buoyancy can be increased “artificially” by intensity of WA on the basis of “standardized biomechanical
utilizing flotation devices (e.g., pull buoys or buoyancy jack- parameters” (such as speed in swimming and boat locomo-
ets); since this equipment comes with a variety of size and tion), the physiological effects of WA are difficult to sum-
shapes this has an obvious influence not only on the value marize and, indeed, the energy requirements of WA could
of B itself but also on the angular momentum (depending on be larger, equal or lower than those of the same exercise
where these devices are positioned on the body) as well as on performed on land. The example of water running will be
hydrodynamic resistance (see below). reported as a reference of this state of affairs.
Buoyant force can reduce the effect of the body’s weight
on its joints thus reducing compressive forces (e.g., 100). WA
can thus be a good alternative to land exercise in persons Deep water running
with low physical fitness, that is, elderly individuals, people Deep water running (DWR) is running in place in the deep-
with orthopedic or neurological disabilities, injured athletes, end of a swimming pool, usually wearing a buoyancy vest that
as well as obese patients (see below). floats the body so the head is out of the water. The standard-
ized technique that must be used is, as an example, described
by Chu and Rhodes (61): “(i) the trunk should be slightly for-
Hydrodynamic resistance
ward in respect to the upright position; (ii) the arms and legs
The resistance to movement in water is the result of an effort should follow a “unilateral forward motion,” thereby avoid-
to move aside masses of water coupled with the effort to ing the motions of treading water (i.e., circular leg and arm
overcome its frictional characteristics (density and viscosity). motions); (iii) the elbows should be at a 90◦ angle with the
When the movement in water is slow (or when the body is trunk; and (iv) the hands should remain completely open in
still) buoyancy is the principal force acting on the body; as the sagittal plane or in a closed fist to avoid “dog paddling” in
the speed of motion increases, the resistance to movement the water.
(D, hydrodynamic resistance) increases, becoming the most In DWR, there is no loading of the skeletal system and
important force acting on the body. As indicated previously, the workload is generally incremented by increasing the fre-
form or pressure drag [Eq. (11)] is the most important compo- quency of the movement (i.e., the “stride frequency”) by using
nent of total drag at low to moderate speeds and thus the most a metronome.
important form of drag for WA. According to Eq. (11), D (and DWR could be considered as: (i) an “aquatic fitness” activ-
thus energy expenditure) will be larger the larger the speed ity when aimed to maintain and improve physical fitness in
(v) of movement (or its frequency) and the larger the sub- health individuals (e.g., 41,316); (ii) an “aqua-training” activ-
merged (wetted) area of the body/body segments in motion ity when utilized to maintain and improve the athlete physical
(A). Indeed, the energy expenditure of a given WA is larger performance (43,324,413); or (iii) an “aquatic rehabilitation”
the larger the movement frequency (e.g., 6, 7, 48, 246, 317). activity when utilized for total or partial orthopedic and neu-
In WA, D can be increased “artificially” by utilizing “resis- rological rehabilitation (e.g., 125).
tance equipment” (e.g., hand paddles). Since this equipment Lower values of VO2 max and HRmax are reported for
comes with a variety of size and shapes this has an obvious DWR compared to running on land or on a treadmill) (e.g.,
influence on A (and hence on D and on energy expenditure). 100, 123, 362). The lower values of HRmax were attributed
Moreover, the “added resistance” depends on how this equip- to physiological factors (e.g., altered baroreflex response
ment is used since the value of A depends on the level of and increased venous return in water compared to land, see
immersion of the equipment and on its orientation along the below) but they were also found to depend on the different
direction of movement. “running techniques” adopted in water that could alter
Water immersion has thus two main consequences on the segment kinematics and muscle activation patterns and could
physiological responses to exercise: (i) it reduces the energy prevent the runners from attaining the same intensity level
needed to rise the body/body segments against gravity thus in the two conditions (266, 362). Indeed, Ghering et al. (143)
1728 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
showed that competitive runners, familiar with water running, WA in “uncontrolled conditions”: General
were capable of achieving similar VO2 max values on land and considerations
in water; however, those who were untrained in water running
Exercising at submaximal levels in TN water HR is simi-
showed a larger difference in VO2 max in the two conditions.
lar (e.g., 11) or slightly reduced (e.g., 305) compared to that
Familiarity thus plays an important role in physiological
assessed at similar VO2 values in air. The differences in the
requirements of DWR as previously shown (27, 124). Thus,
HR response between water and land are expected to increase
in accordance with what found is for water locomotion,
at lower water temperatures where lower HR are observed for
another parameter that has to be taken into consideration
a given VO2 (e.g., 230, 362). The lower HR has to be con-
to explain the energy expenditure of WA is the technical
sidered in WA exercise that is prescribed based on HR in the
skill (the efficiency) in performing that specific movement
swimming pool (with water temperatures of about 28◦ C) even
in water.
if exercise of moderate-high level reduces the temperature of
When comparing land treadmill running with aquatic
thermoneutrality (74).
treadmill running (or with running in shallow water) with
As suggested by Reilly et al. (324), the lower values of
a level of immersion up to the xiphoid process, the differ-
HR at a given VO′ , during submaximal exercise in water
ences in the physiological responses at maximal effort dis- 2
appear (e.g., 349, 388). In this case, however, the running compared to land, can be due to the ability of the subject
technique is expected to be more similar in the two condi- to exercise in water (as it occurs when comparing trained
tions (a push off phase on a solid surface is present in both and nontrained subjects for exercise on land). Also for this
cases) and the “unloading effect” is lower than in DWR as reason, care should be taken when using HR to grade exercise
lower could be expected to be the difference in the kinematic intensity in WA. Finally, the difference in maximal HR and
pattern between the two conditions, and hence in their energy VO2 values observed in some studies (see the example of
expenditure. DWR above) suggests that care should be taken also when
grading WA exercises based on the HRmax and VO2 max values
assessed on land.
WA in “controlled conditions” All these considerations suggest that the differences in
A fair comparison between exercise in water and on land can the physiological response observed in WA studies between
be performed using cycloergometry in TN water conditions water and land exercise in “uncontrolled conditions” could
so that the pattern of movement can be accurately matched be attributable to: (i) differences in exercise intensity (e.g., in
in the two conditions. To match the power output in the two water mechanical power output is influenced by buoyancy and
environments the effect of water resistance on the energy drag and HR could not be used to grade WA intensity), (ii) dif-
requirements of exercise has to be taken into consideration. ferences in the movement pattern (i.e., in neuromuscular and
The oxygen uptake of moving the legs underwater at a fre- kinematic responses); (iii) unfamiliarity/unhabituation with
quency of 60 rpm was suggested to be equivalent to about the “new” environment; and (iv) to thermoregulation issues.
25 W of external power (e.g., 118, 297). By taking this into
account, it is possible to match also the power output in the
two conditions and thus have a direct comparison of the “spe- WA: The effects of training
cific” effect of water immersion on the type of exercise. In Even if it is difficult to estimate with accuracy the inten-
these conditions V′O2 increases linearly as a function of exer- sity/physiological response of a given WA based on some
cise intensity, and the slope in water is comparable to that on E′ versus v relationships, as is the case for swimming and
land; no differences are observed in the VO2 /VE ratio and in the boat locomotion, it is well recognized in the literature that
slope of the HR versus VO2 relationship between conditions. VO2 increases when the immersion level is reduced and when
However, resting HR is about 10 bpm less in water compared the frequency of the movement in increased. This allows the
to land and HR is lower in water (of the same amount) at gradation of any WA in prescribing these exercises in accord
low exercise intensities (< 1-1.2 L/min), as well as at VO2 max . with dose-response principles (e.g., 9) as well as to utilize
Additionally, no differences in VO2 max between conditions these exercises for training purposes in different populations
are observed (309). of subjects.
As a general rule, in HOWI in TN temperature at rest, tho- Water-based physical activities are suitable for persons
racic blood volume, CVP and CO increase (e.g., 11,113), HR who have low physical fitness, that is, elderly people (e.g.,
remains unchanged (11), or decreases slightly (113). In spite 41, 389), persons with orthopedic or neurological disabilities
of the increased CO, MAP is unaffected as TPR is reduced, (e.g., 61, 81, 99), athletes after surgery or for treatment of
secondary to increased blood flow to muscles and/or visceral injuries (e.g., 362), and overweight or obese patients (e.g.,
tissues (e.g., 11, 201). During moderate exercise CO remains 129). Physical activity in water is also beneficial for fitness
elevated whereas ventilation, VO2 , and HR do not differ from for young adults and other healthy persons participating in
those on land (e.g., 11,113,188,297). At higher exercise inten- recreational activities (67,68,241). In general terms, when the
sities CO becomes more directly dependent on VO2 and the effect of water exercises is considered, there is general agree-
ventilatory response is similar to that on land (e.g., 297). ment among the studies that water exercises are an effective
Volume 5, October 2015 1729
The Aquatic Environment Comprehensive Physiology
alternative to traditional physical activities to improve health, expiratory pressures (321, 322, 425), but not to the extent that
physical fitness, aerobic capacity, muscular strength, flexibil- training with 100% did in the previous study (216). In addition
ity, and balance (e.g., 31, 61, 67, 68, 241, 313, 389, 398). in the latter studies (321,322,425), there was an improvement
in respiratory endurance, which was not reported for the train-
ing that used 100% pressures (216). Some previous studies
Respiratory muscle fatigue and training used a fixed resistance over the period of RMT (321,322,425).
In comparison to exercise on land at the surface, exercise More recent studies reported greater improvements in strength
both in and under water has been reported to increase the total and endurance using progressively increasing resistances as
WOB and respiratory muscle fatigue. During submersion, training persisted over 4 weeks (415). It is important to note
divers have increased airflow resistance (227, 233, 392, 393) that many of these studies failed to show an increase in max-
due to breathing resistance and SLL (87, 369). The increased imal VO2 , or cardiovascular function; most of the improve-
WOB is exacerbated at deeper depths as the pressure increases ments were in respiratory function.
gas density in the lung and SCUBA gear that has to be used Several studies have reported a reduced VE for a given VO2
to breathe (227). An additional factor may be increased end after resistive RMT during a submaximal constant-work rate
expiratory lung volume (EELV) present both at rest and during exercise at 70% to 85% of VO2 max exercise test (80% VO2 max )
exercise (227, 364). However, it has been reported that EELV (214,321,322,425). The reduced V̇ E was secondary to reduced
is not elevated under these conditions (364), but negative SLL Bf , even if Vt was either maintained or slightly increased both
may actually decrease EELV at rest and during exercise (227). for exercise on land (214) and in water (320,321,421). Resis-
Breathing at decreased or increased EELV, changes the respi- tive RMT increased the strength of the respiratory muscles
ratory muscle length to a disadvantaged length in reference to and was also associated with reduced VO2 for given WOB
the length-tension relationship and thus the force developed (efficiency). In addition, the ventilatory pattern (increase in
for the same effort is reduced (39,247). The combination of the VT and a decrease in Bf , i.e. reduced dead space ventilation)
factors described above causes an increase in the WOB, and decreased the WOB. The combination of decreased VO2 and
when combined with a lower efficiency (162) lead to higher increased VT allowed swimmer to exercise longer times for
energy cost of ventilation and likely lead to the increased the same work rate.
respiratory muscle fatigue observed in aquatic exercise. Res- Ventilation is known to be tightly correlated to VCO2 , how-
piratory muscle fatigue has been demonstrated for surface ever, in the presence of metabolic acidosis caused by anaer-
swimming, and this observation led to a recommendation to obic glycolysis and lactic acid accumulation VE is increased
use respiratory muscle training (RMT) to improve swimming out of proportion to VCO2 (respiratory compensation for a
performance. metabolic acidosis). Tachypnea occurring at voluntary exer-
Until recently, respiratory muscle fatigue was not appre- cise exhaustion pre-RMT is consistent with an increase in
ciated as limiting exercise power or endurance. However, this lactic acid and may have induced premature respiratory mus-
opinion has evolved recently for both maximal and submaxi- cle fatigue (36-38). It has been demonstrated that 4 days of
mal exercise (38,157,158,158,231,356). Due to the increased nominally 80 cmH2 O intermittent inspiratory loading in dogs
total WOB and potential reduced efficiency, the respiratory increased the expression of the slow myosin heavy chain iso-
system may be more limiting during aquatic exercise, par- form in the costal, crural diaphragm, and intercostal muscles
ticularly at depth. Although it was shown some time ago (134). An increase in the slower myosin heavy chain isoform
that training the respiratory muscles could improve respira- is likely the result of increased airflow resistance and thus,
tory muscle strength and endurance (216), it was not until improves respiratory muscle and exercise endurance, espe-
more recent years that RMT (37) was shown to improve exer- cially under conditions of airflow limitation.
cise performance, and more importantly that various forms of
respiratory muscles training improved running, cycling, and
rowing performance (141, 168, 175, 198, 199, 214, 219, 238,
248,273,329,356,399,410). Leith and Bradley (216) were the Head-Out Water Immersion in Cold
first to demonstrate that RMT could improve peak mouth pres- Water
sures (respiratory muscle strength) and the time a high level
of ventilatory work could be endured (endurance) with spe- Heat loss during cold HOWI is reduced by vasoconstriction
cific protocols that improved either strength or endurance, but of the skin and subcutaneous fat layer that increases tissue
not both (216). They (216) demonstrated that high resistance insulation (289-291, 396). Acclimatization also increases the
breathing (100% of maximal voluntary inspiratory and expira- resistance to heat loss via peripheral vasoconstriction due to
tory) improved maximal respiratory pressures but not respira- either or both central or local factors (213). In addition, to
tory endurance. They also demonstrated that high inspiratory reductions in Ts and Tc , muscle blood flow is reduced in a
and expiratory flows, while isocapnic increased respiratory graded manner to the drop in Ts and Tc and maximal CO is
endurance, but not strength (216). A later study showed that reduced leading to reduced VO2 max and exercise performance
resistance RMT at nominally 40% individual maximal inspi- in the cold (297). If the increased insulation does not prevent
ratory and expiratory pressures increased both inspiratory and a reduction in Ts and or Tc shivering takes place in a graded
1730 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
manner, increasing VO2 and heat production in an attempt to colder the temperature, the shorter the time to hypothermia.
mediate heat loss (213). Shivering endurance is important in thermal protection; the
HOWI in TN water does not increase or decrease resting shivering drive, but not the intensity of shivering, decreases as
VO2 ; however, at cooler water temperatures, VO2 increases a function of time, suggesting fatigue and habituation, which
in proportion to the drop in Ts and Tc as a function of time in turn cause decreased cold sensitivity (377, 378). Blood
(297). Swimming in water increases the work due to its higher glucose levels increase with shivering on land and increase to
density than air, and thus the VO2 for a given velocity is higher levels during immersion, but as time progresses there
increased (307, 308). is increased fat oxidation (378).
The most dangerous situation in the aquatic environment Cold water HOWI, relative to TN water immersion,
is drowning, which is more likely to occur in cold water elicits similar decreases in intracellular fluid volume; how-
immersion. In nonacclimatized individuals, sudden cold water ever, the initial increase in PV is reduced during cold water
immersion results in an increase in HR (31 b/min), hyperven- HOWI (358) compared to TN HOWI. Exercise performance
tilation (both Bf and VT ) with a lowering of PaCO2 , and a is impaired by brief exposures to cold water, even in elite ath-
reduction (50%) in cerebral blood flow velocity (235, 236). letes, and the impairment is magnified by prolonged exposure
These physiological changes can lead to drowning, without (297, 341). SNA is responsible for the majority of physiolog-
hypothermia. Acute cold water immersion commonly results ical changes due immersion in cold water (357).
in an initial gasp, and is followed by hypertension and hyper- CO generally increases similarly during both cold and
ventilation that significantly reduce arterial CO2 (hypocap- TN HOWI but there is a bradycardia during cold immersion,
nia). Thus, the expected effect of hypocapnia on ventilation is which is compensated for the increased SV in HOWI. How-
overridden by the sudden exposure to cold water. (82). It has ever, studies at depth report an increase in CO (411). MAP
been reported that after just 30 min of immersion or swim- is mostly reported to not be elevated in HOWI because the
ming in cold water decision making ability is impaired (101). reduced blood flow to skin, subcutaneous tissues, and mus-
Furthermore, swimming failure in cold water is not due to cle is balanced by increased blood flow to other tissues and
general hypothermia, but more to muscle failure of the arms TPR remains unchanged (297). At pressure, however, there is
or legs as the reduction in core temperature is greater with an elevation of MAP as the thermal-mediated vasoconstric-
movement due to increased convective heat loss (101). tion is not offset by vasodilatation in other areas to offset the
By comparison, instructing subjects about the effects of increased CO (411). In water below TN temperature, there
sudden immersion in cold water is an effective way to reduce is a reduction in cutaneous blood flow due to the reduction
negative physiological effects and to prevent the reduction in Ts . However, if there is also a decrease in Tc , SNA is
in cerebral blood flow velocity (235). In addition, 5 days of increased more causing further reduction in blood flows and
acclimatization to cold immersion (3 min in 10◦ C water) this response is increased by acclimation (283). Cooling the
results in significant reductions in respiratory frequency, skin, but not the core, reduces thermal strain during exer-
minute ventilation, and heart rate, and these effects last 7 cise and may improve performance in warm air environments
to 14 months (383). However, sustained immersion in cold (189). Cooling the body after exercise may facilitate sub-
water can lead to hypothermia, which if uncorrected, does sequent exercise performance and assist with tissue repair.
lead to death. The response to cold water is dependent on However, it should be noted that jumping in cold water baths
both the water temperature and duration of immersion. Many after gym workouts with high Ts and Tc may lead to arrhyth-
studies have shown that TN water temperature is 35◦ C in mias, cessation of ventilation and exasperate the effects of
resting humans. The minimal temperature that can be tol- pulmonary edema.
erated using physiological adjustments (vasoconstriction of Cold HOWI (16.4-24.1◦ C), for up to 10 h, initially
subcutaneous and muscle blood vessels to maximize tissue resulted in an increased Tc , presumably due to cutaneous vaso-
insulation) is the critical water temperature (CWT) and is constriction; but thereafter Tc dropped exponentially down
nominally 30◦ C at rest, while temperature below this results to 35◦ C within 1 to 2 h (376). Shivering can be increased
in increased metabolism, and over time leads to hypothermia. three to four times basal VO2 . Heat debt is peaked after 2 h
CWT is the lowest temperature that can be tolerated at rest of immersion, due to body’s fat, connective tissue, muscle,
for 2 h without increased VO2 , and is associated with maximal and bone components; and Ts and Tc are also reduced (277).
peripheral vasoconstriction and body insulation (178). The Another phenomenon in cold water is cold-induced vasodi-
CWT does not appear to be effected by water depth (178). lation (CIVD) during cold immersion (30 min at 9◦ C) of the
Shivering is driven by changes in Tc , as well as body heat hand in men and women, increasing hand skin temperature,
content (376) and may increase resting metabolism by a factor but not the upper arm Tc (142). CIVD during prolonged cold
of 3 to 4. In water below CWT, there is an association between immersion of the hand has been demonstrated in both men and
changes in deep Ts and hyperventilation, however there is no women, and twitch force, time-to peak tension, and 1 /2 relax-
association with surface Ts (244). Both CWT and the rate ation time were increased during CIVD compared to control
of development of hypothermia are also influenced by the and were associated with the finger temperature (142). Impor-
subject’s subcutaneous fat content (291). The specific time to tantly, CIVD is phasic, does not persist, and is not likely to
hypothermia is dependent on water temperature, that is, the have a major influence on performance in cold water.
Volume 5, October 2015 1731
The Aquatic Environment Comprehensive Physiology
HOWI in cold water immersion immediately decreases Ts increase in plasma NE, but not epinephrine or dopamine
to that of water temperature. However the sensory inputs from (180, 181).
Ts and Tc differ when skin temperature changes are uniform The thresholds for both shivering and vasoconstriction
versus nonuniform as the differences in the uniformity of Ts may be influenced by the initial Ts , either due to previous
yield different physiological responses. With a uniform Ts exposure to warm conditions or exercise. Elevated Ts signif-
(WI in 31.4◦ C) changes in mean Ts and Tc were identical; icantly affects the shivering and vasoconstriction thresholds
however, Ts in trunk was higher and the Ts of the limbs was (190). When subjects were immersed in 10◦ C water with
lower in when Ts changes were nonuniform. Heat production limbs protected but the torso exposed, HR decreased along
and overall skin heat flux with cold HOWI were identical with ventilation and skin blood flow during the first initial
when Ts changes were uniform, but were 25% lower with period of immersion. However, when the torso was protected
nonuniform Ts than with uniform Ts and insulation was higher ventilation and skin blood flow still decreased but HR did
due primarily to higher limb insulation. Thermogenesis due not. This suggests that the cold stimulus to the limbs is more
to shivering was lower (62%) with nonuniform Ts than with important than the cold stimulus to the torso in in regulation
uniform Ts . It can be concluded that when Ts of the trunk is HR during cold HOWI (379), but not for regulating ventilation
higher there is an attenuation of shivering in cold water, and or skin blood flow.
this is likely related to higher overall insulation which defends Plasma renin-angiotensin activity was decreased to 1 /2 by
Tc (58). cold HOWI, but aldosterone levels did not decrease. SNA
Preheating subjects prior to HOWI results in a larger increased but it did not appear to influence HR whereas it was
decrease in Tc and muscle temperature in 14◦ C HOWI in associated with peripheral vasoconstriction (increased TPR)
a time-dependent manner (5-20 min) (296). Another study and a small increase in MAP (180).
showed that increasing Ts by preimmersion in 40◦ C predis- It is well documented that Tc is lower in the morning than
posed subjects to greater heat loss and greater decrements in later in the day. In this regard, men immersed in 20◦ C for 2 h
Tc in cold water than without the increased Ts (7◦ C) (342). in the morning did not display shivering or vasoconstriction,
When subjects were exposed to 18◦ C, 22◦ C, and 26◦ C while later in the day they did and they were important adap-
HOWI for up to 90 min, some subjects completed the set tations to maintain Tc . This suggests that there is a greater risk
of immersions, others did not. The subjects who completed of hypothermia during cold exposure in the morning (49).
the test and those that did not had the same TS and increase Protection against cold water exposure can be achieved by
in VO2 ; however, Tc dropped more rapidly in the intolerant insulating suits such as a wet suit, dry suit, or active heating
group, presumably due to less metabolic adjustment, as well suit. Wearing thermal protection gear provides insulation but
as less vasoconstriction of the skin and fat tissues and therefore results in nonuniform and higher skin temperatures. Although
lower overall body insulation. This suggests that shivering- there are apparently no differences in thermal sensation and
induced thermogenesis can provide enough heat to protect shivering thermogenesis when Ts decreases uniformly versus
some individuals but not all (146). nonuniformly (wet suit covering trunk upper arms and legs),
The depth of immersion affects thermal regulation, as is tissue insulation (vasoconstriction) was significantly higher
the case with the cardiovascular responses to graded HOWI. In when Ts changes were nonuniform due to augmented cold
cold water (15◦ C), Ts reductions were similar for the shoulder sensory input form the periphery (404). It has also been noted
and hip, but higher for the knee during both rest and exercise that when Ts were maintained at a higher level during cold
(215). In 25◦ C water, Ts reductions when the level of HOWI immersion the temperature gradient between body and water
was below neck level were less than mid-cervical HOWI, and actually increases and this may result in greater heat loss
Ts levels during exercise were higher (215). and decrease in core temperature (16, 267, 305). This may
HOWI for one hour at 32◦ C did not affect VO2 or Tc but be an issue with wet suits. Wearing a wet suit in cold water
lowered HR (15%) and SBP and diastolic blood pressure resulted in a higher esophageal temperature and attenuation
(DBP) (12%) compared to the nonimmersed condition. By of shivering and thus VO2 did not increase as much due to the
comparison, HOWI at 20◦ C lowered Tc and increased VO2 higher insulation (404).
(93%) and urine flow increased sharply (89%), while levels Wearing a wet suit during intermittent exercise in cold
of renin, HR, and BP were similar to TN HOWI. In 18◦ C, water was superior to continuous thermogenesis in sustaining
there was a further decrease in Tc and a further increase of body temperatures (402). While wearing a wet suit does not
VO2 (230%) and HR and MAP (5-8%), while plasma NE rose affect the acute response to cold water immersion, wearing a
(250-530%) and urine flow (163%) increased more. When dry suit significantly blunts decreases in body temperatures
both Ts and Tc fall there is a greater effect on thermogenesis in cold water (380). Although wet suits significantly increase
than when Tc alone falls (402). Changes in plasma cortisol body insulation, the higher Ts while wearing a wet suit may
are not temperature dependent, and there is no association result in greater heat loss. Therefore, wet suits may not provide
between Tc and other hormonal responses. These data suggest sustained thermal protection.
that in addition to physiological responses to WI per se, cold Although wearing a dry suit can provide thermal insula-
WI specifically, increases SNA (357). HOWI for one hour tion sufficient to prevent hypothermia, it is only the case if
in 14◦ C water increased SNA, as indicated by a fourfold the suit stays dry; even then it does not adequately protect
1732 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
the hands and feet of the subject. Use of a dry suit eliminates was no significant change in CO in cold water compared the
long term core cooling; however, greater cooling (Ts and Tc ) TN water. Both MAP and TPR are increased in cold water,
has been observed in the first 10 min of HOWI in cold water while they are decreased in warm water (33).
(112). Active heating systems are available and have been HOWI in 39◦ C causes dehydration, even with fluid
shown to protect the swimmer from hypo- and hyperthermia replacement. Hematocrit increases and there is a decline in
(16, 267, 305); however, they require an electric power source mean power and peak power during exercise as well as a
and thus may not be practical. Previous studies have shown greater level of perceived exertion (200). HOWI in warm
that having divers cool during compression and warm during water has been shown to increase total urinary Aquaporin 2
decompression is advantageous for N2 washout (less wash- excretion suggesting elevation of plasma vasopressin levels
in and greater washout) and may reduce the incidence of (391). Forty-five minutes of TN HOWI followed by warm
DCS (140). water immersion at 41◦ C caused an immediate decrease of
plasma fibrinogen and plasminogen activator inhibitor activ-
ity concentration decreased immediately. These observation
Head-Out Water Immersion in Warm suggest that warm HOWI leads to hemoconcentration and
Water minimal activation of coagulation, implying increased risk of
thrombotic activity (32).
Cold HOWI has been well researched, with most adjustments
known. However, swimming and diving also occurs in warm
water. Immersion in warm water at or under water, when Acclimatization
combined with exercise, results in an uncompensated heat While acute HOWI in water below TN temperature causes
load which cannot be balanced by heat loss. Moreover, the adaptations, chronic exposure results in acclimation, and may
reverse thermal gradient (water to body) may lead to hyper- be a result of central or/and peripheral adaptations. Original
thermia and even death. There are likely few acclimatizations studies of fishermen indicated that they had developed suffi-
in warm water as those factors that show this adjustment cient acclimatization of the circulation of the hand allowing
in air cannot function in water (sweating, evaporation, etc.). them to work for long periods while fishing. However, in this
Immersion/submersion in warm water results in a temperature case the cold exposure was confined to the hands, while the
gradient favoring increased body heat stores. The inability to rest of the body was warm. More recent studies in air have
evaporate sweat causes a fast and high elevation in Ts and shown that if the body (torso) is warmed, blood flow to the
Tc which could quickly reach serious levels. The addition of hands is maintained and the hands remain functional in cold
exercise leads to significant additional heat production and air (101). However, this has not been shown to be the case
thus increases the risk of hyperthermia. Although sweat can- when the total body is immersed or submersed.
not be evaporated, sweating continues, and eventually would One study has shown that 5 days of acclimatization to
result in reduced PV and, when added to the increased blood cold HOWI (3 min in 10◦ C water) resulted in significant
flow to the skin, leads to lower CO and skeletal muscle blood reductions in Bf , V̇ E , and HR, and these effects last 7 to 14
flow, resulting in reduced exercise capacity and hyperthermia. months (383). However, these changes do not effect overall
Although not documented, based on data for subjects accli- thermal resistance which is likely not changed much due to
matized to air persons in water could be at a greater risk of acclimatization to immersion in water.
hyperthermia as this may potentiate sweating and vasodilata- Chronic exposure of the hands to 10◦ C water resulted in
tion, risking reduced PV, and blood flow to working muscle reduced HR and ventilatory responses in habituated male sub-
and brain. Immersion in water at temperatures greater than jects, in spite of identical Ts declines, suggesting a more cen-
TN can cause hyperthermia. This condition is more risky than tral regulation of circulatory and ventilatory responses (382).
hypothermia because there are no defenses against hyperther- This is in agreement with the historic study of the responses of
mia in warm water due to the high heat conductivity of water fishermen to cold hand immersion. It has been suggested that
and elimination of heat loss by evaporation of sweat. This is the vasoconstriction response due to cutaneous cold receptors
an area of underwater physiology that needs additional study. in 15◦ C can protect even in colder water (382). These adap-
It has been proposed that intrathoracic blood volume tations are due to a decrease in the immediate changes in Bf
should be less in warm water due to the peripheral vasodi- and VT , and HR to acute HOWI (381, 382). Repeated HOWIs
latation (109); however, it was shown to be not lower in 41◦ C in 15◦ C for 1 h three times per week for 4 to 6 weeks has
HOWI, compared to 35◦ C and 25◦ C HOWI (279). This is sup- demonstrated that subjects had lower Tc , presumably due to a
ported by the demonstration that HOWI in water temperatures delayed metabolic response and subjective shivering in accli-
of 32◦ C, 34.5◦ C, or 36◦ C did not affect the net transcapillary matized subjects, while they had less sensation to the cold.
fluid shift into in the face of temperature-dependent increases These changes suggest a slight increase in insulation due to
or decreases in vascular tone (426). TN HOWI increases SV acclimatization (180).
and CO and HR is decreased. By comparison, HOWI in warm While acclimatization has some cardiorespiratory effects
water results in an increase in HR of 32%, while CO increased it does not appear to have a major effect on thermal status,
18% as compared to a 44% increase in TN water and there which is also the case for plasma renin-angiotensin activity
Volume 5, October 2015 1733
The Aquatic Environment Comprehensive Physiology
and aldosterone concentrations (181). Chronic HOWI in due mainly to decreased water reabsorption (289). The renin-
10◦ C to 4◦ C water for three months resulted in decreased angiotensin II-aldosterone system is activated at depth in dry
catecholamine response to cold HOWI (174). conditions secondary to the transient dehydration induced by
the early hyperbaric diuresis (289). Although these responses
are due to pressure alone, when the subject is submersed in
Submersion—Diving water the effects of the submersion overshadow the pressure
effects and the cardio-renal responses are similar to those
Ventilation can be maintained during shallow immersion described above for HOWI.
while breathing from a snorkel, however during submersion
special equipment is needed to compensate for the hydrostatic
pressure created by the depth of immersion. The required Pulmonary gas exchange during diving
equipment for breathing underwater (SCUBA) provides com- During exercise at 1 ATA V̇ E normally increases in proportion
pressed gas with a pressure that compensates for the hydro- to metabolic demand, which maintains arterial pH constant.
static pressure, allowing breathing (23). In theory breathing In untrained individuals exercising at a constant work rate
from SCUBA has no depth limit; however, physiologically (nominally 50% VO2 max ) there is a 20% to 25% increase in
there are limits. One limit is the potential for oxygen toxicity VE after 12 to 15 min (425). A similar, more gradual increase
while breathing air with the pressure-dependent increase in in VE occurs during the same timeframe underwater (321).
partial pressure of O2 (23). Another issue is that the nitrogen This is not due to a change in acid-base status (292), and since
pressure in air nitrogen is a depressant (nitrogen narcosis) at it can be attenuated or abolished by RMT (321, 425), is most
depths greater than nominally 100 fsw. Still another issue is if likely due to respiratory muscle fatigue. At extreme levels
a diver breath-holds during ascent the air in the lungs would of exercise acidemia may occur despite disproportionately
expand with the potential for alveolar rupture (embolism), increased V̇ E and hypocapnia.
even in relatively shallow waters (23). By following proper Compared with the surface, for any given work rate during
procedures, these risks can be minimized; however, there is a a dive V̇ E tends to be lower, resulting in hypercapnia. All but
further complication of diving with SCUBA. While the sub- a few studies examining contributors to hypercapnia in diving
ject is breathing compressed gas the body takes up inert gas, (56, 210, 278, 335-337) have used end-tidal PCO2 (PET CO2 )
usually N2 , and as the diver ascends, this gas has to be elim- as a surrogate for arterial PCO2 (PaCO2 ), which is usually
inated. If this is not done following proper decompression valid under resting conditions. However, during exercise the
protocols, it can lead to the formation of bubbles which may approximation is less satisfactory: during exercise at 1 ATA
form at the joints causing the victim pain. A further compli- PET CO2 exceeds PaCO2 (222); under conditions in which
cation is that the bubbles formed during decompression may dead space is increased (e.g., when gas density is increased)
occlude blood flow and compress nervous tissues, causing the PET CO2 is lower than PaCO2 . Only two studies have directly
victim neurological pain. This condition is called DCS or the correlated the two in diving, in the dry at 2.8 ATA (278) and
bends. DCS rarely occurs in diving that follows acceptable submersed at 4.7 ATA (56), both demonstrating a reasonable
decompression procedures. correlation, although with significant scatter.
Total ventilation is maintained to result in an alveolar ven-
tilation that is tightly coupled to PaCO2 , typically ∼40 mmHg
Cardiovascular and renal responses to diving in healthy individuals (167), while matching O2 delivery to
Submersion has been shown to increase CO and more in cold metabolic demands (1). Divers have been reported to sponta-
water than TN water (411). Breath-holding during submer- neously or voluntarily hypoventilate leading to CO2 retention
sion results in greater depression of CO than during immer- (272). Hypoventilation and thus CO2 retention can also be
sion with free breathing, as the bradycardia is due to face due to divers’ inability to meet the force and energy require-
immersion related to the diving reflex (218). Subjects who do ment of the increased respiratory work secondary to weak or
not ventilate sufficiently have increased PaCO2 , however, this fatigued respiratory muscles. Hypoventilation and CO2 reten-
does not cause modulation of cardiovascular variables (17). tion (see below) may increase the likelihood of CO2 narcosis
HR at depth is reduced compared to submersion at the sur- (e.g., 17, 212, 406), as well as central nervous system oxygen
face resting, as well as at exercise intensities (303), resulting toxicity and nitrogen narcosis (44, 212). A study has shown
in lower maximal HR at maximal exercise. In addition, the that CO2 retention in divers may cause convulsions due to
reduced maximal CO may account for the reduced maximal O2 toxicity, in spite of the dive profile being what would be
VO2 observed at depth, in spite of the increased PO2 . The considered a safe limit for hyperoxic exposure (212).
changes in CO are less important at depth than the changes in In resting subjects, VE is increased at depth primarily due
pulmonary function. The latter is discussed at depth below. to an increase in VT with submersion depth (162, 280, 406).
The cardio-renal responses to dry pressure exposure alone It has been hypothesized that the depth-dependent hyperoxic
result in an increased urine flow, but not GFR (289). This hyperventilation is due to the effects of high PO2 at depth
diuresis is accompanied by excretion of potassium, sodium, on the reduced peripheral chemoreceptor sensitivity (293).
calcium, and phosphate (289). Urine osmolality is reduced Reactive oxygen species, secondary to the high PO2 at depth
1734 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
are proposed to accumulate in the tissues of the brain and are the effects of diving on mechanical load, gas mixing and
result in stimulation of the central chemoreceptors in the cau- diffusion, VA /Q matching and respiratory drive (271).
dal solitary complex (84), resulting in the observed hyperven-
tilation, by dampening the feedback in the respiratory control.
Mechanical Load
This postulate is supported by data from a study that reported
a similar observation after carotid body denervation in vivo During a dive there are three load parameters that change. The
(73, 133). If hyperventilation occurs by this, or other mech- major one is flow resistance due to the higher gas density (10),
anism, it would result in a reduction of arterial PCO2 below which increases linearly with ambient pressure. In turbulent
its normal level; however, this is not supported by studies flow (which occurs in large airways) resistance is density-
examining this potential mechanism (120). It is also possible dependent. Higher airways resistance caused by increased
that the depth-dependent hyperventilation observed at rest at gas density occurs during both inspiration and expiration.
depth is the “Haldane effect.” This effect suggests that if there During expiration there can also be expiratory flow limitation
is less O2 released by hemoglobin that CO2 elimination would due to airway collapse (421). These effects can be detected by
be reduced leading to increased PaCO2 which would lead to reduced forced expiratory volume in one second (FEV1 ), peak
a hyperventilation to reduce PaCO2 (227). The hyperventila- expiratory flow and maximum voluntary ventilation (MVV)
tion many have negative consequences for the brain (208), as (70, 209, 233, 355, 401). At any gas density ρ, peak expiratory
well as stimulating central chemoreceptors. However, even if flow or MVV can be predicted by the following formula (420,
these changes occur PaCO2 would be only slightly increased 422):
(nominally by 1 mmHg), and thus not important (272). It
has also been shown, and is the most probable explanation A = Ao (ρ∕ρo )−k
for the depth-dependent hyperventilation, that dead space
ventilation is increased, as is the dead space and the dead where A is either MVV or peak expiratory flow at gas density
space-to-tidal volume ratio, as a function of the less effective ρ, A0 is MVV (or peak expiratory flow) at 1 ATA, ρ is gas
gas mixing in the lungs at depth (272). To compensate for the density at the ambient pressure of the dive, ρ0 is gas density
increased dead space the diver would have to increase V̇ E via at 1 ATA, and k is a constant with the value 0.4 to 0.5. A sim-
an increase in VT to maintain adequate alveolar ventilation. ilar equation has been published for the relationship between
The increased VO2 and VCO2 during exercise results in an airway conductance and gas density (10).
increase in VE in a dose-dependent manner. The increase in External resistance is present in all underwater breathing
VE as a function of VO2 was reported to be greater when sub- apparatus and adds to the overall respiratory load. Changes in
mersed than in the dry condition, but was decreased at depth viscosity could affect gas flow in small airways where there
when compared to the surface (162). Increased V̇ E has been may be laminar flow. However, within the pressure range to
suggested to be due to facial immersion when submersed (82); which humans have been exposed (up to 70 ATA), there is no
however, another study does not support this conclusion (56). measurable change in gas viscosity.
The increased SLL at depth likely results in increased respira- A second component of mechanical load is elastance.
tory muscle activation during inspiration, as well as increased Elastance is the quality of recoiling on removal of pressure
duty cycle (162). It has been reported that VT is increased without disruption, or an expression of the measure of the
at depth; however, V̇ E was reduced resulting in an increase ability to do so in terms of unit of volume change per unit
in elastic work (162). This breathing pattern could blunt the of pressure change; it is the reciprocal of compliance. Tho-
effect of the depth-dependent increased airway resistance and racic elastance is composed of the individual elastances of the
work due to the increased gas density at depth, but it could lung and chest wall. Chest wall compliance does not change
maintain alveolar ventilation even though there is increased significantly during immersion; however, lung elastance is
dead space. During spontaneous breathing at 1 ATA the bf and increased, most likely due to vascular engorgement caused
VT are proposed to be regulated to produce the most efficient by redistribution of blood from the periphery into the tho-
duty cycle (251, 286, 287). If the same is true at depth both at rax (78).There may also be an effect on elastic load of the
rest and during exercise, bf and VT are likely balanced by the difference in external hydrostatic pressure between the lung
respiratory drive in response to the increased dead space and and the mouth due to the position of the diver in the water
higher PaO2 to optimize V̇ E . column (365, 366). The immersion-related increase in elas-
High external breathing resistance may cause severe tic load causes a further decrease in MVV from that due to
hypercapnia without prodromal symptoms (dyspnea) increased gas density (424).
(212,406). One possible mechanism is inadequate respiratory The third component of respiratory load is inertance,
muscle performance (e.g., due to fatigue). Interestingly, which is the tendency to resist acceleration. Inertance is
RMT can improve respiratory muscle function and exercise a function of the combined masses of the chest wall, the
capacity (214, 219, 425). CO2 sensitivity in low responders gas flowing within the airways and breathing apparatus,
tends to increase; in high responders it tends to decrease and to a minor extent the water surrounding a diver’s torso.
(304). Respiratory muscle fatigue and CO2 retention are Respiratory system inertance at 1 ATA, typically 0.01
both attenuated (321). The principal causes of hypocapnia cmH2 O⋅L−1 ⋅s2 , increases in direct proportion to gas density
Volume 5, October 2015 1735
The Aquatic Environment Comprehensive Physiology
(250, 310). During cyclic breathing at a frequency lower than reduction in WOB (321, 322), as well as increased efficiency
the resonant frequency of the system inertial impedance is (351). These data further demonstration that RMT reduced
less than elastic impedance. At a higher frequency, inertial the energy cost of ventilation (VO2 and La) for iso-workloads,
impedance exceeds elastic impedance. Resonant frequency which has been shown by many authors (356). Prior to RMT,
of the human respiratory system is typically 6 Hz at 1 ATA the increase in V̇ E and fb combined with a decrease in VT at
breathing air. This decreases to around 2 Hz if breathing gas the end of exercise as well as the reduced ability to generate
density is higher, as is the case at depth. Therefore, since maximal expiratory and inspiratory pressure postexercise sug-
most divers tend to breathe more slowly at rest and during gests that reduced respiratory muscle performance may have
exercise underwater (56, 119, 164, 278, 292, 337), inertial been a limiting factor during the swimming endurance test
impedance plays only a minor role in overall respiratory at depth.
effort. Assuming a reasonable value for peak acceleration of Increased hydrostatic pressure is depth dependent and
30 L⋅s−2 , in an exercising diver breathing a gas with density causes an increase in the POB. The increase in POB as a func-
10 g⋅L−1 , the transrespiratory pressure due to inertance tion of depth is mostly a result of the increase in the airway
would be only ∼3 cmH2 O (271). Inertance can actually be resistance which is related to gas density, which is increased in
manipulated to a diver’s benefit: if a breathing circuit is a depth dependent manner (240). Airway resistance recently
deliberately designed such that the resonant frequency of the has been calculated from measures of esophageal pressure as
system approximates the normal breathing frequency, elastic an estimate of alveolar pressure (PA ) and air flow (179, 252);
and inertial work offset each other, resulting in a reduction however, a more accurate measure of PA may be made from
in peak-to-peak (inspiratory-to-expiratory) pressure. Using the mouth pressure measured during an airway occlusion
this principle to design a tunable closed circuit breathing accomplished by a shutter placed at the mouthpiece (P.1 tech-
apparatus, Fothergill et al. demonstrated that divers optimize nique) (285, 318). P.1 also measures the level of activation
their breathing pattern by adjusting their respiratory rate to of the respiratory muscles (161), as well as central nervous
match the resonant frequency of the system (121). system respiratory drive (419). Airway resistance at sea level
using the P.1 technique are not different from those measured
using the esophageal balloon method (179, 252). In the past
Work and Energy Cost of Breathing Underwater
the P.1 was used to estimate PA and to calculate airway resis-
Respiratory muscles, like other muscles, perform work to tance in subjects submersed at depths of 45 ATA (63).
inspire and in some cases expire (WOB). However, as VE is a Another factor affecting pulmonary mechanics is the role
rate it is the POB, along with net mechanical efficiency that of NO in pulmonary resistance. Previous studies in animal
determines the energy cost of ventilation. models have demonstrated a role of NO in airway resistance,
Negative SLL causes the inspiratory muscles to work that is, increased NO reduces airway resistance in a dose-
harder, but may benefit the expiratory muscles. This is also dependent manner (103, 166). In addition, the effect of depth
associated with the increase in thoracic blood volume due to on NO production (V̇ NO ) is reduced in the cerebral vascular
its translocation from the dependent limbs during submersion as the PO2 increases in a depth-dependent manner (85) to
(78), which also results in a decrease in total lung capac- prevent an increase in PO2 to the brain to maintain normoxia
ity and residual volume (78, 272, 364) and lung compliance (30). These studies in the brain suggest a similar effect of NO
(78). Combined, these factors during submersion cause an on the smooth muscle of the respiratory airways. If this is the
increased POB due to the elastic component. Increased blood case a reduced VNO would constrict the airways and lead to an
volume in the chest may provide a small increase in the airway increased airway resistance in a depth-dependent manner. If
pressure and require less work to generate expiratory pressure there is bronchoconstriction and increased airway resistance
(PE max ) as blood is nearly incompressible. due to depth, the PA would have to be increased to accomplish
The effect of water depth on total WOB has been shown the required alveolar ventilation.
to have a dose response relationship, as have the RMT-
induced improvements in swimming endurance progressively
Gas mixing and diffusion
increased with greater depth, that is, 30% for surface, 50%
for 4’ and 60% for 55’ and 86% for 120’ of water depth There are three processes by which inspired gas mixes with
(321, 322, 425). These data strongly suggest that respiratory alveoli gas: convective mixing, Taylor dispersion, and diffu-
muscular adaptations due to RMT were primarily responsible sion (107). Convective mixing of inspired and resident gases
for increased swimming time, especially when studies using occurs predominantly due to turbulent flow in large conduct-
placebo groups failed to show any performance improvement ing airways. Taylor dispersion consists of radial diffusion
(214, 425). Protocols where subjects were studied at the time along a radial concentration gradient that occurs in laminar
of exhaustion, prior to and after RMT, show that the res- flow due to the parabolic flow distribution, where flow rate at
piratory muscles have greater strength and endurance sug- the center of a tube that at its periphery. Mixing of inspired
gesting they were less fatigued post-RMT (321, 322, 425). In and resident gases is further augmented by both Taylor diffu-
addition, it has been shown that RMT reduced the energy sion and cardiogenic oscillations. Diffusion occurs in distal
cost of swimming (351) and these changes were related to gas exchange units where flow is extremely low.
1736 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
When gas density is increased, turbulent flow occurs in while submersed, the SLL in submersion likely assisted expi-
more distal airways, thus facilitating convective mixing and ration and thus Ẇ E was not different during submersed and
improving gas exchange efficiency (271). Increased gas den- dry conditions (162).
sity is also likely to facilitate cardiogenic mixing (353). On the NO inhaled or produced results in bronchodilation of the
other hand, higher gas density should reduce the effect of Tay- airways (21, 249), thus should have an impact on breathing
lor dispersion (and thus worsen gas exchange) by reducing the resistance during submersion and could be affected by the
number of airways with laminar flow. Increased density also depth of submersion. However, recent data suggest that V̇ NO
reduces gas phase diffusivity (393). Diffusion depends on gas during submersion was not significantly different from the
diffusivity (related to molecular weight), concentration gradi- dry condition, both at rest and during exercise (162). The
ents, time for diffusion, number of molecules per unit volume, V̇ NO observed while exercising at 50% of VO2 max at 2.7 ATA
and the shape of the space in which the gas is contained (393). was slightly decreased compared to rest (162). One possibil-
While gas phase diffusion is impaired by higher gas den- ity for the lack of increase, and decrease, in V̇ NO could be
sity, convective mixing is enhanced. The net effect of these the depth-related increase in PaO2 (hyperoxia), which was
processes on pulmonary gas exchange has been illustrated proposed earlier (85), which may have blunted the increased
by measurements of arterial blood gases during hyperbaric VNO that has been reported for similar exercise intensities at 1
chamber studies (56, 126, 192, 278, 288, 292, 335-337). Over- ATA (57, 177). In addition to the high variability among sub-
all, despite mild or moderate hypercapnia, adequate blood jects due to fitness (57, 177, 239) and body types (284), the
oxygenation occurs at gas densities up to 17 g/L (337) and competing effects of exercise, submersion and depth likely
exercise performance is maintained up to 25 g/L (209). account for the lack of change or decrease reported (162).
The interaction with depth and submersion may account for
the VNO not being elevated during exercise that has typically
Airway resistance, alveolar pressure, and work of
been observed (57, 177, 239). The effects of submersion and
breathing
depth on V̇ NO during exercise may be due to the PO2 in these
Airway resistance (Raw ) increases with increasing gas den- conditions as studies at 1 ATA have shown that NO production
sity secondary to increased hydrostatic pressure, thus PA has is associate with PO2 in the surrounding tissue thus is likely
to increase proportionally to ensure adequote alveolar ven- responsible for ensuring appropriate tissue PO2 (30, 104). If
tilation (24, 405). Raw increases by the square root of the the effect of PO2 at the surface is true at depth, the decreased
increase in density (294). The increase in VE and rate of VNO at depth (i.e., increased PO2 ) previously reported (162)
flow are increased by exercise resulting in an increase in would be reasonable. In this case NO may be regulated to
Raw which requires and higher PA (163). Reviewing studies ensure PO2 to the tissues does not increase with hydrostatic
does not suggest that Raw would be affected by submersion pressure and not to minimize airway resistance which may be
per se (34). However, a recent study has shown inspiratory the case during exercise.
resistance (RawI ) and expired airway resistance (RawE ) were
decreased in submersion in resting subjects (162), in spite of
Energy cost of ventilation
the observation that Bf , VT , VE , PA during expiration, POB
during expiration that effect RawI and RawE were not signifi- Since the respiratory muscles are comprised primarily of
cantly affected by submersion (162). Based on these changes slow twitch oxidative fibers, the energy required for respi-
airway caliber was likely greater during submersion than in ratory muscle contraction is largely from oxidative mecha-
the dry conditions, in contrast to decreased VC (5,162,207) as nism (VO2 ). Using a unique protocol to determine the VO2
decreased lung volume has been reported to affect Raw (40). to breathing two studies have shown an increase in VO2 sec-
The more-negative PA during inspiration recently reported ondary to the increase WOB and POB in submersed subjects.
for submersed subjects is most likely related to SLL and not In addition to the increased WOB and POB, calculated net
submersion, per se, as the latter would increase chest wall mechanical efficiency (WOB/VO2 after correction for units)
elastic recoil at the start of inspiration (369). is reduced slightly during submersion (162, 351). It has been
The changes in Raw and PA previously reported (162) shown that RMT could reduce WOB (321, 322), and may
resulted in increased WOB and POB (162). Expectantly then, improve net mechanical efficiency (162).
POB increases with greater depth, as its components are also
increased with depth (162). The increased PA at depth is
Distributions of ventilation, blood flow, VA /Q
needed to ventilate with the greater density of gas at depth
where there is also increased airway resistance. Submersion Distribution of ventilation depends upon several factors,
has been reported to decrease inspiratory POB, mainly due including cyclic fluctuations in externally applied pressure
reduced RawI and thus the WOB per breath, at rest; however, from the respiratory muscles and regional mechanical prop-
it is increased while exercising (162). During exercise sub- erties of the lung and chest wall. Despite the vast range in path
mersed, bf has been reported to be higher than dry; however, length in the lung from large airways to gas exchange units,
WOB per breath was unchanged, and thus inspiratory Ẇ I was at 1 ATA breathing air ventilatory time constants of different
greater (162). Although POB during inspiration is increased lung units, and hence ventilation of different lung regions, are
Volume 5, October 2015 1737
The Aquatic Environment Comprehensive Physiology
Human dry, 1 ATA 1.00
Human dry, 1-7 ATA
Anesthetized dogs dry, 1 ATA VD/VT = 0.331+0.138*log10 ρ (R2 = 0.85)
40
Deadspace/tidal volume ratio
Human immersed, 1 and 19 ATA
0.75
30
PAO2 -PaO2 (mmHg)
0.50
20
0.25
10
0
0 0.1 10 100 1000
0.1 1 10 Density (g/L)
Breathing gas density (g/L)
Figure 16 Dead space/tidal volume ratio versus gas density. From
Figure 15 Alveolar-arterial PO2 difference versus gas density in four Moon et al. with permission (272).
experiments. From Moon et al. with permission (271).
with respiration. It has been predicted that this phenomenon
similar. This is largely due to the geometric properties of the improves alveolar-pulmonary capillary oxygen exchange
airways. However, at increased gas density the geometry of (13). Dense gas breathing leads to greater breath-to-breath
the lung is no longer optimal and heterogeneity of ventilation variation in pleural pressure, thus augmenting cyclic vari-
is increased. Time constants are more variable and ventilation ability in lung perfusion and improving pulmonary oxygen
of different lung units can become asynchronous (119, 295). exchange (reduced alveolar-arterial PO2 , A-aDO2 ) (12).
Gas distribution may also depend on other factors. Pleu-
ral pressure variation is not uniform over the entire lung
Pulmonary-blood transfer of oxygen
(107). Even during resting breathing at 1 ATA, regional pres-
sure changes are less in the upper than in the lower chest Increased affinity of hemoglobin for oxygen (decreased P50)
(79). When gas density is increased this variation becomes has been observed at high pressures in vitro (139, 193, 194,
exaggerated. 323, 359) and in a human in vivo study during a saturation
If regional ventilatory inequalities are appropriately dive to 49.5 ATA (355). This is probably due to pressure-
matched by changes in perfusion, VA /Q matching would be related conformational changes in hemoglobin and, to a small
preserved. Indeed, despite evidence of impaired CO2 trans- extent, binding by inert gas. The effect of these small changes
port (increased physiological dead space) breathing dense gas in hemoglobin P50 on pulmonary gas exchange or exercise
actually seems to improve VA /Q matching, as evidenced by a capacity is probably minor (403).
decrease in alveolar-arterial PO2 difference as seen in Figure
15 (60, 118, 144, 335, 423). Decreased alveolar-arterial PO2
indicates more efficient matching of ventilation and perfu- Ventilatory drive
sion. Paradoxically, dead space/tidal volume ratio (VD /VT ) is One mechanism for hypoventilation in divers may be low
usually increased (56, 249, 278, 335, 423), implying impaired ventilatory CO2 sensitivity (hypercapnic ventilatory response,
pulmonary exchange of CO2 . Immersion effects modify the HCVR) (56,191,211,274-276). Overall, however, while there
effect, as shown by Peacher et al. In their study, the increase is indeed a correlation between low HCVR and hypercapnia
in dead space/tidal volume ratio may not occur during immer- at depth there are many outliers, and this test cannot be used
sion except at extremely high PO2 (1.75 ATA) (292). as a predictor for a particular individual (56, 229, 292): in one
A previous study speculated that increased breathing gas study, only 60% of military divers with hypercapnia at depth
density reduces PAO2 − PaO2 by promoting intraregional had a low HCVR (211). It has been reported that a subject
convective mixing and thus reduced VA /Q dispersion (423), with extremely low HCVR (0.10 L⋅min−1 ⋅mmHg−1 ) had an
which affects VD /VT to a lesser degree than PAO2 − PaO2 as arterial PCO2 no higher than 43 mmHg during immersed exer-
shown in Figure 16. They proposed that the increase in VD /VT cise (VO2 2.3 L/min) at 37 m depth with a breathing gas PO2
is mostly due to impaired molecular diffusion of carbon diox- of 1.75 ATA (292).
ide (Fig. 16). Although oxygen diffusion should be similarly As pointed out earlier, HCVR can be influenced by RMT,
affected, they suggested this may be insufficient to offset the which tends to change the HCVR of both low and high respon-
convective mixing effect (97, 98). ders toward the mean (304), suggesting that RMT could
Another phenomenon is related to the fact that lung reduce the likelihood of hypercapnia in susceptible divers
perfusion is not temporally uniform, but varies cyclically (CO2 retainers).
1738 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
Effect of hyperoxia impairment in pulmonary gas exchange (374). A major role
for pulmonary oxygen toxicity is supported by results of an
It has been speculated that respiratory drive in divers may experiment in which volunteers were exposed for 28 days in a
be affected by a high partial pressure of oxygen, which for hyperbaric chamber to an ambient pressure of either 2.5 ATA
a fixed O2 fraction as in most diving, increases linearly with (atmospheric PO2 0.4 atm) or 1.5 ATA (atmospheric PO2 0.21
depth. Hyperoxia is therefore a feature of diving even using atm). Neither exposure produced venous gas emboli during
a breathing gas that is normoxic at the surface. Still higher decompression. Nevertheless, the participants exposed to the
PO2 can occur (up to 1.75 atm) when using enriched oxy- higher PO2 experienced a significant reduction in VO2 max and
gen breathing gas mixtures that are intentionally designed carbon monoxide transfer factor, with no change in DL CO
to reduce inert gas partial pressure. Hyperoxia attenuates after the lower pressure exposure (373). These data strongly
the ventilatory response to hypercapnia (77, 135, 265, 293), suggest that hyperoxia is the major contributor to pulmonary
and has been observed to decrease VE during exercise gas impairment after long saturation dives.
(3, 106, 165, 210, 264, 292, 311, 418). However, even under
extreme hyperoxia (breathing 100% O2 at 2 ATA) the rise
in arterial PCO2 during moderately heavy exercise has been Immersion pulmonary edema
observed to be modest (PaCO2 = 44 mmHg) (62). Immersion pulmonary edema (IPE, often termed swimming-
induced pulmonary edema, SIPE) causes cough, hemoptysis,
Effect of narcosis dyspnea, and hypoxemia after surface swimming or diving,
It has been suggested that inert gas narcosis, for example frequently in young, healthy individuals (156, 196, 224, 232,
when breathing nitrogen-oxygen mixtures, could contribute 242,352,416), including exceptionally fit military divers (226,
to hypercapnia during diving. Indeed, HCVR is reduced 232, 346, 409). The condition usually resolves spontaneously,
at an increased ambient pressure; however, studies using although it can be fatal in some subjects (66, 105, 352). β2
increased breathing resistance and non-narcotic gases sug- adrenergic agonists or diuretics have been used for treatment.
gest that increased gas density is the predominant mechanism Risk factors may include cold water (196,416), exertion (156,
(56, 136, 229). 346,347,409), fluid loading (409), negative SLL (375), or low
VC (346).
It has been proposed that hydrostatic pulmonary edema
Effect of pressure
is due to capillary stress failure due to high pulmonary cap-
In one study in normal volunteers breathing gases of differing illary flow and pressure (196, 225). Possible mechanisms for
densities at rest, it was observed that while increased ambi- high pulmonary vascular pressure include the additive effects
ent pressure was associated with an increase in PaCO2 , gas of increased afterload, immersion-induced increase in pul-
density appeared to have only a small effect (335). The mech- monary blood volume and pulmonary artery hypertension due
anism of this effect is unclear, but exercise studies have largely to exertion, and cold water (138, 416).
excluded pressure per se as having a significant influence on Many of the published IPE cases have occurred in mil-
ventilation (221). itary divers or combat swimmer trainees, in whom no pre-
disposing factors can generally be identified. Pulmonary
artery wedge pressure after an IPE episode has been reported
Pathological Effects of Diving as normal (156), although pulmonary capillary hyperten-
sion is likely during the acute IPE event. Bronchoalveolar
Impaired gas exchange after saturation dives lavage studies have excluded an inflammatory process. Post
During saturation dives, divers often remain in a hyperbaric event echocardiography in military cases is usually normal
environment for several days or weeks. There are reduced (156, 196, 224, 352). In nonmilitary cases identifiable pre-
opportunities for normal exercise activity, thus cardiorespi- disposing factors have been found, including left ventricular
ratory fitness is gradually reduced. Furthermore, the ambient dysfunction (20, 89) and acute coronary syndrome (137). A
PO2 is higher than normal (typically 0.4-0.5 ATA), thus review of published cases and series revealed potential risk
exposing the divers to oxygen tensions that could be mildly factors in approximately 50% of civilian cases (245). A recent
toxic to the lung. Additionally, venous gas embolism often publication observed acute reversible myocardial dysfunction
occurs during decompression, often lasting for several days. in nearly 1 /3 of 54 consecutive civilian cases of IPE (138),
Thorsen has observed that after a saturation dive to 37 ATA suggesting that during the acute event hypoxemia due to pul-
divers may experience persistent reduction in VO2 max and monary edema may have impaired cardiac function. A number
DL CO, and increased respiratory deadspace (372). Decon- of the cases reported in previous studies developed hyperten-
ditioning, the cumulative effect of venous gas embolism on sion, consistent with increased afterload and perhaps SNA as
the lung (372) and mild pulmonary oxygen toxicity may predisposing factors (138, 416).
all contribute. Logistic regression analysis of possible risk By contrast, compressed gas in isolated spaces, such as
factors after a series of saturation dives implicated both the middle ears and sinuses, has to be vented during decreases
hyperoxia and venous gas embolism as factors contributing to in pressure as depth is decreased to prevent barotrauma (24).
Volume 5, October 2015 1739
The Aquatic Environment Comprehensive Physiology
Figure 17 Mechanism of pulmonary barotrauma in a diver breathing compressed
gas and ascending while holding his breath. From Vann et al. with permission (394).
A diver breathing from diving breathing gear, breathes gas commonly tracks through the pulmonary interstitium into the
provided at essentially the same pressure as the hydrostatic mediastinum, from where it can enter the neck, subcutaneous
pressure on the chest. If however, the diver ascends after tissue or abdomen. It can also enter the pulmonary capillary
inspiration that fills the lung at depth and does not expire blood, and then arterial tree causing arterial gas embolism
gas to eliminate the expanded volume there is risk of pul- (AGE) as seen in Figure 17. Pleural rupture and pneumotho-
monary barotrauma and gas embolism (24). Another fac- rax are less common. The second mechanism is in situ bubble
tor is that the depth-dependent elevated gas pressure in the formation due to supersaturation of inert gas in tissues. This
lungs causes an increased partial pressure of the gases and occurs with slow tissue inert washout during decompression,
may introduce the potential for nitrogen narcosis and oxygen allowing tissue inert gas tension to exceed ambient pressure.
poisoning (24). De novo bubble formation can occur in tissues around joints,
in spinal cord, and other tissues. Clinical manifestations due
to the second mechanism are referred to as DCS. AGE and
Decompression illness DCS are collectively referred to as DCI.
Decompression illness (DCI) consists of a syndrome initiated Bubbles exert their immediate effects via mechanical dis-
by vascular or tissue bubbles. There are two mechanisms for tortion (pain) and vascular occlusion (stroke-like manifesta-
bubble formation in divers breathing compressed gas. Alve- tions). Secondary effects include endothelial disruption caus-
oli can hyperexpand and rupture during ascent when gas exit ing extravasation of plasma, hemoconcentration, and shock.
through the tracheobronchial tree is prevented by breath hold- Vasoplegia due to endothelial hyporesponsiveness to vasoac-
ing or bronchial obstruction. In such cases, alveolar gas most tive agents has been reported in vitro. Platelet activation
1740 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
and endothelium-leukocyte adhesion have also been reported. experimentally, exercise is carried out on a cycle ergometer,
Microparticle generation may also play a role (370,371,427). in practice locomotion in water is typically carried out by
Tissues commonly targeted include the joints (pain), spinal swimming, where the efficiency is lower and the resistance
cord, brain, and inner ear, although skin and lung can also to movement (drag) is much greater. Drag is comprised of
be involved. The most common manifestations include pain friction, form and wave forms and all are velocity dependent.
(typically near a joint), hypesthesia/paresthesias, nonspe- As the drag increases with increasing swimming velocity
cific malaise, motor weakness, mental status changes, dizzi- with an exponent from 1.7 to 2.0, the increase in the energy
ness/vertigo, and incoordination. Frank paralysis is less com- cost of swimming increases exponentially with velocity, as
mon (394). Symptoms of DCI typically occur within minutes opposed to land exercise which increases linearly with speed.
of surfacing in AGE, while DCS manifestations can also be Major differences between the sexes in physiological
delayed, often up to 24 h after surfacing. responses to the aquatic environment have not been reported,
even after correction for body size and fatness. Age does
make a difference in physiological responses to the aquatic
Summary environment. Adolescents appear to have greater sympathetic
neural response that declines with maturation, while older
The physical properties of the underwater environment make subjects have blunted cardio-renal and sympathetic responses
it unique, and impose pronounced physiological stresses on to HOWI.
humans. It imposes major stresses due to the unbreathable A major modulator of physiological responses to the
ambient medium, water temperatures higher and lower than aquatic environment is the temperature of the water, as Ts
TN temperatures, and pressure stress breathing, circulation, rapidly equilibrates with ambient temperature. A decrease in
renal-body fluid and electrolyte balance, locomotion, and Ts results in a proportional increase in heat flux from the body,
thermal balance. These stresses are all unique to the underwa- unless it is opposed by increased body insulation. Thermo-
ter environment. Even immersion at the surface of the water genesis is also triggered by decreases in Ts and Tc , which
poses different challenges vs. being in air, and these chal- can increase VO2 by threefold to fourfold, but in colder tem-
lenges are amplified with submersion and its depth. HOWI peratures thermogenesis is not sufficient to maintain a phys-
results in fluid shifts from both cell and the vascular compart- iological Tc . Immersion in water lower the TN temperature
ment, resulting in an expansion of PV and venous return, thus results in increased vascular resistance of subcutaneous tis-
increasing CO, in spite of the reduced HR as SV is increased sues, as well as muscle to increase resistance to heat loss.
by increased cardiac preload. In spite of the increased CO, This vasoconstriction is initiated by a decrease in Ts , but as
BP is generally believed to be unchanged, secondary to a Tc decreases the vasoconstriction become more pronounced.
reduction in SNA reducing vascular resistance. The reduced At a CWT, resistance is maximized and Tc is sustained at a
vascular resistance leads to increases in tissue blood flows that normal level. At temperatures below this the body cools in
are time-dependently regulated among tissues to prevent sus- a time-dependent manner, and hypothermia can occur. Insu-
tained overperfusion. The increased venous return and atrial lation suits can only partially protect divers in cold water.
stretch lead to attenuated secretion of antinatriuretic hormones Exposure to warm or hot water is even more threatening than
and vasopressin which result in a diuresis and natriuresis that cold water, and occurs in water temperatures above 35◦ C. As
act to return the PV to normal levels. As restoration of PV the body takes up heat from the water, and the ability to elim-
evolves, there may be a small overshoot and PV may decrease inate heat by evaporation is limited, body temperature can
an additional 7% as the increased CO is sustained. While the rise rapidly to dangerous levels, particularly during exercise.
diuresis peaks at about 2 h and then abates the renal-hormones In warm water, no apparent protection is known, and active
remain elevated, indicating the regulation of PV is multifac- cooling systems are required to maintain core temperature.
torial. Another major modulator of the physiological responses
The translocation of blood effects on pulmonary blood to the aquatic environment is the depth of the water, and
flow and gas compartments. There is an increase in ventilation the resultant hydrostatic pressure. There are cardio-renal
during HOWI. The increased blood volume in the lung results responses to pressure per se, however, in submersed con-
in engorgement of capillaries which displaces gas volumes ditions, the responses are primarily due to the submersion.
and may increase the risk of pulmonary edema. In spite of There are suggestions that postdive resting cardiac responses
these changes, arterial saturation is not compromised, even are depressed, but it is unclear for how long and if this has
during exercise. physiological significance. The major effects of depth are
Although resting cardiorespiratory variables are altered in on the respiratory system. In addition, to the increased fluid
HOWI, the cardiopulmonary responses to exercise are simi- volume and reduced gas volume in the lung due to immer-
lar; however, maximal aerobic power is lower, secondary to a sion/submersion, the presence of SLL, increased breathing
lower maximal CO. A negative consequence of the increased gear resistance and hydrostatic pressure on the lung increases
pulmonary blood flow and blood pressure that causes the work (power) of both inspiration and expiration, reduces
lung capillary engorgement may cause pulmonary edema, mechanical efficiency and thus increases the energy cost of
particularly during hard exercise and in cold water. While ventilation.
Volume 5, October 2015 1741
The Aquatic Environment Comprehensive Physiology
Exercising at a moderate to high intensity, especially in 20. Beinart R, Matetzky S, Arad T, Hod H. Cold water-induced pulmonary
cold water, may lead to pulmonary edema in some individu- edema. Am J Med 120: e3, 2007.
21. Belvisi MG, David Stretton C, Yacoub M, Barnes PJ. Nitric oxide is
als. Diving is very safe if done properly as there is minimal the endogenous neurotransmitter of bronchodilator nerves in humans.
risk. However, if performed improperly, there is a risk of Eur J Pharmacol 210: 221-222, 1992.
22. Bennett PB, Towse EJ. The high pressure nervous syndrome during
decompression illness, and AGE. a simulated oxygen-helium dive to 1500 ft. Electroencephalogr Clin
Neurophysiol 31: 383-393, 1971.
23. Bennett PB, Elliott D. In: Brubakk A, Neuman T, editors. The Physiol-
ogy and Medicine of Diving, 5th edn. London: W. B. Saunders Company
Ltd Publishers, 2003.
Acknowledgements 24. Bennett PB, McLeod M. Probing the limits of human deep diving.
Philos Trans R Soc Lond B Biol Sci 304:105-117, 1984.
25. Bhandari V. The role of nitric oxide in hyperoxia-induced injury to the
The authors wish to acknowledge Journal of Applied Physi- developing lung. Frontiers in Bioscience 8: e361-e369, 2003.
ology, European Journal of Applied Physiology and Elsevier 26. Bie P, Mumksdorf M, Warburg J. Renal effects of over-hydration during
vasopressin infusion in conscious dogs. Am J Physiol 247: F103-F109,
Limited, Oxford, United Kingdom for permission to use some 1984.
material from previous publications by these authors. 27. Bishop PA, Frazier S, Smith J, Jacobs D. Physiological responses to
treadmill and water running. Phys Sports Med 17: 87-94, 1989.
28. Blanker MH, Bernsen RM, Bosch JL, Thomas S, Groeneveld FP, Prins
A, Bohnen AM. Relations between nocturnal voiding frequency and
nocturnal urine production in older men: A population-based study.
References Urology 60:612-616, 2002.
29. Blatteau JE, Boussuges A, Gempp E, Pontier JM, Castagna O, Robi-
net C, Galland FM, Bourdon L. Haemodynamic changes induced by
1. Aaron E, Seow K, Johnson B, Dempsey J. Oxygen cost of exercise submaximal exercise before a dive and its consequences on bubble
hyperpnea: Implications for performance. J Appl Physiol 72: 1818- formation. Brit J Sports Med 41: 375-9, 2007.
1825, 1992. 30. Blitzer M, Loh E, Roddy M, Stamler J, Creager M. Endothelium-
2. Abbott AV, Brooks AN, Wilson DG. Human powered watercrafts. In: derived nitric oxide regulates systemic and pulmonary vascular resis-
Abbott AV, Wilson DR, editors. Human Powered Vehicles. Champaign, tance during acute hypoxia in humans. J Am Coll Cardiol 28: 591-596,
Ill: Human Kinetics, 1995, pp. 47-92. 1996.
3. Adams RP, Welch HG. Oxygen uptake, acid-base status, and perfor- 31. Bocalini DS, Serra AJ, Murad N, Levy RF. Water- versus land-based
mance with varied inspired oxygen fractions. J Appl Physiol 49: 863- exercise effects on physical fitness in older women. Geriatr Gerontol
868, 1980. Int 8(4):265-71, 2008.
4. Adnot S, Raffestin B, Eddahibi S. NO in the lung. Resp Physiol 101: 32. Boldt L, Fraszi W, Rocker L, Schefold J, Steinach M, Noack T,
109-120, 1995. Gunga H. Changes in the haemostatic system after thermoneutrial and
5. Agostoni E, Gurtner G, Torri G, Rahn H. Respiratory mechanics during hyperthermic water immersion. Eur J Appl Physiol 102(5): 547-54,
submersion and negative-pressure breathing. J Appl Physiol 21: 251- 2008.
258, 1966. 33. Bonde-Petersen F, Schultz-Pedersen L, Dragsted N. Peripheral and
6. Alberton CL, Tartaruga MP, Pinto SS, Cadore EL, Silva EM, Kruel central blood flow in man during cold, thermoneutral, and hot water
LFM. Cardiorespiratory responses to stationary running at different immersion. Aviat Space Envir Med 63(5):346-50, 1992.
cadences in water and on land. J Sport Med Phys Fitness 49: 142-151, 34. Bondurant S, Hickam JB, Isley JK. Pulmonary and circulatory effects
2009. of acute pulmonary vascular engorgement in normal subjects. J Clin
7. Alberton CL, Cadore EL, Pinto SS, Tartaruga MP, Silva EM, Kruel Invest 36: 59-66, 1957.
LFM. Cardiorespiratory, neuromuscular and kinematic responses to 35. Boussuges A, Gole Y, Mourot L, Jammes Y, Melin B, Regnard J,
stationary running performed in water and on dry land. Eur J Appl Robinet C. Haemodynamic changes after prolonged water immersion.
Physiol 111: 1157-1166, 2011. J Sports Sci 27(6):641-649, 2009.
8. Alexander RMcN. Swimming. In: Alexander RMcN, Goldspink G, 36. Boutellier U. Respiratory muscle fitness and exercise endurance in
editors. Mechanics and Energetics of Animal Locomotion. London: healthy humans. Med Sci Sports Exerc 30(7): 1169-1172. 1998.
Chapman, 1977, pp. 222-248. 37. Boutellier U, Buchel R, Kundert A, Spengler C. The respiratory system
9. American College of Sport Medicine Guidelines for Exercise Test- as an exercise limiting factor in normal trained subjects. Eur J Appl
ing and Prescription, 8th edn. Baltimore, MA: Lippincott Williams & Physiol Occup Physiol 65: 347- 353, 1992.
Wilkins, 2010. 38. Boutellier U, Piwko P. The respiratory system as an exercise limiting
10. Anthonisen NR, Bradley ME, Vorosmarti J, Linaweaver PG. Mechan- factor in normal sedentary subjects. Eur J Appl Physiol Occup Physiol
ics of breathing with helium-oxygen and neon-oxygen breathing mix- 64: 145-152, 1992.
tures in deep saturation diving. In: Lambertsen CJ, editor. Underwater 39. Braun NM, Arora NS, Rochester DF. Force-length relationship of the
Physiology IV: Proceedings of the Fourth Symposium on Underwater normal human diaphragm. J Appl Physiol: Respir, Envir Exerc Physiol
Physiology. New York, NY: Academic Press, 1971, pp. 339-345. 53: 405-412, 1982.
11. Arborelius MJ, Balldin UI, Lilja B, Lundgren CEG. Hemodynamic 40. Briscoe WA, DuBois AB. The relationship between airway resistance,
changes in man with head above water. Aerospace Med 43:592-598, airway conductance and lung volume in subjects of different age and
1972. body size. J Clin Invest 37: 1279-1285, 1958.
12. Arieli R. Cyclic perfusion of the lung by dense gas breathing may reduce 41. Broman G, Quintana M, Lindberg T, Jansson E, Kaijser L. High inten-
the (A-a)DO2. J Basic Clin Physiol Pharmacol 3: 207-221, 1992. sity deep water training can improve aerobic power in elderly women.
13. Arieli R, Farhi LE. Gas exchange in tidally ventilated and non-steadily Eur J Appl Physiol 98: 117-123, 2006.
perfused lung model. Respir Physiol 60: 295-309, 1985. 42. Buglione A, Lazzer S, Colli R, Introini E, di Prampero PE. Energetics
14. Askanazi J, Silverberg P, Foster R, Hyman A, Milic-Emili J, Kinney of best performances in elite kayakers and canoeists. Med Scie Sports
J. Effects of respiratory apparatus on breathing pattern. J Appl Physiol Exerc 43: 877-884, 2011.
48: 577-580, 1980. 43. Bushman BA, Flynn MG, Andres FF. Effects of 4 weeks of deep water
15. Balldin U, Lundgren CEG. Effects of immersion with the head above run training on running performance. Med Sci Sports Exerc 29: 694-
water on tissue nitrogen elimination in man. Aerospace Med 43:1101- 699, 1997.
1108, 1972. 44. Camporesi E, Bosco G. Ventilation, gas exchange and exercise under
16. Bardy E, Mollendorf JC, Pendergast, DR. Regional and total body active pressure. In: Bennett PB, Elliott D, editors. The Physiology and
heating and cooling of a resting diver in water of varying temperatures. Medicine of Diving, 5th edn. Edinburgh: Saunders, Elsevier Science
J Phys D:Appl Phys 41: 5501-5512, 2008. Limited, 2003, pp. 77-114.
17. Barlow HB, Macintosh FC. Shallow water Blackout. U.P.S. 48(a). Royal 45. Capelli C, Donatelli C, Moia C, Valier C, Rosa G, di Prampero PE.
Naval Personnel Committee 44: 125, 1944. Energy cost and efficiency of sculling a Venetian gondola. Eur J Appl
18. Begin R, Epstein M, Sackner MA, Levinson R, Dougherty R, Duncan Physiol 105: 635-661, 1990.
D. Effects of water immersion to the neck on pulmonary circulation 46. Capelli, C., Tarperi, C., Schena, F., Cevese, A. Energy cost and effi-
and tissue volume in man. J Appl Physiol 40:293-299, 1976. ciency of Venetian rowing on a traditional flat hull boat (Bissa). Eur J
19. Behn C, Gauer OH, Kirsch K, Eckert P. Effects of sustained intratho- Appl Physiol 105: 635- 661, 2009.
racic vascular distention on body fluid distribution and renal excretion 47. Capelli C, Termin B, Pendergast DR. Energetics of swimming at max-
in man. Pflugers Archiv 313:123-135, 1969. imal speed in humans. Eur J Appl Physiol 78: 385-393, 1998.
1742 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
48. Cassady SL, Nielsen DH. Cardiorespiratory responses of healthy sub- 78. Dahlbäck G, Jönsson E, Liner M. Influence of hydrostatic compression
jects to calisthenics performed on land versus in water. Phys Ther 72: of the chest and intrathoracic blood pooling on static lung mechanics
552-538, 1992. during head-out immersion. Undersea Biomed Res 5: 71, 1978.
49. Castellani JW, Young AJ, Kain JE, Sawka MN. Thermoregulatory 79. Daly WJ, Bondurant S. Direct measurement of respiratory pleural pres-
responses to cold water at different times of day. J Appl Physiol 87(1): sure changes in normal man. J Appl Physiol 18: 513-518, 1963.
243-6, 1999. 80. Daniel TL. Efficiency in aquatic locomotion: Limitations from sin-
50. Cavagna GA, Kaneko M. Mechanical work and efficiency in level gle cells to animals. In: Blake RW, editor. Efficiency and Econ-
walking and running. J Physiol (Lond) 268: 467-481, 1977. omy in Animal Physiology. Cambridge: University Press, 1991,
51. Celentano F, Cortili G, di Prampero PE, Cerettelli P. Mechanical aspects pp. 83-96.
of rowing. J Appl Physiol 36, 642-647, 1974. 81. Danneskiold-Samsoe B, Lyngberg K, Risum T, Telling M. The effect
52. Chatard JC, Lavoie JM, Lacour JR. Analysis of determinants of swim- of water exercise therapy given to patients with rheumatoid arthritis.
ming economy in front crawl. Eur J Appl Physiol 61: 88-92, 1990. Scand J Rehabil Med 19(1): 31-35, 1987.
53. Chatard JC, Lavoie JM, Lacour JR. Energy cost of front crawl swim- 82. Datta A, Tipton M. Respiratory responses to cold water immersion:
ming in women. Eur J Appl Physiol 63, 12-16, 1991. Neural pathways, interactions, and clinical consequences awake and
54. Chatard JC, Wilson B. Drafting distance in swimming. Med Sci Sports asleep. J Appl Physiol 100: 2057, 2006.
Exerc 35: 1176- 1181, 2003. 83. Davis JT, DuBois A. Immersion diuresis in dogs. J Appl Physiol 42:
55. Chatard JC, Wilson B. Effect of fastskin suits on performance, drag, 915-922, 1977.
and energy cost of swimming. Med Sci Sports Exerc 40: 1149-1154, 84. Dean J, Mulkey D, Henderson III R, Potter S, Putnam R. Hyperoxia,
2008. reactive oxygen species, and hyperventilation: Oxygen sensitivity of
56. Cherry AD, Forkner IF, Frederick HJ, Natoli MJ, Schinazi EA, Long- brain stem neurons. J Appl Physiol 96: 784, 2004.
phre JP, Conard JL, White WD, Freiberger JJ, Stolp BW. Predictors of 85. Demchenko IT, Boso AE, Bennett PB, Whorton AR, and Piantadosi
increased PaCO2 during immersed prone exercise at 4.7 ATA. J Appl CA. Hyperbaric oxygen reduces cerebral blood flow by inactivating
Physiol 106: 316-325, 2009. nitric oxide. J Appl Physiol 4: 597-608, 2000.
57. Chirpaz-Oddou M, Favre-Juvin A, Flore P, Eterradossi J, Delaire M, 86. Derion T, Guy HJ. Effects of age on closing volume during head-out
Grimbert F, Therminarias A. Nitric oxide response in exhaled air during water immersion. Respir Physiol 95(3): 273-80, 1994.
an incremental exhaustive exercise. J Appl Physiol 82: 1311, 1997. 87. Derion T, Guy HJ, Tsukimoto K, Schaffartzik W, Prediletto R, Poole
58. Choi JK, Lee HS, Park YS, Shiraki K. Effect of uniform and non- DC, Knight DR, Wagner PD. Ventilation-perfusion relationships in the
uniform skin temperature on thermal exchanges in water in humans. lung during head-out water immersion. J Appl Physiol 72(1): 64-72,
Inter J Biometeorol 47(2): 80- 6, 2003. 1992.
59. Christie JL, Sheldahl LM, Tristani FE, Wann LS, Sagar KB, Levankoski 88. Derion T, Reddan W, Lanphier E. Static lung load and posture effects
SG, Ptacin MJ, Sobocinsiki KA, Morris RD. Cardiovascular regulation on pulmonary mechanics and comfort in underwater exercise. Undersea
during head-out water immersion exercise. J Appl Physiol 69: 657-664, Biomed Res 19(2):85-96, 1992.
1990. 89. Dessardo S, Tomulic V, Dessardo NS. Tako-tsubo syndrome in a 12-
60. Christopherson SK, Hlastala MP. Pulmonary gas exchange during year-old girl: Exhausted heart, not broken heart. Pediatr Cardiol 32:
altered density gas breathing. J Appl Physiol 52: 221-225, 1982. 1008-1011, 2011.
61. Chu KS, Rhodes EC. Physiological and cardiovascular changes asso- 90. DiBona GF, Kopp UG. Neural control of renal function. Physiol Revs
ciated with deep water running. Sports Med 31: 33-46, 2001. 77: 176-197, 1997.
62. Clark JM, Gelfand R, Lambertsen CJ, Stevens WC, Beck G, Jr, Fisher 91. Dijkhorst-Oei LT, Boer P, Rabelink TJ, Koomans HA. Nitric
DG. Human tolerance and physiological responses to exercise while oxide synthesis inhibition does not impair water immersion-induced
breathing oxygen at 2.0 ATA. Aviat Space Environ Med 66: 336-345, renal vasodilation in humans. J Am Soc Nephrol 11(7):1293-302,
1995. 2000.
63. Clarke JR, Jaeger MJ, Zumrick JL, O’Bryan R, Spaur WH. Respiratory 92. di Prampero PE, Cortili G, Celentano F, Cerretelli PC. Physiological
resistance from 1 to 46 ATA measured with the interrupter technique. aspects of rowing. J Appl Physiol 31, 853-857, 1971.
J Appl Physiol 52: 549-555, 1982. 93. di Prampero PE. Energetics of muscular exercise. Rev Physiol Biochem
64. Clarys JP. Human morphology and hydrodynamics. In: Terauds J, Bed- Pharmacol 89: 143-222, 1981.
ingfield EW, editors. Swimming III. Baltimore: University Park Press, 94. di Prampero PE. The energy cost of human locomotion on land and in
1979, pp. 3-41. water. Int J Sports Med 7: 55-72, 1986.
65. Claybaugh JR, Pendergast DR, Davis JE, Akiba C, Pazik MM, Hong 95. di Prampero PE. Factors limiting maximal performance in humans. Eur
SK. Fluid conservation in athletes: Responses to water intake, supine J Appl Physiol 90: 420-429, 2003.
posture and immersion. J Appl Physiol 61: 7-15, 1986. 96. di Prampero PE, Pendergast DR, Wilson D, Rennie DW. Energetics of
66. Cochard G, Arvieux J, Lacour JM, Madouas G, Mongredien H, Arvieux swimming in man. J Appl Physiol 37: 1-5, 1974.
CC. Pulmonary edema in scuba divers: recurrence and fatal outcome. 97. Donald KW. Oxygen poisoning in man. I. Br Med J 1: 667-672, 1947a.
Undersea Hyperb Med 32: 39-44, 2005. 98. Donald KW. Oxygen poisoning in man. II. Br Med J 1: 712-717, 1947b.
67. Colado JC, Tella V, Triplett NT, Gonzalez LM. Effects of a short-term 99. Dowzer CN, Reilly T, Cable NT. Effects of deep and shallow water
aquatic resistance program on strength and body composition in fit running on spinal shrinkage. Br J Sports Med 32: 44-48, 1998.
young men. J Strength Cond Res 23(2): 549-59, 2009. 100. Dowzer CN, Reilly T, Cable NT, Nevill A. Maximal physiological
68. Colado JC, Triplett NT, Tella V, Saucedo P, Abellan J. Effects of aquatic responses to deep and shallow water running. Ergonomics 42: 275-281,
resistance training on health and fitness in postmenopausal women. Eur 1999.
J Appl Physiol 106(1): 113-22, 2009. 101. Ducharme MB, Lounsbury DS. Self-rescue swimming in cold water
69. Cole, G.A. Textbook of Limnology, 3rd edn, Prospect Hts., IL: Waveland the latest advice. Appl Physiol Nutr Metab 32(4): 799-807, 2007.
Press, 1983, p. 401 pp. Chap 8-9. 102. Dujic Z, Duplancic D, Marinovic-Terzic I, Bakovic D, Ivancev V, Valic
70. Comroe JH RF, Dubois AB, Briscoe WA, Carlsen E. The Lung. Z, Eterovic D, Petri NM, Wisloff U, Brubakk AO. Aerobic exercise
Chicago: Year Book Medical Publishers Inc, 1962, p. 390. before diving reduces venous gas bubble formation in humans. J of
71. Costill DL, Kovalesky J, Porter D, Kirwanm J, Fielding R, King D. Physiol 555: 637-42, 2004.
Energy expenditure during front crawl swimming: predicting success 103. Dupuy P, Shore S, Drazen J, Frostell C, Hill W, and Zapol W. Bron-
in middle distance events. Int J Sport Med 6: 266-270, 1985. chodilator action of inhaled nitric oxide in guinea pigs. J Clin Invest
72. Cowley AW. Long-term control of arterial pressure. Physiol Revs 72: 90: 421, 1992.
231-300, 1992. 104. Dweik R, Laskowski D, Abu-Soud H, Kaneko F, Hutte R, Stuehr D,
73. Cragg P, Drysdale D, Hamilton J. Ventilation in intact and glossopha- Erzurum S. Nitric oxide synthesis in the lung. Regulation by oxygen
ryngeal nerve sectioned anaesthetized rats exposed to oxygen at high through a kinetic mechanism. J Clin Invest 101: 660, 1998.
pressure. J Physiol 370: 489- 499, 1986. 105. Edmonds C, Lippmann J, Lockley S, Wolfers D. Scuba divers’ pul-
74. Craig ABJr, Dvorak M. Thermal regulation during water immersion. monary oedema: Recurrences and fatalities. Diving Hyperb Med 42:
J Appl Physiol 21: 1577-1585, 1966. 40-44, 2012.
75. Craig ABJr, Pendergast DR. Relationships of stroke rate, distance per 106. Ekblom B, Huot R, Stein EM, Thorstensson AT. Effect of changes in
stroke and velocity in competitive swimming. Med Sci Sports Exer 11: arterial oxygen content on circulation and physical performance. J Appl
278-283, 1979. Physiol 39: 71-75, 1975.
76. Crapo JD, Chang L-Y, Solt JW. Hyperoxia. Lung injury and the local- 107. Engel LA, Macklem PT. Gas mixing and distribution in the lung. Int
ization of antioxidant defenses. In: Dejoures, Comparative Physiology Rev Physiol 14: 37-82, 1977.
of Environmental Adaptation, 8th ESCP Conference, Strasbourg, Basal: 108. Epstein M. Renal effects of head-out water immersion in man: implica-
Krager, 1987, Vol. 2, pp. 163-176, 1986. tions for an understanding of volume homeostasis. Physiol Revs 58:529-
77. Dahan A, DeGoede J, Berkenbosch A, Olievier IC. The influence of 581, 1978.
oxygen on the ventilatory response to carbon dioxide in man. J Physiol 109. Epstein M. Renal effects of head-out water immersion in humans: A
428: 485-499, 1990. 15-year update. Physiol Revs 72: 563-621, 1992.
Volume 5, October 2015 1743
The Aquatic Environment Comprehensive Physiology
110. Epstein M, DeNunzio AG, Loutzenheiser RD. Effects of vasopressin 136. Gelfand R, Lambertsen CJ, Peterson RE. Human respiratory control at
administration on the diuresis of water immersion in normal humans. high ambient pressures and inspired gas densities. J Appl Physiol 48:
J Appl Physiol 51:1384-1387, 1981. 528-539, 1980.
111. Epstein M, Johnson M, DeNunzio AG. Effects of water immersion on 137. Gempp E, Boussuges A, Poyet R, Blatteau JE. Acute coronary event
plasma catecholamines in normal humans. J Appl Physiol 54:244-248, revealed by diving-related pulmonary edema. Ann Cardiol Angeiol
1983. (Paris) 58: 240-243, 2009.
112. Faerevik H, Reinertsen RE. Initial heat stress on subsequent responses 138. Gempp E, Louge P, Henckes A, Demaistre S, Heno P, Blatteau JE.
to cold water immersion while wearing protective clothing. Aviat Space Reversible myocardial dysfunction and clinical outcome in scuba divers
Envir Med 83(8): 746-50, 2012. with immersion pulmonary edema. Am J Cardiol 111: 1655-1659,
113. Farhi LE, Linnarsson D. Cardiopulmonary readjustments during graded 2013.
immersion in water at 35◦ C. Respir Physiol 30: 35-50, 1977. 139. Gerth WA. Nitrogen binding to deoxyhemoglobin at high pressures and
114. Farhi LE, Pendergast DR, Abdel-Nabi HH, Shykoff BE, Prezio JA. its relation to changes in hemoglobin-oxygen affinity. J Biol Chem 263:
Effects of gravity on pulmonary blood volume, its distribution and pul- 13515-13521, 1988.
monary hemodynamics. 15th Annual Gravitational Physiology Meet- 140. Gerth WA, Ruterbusch VL, Long ET. The influence of thermal exposure
ing. Barcelona, Spain, October 4-7, 1993. on diver susceptibility to decompression sickness. Navy Experimental
115. Figueiredo P, Zamparo P, Sousa A, Vilas-Boas JP, Fernandes RJ. An Diving Unit Technical Report 06-07, Nov 2007.
energy balance of the 200 m front crawl race. Eur J Appl Physiol 111: 141. Gething AD, Williams M, Davies B. Inspiratory resistive loading
767-777, 2011. improves cycling capacity: A placebo controlled trial. BJSM online
116. Fish F. Comparative kinematics and hydrodynamics of odontocete 38: 730-736, 2004.
cetaceans: morphological and ecological correlates with swimming per- 142. Geurts CL, Sleivert GG, Cheung SS. Effect of cold-induced vasodilation
formance. J Exp Bio 210: 2867-2877, 1998. in the index finger on temperature and contractile characteristics of
117. Florian JP, Simmons EE, Chon KH, Faes L, Shykoff BE. Cardiovascular the first dorsal interosseus muscle during cold-water immersion. Appl
and autonomic responses to physiological stressors before and after six Physiol Nutr Metab 31(6): 717-25, 2006.
hours of water immersion. J Appl Physiol 115:1275-1289, 2013. 143. Ghering MM, Keller BA, Brehm BA. Water running with and without
118. Flynn ET, Saltzman HA, Summitt JK. Effects of head-out immersion a flotation vest in competitive and recreational runners. Med Sci Sports
at 19.18 Ata on pulmonary gas exchange in man. J Appl Physiol 33: Exerc 29: 1374-1378, 1997.
113-119, 1972. 144. Gledhill N, Froese AB, Buick FJ, Bryan AC. VA/Q inhomogeneity and
119. Forkert L, Wood LD, Cherniack RM. Effect of gas density on dynamic AaDO2 in man during exercise: effect of SF6 breathing. J Appl Physiol
pulmonary compliance. J Appl Physiol 39: 906-910, 1975. 45: 512-515, 1978.
120. Forkner IF, Piantadosi CA, Scafetta N, Moon RE. Hyperoxia-induced 145. Gleim GW, Nicholas JA. Metabolic cost and heart rate responses to
tissue hypoxia: A danger? Anesthesiology 106: 1051, 2007. treadmill walking in water at different depths and temperatures. Am J
121. Fothergill DM, Joye DD, Carlson NA. Diver respiratory responses to a Sports Med 17: 248-252, 1989.
tunable closed-circuit breathing apparatus. Undersea Hyperb Med 24: 146. Glickman-Weiss E, Hearon CM, Nelson AG. Does shivering thermo-
91-105, 1997. genesis enhance the individual’s ability to maintain rectal tempera-
122. Fox RW, McDonald AT. Fluid machines. In: Fox RW, McDonald ture during immersion in cold water? Wilderness Envir Med 8(1): 3-7,
AT, editors. Introduction to Fluid Machines. New York: Wiley, 1992, 1997.
pp. 544-625. 147. Glickman EL, Caine-Bish N, Cheathan CC, Blegen M, Potkanowicz ES.
123. Frangolias DD, Rhodes EC. Maximal ventilator threshold responses The influence of age on thermosensitivity during cold water immersion.
to treadmill and water immersion running. Med Sci Sports Exerc 27: Wilderness & Envir Med 13:194-202, 2002.
1007-1013, 1995. 148. Glickman-Weiss EL, Cheatham C, Caine M, Blegen M, Marcinkiewicz
124. Frangolias DD, Rhodes EC, Taunton JE. The effect of familiarity with J, Mittleman KD. The influence of gender and menstrual phase on
deep water running on maximal oxygen consumption. J Strength Cond thermosensitivity during cold water immersion. Aviat Space Envir Med
Res 10: 215-219, 1996. 71: 715-722, 2000.
125. Frangolias DD, Tauton JE, Rodhes EC, McConkey JP, Moon M. Main- 149. Goetz, KL, Wang BC, Geer PG, Lendly RJJr, Reinhardt HW. Atrial
tenance of aerobic capacity during recovery from right foot Jones frac- stretch increases sodium excretion independently of release of atrial
ture: A case study. Clin J Sports Med 1: 54-57, 1997. peptides. Am J Physiol 250: R946-R950, 1986.
126. Fraser JA, Peacher DF, Freiberger JJ, Natoli MJ, Schinazi EA, Beck 150. Gregson W, Black MA, Jones H, Millson J, Morton J, Dawson B,
IV, Walker JR, Doar PO, Boso AE, Walker AJ, Kernagis DN, Moon Atkinson G, Green DA. Influence of cold water immersion on limb and
RE. Risk factors for immersion pulmonary edema: Hyperoxia does not cutaneous blood flow at rest. Am J Sports Med 39(6): 1316-23, 2011.
attenuate pulmonary hypertension associated with cold water-immersed 151. Guyton AC, Coleman TG. Quantitative analysis of the pathophysiology
prone exercise at 4.7 ATA. J Appl Physiol 110: 610-618, 2011. of hypertension. Cir Res 24:1-12, 1980.
127. Gabrielsen A, Sorensen VB, Pump B, Galatius S, Videbaek R, Bie 152. Hagerman, F.C. Physiology of competitive rowing. In: Garret WE,
P, Warburg J, Christensen NJ, Wroblewski H, Kastrup J, Norsk Kirkendall DT, editors. Exercise and Sport Sciences, Philadelphia: Lip-
P. Cardiovascular and neuroendocrine responses to water immer- pincott, Williams and Wilkins, 2000, pp. 843-874.
sion in compensated heart failure. Am J Physiol 279: H1931-H1940, 153. Hajduczok G, Hong SK, Claybaugh JR, Krasney JA. The role of the
2000. cardiac nerves in the hemodynamic and renal responses to head-out
128. Gabrielsen A, Warberg J, Christensen NJ, Bie P, Stadeager C, Pump water immersion in conscious dogs. Am J Physiol 253: R242-R253,
B, Norsk P. Arterial pulse pressure and vasopressin release during 1987.
graded water immersion in humans. Am J Physiol 278: R1583-R1588, 154. Hajduczok G, Miki K, Claybaugh JR, Hong SK, Krasney JA. Regional
2000. circulatory responses to head-out water immersion in conscious dogs.
129. Gappmaier E, Lake W, Nelson AG, Fisher AG. Aerobic exercise in Am J Physiol 253: R254- R263, 1987.
water versus walking on land: Effects on indices of fat reduction and 155. Hammerum MS, Bie P, Pump B, Johansen LB, Christensen NJ, Norsk P.
weight loss of obese women. J Sports Med Phys Fitness 46(4): 564-569, Vasopressin, angiotensin II and renal responses during water immersion
2006. in hydrated humans. J Physiol 511(Pt 1):323-30, 1998.
130. Gauer OH, Henry JP, Sieker HO, Wendt WE. Heart and lungs as a 156. Hampson NB, Dunford RG. Pulmonary edema of scuba divers. Under-
receptor region controlling blood volume. Am J Physiol 167: 786-794, sea Hyperb Med 24: 29-33, 1997.
1951. 157. Harms CA, Babcock MA, McClaran SR, Pegelow DF, Nickele GA,
131. Gauer OH, Henry JP. Neurohumoral control of plasma volume. In: Nelson WB, Dempsey JA. Respiratory muscle work compromises leg
Guyton AC, Cowley AW, editors. Cardiovascular Physiology II. Bal- blood flow during maximal exercise. J Appl Physiol 82: 1573-1583,
timore: University Park Press, 1976, pp. 145-189. 1997.
132. Gauer OH, Thron HL. Postural changes in the circulation. In: Hamilton 158. Harms CA, Wetter TJ, St Croix CM, Pegelow DF, Dempsey JA. Effects
WF, Dow P, editors. Handbook of Physiology. Circulation. Ameri- of respiratory muscle work on exercise performance. J Appl Physiol
can Washington, DC: Physiological Society, 1965, Section 2, Vol. III, 89: 131-138, 2000.
pp. 2409-2439. 159. Havriluk, R. Performance level differences in swimming: A meta-
133. Gautier H, Bonora M, Gaudy J. Ventillatory response of the conscious analysis of passive drag forces. Res Q Exerc Sport 76: 112-118, 2005.
or anesthetized cat to oxygen breathing. Resp Physiol 65: 181-196, 160. Havriluk, R. Variability in measurements of swimming forces: A meta-
1986. analysis of passive and active drag. Res Q Exerc Sport 78: 32-39, 2007.
134. Gea J, Hamid Q, Czaika G. Expression of myosin heavy-chain isoforms 161. Hayot M, Ramonatxo M, Matecki S, Milic-Emili J, Prefaut C. Nonin-
in the respiratory muscles following inspiratory resistive breathing. Am vasive assessment of inspiratory muscle function during exercise. Am
J Respir Crit Care Med 161(4 Pt 1):1274-1278, 2000. J Resp Crit Care 162: 2201, 2000.
135. Gelfand R, Lambertsen CJ. Dynamic respiratory response to abrupt 162. Held HE, Pendergast DR. Relative effects of submersion and increased
change of inspired CO2 at normal and high PO2. J Appl Physiol 35: pressure on respiratory mechanics, work, and energy cost of breathing.
903-913, 1973. J Appl Physiol 114: 1-13, 2013.
1744 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
163. Hesser CM, Linnarsson D, Fagraeus L. Pulmonary mechanisms and 190. Kenny GP, Denis PM, Proulx CE, Giesbrecht GG. The effect of
work of breathing at maximal ventilation and raised air pressure. J Appl dynamic exercise on resting cold thermoregulatory responses measured
Physiol, Respir Envir Exer Physiol 50: 747-753, 1981. during water immersion. Eur J Appl Physiol Occupat Physiol 79(6):
164. Hesser CM, Lind F, Linnarsson D. Significance of airway resistance 495-499, 1999.
for the pattern of breathing and lung volumes in exercising humans. 191. Kerem D, Daskalovic YI, Arieli R, Shupak A. CO2 retention during
J Appl Physiol 68: 1875-1882, 1990. hyperbaric exercise while breathing 40/60 nitrox. Undersea Hyperb
165. Hickam JB, Pryor WW, Page EB, Atwell RJ. Respiratory regulation Med 22: 339-346, 1995.
during exercise in unconditioned subjects. J Clin Invest 30: 503-516, 192. Kerem D, Melamed Y, Moran A. Alveolar PCO2 during rest and exer-
1951. cise in divers and non-divers breathing O2 at 1 ATA. Undersea Biomed
166. Hjoberg J, Shore S, Kobzik L, Okinaga S, Hallock A, Vallone J, Sub- Res 7: 17-26, 1980.
ramaniam V, De Sanctis GT, Elias JA, Drazen JM. Expression of nitric 193. Kiesow LA. Hyperbaric inert gases and the hemoglobin-oxygen
oxide synthase-2 in the lungs decreases airway resistance and respon- equilibrium in red blood cells. Undersea Biomed Res 1: 29-43,
siveness. J Appl Physiol 97: 249, 2004. 1974.
167. Hlastala MP, Berger AJ. Physiology of Respiration. New York: Oxford 194. Kiesow LA, Bless JW, Shelton JB. Oxygen dissociation in human
Press, 1996. erythrocytes: Its response to hyperbaric environments. Science 179:
168. Holm P, Sattler A, Fregosi RF. Endurance training of respiratory mus- 1236-1238, 1973.
cles improves cycling performance in fit young cyclists. BMC Physiol 195. Kjendlie PL, Ingjer F, Madsen O, Stallman RK, Gunderson JS. Differ-
4: 9, 2004. ences in the energy cost between children and adults during front crawl
169. Holmer I. Oxygen uptake during swimming in man. J Appl Physiol 33: swimming. Eur J Appl Physiol 91: 473-480, 2004.
502-509, 1972. 196. Koehle MS, Lepawsky M, and McKenzie DC. Pulmonary oedema of
170. Holmer I. Swimming physiology. Ann Physiol Anthrop 11: 269-276, immersion. Sports Med 35: 183-190, 2005.
1992. 197. Kolmogorov SV, Duplisheva OA. Active drag, useful mechanical power
171. Hong SK, Ceretelli P, Cruz JC, Rahn H. Mechanisms of respira- and hydrodynamic force coefficient in different swimming strokes at
tion during submersion under water. J Appl Physiol 27:535-538, maximal velocity. J Biomech 25: 311-318, 1992.
1969. 198. Koppers RJH, Vos PJE, Folgering HTM. Tube breathing as a new poten-
172. Hong SK, Henderson J, Olszowka A, Hurford, WE, Falke KJ, Qvist J, tial method to perform respiratory muscle training: Safety in healthy
Radermacher P, Shiraki K, Mohri M, Takeuchi H. Daily diving pattern volunteers. Respir Med 100: 714- 720, 2006.
of Korean and Japanese breath-hold divers (ama). Undersea Biomed 199. Koutedakis Y, McNaughton L, Backx K, Jones DA. Inspiratory muscle
Res 18(5-6):433-43, 1991. training improves rowing performance. Med Sci Sports Exerc 33: 803-
173. Hunt NCIII. Positive pressure breathing during water immersion. 809, 2001.
Aerosp Med. 38(7):731-735, 1967. 200. Kraft JA. Green JM. Bishop PA. Richardson MT. Neggers YH. Leeper
174. Huttunen P, Rintamaki H, Hirvonen J. Effect of regular winter swim- JD. Effects of heat exposure and 3% dehydration achieved via hot water
ming on the activity of the sympathoadrenal system before and after a immersion in repeated cycle sprint performance. J Strength Condition-
single cold water immersion. Inter J Circumpolar Health 60(3): 400- ing Res 25(3): 778-86, 2011.
406, 2001. 201. Krasney JA. Physiological Responses to Head-Out Water Immersion:
175. Illi SK, Held U, Frank I, Spengler CM. Effect of respiratory muscle Animal Studies. In: Fregly MJ and Blatteis C, editors. Handbook of
training on exercise performance in healthy individuals. Sports Med 42: Physiology: Environmental Physiology Volume II. New York: Oxford
707-724, 2012. University Press, 1996, pp. 855-888.
176. Isii Y, Matsukawa K, Tsuchimochi H, Nakamoto T. Ice-water hand 202. Krasney JA, Carroll M, Krasney E, Iwamoto J, Claybaugh JR, Hong
immersion causes a reflex decrease in skin temperature in the contralat- SK. Renal, hormonal and fluid shift responses to ANP during head-
eral hand. J Physiol Sci:JPS 57(4): 241-8, 2007. out water immersion in awake dogs. Am J Physiol 261: R188-R197,
177. Iwamoto J, Pendergast D, Suzuki H, Krasney J. Effect of graded exercise 1991.
on nitric oxide in expired air in humans. Resp Physiol 97: 333-345, 203. Krasney JA, Hajduczok G, Miki K, Claybaugh JR, Sondeen JL, Pen-
1994. dergast DR, Hong SK. Head-out water immersion: A critical evaluation
178. Iwamoto J, Sagawa S, Tajima F, Miki K, Shiraki K. Critical water of the Gauer-Henry hypothesis. In: Claybaugh JR, Wade CE, editors.
temperature during water immersion at various atmospheric pressures. Hormonal Regulation of Fluids and Electrolytes. Plenum, New York,
J Appl Physiol 64(6): 2444-2448, 1988. 1989, pp. 147-185.
179. Jackson AC, Milhorn HT, Norman JR. A reevaluation of the interrupter 204. Krasney JA, Pendergast DR. The Physiology of Water Immerson. In:
technique for airway resistance measurement. J Appl Physiol 36: 264- Taylor NAS, Groeller H, editors. Physiological Bases of Human Per-
268, 1974. formance During Work and Exercise. Edinburgh, UK: Elsevier, Chap
180. Jansky L. Janakova H. Ulicny B. Sramek P. Hosek V. Heller J. Parizkova 22. pp. 401-412, 2008.
J Changes in thermal homeostasis in humans due to repeated cold 205. Krishna GG, Danovitch GM. Renal response to central volume expan-
water immersions. Pflugers Archiv -Eur J Physiol 432(3): 368-72, sion in humans is attenuated at night. Am J Physiol 244: R48-R486,
1996. 1983.
181. Jansky L, Sramek P, Savlikova J, Ulicny B, Janakova H, Horky K. 206. Kubo K, Kanethisa H, Fukunaga T. Effects of cold and hot water
Change in sympathetic activity, cardiovascular functions and plasma immersion on the mechanical properties of human muscle and tendon
hormone concentrations due to cold water immersion in men. Eur J in vive. Clin Biomech 20(3):291-300, 2005.
Appl Physiol Occupat Physiol 74(1-2):148-52, 1996. 207. Kurss DI, Lundgren CEG, Pasche AJ. Effect of water temperature on
182. Jarrett AS. Alveolar carbon dioxide tension at increased ambient pres- vital capacity in head-out immersion. In: Bachrach AJ, Matzen MM,
sures. J Appl Physiol 21: 158-162, 1966. editors. Underwater Physiology VII: Proceedings of the 7th Symposium
183. Jimenez C, Regnard J, Robinet C, Mourot L, Gomez-Merino D, Chen- on Underwater Physiology. Bethesda, MD: Undersea and Hyperbaric
naoui M, Jammes Y, Dumoulin G, Desruelle AV, Melin B. Whole body Medical Society, 1981, pp. 297-301.
immersion and hydromineral homeostasis; effect of water temperature. 208. Lambertsen C, Kough R, Cooper D, Emmel GL, Loeschcke H, Schmidt
Eur J Appl Physiol 108(1): 49-58, 2010. C. Oxygen toxicity effects in man of oxygen inhalation at 1 and 3.5
184. Johansen LB, Bie P, Warberg J, Christensen NJ, Norsk P. Role of atmospheres upon blood gas transport, cerebral circulation and cerebral
hemodilution on renal responses to water immersion in humans. Am J metabolism. J Appl Physiol 5: 471-486, 1953.
Physiol 269: R1068-R1076, 1995. 209. Lambertsen CJ, Gelfand R, Peterson R, Strauss R, Wright WB, Dickson
185. Johansen LB, Foldager N, Stadeager C, Kristensen MS, Bie P, Warberg JGJr, Puglia C, Hamilton RWJr. Human tolerance to He, Ne, and N2
J, Kamegai M, Norsk P. Plasma volume, fluid shifts and renal responses at respiratory gas densities equivalent to He-O2 breathing at depths to
in humans during 12 h of head-out water immersion. J Appl Physiol 1200, 2000, 3000, 4000, and 5000 feet of sea water (Predictive Studies
73:539-544, 1992. III). Aviat Space Environ Med 48: 843-855, 1977.
186. Johansen LB, Jensen TU, Pump B, Norsk P. Contribution of abdomen 210. Lambertsen CJ, Owen SG, Wendel H, Stroud MW, Lurie AA, Lochner
and legs to central blood volume expansion in humans during immersion W, Clark GF. Respiratory and cerebral circulatory control during exer-
J Appl Physiol 83: 695- 699, 1997. cise at .21 and 2.0 atmospheres inspired pO2. J Appl Physiol 14: 966-
187. Johansen LB, Pump B, Warburg J, Christensen NJ, Norsk P. Preventing 982, 1959.
hemodilution abolishes natriuresis of water immersion in humans. Am 211. Lanphier E. Nitrogen-Oxygen Mixture Physiology. Phase 4. Carbon
J Physiol 275: R879-R888, 1998. Dioxide Sensitivity as a Potential Means of Personnel Selection. Phase
188. Kame V, Pendergast DR. Effects of short term and prolonged immersion 6: Carbon Dioxide Regulation Under Diving Conditions. Washington,
on the cardiovascular responses to exercise. Aviat Space Envir Med 66: DC: Navy Experimental Diving Unit, Publication No. 7-58, Washington
20-25, 1995. Navy Yard, 1958.
189. Kay D, Taaffe DR, Marino FE. Whole-body core-cooling and heat 212. Lanphier EH, Bookspan J. Carbon dioxide retention. In: Lundgren
storage during self-paced cycling performance in warm humid envi- CEG, Miller JN, editors. Lung Biology in Health and Disease: The
ronment. J Sports Sci 17:937-944, 1999. Lung at Depth. New York: Dekker, 1999, pp. 211-236.
Volume 5, October 2015 1745
The Aquatic Environment Comprehensive Physiology
213. Leblanc J. Factors affecting cold acclimation and thermogenesis in 242. Martina SD, Peacher DF, Moon RE. Immersion pulmonary edema:
man. Med Sci Sports Exer 20: S193-S196, 1988. Cardiorespiratory factors. In: UHMS 45th Annual Scientific Meeting.
214. Leddy JJ, Limprasertkul A, Patel S, Modlich F, Buyea C, Pendergast, Phoenix, AZ: Undersea & Hyperbaric Medical Society, 2012, p. D137.
DR, Lundgren CEG. Isocapnic hyperpnea training improves perfor- 243. Martin RB, Yeater RA, White MK. A simple analytical model for the
mance in competitive male runners. Eur J Appl Physiol 99: 665-676, crawl stroke. J Biomech, 14: 539-548, 1981.
2007. 244. Martin S, Cooper KE, The relationship of deep and surface skin temper-
215. Lee DT, Toner MM, McArdle WD, Vrabas IS, Pandolf KB. Thermal atures to the ventilator responses elicited during cold water immersion.
and metabolic responses to cold-water immersion at knee, hip, and Can J Physiol Pharm 56(6): 999-1004, 1978.
shoulder levels. J Appl Physiol 82(5): 1523-1530, 1997. 245. Martina SD, Peacher DF, Moon RE. Immersion pulmonary edema:
216. Leith DE, Bradley M. Ventilatory muscle strength and endurance train- Cardiorespiratory factors. In: UHMS 45th Annual Scientific Meeting.
ing. J Appl Physiol 41: 508-516, 1976. Phoenix, AZ: Undersea Hyperbaric Med Soc 2012, p. D137.
217. Lighthill, MJ. Hydrodynamics of aquatic animal propulsion. In: 246. Masumoto K, Delion D, Mercer JA. Insight into muscle activity during
Lighthill, MJ, editor. Mathematical Biofluidodynamics. Philadelphia: deep water running. Med Sci Sports Ecerc 41: 1958-1964, 2009.
Society for Industrial and Applied Mathematics, 1975, pp. 11-43. 247. McCully KK, Faulkner JA. Length-tension relationship of mammalian
218. Lindholm P, Lundgren CEG. Alveolar gas composition before and after diaphragm muscles. J Appl Physiol: Respir Envir Exer Physiol 54:
maximal breath-holds in competitive divers. Undersea Hyperb Med 33: 1681-1686, 1983.
463-467, 2006. 248. McMahon ME, Boutellier U, Smith RM, Spengler CM. Hyperpnea
219. Lindholm P, Wylegala J, Pendergast DR, Lundgren CEG. Resistive res- training attenuates peripheral chemosensitivity and improves cycling
piratory muscle training improves and maintains endurance swimming endurance. J Exp Biol 205: 3937-3943, 2002.
performance in divers. Undersea Hyperb Med 34: 169-180, 2007. 249. McMahon TJ, Moon RE, Luschinger BP, Carraway MS, Stone AE,
220. Lindholm P, Lundgren CG. The physiology and pathophysiology of Stolp BW, Gow AJ, Pawloski JR, Watke P, Singel DJ, Piantadosi CA,
human breath-hold diving. J Appl Physiol 106:284-92, 2009. Stamler JS. Nitric oxide in the human respiratory cycle. Nat Med 8:
221. Linnarsson D, Ostlund A, Lind F, Hesser CM. Hyperbaric bradycardia 711-717, 2002.
and hypoventilation in exercising men: Effects of ambient pressure and 250. Mead J. Measurement of inertia of the lungs at increased ambient
breathing gas. J Appl Physiol 87: 1428-1432, 1999. pressure. J Appl Physiol 9: 208-212, 1956.
222. Liu Z, Vargas F, Stansbury D, Sasse SA, Light RW. Comparison of the 251. Mead J. Control of respiratory frequency. J Appl Physiol 15: 325-336,
end-tidal arterial PCO2 gradient during exercise in normal subjects and 1960.
in patients with severe COPD. Chest 107: 1218-1224, 1995. 252. Mead J, Whittenberger JL. Evaluation of airway interruption technique
223. Lollgen H, van Nieding G, Kreketer H, Smidt U, Koppenhagen K, as a method for measuring pulmonary air-flow resistance. J Appl Physiol
Frank H. Respiratory gas exchange and lung perfusion in men during 6: 408-416, 1954.
and after head-out water immersion. Undersea Biomed Res 3(1): 49-56, 253. Metzler CJ, Ramsay DJ. Atrial peptide potentiates renal responses to
1976. volume expansion in conscious dogs. Am J Physiol 256: R284-R289,
224. Ludwig B, Mahon RT. Cardiopulmonary risk factors in swimming 1989.
induced pulmonary edema. Am J Respir Crit Care Med 167: A564, 254. Miki K, Hajduczok G, Hong SK, Krasney JA. Plasma volume changes
2003. during head-out water immersion in the conscious dog. Am J Physiol
225. Ludwig BB, Mahon RT, Parrish JS, Lamb C, Kerr S. Pulmonary edema 251: R284-R289, 1986a.
in combat swimmers: Clinical and bronchoalveolar lavage description 255. Miki K, Hajduczok G, Klocke MJ, Krasney JA, Hong SK, DeBold
demonstrating stress failure of the pulmonary capillaries. Undersea AJ. Atrial natriuretic factor and renal function during head-out water
Hyperb Med 31: 318, 2004. immersion in conscious dogs. Am J Physiol 251: R1000-R1008,
226. Lund KL, Mahon RT, Tanen DA, Bakhda S. Swimming-induced pul- 1986b.
monary edema. Ann Emerg Med 41: 251-256, 2003. 256. Miki K, Hajduczok G, Hong SK, Krasney JA. Extracellular fluid and
227. Lundgren CEG. Respiratory function during simulated wet dives. plasma volumes during water immersion in nephrectomized dogs. Am
Undersea Biomed Res 11:139-147, 1984. J Physiol 252:R972-R978, 1987.
228. Lundgren CEG. Immersion effects. In: Lundgren CE, Miller J, editors. 257. Miki K, Hayashida Y, Sagawa S, Shiraki K. Renal sympathetic nerve
The Lung at Depth. New York: Dekker, 1999, pp. 91-128. activity and natriuresis during water immersion in conscious dogs. Am
229. Lundgren CEG, Miller JN. Carbon dioxide retention: identification of J Physiol 256: R299-R305, 1989a.
CO2 retainers. In: Lundgren CEG, Miller JN, editors. Lung Biology 258. Miki K, Hayashida Y, Shiraki K. Role of cardiac-renal neural reflex
in Health and Disease: The Lung at Depth. New York: Dekker, 1999, in regulating sodium excretion during water immersion in conscious
p. 229. dogs. J Physiol (Lond) 545(Pt 1): 305-312, 2002.
230. MacArdle WD, Katch FI, Katch VL. Sports Exer Nutr. Philadelphia: 259. Miki K, Shiraki K, Sagawa S, DeBold AJ, Hong SK. Atrial natriuretic
Lippincott, Williams and Wilkins, 2005, p. 182. factor during head-out immersion at night. Am J Physiol 254: R235-
231. Mador MJ, Acevedo FA. Effect of respiratory muscle fatigue on breath- R241, 1988.
ing pattern during incremental exercise. Am Rev Respir Dis 143: 462- 260. Miki K, Yoshimoto M, Hayashida Y, Shiraki K. Role of cardiopul-
468, 1991. monary and carotid sinus baroreceptors in regulating renal sympathetic
232. Mahon RT, Kerr S, Amundson D, Parrish JS. Immersion pulmonary nerve activity during water immersion in conscious dogs. Am J Physiol-
edema in special forces combat swimmers. Chest 122: 383-384, 2002. Reg Integr Comp Physiol 296(6): R1807-12, 2009.
233. Maio DA, Farhi LE. Effect of gas density on mechanics of breathing. 261. Minetti AE. Passive tools for enhancing muscle-driven motion and
J Appl Physiol 23: 687-693, 1967. locomotion. J Exp Biol 207, 1265-1272, 2004.
234. Malkinson TJ, Martin S, Simper P, Cooper KE. Expired air volumes 262. Miwa C, Mano T, Saito M, Iwase S, Matsukawa T, Sugiyama Y, Koga
of males and females during cold water immersion. Canad J Physiol K. Ageing reduces sympatho-suppressive response to head-out water
Pharmacol 59(8): 843-6, 1981. immersion in humans. Acta Physiol Scand 158(1): 15-20, 1996.
235. Mantoni T, Belhage B, Pedersen LM, Pott FC. Reduced cerebral per- 263. Miwa C, Sugiyama Y, Mano T, Iwase S, Matsukawa T. Sympatho-vagal
fusion on sudden immersion in ice water, a possible cause of drowning. responses in humans to thermoneutral head-out water immersion. Aviat
Aviat Space Envir Med 78(4): 374-6, 2007. Space Envir Med 68(12):1109-1114, 1997.
236. Mantoni T, Rasmussen JH, Belhage B, Pott FC. Voluntary respiratory 264. Miyamoto Y, Niizeki K. Ventilatory responses during incremental exer-
control and cereberal blood flow velocity upon ice-water immersion. cise in men under hyperoxic conditions. Jpn J Physiol 45: 59-68, 1995.
Aviat Space Envir Med 79(8):765-8, 2008. 265. Miyamura M, Folgering HT, Binkhorst RA, Smolders FD. Ventila-
237. Marabotti C, Belardinelli A, L’Abbate A, Scalzini A, Chiesa F, Cialoni tory response to CO2 at rest and during positive and negative work in
D, Passera M, Bedini R. Cardiac function during breath-hold diving normoxia and hyperoxia. Pflugers Arch 364: 7-15, 1976.
in humans: An echocardiographic study. Undersea Hyperb Med 35(2): 266. Moening D, Scheidt A, Shepardson L, Davies GJ. Biomechanical com-
83-90, 2008. parison of water running and treadmill running. Isokinetic Exerc Scie
238. Markov G, Spengler CM, Knopfli-Lenzin C, Stuessi C, Boutellier U. 3: 207-215, 1993.
Respiratory muscle training increases cycling endurance without affect- 267. Mollendorf JC, Pendergast DR. Thermal protection system for under-
ing cardiovascular responses to exercise. Eur J Appl Physiol 85: 233- water use in cold and hot water. J Thermal Sci and Eng Appl (ASME J)
239, 2001. 2:1-12, 2010.
239. Maroun MJ, Mehta S, Turcotte R, Cosio MG, Hussain SN. Effects of 268. Mollendorf JC, Termin AC II, Oppenheim E, Pendergast DR. Effect of
physical conditioning on endogenous nitric oxide output during exer- swim suit design on passive drag. J Med Sci Sports Exerc. 36:1029-
cise. J Appl Physiol 79: 1219-1225, 1995. 1035, 2004.
240. Marshall R, Lanphier EH, DuBois AB. Resistance to breathing in nor- 269. Montpetit, R.R., Lavoie, J.M., Cazorla, G.A. Aerobic energy cost of
mal subjects during simulated dives. J Appl Physiol 9: 5-10, 1956. swimming the front crawl at high velocity in international class and
241. Martel GF, Harmer ML, Logan JM, Parker CB. Aquatic plyometric adolescent swimmers. In: Hollander AP, Huijing PA, de Groot G,
training increases vertical jump in female volleyball players. Med Sci editors. Biomechanics and Medicine in Swimming, Champaign: Human
Sports Exerc 37(10): 1814-1819, 2005. Kinetics, 1983, pp. 228-234.
1746 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
270. Montpetit R, Cazorla G, Lavoje JM. Energy expenditure during 300. Pendergast DR, di Prampero PE, Craig A, Wilson DR, Rennie DW.
front crawl swimming: a comparison between males and females. In: Quantitative analysis of the front crawl in men and women. J Appl
Ungherechts BE, Wilke K, Reischle K, editors. Swimming Science V. Physiol 43: 475-479, 1977.
Champaign: Human Kinetics, 1988, pp. 229-236. 301. Pendergast DR, DeBold AJ, Pazik M, Hong SK. Effect of head-out
271. Moon RE, Cherry AD, Stolp BW, Camporesi EM. Pulmonary gas immersion on plasma atrial natriuretic factor in man. Proc Soc Experl
exchange in diving. J Appl Physiol 106: 668-677, 2009. Bio Med 184:429-435, 1987.
272. Moon RE. Predictors of increased PaCO2 during immersed prone exer- 302. Pendergast DR, Fisher NM, Calkins E. Cardiovascular, neuromuscular,
cise at 4.7 ATA. J Appl Physiol 106: 316-325, 2009. and metabolic alterations with age leading to frailty. J Gerontol: Biol
273. Morgan DW, Kohrt WM, Bates BJ, Skinner JS. Effects of respiratory Sci 48: 61-67, 1993.
muscle endurance training on ventilatory and endurance performance 303. Pendergasty DR, Krasney JA, DeRoberts D. Effects of immersion in
of moderately trained cyclists. Int J Sports Med 8: 88-93, 1987. cool water on lung-exhaled nitric oxide at rest and during exercise.
274. Morrison JB, Florio JT, Butt WS. The effect of insensitivity to carbon Respir Physiol 115: 73-81, 1999.
dioxide on the respiratory response to exercise at 4 ATA. R Naval 304. Pendergast DR, Lindholm P, Wylegala J, Warkander D, Lundgren CEG.
Physiol Lab Rep 2: 1976. Effects of respiratory muscle training on CO2 sensitivity in SCUBA
275. Morrison JB, Florio JT, Butt WS. Observations after loss of conscious- divers. Undersea Hypobaric Med 33: 447-455, 2006.
ness under water. Undersea Biomed Res 5: 179-187, 1978. 305. Pendergast DR, Mollendorf JC. Exercising divers’ thermal protection
276. Morrison JB, Florio JT, Butt WS. Effects of CO2 insensitivity and as a function of water temperature. Undersea Hyperbaric Med 38:
respiratory pattern on respiration in divers. Undersea Biomed Res 8: 125-134, 2011.
209-217, 1981. 306. Pendergast DR, Mollendorf JC, Cuviello R, Termin AC II. Application
277. Mourot L, Bouhaddi M, Gandelin E, Cappelle S, Dumoulin G, Wolf of theoretical principles to swimsuit drag reduction. Sports Engineering
JP, Rouillon JD, Regnard J. Cardiovascular autonomic control during 9:65-76, 2006.
short-term thermoneutral and cool head-out immersion. Aviat Space 307. Pendergast DR, Mollendorf J, Zamparo P, Termin AII, Bushnell D,
Environ Med 79(1):14-20, 2008. Paschke D. The influence of drag on human locomotion in water.
278. Mummery HJ, Stolp BW, Dear GdL, Doar PO, Natoli MJ, Boso AE, Undersea Hypobaric Med 32:45-58, 2005.
Archibald JD, Hobbs GW, El-Moalem HE, Moon RE. Effects of age 308. Pendergast D, Zamparo P, di Prampero PE, Capelli C, Cerretelli P,
and exercise on physiological dead space during simulated dives at 2.8 Termin A, Craig AJr, Bushnell D, Paschke D, Mollendorf J. Energy
ATA. J Appl Physiol 94: 507-517, 2003. balance of human locomotion in water. Eur J Appl Physiol 90: 377-
279. Nishimura M. Onodera S. Effects of water temperature on cardiac 386, 2003.
autonomic nervous system modulation during supine floating. J Gravit 309. Perini R, Milesi S, Biancardi L, Pendergast DR, Veicsteinas A. Heart
Physiol: J Inter Soc Gravit Physiol 8(1):P65-P66, 2001. rate variability in exercising humans: Effect of water immersion. Eur J
280. Norfleet W, Hickey D, Lundgren C. A comparison of respiratory func- Appl Physiol 77:326-332, 1998.
tion in divers breathing with a mouthpiece or a full face mask. Undersea 310. Peterson RE, Wright WB. Pulmonary mechanical functions in man
Biomed Res 14: 503, 1987. breathing dense gas mixtures at high ambient pressures-Predictive Stud-
281. Norsk P, Bonde-Peterson F, Christensen NJ. Catecholamines, circula- ies III. In: Lambertsen CJ, editor. Underwater Physiology V: Proceed-
tion and the kidney during head-out water immersion in humans. J Appl ings of the Fifth Symposium on Underwater Physiology. Bethesda, MD:
Physiol 69: 479-484, 1990. Federation of American Societies for Experimental Biology, 1976, pp.
282. Norsk P, Epstein M. Effects of water immersion on arginine vasopressin 67-77.
release in humans. J Appl Physiol 64: 1-10, 1988. 311. Pirnay F, Marechal R, Dujardin R, Lamy M, Deroanne R, Petit JM.
283. O’Brien C, Young AJ, Lee DT, Shitzer A, Sawka MN, Pandolf KB. Exercise during hyperoxia and hyperbaric oxygenation. Int Z Angew
Role of core temperature as a stimulus for cold acclimation during Physiol 31: 259-268, 1973.
repeated immersion in 20 degrees C water. J Appl Physiol 89: 242-250, 312. Poujade B, Hautier CA, Rouard A. Determinants of the energy cost of
2000. front crawl swimming in children. Eur J Appl Physiol 87, 1-6, 2002.
284. Olin AC, Rosengren A, Thelle DS, Lissner L, Bake B, Torén K. Height, 313. Poyhonen T, Aveia J. Effect of head-out water immersion on neuro-
age, and atopy are associated with fraction of exhaled nitric oxide in a muscular function of the plantar flexor muscles. Aviat Space Envir Med
large adult general population sample. Chest 130: 1319-1325, 2006. 73(12):1215-8, 2002.
285. Otis A, Proctor D. Measurement of alveolar pressure in human subjects. 314. Prefaut C, Dubois F, Roussos C, Amaral-Marque R, Macklem PT,
Am J Physiol 152: 106, 1947. Ruff F. Influence of immersion to the neck in water on airway clo-
286. Otis AB. The work of breathing. Physiol Rev 34: 449-458, 1954. sure and distribution of perfusion in man. Respir Physiol 37:313-323,
287. Otis AB, Fenn WO, Rahn H. Mechanics of breathing in man. J Appl 1979.
Physiol 2: 592- 607, 1950. 315. Prisby R, Glickman-Weiss EL, Nelson AG. Caine N. Thermal and
288. Overfield EM, Saltzman HA, Kylstra JA, Salzano JV. Respiratory gas metabolic responses of high and low fat woman to cold water immer-
exchange in normal men breathing 0.9% oxygen in helium at 31.3 Ata. sion. Aviat Space Envir Med 70(9): 887-91, 1999.
J Appl Physiol 27: 471-475, 1969. 316. Quinn TJ, Sedory DR, Fisher BS. Physiological effects of deep water
289. Park YS, Claybaugh JR, Shiraki K, Mohri M. Renal function in hyper- running following a land based training program. Res Q Exerc Sport
baric environment. Appl Human Sci 17:1-8, 1998. 65: 386-389, 1994.
290. Park YS, Hong SK. Physiology of cold-water diving as exemplified by 317. Raffaelli C, Lanza M, Zanolla L, Zamparo P. Exercise intensity of
Korean women divers. Undersea Biomed Res 18(3): 229-41, 1991. head out water based activities (water fitness). Eur J Appl Physiol 109:
291. Park YS, Pendergast DR, Rennie DW. Decrease in body insulation with 829-838, 2010.
exercise in cool water. Undersea Biomed Res 11(2):159-168, 1984. 318. Rahn H, Fenn WO, Otis AB. Daily variations of vital capacity, residual
292. Peacher DF, Pecorella SR, Freiberger JJ, Natoli MJ, Schinazi EA, Doar air, and expiratory reserve including a study of the residual air method.
PO, Boso AE, Walker AJ, Gill M, Kernagis D, Uguccioni D, Moon J Appl Physiol 1: 725- 736, 1949.
RE. Effects of hyperoxia on ventilation and pulmonary hemodynamics 319. Rascher W, Tulassay T, Sevberth HW, Himbert U, Lang U, Scharer
during immersed prone exercise at 4.7 ATA: Possible implications for K. Diuretic and hormonal responses to head-out water immersion in
immersion pulmonary edema. J Appl Physiol 109: 68-78, 2010. nephrotic syndrome. J Ped 109:609-614, 1986.
293. Pedersen MEF, Fatemian M, Robbins PA. Identification of fast and slow 320. Ratel S, Poujade B. Comparative analysis of the energy cost during
ventilatory responses to carbon dioxide under hypoxic and hyperoxic front crawl swimming in children and adults. Eur J Aplpl Physiol 105:
conditions in humans. J Physiol 521: 273-287, 1999. 543-549, 2009.
294. Pedley T, Schroter R, Sudlow M. The prediction of pressure drop 321. Ray AD, Pendergast DR, Lundgren CEG. Respiratory muscle training
and variation of resistance within the human bronchial airways. Resp improves swimming performance at depth. Undersea Biomed Res 35:
Physiol 9: 387-405, 1970. 185-196, 2008.
295. Pedley TJ, Sudlow MF, Milic-Emili J. A non-linear theory of the dis- 322. Ray AD, Pendergast DR, Lundgren CEG. Respiratory muscle training
tribution of pulmonary ventilation. Respir Physiol 15: 1-38, 1972. reduces the work of breathing at depth. Eur J Appl Physiol 108: 811-
296. Peiffer JJ, Abbiss CR, Watson G, Nosaka K, Laursen PB. Effect of cold- 820, 2010.
water immersion duration on body temperature and muscle function. 323. Reeves RB, Morin RA. Pressure increases oxygen affinity of whole
J Sports Sci 27(10):987-993, 2009. blood and erythrocyte suspensions. J Appl Physiol 61: 486-494, 1986.
297. Pendergast DR. The effect of body cooling on oxygen transport during 324. Reilly T, Dowzer CN, Cable NT. The effect of a 6-week land and water
exercise. Med Sci Sports Exer 20: S171-S176, 1988. running training program on aerobic, anaerobic and muscle strength
298. Pendergast DR, Abdel-Nabi HH, Shykoff BE, Prezio JA, Farhi LE. measures. J Sport Sci 21: 333-334, 2002.
The influence of changes in gravity on cardiac output and blood vol- 325. Reilly T, Dowzer CN, Cable NT. The physiology of deep water running.
ume. 15th Annual Gravitational Physiology Meeting. Barcelona, Spain, J Sport Sci 21: 959-972, 2003.
October 4-7, 1993. 326. Rim H, Yun YM, Lee KM, Kwak JT, Ahn DW, Choi JK, Kim KR, Joh
299. Pendergast DR, Bushnell D, Wilson DR, Cerretelli P. Energetics of YD, Kim JY, park YS. Effect of physical exercise on renal response to
kayaking. Eur J Appl Physiol 59: 342-350, 1989. head-out water immersion. Appl Human Sci 16: 35-43, 1997.
Volume 5, October 2015 1747
The Aquatic Environment Comprehensive Physiology
327. Rodriguez FA, Keskinen K, Malvela M, Keskinen O. Oxygen uptake 355. Spaur WH, Raymond LW, Knott MM, Crothers JC, Braithwaite WR,
kinetics during free swimming: A pilot study. In: Chatard JC, editor. Thalmann ED, Uddin DF. Dyspnea in divers at 49.5 ATA: Mechanical,
Biomechanics and Medicine in Swimming IX. Saint Etienne: University not chemical in origin. Undersea Biomed Res 4: 183-198, 1977.
Press, 2003, pp. 379-390. 356. Spengler CM, Roos M, Laube SM, Boutellier U. Decreased exer-
328. Rohdin M, Petersson J, Sundbland P, Mure M, Glenny RW, Lindahl cise blood lactate concentrations after respiratory endurance training
SGE, Linnarsson D. Effects of gravity on lung diffusing capacity and in humans. Eur J Appl Physiol Occupat Physiol 79: 299-305, 1999.
cardiac output in prone and supine humans. J Appl Physiol 95: 3-10, 357. Sramek P, Simeckova M, Jansky L, Savlikova J, Vybiral S. Human
2003. physiological responses to immersion into water of different tempera-
329. Romer LM, McConnell AK, Jones DA. Effects of inspiratory muscle tures. Eur J Appl Physiol 81:436-42, 2000.
training on time- trial performance in trained cyclists. J Sports Sci 20: 358. Stocks JM, Patterson MJ, Hyde DE, Jenkins AB, Mittleman KD, Tay-
547-562, 2002. lor NA. Effects of immersion water temperature on whole-body fluid
330. Rossiter HB, Ward SA, Kowalchuk JM, Howe FA, Griffiths FA, Whipp distribution in humans. Acta Physiol Scand 182: 3-10, 2004.
BJ. Dynamic asymmetry of phosphocreatine concentration and O2 359. Stolp BW, Moon RE, Salzano JV, Camporesi EM. P-50 in divers
uptake between the on-and off-transients of moderate and high intensity decompressing from 650 msw. In: Bachrach AJ, Matzen MM, editors.
exercise in humans. J Physiol 541: 991-1002, 2002. Underwater Physiology VIII Proceedings of the Eighth Symposium on
331. Rostain JC, Balon N. Recent neurochemical basis of inert gas narcosis Underwater Physiology. Bethesda, MD: Undersea Medical Society,
and pressure effects. Undersea Hyperb Med 33: 197-204, 2006. 1984, pp. 315-326.
332. Rowell LB. Human Circulation Regulation During Physical Stress. 360. Strange K. Cellular volume homeostasis. Adv Physiol Edu 28: 155-159,
New York: Oxford University Press, 1986. 2004.
333. Rowell LB. Human Cardiovascular Control. New York: Oxford Uni- 361. Sugiyama Y, Miwa C, Xue Y, Iwase S, Suzuki H, Matsukawa T,
versity Press, 1993. Watanabe T, Kobayashi F, Mano T. Cardiovascular function in the
334. Rutlen DL, Christensen G, Helgesen KG, Ilebekk A. Influence of atrial elderly during water immersion. Environ Med 37(1): 91-94, 1993.
natriuretic factor on intravascular volume displacement in pigs. Am J 362. Svedenhag J, Seger J. Running on land and in water: Comparative
Physiol 259: H1595-H1600, 1990. exercise physiology. Med Sci Sports Exerc 24: 1155-1160, 1992.
335. Saltzman HA, Salzano JV, Blenkarn GD, Kylstra JA. Effects of pressure 363. Tajima F, Sagawa S, Iwamoto J, Miki K, Claybaugh JR, Shiraki K.
on ventilation and gas exchange in man. J Appl Physiol 30: 443-449, Renal and endocrine responses in the elderly during head-out water
1971. immersion. Am J Physiol 254: R977-R983, 1988.
336. Salzano J, Rausch DC, Saltzman HA. Cardiorespiratory responses to 364. Taylor NA, Morrison JB. Lung volume changes in response to altered
exercise at a simulated seawater depth of 1,000 feet. J Appl Physiol 28: breathing gas pressure during upright immersion. Eur J Appl Physiol
34-41, 1970. Occup Physiol 62: 122-129, 1991.
337. Salzano JV, Camporesi EM, Stolp BW, Moon RE. Physiological 365. Taylor NA, Morrison JB. Static and dynamic pulmonary compliance
responses to exercise at 47 and 66 ATA. J Appl Physiol 57: 1055-1068, during upright immersion. Acta Physiol Scand 149: 413-417, 1993.
1984. 366. Taylor NA, Morrison JB. Static respiratory muscle work during immer-
338. Samimy S, Mollendorf JC, Pendergast DR. A theoretical and experi- sion with positive and negative respiratory loading. J Appl Physiol 87:
mental analysis of diver techniques in underwater fin swimming. Sports 1397-1403, 1999.
Engineer 8(1): 27-39, 2005. 367. Termin B, Pendergast DR. Training using the stroke frequency-velocity
339. Sato D, Onshi H, Yamashiro K, Iwabe T, Shimoyama Y, Maruyama A. relationship to combine biomechanical and metabolic paradigms. J
Water immersion too the femur level affects cerebral cortical activity in Swim Res 14: 9-17, 2001.
humans; functional near-infrared spectroscopy study. Brain topography 368. Thalmann ED, Sponholtz DK, Lundgren CEG. Chamber-based system
25(2): 220-7, 2012. for physiological monitoring of submerged exercising subjects. Under-
340. Schou M, Gabrielsen A, Bruun NE, Skott P, Pump B, Dige-Petersen H, sea Biomed Res 5(3):293-300, 1978.
Frandsen E, Bie P, Warberg J, Christensen NJ, Norsk P. Angiotensin II 369. Thalmann ED, Sponholtz DK, Lundgren CEG. Effects of immersion
attenuates the natriuretic of water immersion in humans. Am J Physiol- and static lung loading on submerged exercise at depth. Undersea
Reg Integr Comparat Physiol 283(1): R187-96, 2002. Biomed Res 6: 259-290, 1979.
341. Schniepp J, Campbell TS, Powell KL, Pincivero DM. The effects of 370. Thom SR, Milovanova TN, Bogush M, Bhopale VM, Yang M, Bush-
cold-water immersion on power output and heart rate in elite cyclists. mann K, Pollock NW, Ljubkovic M, Denoble P, Dujic Z. Micropar-
J Strength Conditioning Res 16:561-566, 2002. ticle production, neutrophil activation, and intravascular bubbles fol-
342. Scott CG. Ducharme MB. Haman F. Kenny GP. Warning by immersion lowing open-water SCUBA diving. J Appl Physiol 112: 1268-1278,
or exercise affects initial cooling rate during subsequent cold water 2012.
immersion. Aviat Space Envir Med 75(11): 956-63, 2004. 371. Thom SR, Yang M, Bhopale VM, Huang S, Milovanova TN. Micropar-
343. Secher NH. Physiological and biomechanical aspects of rowing. Sports ticles initiate decompression-induced neutrophil activation and subse-
Med 15: 24-42, 1993. quent vascular injuries. J Appl Physiol 110: 340-351, 2011.
344. Shiraki K, Konda N, Sagawa S, Claybaugh JR, Hong SK. Cardiorenal- 372. Thorsen E, Hjelle J, Segadal K, Gulsvik A. Exercise tolerance and
endocrine responses to head-out immersion at night. J Appl Physiol 60: pulmonary gas exchange after deep saturation dives. J Appl Physiol 68:
176-183, 1986. 1809-1814, 1990.
345. Sherman D, Eilender E, Shefer A, Kerem D. Respiratory and occlusion- 373. Thorsen E, Segadal K, Reed JW, Elliott C, Gulsvik A, Hjelle JO.
pressure responses to hypercapnia in divers and non-divers. Undersea Contribution of hyperoxia to reduced pulmonary function after deep
Biomed Res 7: 61-74, 1980. saturation dives. J Appl Physiol 75: 657-662, 1993.
346. Shupak A, Weiler-Ravell D, Adir Y, Daskalovic YI, Ramon Y, Kerem 374. Thorsen E, Segadal K, Kambestad BK. Mechanisms of reduced pul-
D. Pulmonary oedema induced by strenuous swimming: A field study. monary function after a saturation dive. Eur Respir J 7: 4-10, 1994.
Respir Physiol 121: 25-31, 2000. 375. Thorsen E, Skogstad M, Reed JW. Subacute effects of inspiratory resis-
347. Shupak A, Guralnik L, Keynan Y, Yanir Y, Adir Y. Pulmonary edema tive loading and head-out water immersion on pulmonary function.
following closed-circuit oxygen diving and strenuous swimming. Aviat Undersea Hyperb Med 26: 137-141, 1999.
Space Environ Med 74: 1201-1204, 2003. 376. Tikuisis P. Heat balance precedes stabilization of body temperatures
348. Shykoff B, Farhi LE, Olszowka AJ, Pendergast DR, Rokitka MA, Eisen- during cold water immersion. J Appl Physiol 95(1): 89-96, 2003.
hardt CG, Morin RA. Cardiovascular responses to submaximal exercise 377. Tikuisis P.Eyolfson DA.Xu X.Giesbrecht GG. Shivering endurance and
in sustained microgravity. J Appl Physiol 81(1): 26-32, 1996. fatigue during cold water immersion in human. Eur J Appl Physiol
349. Silvers WM, Rutledge ER, Dolny DG. Peak cardiorespiratory responses 87(1): 50-8, 2002.
during aquatic and land treadmill exercise. Med Sci Sports Exerc 39: 378. Tikuisis P, Jacobs I, Moroz D, Vallerand AL, Martineau L. Comparison
969-975, 2007. of thermoregulatory responses between men and women in cold water.
350. Simanonok KE, Bernauer E. Blood volume reduction counter acts fluid J Appl Physiol 89: 1403-1411, 2000.
shifts in water immersion. Aviat Space Envir Med 64(2):139-45, 1993. 379. Tipton M, Golden FS. The influence of regional insulation on the initial
351. Simpson A-LE, Ray AD, Lundgren CEG, Pendergast DP. Energy cost responses to cold immersion. Aviat Space Envir Med 58(12):1192-6,
of breathing at depth: Effect of respiratory muscle training. Undersea 1987.
and Hyperbaric Med 39: 827-834, 2012. 380. Tipton MJ, Vincent MJ. Protection provided against the initial responses
352. Slade JBJr, Hattori T, Ray CS, Bove AA, Cianci P. Pulmonary edema to cold immersion by a partial coverage wet suit. Aviat Space Envir Med
associated with scuba diving: case reports and review. Chest 120: 1686- 60(8): 769-73, 1989.
1694, 2001. 381. Tipton MJ, Eglin CM, Golden FS. Habituation of the initial responses
353. Slutsky AS. Gas mixing by cardiogenic oscillations: A theoretical quan- to cold water immersion in humans a central or peripheral mechanism?
titative analysis. J Appl Physiol 51: 1287-1293, 1981. J Physiol 512(Pt 2): 621-8, 1998.
354. Sondeen JL, Hong SK, Claybaugh JR, Krasney JA. Effect of hydration 382. Tipton MJ. Golden FS. Higenbottam C. Mekjavic IB. Eglin CM. Tem-
state on renal responses to head-out water immersion in conscious dogs. perature dependence of habituation of the initial responses to cold-water
Undersea Biomed Res 17:395-411, 1990. immersion. Eur J Appl Physiol Occupat Physiol 78(3): 253-7, 1998.
1748 Volume 5, October 2015
Comprehensive Physiology The Aquatic Environment
383. Tipton MJ, Mekjavic IB, Eglin CM. Permanence of the habituation of 410. Wells GD, Plyley M, Thomas S, Goodman L, Duffin J. Effects of
the initial responses to cold-water immersion in humans. Eur J Appl concurrent inspiratory and expiratory muscle training on respiratory
Physiol 83(1):17-21, 2000. and exercise performance in competitive swimmers. Eur J Appl Physiol
384. Tonner PH, Poppers DM, Miller KW. The general anesthetic potency 94: 527-540, 2005.
of propofol and its dependence on hydrostatic pressure. Anesthesiology 411. Wester TE, Cherry AD, Pollock NW, Freiberger JJ, Natoli MJ, Schinazi
77: 926-931, 1992. EA, Doar PO, Boso AE, Alford EL, Walker AJ, Uguccioni DM, Ker-
385. Tonner PH, Scholz J, Koch C, Schulte AM, Esch J. The anesthetic effect nagis D, Moon RE. Effects of head and body cooling on hemodynamics
of dexmedetomidine does not adhere to the Meyer-Overton rule but is during immersed prone exercise at 1 ATA. J Appl Physiol 106:691-700,
reversed by hydrostatic pressure. Anesth Analg 84: 618-622, 1997. 2009.
386. Toussaint HM, Beleen A, Rodenburg A, Sargeant AJ, De Groot G, 412. Wierzba T.H., Musial P., Cwikalowska H. Veriable profile of individual
Hollander AP, van Ingen Schenau GJ. Propelling efficiency of front heart rate responses to cold water immersion apnea in healthy late
crawl swimming. J Appl Physiol 65, 2506-2512, 1988. adolescent men. Georgian Med News 196-197:28-38, 2011.
387. Toussaint HM, Knops W, De Groot G, Hollander AP. The mechanical 413. Wilber RL, Moffalt RJ, Scott BE, Lee DT, Cucuzzo NA. Influence of
efficiency of front crawl swimming. Med Sci Sports Exerc 22, 408-402, water run training on the maintenance of aerobic performance. Med Sci
1990. Sports Exerc 28: 1056-1062, 1996.
388. Town, GP, Bradely SS. Maximal metabolic responses of deep and 414. Wilkie DR. Equations describing power input by humans as a function
shallow water running in trained runners. Med Sci Sports Exerc 23: of duration of exercise. In: Cerretelli P, Whipp BJ, editors. Exercise
138-241, 1991. Bioenergetics and Gas Exchange. Amsterdam: Elsevier, 1980, pp. 75-
389. Tsourlou T. Benik A. Dipla K. Zafeiridis A. Kellis S. The effects 80.
of a twenty-four-week aquatic training program on muscular strength 415. Wilmore JH, Costill DL. Physiology of Sport and Exercise. Champaign,
performance in healthy elderly women. J Strength Cond Res 20(4):811- IL: Human Kinetics, 2004, pp. 89.
8, 2006. 416. Wilmshurst PT, Nuri M, Crowther A, Webb-Peploe MM. Cold-induced
390. Ueno L, Miyachi M, Matsui T, Takahashi K, Yamazaki K, Hayashi K, pulmonary oedema in scuba divers and swimmers and subsequent
Onodera S, Moritani T. Effect of aging on carotid artery stiffness and development of hypertension. Lancet 1: 62-65, 1989.
baroreflex sensitivity during head-out water immersion in men. Brazil 417. Wilson B, Thorp R. Active drag in swimming. In: Chatard JC, editor.
J Med Bio Res 38(4):629-37, 2005. Biomechanics and Medicine in Swimming IX. Saint Etienne: University
391. Valenti G, Fraszl W, Addabbo F, Tamma G, Procino G, Satta E, Cirillo Press, 2003, pp. 15-20.
M, De Santo NG, Drummer C, Bellini L, Kowoll R, Schlemmer M, 418. Wilson BA, Welch HG, and Liles JN. Effects of hyperoxic gas mixtures
Vogler S, Kirsch KA, Svelto M, Gunga HC, Water immersion is asso- on energy metabolism during prolonged work. J Appl Physiol 39: 267-
ciated with an increase in aquaporin-2 excretion in healthy volunteers. 271, 1975.
Biochimica et Biophysica Acta 1758(8):1111-1116, 2006. 419. Whitelaw W, JPDerenne, JMilic-Emili. Occlusion pressure as a mea-
392. Van Liew HD, Thalmann ED, Sponholtz DK. Diffusion-dependence of sure of respiratory center output in conscious man. Resp Physiol 23:
pulmonary gas mixing at 5.5 and 9.5 ATA. Undersea Biomed Res 6: 181-199, 1957.
251-258, 1979. 420. Wood WB. Ventilatory dynamics under hyperbaric states. In: Lambert-
393. Van Liew HD, Thalmann ED, Sponholtz DK. Hindrance to diffusive sen CJ, Greenbaum LJJr, editors. Proceedings of the Second Sympo-
gas mixing in the lung in hyperbaric environments. J Appl Physiol 51: sium on Underwater Physiology. Washington, DC: National Academy
243-247, 1981. of Sciences-National Research Council (Publication 1181), 1963, pp.
394. Vann RD, Butler FK, Mitchell SJ, Moon RE. Decompression illness. 108-123.
Lancet 377: 153-164, 2011. 421. Wood L, Bryan A. Exercise ventilatory mechanics at increased ambient
395. Vargas F, Ortiz MC, Fortepiani LA, Atucha NM, Garcia-Estan J. Age- pressure. J Appl Physiol 44: 231-237, 1978.
related changes in the pressure diuresis and natriuresis response. Am J 422. Wood LD, Bryan AC. Effect of increased ambient pressure on flow-
Physiol 273:R578-82, 1997. volume curve of the lung. J Appl Physiol 27: 4-8, 1969.
396. Veicsteinas A, Ferretti G, Rennie DW. Superficial shell insulation in 423. Wood LD, Bryan AC, Bau SK, Weng TR, Levison H. Effect of increased
resting and exercising men in cold water. J Appl Physiol 52(6):1557- gas density on pulmonary gas exchange in man. J Appl Physiol 41: 206-
1564, 1982. 210, 1976.
397. Vogel S. Life in Moving Fluids. Princeton NJ: Princeton University 424. Wright WB, Crothers JR. Effects of immersion and high pressures on
Press, 1994. pulmonary mechanical functions in man (Abstract). In: Aerospace Med-
398. Volaklis KA, Spassis AT, Tokmakidis SP. Land versus water exercise ical Association Annual Scientific Meeting Aerospace Medical Associ-
in patients with coronary artery disease: Effects on body composi- ation, p. 39, 1973.
tion, blood lipids, and physical fitness. Am Heart J 154(3):560.e1-e6, 425. Wylegala J, Pendergast DR, Gosselin LE, Warkander DE, Lundgren
2007. CEG. Respiratory muscle training improves swimming endurance in
399. Volianitis S, McConnell AK, Koutedakis Y, McNaughton L, Backx K, divers. Eur J. Appl Physiol 99(4): 393-404, 2007.
Jones DA. Inspiratory muscle training improves rowing performance. 426. Yamazaki F, Endo Y, Torii R, Sagawa S, Shiraki K. Continuous mon-
Med Sci Sports Exerc 33(5): 803-9, 2001. itoring of change in haemostatic during water immersion in humans
400. Von Diringshofen H. Die Wirkungen des hydrostatischen druckes des effect of water temperature. Aviat Space Envir Med 71(6):632-639,
wasserbades auf den blutdruck in den kapillaren un die bindegeweb- 2000.
sentwasserung 7. Kreislaufforschung 37:382-390, 1948. 427. Yang M, Kosterin P, Salzberg BM, Milovanova TN, Bhopale VM,
401. Vorosmarti J, Bradley ME, Anthonisen NR. The effects of increased Thom SR. Microparticles generated by decompression stress cause
gas density on pulmonary mechanics. Undersea Biomed Res 2: 1-10, central nervous system injury manifested as neurohypophisial ter-
1975. minal action potential broadening. J Appl Physiol 115: 1481-1486,
402. Waag T, Hesselberg O, Reinertsen RE. Heat production during cold 2013.
water immersion the role of shivering and exercise in the development 428. Yun SH, Choi JK, Park YS. Cardiovascular responses to head-out water
of hypothermia. Arctic Med Res 54(Suppl 2):60-64, 1995. immersion in Korean women breathing-hold divers. Eur J Appl Physiol
403. Wagner PD. Insensitivity of VO2 max to hemoglobin-P50 as sea level 91(5-6):708-11, 2004.
and altitude. Respir Physiol 107: 205-212, 1997. 429. Zamparo P. Effects of age and gender on the propelling efficiency of
404. Wakabayashi H, Hanai A, Yokoyama S, Nomura T. Thermal insula- the arm stroke. Eur J Appl Physiol 97, 52-58, 2006.
tion and body temperature wearing a thermal swimsuit during water 430. Zamparo P, Antonutto G, Capelli C, Francescato MP, Girardis M,
immersion. J Physiol Anthro 25(5):331-8, 2006. Sangoi R, Soule RG, Pendergast DR. Effects of body size, body density,
405. Wakabayashi H, Kaneda K, Sato D, Tochihara Y, Nomura T. Effect gender and growth on underwater torque. Scand J Med Sci Sports 6:
of non-uniform skin temperature on thermoregulatory response during 273-280, 1996.
water immersion. Eur J Appl Physiol 104(2):175-81, 2008. 431. Zamparo P, Capelli C, Cautero M, Di Nino A. Energy cost of front
406. Warkander DE, Norfleet WT, Nagasawa GK, Lundgren CE. Physi- crawl swimming at supramaximal speeds and underwater torque in
ologically and subjectively acceptable breathing resistance in divers’ young swimmers. Eur J Appl Physiol 83, 487-491, 2000.
breathing gear. Undersea Biomed Res 19: 427-445, 1992. 432. Zamparo P, Capelli C, Guerrini G. Energetics of kayaking at sub-
407. Washington LL, Gibson SJ, Helme RD. Age-related differences in the maximal and maximal speeds. Eur J Appl Physiol 80 (6): 542-548,
endogenous analgesic response to repeated cold water immersion in 1999.
human volunteers. Pain 89(1):89-96, 2000. 433. Zamparo P, Capelli C, Pendergast DR. Energetics of swimming: A
408. Watenpaugh, DE, Pump B, Bie P, Norsk P. Does gender influence historical perspective. Eur J Appl Physiol 111: 367-378, 2011.
human cardiovascular and renal responses to water immersion? J Appl 434. Zamparo P, Carignani G, Plaino L, Sgalmuzzo B, Capelli C. Energetics
Physiol 89:621-628, 2000. of locomotion with pedal driven watercrafts. J Sport Sci 26 (1): 75-81,
409. Weiler-Ravell D, Shupak A, Goldenberg I, Halpern P, Shoshani 2008.
O, Hirschhorn G, Margulis A. Pulmonary oedema and haemoptysis 435. Zamparo P, Dall’Ora A, Toneatto A, Cortesi M, Gatta G. The deter-
induced by strenuous swimming. BMJ 311: 361-362, 1995. minants of performance in master swimmers II: age related changes in
Volume 5, October 2015 1749
The Aquatic Environment Comprehensive Physiology
propelling efficiency, hydrodynamic position and energy cost of front 439. Zamparo P, Pendergast DR, Termin AIII, Minetti A. Economy and
crawl. DOI: 10.1007/s00421-012-2376- y, 2012. efficiency of swimming at the surface with fins of different size and
436. Zamparo P, Gatta G, Capelli C, Pendergast DR. Active and passive stiffness. Eur J Appl Physiol 96:459-470, 2006.
drag, the role of trunk incline. Eur J Appl Physiol 106: 195-205, 2009. 440. Zamparo P, Pendergast DR, Termin A, Minetti AE. How fins affect the
437. Zamparo P, Lazzer S, Antoniazzi C, Cedolin S, Avon R, Lesa C. The economy and efficiency of human swimming. J Exp Bio 205: 2665-
interplay between propelling efficiency, hydrodynamic position and 2676, 2002.
energy cost of front crawl in 8- to19-year-old swimmers. Eur J Appl 441. Zamparo P, Swaine I. Mechanical and propelling efficiency in swim-
Physiol 104: 689-699, 2008. ming derived from exercise using a laboratory based whole-body swim-
438. Zamparo P, Pendergast DR, Mollendorf J, Termin A, Minetti AE. An ming ergometer. J Appl Physiol 113: 584-594, 2012.
energy balance of front crawl. Eur J Appl Physiol 94, 134-144, 2005.
1750 Volume 5, October 2015
View publication stats
You might also like
- The Patophisiology of Breath Hold DivingDocument9 pagesThe Patophisiology of Breath Hold DivingJuan Manuel Arreola MéndezNo ratings yet
- Perubahan Fisiologi Ibu HamilDocument20 pagesPerubahan Fisiologi Ibu HamilMarisa IzzaNo ratings yet
- 1995 Maximeetal Circul Respir Effects Hypoxic Stress Respir PhysiolDocument11 pages1995 Maximeetal Circul Respir Effects Hypoxic Stress Respir PhysiolRaluca GuriencuNo ratings yet
- Physiology of Drowning PDFDocument63 pagesPhysiology of Drowning PDFPeter PhelpsNo ratings yet
- Diving Physiology Effects of Pressure on the Human BodyDocument23 pagesDiving Physiology Effects of Pressure on the Human BodyHafizh Zaki IrsyadNo ratings yet
- Fisiologi PenyelamanDocument17 pagesFisiologi PenyelamandararidiniNo ratings yet
- Kidney Physiology and Pathophysiology During Heat Stress and The Modification by Exercise Dehydration Heat Acclimation and AgingDocument53 pagesKidney Physiology and Pathophysiology During Heat Stress and The Modification by Exercise Dehydration Heat Acclimation and AgingElda Oncossya PanggabeanNo ratings yet
- Water and electrolyte balance guide for athletesDocument10 pagesWater and electrolyte balance guide for athletesFavio Alvarez De BejarNo ratings yet
- 115 FullDocument11 pages115 FullYashmine CastrenceNo ratings yet
- Death Due To DrowningDocument3 pagesDeath Due To DrowningALTAF HUSAINNo ratings yet
- Cold Water Immersion: A Review of The Literature For Winter SwimmingDocument8 pagesCold Water Immersion: A Review of The Literature For Winter SwimmingUrs MüllerNo ratings yet
- DrowningDocument14 pagesDrowningkrisnandarNo ratings yet
- Nutrients: of Mice and Men-The Physiology, Psychology, and Pathology of OverhydrationDocument14 pagesNutrients: of Mice and Men-The Physiology, Psychology, and Pathology of OverhydrationSuis MionooNo ratings yet
- 2012, Medicina de Altura - Revisión J. WestDocument9 pages2012, Medicina de Altura - Revisión J. WestMarco Antonio Garcia ValenzuelaNo ratings yet
- Optimal Composition of Fluid-Replacement Beverages: Comprehensive Physiology April 2014Document47 pagesOptimal Composition of Fluid-Replacement Beverages: Comprehensive Physiology April 2014rockhountNo ratings yet
- Truijens & Rodriguez (World Book of Swimming - Nova Science 2011) PDFDocument16 pagesTruijens & Rodriguez (World Book of Swimming - Nova Science 2011) PDFAngie TarazonaNo ratings yet
- DivingDocument5 pagesDivingNantini GopalNo ratings yet
- Scientifi C Evidence-Based Effects of Hydrotherapy On Various Systems of The BodyDocument12 pagesScientifi C Evidence-Based Effects of Hydrotherapy On Various Systems of The BodyDeni MalikNo ratings yet
- Inotul Si InimaDocument8 pagesInotul Si InimaMihail RonnyNo ratings yet
- The Management of Near DrowningDocument8 pagesThe Management of Near DrowningneddiantiseptikaNo ratings yet
- Respiratory Research Final Draft 1Document19 pagesRespiratory Research Final Draft 1api-733590799No ratings yet
- Aquatic Therapy ScientificAspects PDFDocument14 pagesAquatic Therapy ScientificAspects PDFCarlos Ernesto AriasNo ratings yet
- Osmotic HomeostasisDocument11 pagesOsmotic HomeostasisSamuel RodríguezNo ratings yet
- Dry Weight in HemodialysisDocument12 pagesDry Weight in HemodialysisAnik PriyaniNo ratings yet
- Jurnal Body Fluid AnalisisDocument7 pagesJurnal Body Fluid AnalisisMelati GanezaNo ratings yet
- Scientific Evidence-Based Effects of Hydrotherapy On Various Systems of The BodyDocument16 pagesScientific Evidence-Based Effects of Hydrotherapy On Various Systems of The BodyZulaikah Nur IstiqomahNo ratings yet
- Diving Physiology of Sea AnimalsDocument5 pagesDiving Physiology of Sea AnimalsSanahKumarNo ratings yet
- Nutrition Considerations PDFDocument11 pagesNutrition Considerations PDFNutricion Buap ComdeNo ratings yet
- Fluid Ingestion and Exercise Hyperthermia: Implications For Performance, Thermoregulation, Metabolism and The Development of FatigueDocument12 pagesFluid Ingestion and Exercise Hyperthermia: Implications For Performance, Thermoregulation, Metabolism and The Development of Fatiguecraig1014No ratings yet
- Ascites Syndrome in Broilers Physiological and Nutritional PerspectivesDocument11 pagesAscites Syndrome in Broilers Physiological and Nutritional PerspectivesMin Min MinNo ratings yet
- SMW 09706Document11 pagesSMW 09706vlachos1821No ratings yet
- Assessment of Dry Weight in Hemodialysis: An Overview: ReviewDocument12 pagesAssessment of Dry Weight in Hemodialysis: An Overview: ReviewAshleyNo ratings yet
- Thermal Effects of Water on Heart Rate, Blood Pressure and Respiratory SystemDocument8 pagesThermal Effects of Water on Heart Rate, Blood Pressure and Respiratory SystemOwooluwa AdegboyegaNo ratings yet
- Respiratory Physiology & NeurobiologyDocument5 pagesRespiratory Physiology & Neurobiologyrafi surya ghaniNo ratings yet
- Freedive Earth - The Mammalian Diving ReflexDocument5 pagesFreedive Earth - The Mammalian Diving ReflexAryaNo ratings yet
- 1 Environmental Physiology and Diving MedicineDocument10 pages1 Environmental Physiology and Diving MedicinededdyNo ratings yet
- Comparative Human Ventilatory Adaptation To High AltitudeDocument20 pagesComparative Human Ventilatory Adaptation To High AltitudeAbeer SallamNo ratings yet
- Effects of CO2 on trout health and growth in recirculating aquacultureDocument7 pagesEffects of CO2 on trout health and growth in recirculating aquaculturePrajwolNo ratings yet
- A Review of Hydration.6Document8 pagesA Review of Hydration.6Paulo TsunetaNo ratings yet
- Causes, Effects and Treatment of Submersion InjuriesDocument9 pagesCauses, Effects and Treatment of Submersion InjuriesJ-two PallayaNo ratings yet
- ARTÃ CULO Limitaciones en La Actividad Fã SicaDocument14 pagesARTÃ CULO Limitaciones en La Actividad Fã SicaTatiana FlorianNo ratings yet
- Epidemiology, Pathophysiology, and Management of Hyponatremic EncephalopathyDocument11 pagesEpidemiology, Pathophysiology, and Management of Hyponatremic EncephalopathyAnonymous Us5v7C6QhNo ratings yet
- The Role of Training in The Development of Adaptive Mechanisms in FreediversDocument14 pagesThe Role of Training in The Development of Adaptive Mechanisms in Freediversalena292007No ratings yet
- Diving Medicine in Clinical Practice: Lars Eichhorn, Dieter LeykDocument14 pagesDiving Medicine in Clinical Practice: Lars Eichhorn, Dieter LeykyantiNo ratings yet
- Senam OtakDocument15 pagesSenam OtakDewi WulandariNo ratings yet
- Brain Electrolytes: Water Intoxication, Also Known As Water Poisoning or DilutionalDocument4 pagesBrain Electrolytes: Water Intoxication, Also Known As Water Poisoning or DilutionalSivasakty ShanuNo ratings yet
- Ploidy Influence on Saltwater Adaptation and Stress Response in Rainbow TroutDocument12 pagesPloidy Influence on Saltwater Adaptation and Stress Response in Rainbow TroutanimoysonrieNo ratings yet
- Cardiovascular Adaptation To High-Altitude HypoxiaDocument19 pagesCardiovascular Adaptation To High-Altitude HypoxiaChethan UpadhyayaNo ratings yet
- The Physiologic Basis of High-Altitude DiseasesDocument12 pagesThe Physiologic Basis of High-Altitude DiseasesMario LosadaNo ratings yet
- Direct Peritoneal ResuscitationDocument5 pagesDirect Peritoneal ResuscitationDanny NguyenNo ratings yet
- MicroAlgae Test For Determining Death by DrowningDocument7 pagesMicroAlgae Test For Determining Death by DrowningmuyenzoNo ratings yet
- Fefelethu Motlhoiwa - 34903577 - Life 322 - Assignment 3Document7 pagesFefelethu Motlhoiwa - 34903577 - Life 322 - Assignment 3Fefelethu MotlhoiwaNo ratings yet
- Physiology of Breathlessness Associated With Pleural EffusionsDocument8 pagesPhysiology of Breathlessness Associated With Pleural EffusionsKevin Julio Huayllane SolisNo ratings yet
- The Use of Hypertonic Saline For Fluid Resuscitation in SepsisDocument4 pagesThe Use of Hypertonic Saline For Fluid Resuscitation in Sepsisgabro saputraNo ratings yet
- Murray 2016 Experimental PhysiologyDocument5 pagesMurray 2016 Experimental PhysiologyCender U. QuispeNo ratings yet
- Nutrients: Hydration Status and Cardiovascular FunctionDocument21 pagesNutrients: Hydration Status and Cardiovascular FunctionS Dian RNo ratings yet
- Pulmonary Arterial Hypertension (Ascites Syndrome) in Broilers: A Review ReviewDocument20 pagesPulmonary Arterial Hypertension (Ascites Syndrome) in Broilers: A Review ReviewAh ZainiNo ratings yet
- Overventilation and Lung DamageDocument8 pagesOverventilation and Lung DamageDaniel MoralesNo ratings yet
- Effects of Aquatic Exercise On Mental Health, Functional Autonomy and Oxidative Stress in Depressed Elderly Individuals PDFDocument7 pagesEffects of Aquatic Exercise On Mental Health, Functional Autonomy and Oxidative Stress in Depressed Elderly Individuals PDFMARIA CAMILA RENGIFO CAICEDONo ratings yet
- Human Physiology in An Aquatic EnvironmentDocument47 pagesHuman Physiology in An Aquatic EnvironmentMARIA CAMILA RENGIFO CAICEDONo ratings yet
- Analysis of Cognitive Abilities in Female Swimmers PDFDocument9 pagesAnalysis of Cognitive Abilities in Female Swimmers PDFMARIA CAMILA RENGIFO CAICEDONo ratings yet
- Effects of Aquatic Exercise On Mental Health, Functional Autonomy and Oxidative Stress in Depressed Elderly Individuals PDFDocument7 pagesEffects of Aquatic Exercise On Mental Health, Functional Autonomy and Oxidative Stress in Depressed Elderly Individuals PDFMARIA CAMILA RENGIFO CAICEDONo ratings yet
- Analysis of Cognitive Abilities in Female Swimmers PDFDocument9 pagesAnalysis of Cognitive Abilities in Female Swimmers PDFMARIA CAMILA RENGIFO CAICEDONo ratings yet
- Male - Contraceptive WikiDocument11 pagesMale - Contraceptive WikiUnggul YudhaNo ratings yet
- Sections: Tips For Wiki Navigation & PrintingDocument2 pagesSections: Tips For Wiki Navigation & PrintingRutvik ShahNo ratings yet
- Journal NeurotraumaDocument34 pagesJournal NeurotraumaCarolina MuñozNo ratings yet
- Drug Study (Ranitidine, Citicoline, Enalapril, Aspilet, Cefuroxime Etc)Document9 pagesDrug Study (Ranitidine, Citicoline, Enalapril, Aspilet, Cefuroxime Etc)gino_23_28No ratings yet
- A Course of Home Study For Pharmacists (1896)Document620 pagesA Course of Home Study For Pharmacists (1896)dluker2pi1256No ratings yet
- HeroineDocument4 pagesHeroineMarla DaigneaultNo ratings yet
- Reference CardsDocument2 pagesReference Cardsbonjh0eNo ratings yet
- Apotek Agung Medika Farma: Jalan Ki Warsiki Blok Ki Buyut Desa Kedungdalem Gegesik - Kabupaten CirebonDocument10 pagesApotek Agung Medika Farma: Jalan Ki Warsiki Blok Ki Buyut Desa Kedungdalem Gegesik - Kabupaten CirebonagungNo ratings yet
- Central and Peripheral Factors in FatigueDocument6 pagesCentral and Peripheral Factors in FatigueEduardo VieyraNo ratings yet
- Test Bank Pharmacology 3rd Edition Brenner StevensDocument24 pagesTest Bank Pharmacology 3rd Edition Brenner StevensAmberLongpmtg100% (44)
- The Pharmacology of Inhaled Anesthetics - Eger, Edmond I., 1930 - Eisenkraft, James B Weiskopf, - 2002 - (S.L.) - Edmond I Eger - Anna's ArchiveDocument360 pagesThe Pharmacology of Inhaled Anesthetics - Eger, Edmond I., 1930 - Eisenkraft, James B Weiskopf, - 2002 - (S.L.) - Edmond I Eger - Anna's ArchiveBhrahmadhathan U M TNo ratings yet
- Fonc 13 1226289Document19 pagesFonc 13 1226289Shady tantawyNo ratings yet
- Positive and Negative Effects of Cannabis On Health - 2019Document9 pagesPositive and Negative Effects of Cannabis On Health - 2019Carlos Ferrete JuniorNo ratings yet
- PUSKESMAS TAOPA Laporan Pemakaian dan Lembar Permintaan Obat (LPLPO) Bulan Agustus 2020Document25 pagesPUSKESMAS TAOPA Laporan Pemakaian dan Lembar Permintaan Obat (LPLPO) Bulan Agustus 202012rahmatajangNo ratings yet
- Approach to Diagnosing Wide QRS Complex TachycardiaDocument72 pagesApproach to Diagnosing Wide QRS Complex TachycardiaGadisa DejeneNo ratings yet
- (2020) Effect of Rectal Ozone (O3) in Severe COVID-19 Pneumonia - Preliminary ResultsDocument9 pages(2020) Effect of Rectal Ozone (O3) in Severe COVID-19 Pneumonia - Preliminary ResultsVu TranNo ratings yet
- Hemophilia and Inhibitors - ASHDocument6 pagesHemophilia and Inhibitors - ASHinterna MANADONo ratings yet
- PPIs and Kidney DiseaseDocument6 pagesPPIs and Kidney DiseaseSonia jolandaNo ratings yet
- Pathological Profile and Recovery Rate in Patients With Drug-Induced Acute Kidney Injury: A Retrospective Study From North-East IndiaDocument7 pagesPathological Profile and Recovery Rate in Patients With Drug-Induced Acute Kidney Injury: A Retrospective Study From North-East IndiaIJAR JOURNALNo ratings yet
- Basic Concepts of Pharmacology - WikiVet EnglishDocument1 pageBasic Concepts of Pharmacology - WikiVet EnglishŠhâh NawazNo ratings yet
- An Approach To Treating Long COVID: First Line TherapiesDocument3 pagesAn Approach To Treating Long COVID: First Line TherapiesflorentinaNo ratings yet
- MP 2015162Document7 pagesMP 2015162Luis Juárez GtzNo ratings yet
- Antibiotic ClassificationDocument29 pagesAntibiotic ClassificationDr Sumant Sharma100% (1)
- Prevention and Control of AidsDocument30 pagesPrevention and Control of Aidsutsavshrestha05No ratings yet
- A6967DE8-A1F0-446A-B423-6FB2815A2E4D (2)Document74 pagesA6967DE8-A1F0-446A-B423-6FB2815A2E4D (2)zainNo ratings yet
- Exhibit 1 18 Presents Common Size Income Statements and Balance Sheets ForDocument1 pageExhibit 1 18 Presents Common Size Income Statements and Balance Sheets ForTaimur TechnologistNo ratings yet
- Minims Povidone Iodine 5% W/V Eye Drops, Solution: Adults (Including The Elderly)Document7 pagesMinims Povidone Iodine 5% W/V Eye Drops, Solution: Adults (Including The Elderly)royNo ratings yet
- 03 Expert Opinion FemiSan A Plus Maca-ENG PDFDocument13 pages03 Expert Opinion FemiSan A Plus Maca-ENG PDFPredrag IvanovićNo ratings yet
- Questions From Pharmacology Test Prep 638046474180980097Document5 pagesQuestions From Pharmacology Test Prep 638046474180980097mohamedhaiderabidNo ratings yet
- Nifedipine Drug StudyDocument2 pagesNifedipine Drug StudyMary Shane MoraldeNo ratings yet