Professional Documents
Culture Documents
Bony Pelvis, Pelvic Walls, and Pelvic Measurements Text - P
Uploaded by
Shouq Khair AllaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bony Pelvis, Pelvic Walls, and Pelvic Measurements Text - P
Uploaded by
Shouq Khair AllaCopyright:
Available Formats
Bony pelvis, pelvic walls, and pelvic
measurements
Dr. Akef Obeidat
Objectives
1. Demonstrate knowledge of the gross anatomy of the bony pelvis, pelvic walls, and pelvic
measurements.
2. Demonstrate knowledge of the gross anatomy of the internal female reproductive organs.
3. Recognize and describe the appearance of: The uterus, the cervix, the vagina, the fallopian
tubes, and the ovaries.
Keywords
Bony pelvis
Pelvic walls
Pelvic diaphragm
Female reproductive organs
Female genitalia
Uterus
Cervix
Vagina
Fallopian tubes
Oviduct
Ovaries
Broad ligaments
Lecture
The Bony Pelvis
The bony pelvis provides strong, stable connection between the trunk and the lower extremities.
It contains, supports, and protects the pelvic viscera.
It is composed of 4 bones:
2 innominate (hip) bones.
Sacrum.
Coccyx.
The two hip bones articulate with each other anteriorly at the symphysis pubis, and posteriorly
with the sacrum at the sacroiliac joints.
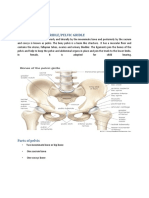
Hip Bone (Innominate Bone)
In children, each hip bone consists of the ilium, the ischium, and the pubis.
At puberty, these 3 bones fuse together.
The Ilium
Consists of an upper fan-shaped segment (ala=wing=fossa), and an inferior body.
The arcuate line (iliopectineal line) is a curved bony ridge on the interior surface dividing
the iliac fossa from the lower portion of the ilium. It also divides the false from the true
pelvis.
The curved upper edge of the ilium is known as iliac crest which runs between anterior and
posterior iliac spines.
Below these spines are the corresponding inferior iliac spines.
The Ischium
Consists of:
1. A lower thick, bony process (ischial tuberosity) fusing with the inferior ramus of the pubis
(ischiopubic ramus) forming the lower perimeter of the obturator foramen.
2. An upwardly directed bony process that fuses with the ilium and the superior ramus of the
pubis, forming part of the upper perimeter of the obturator foramen.
3. The ischial spine protrudes 2-3 cm superior to the ischial tuberosity.
4. The lesser sciatic notch: curved bony edge (inwardly) connecting the ischial spine to the
tuberosity.
5. The greater sciatic notch is a similar but a larger curve that extends between the ischial
spine and the articular surface of the sacroiliac joint.
N.B. The sciatic notches are converted into the greater and lesser sciatic foramina by the
presence of the sacrotuberous and sacrospinous ligaments.
The pubis
V shaped, with a body (apex pointing medially), and two rami (superior and inferior).
The pubic symphysis consists of a fibro- cartilaginous disk between the opposed pubic
articular surfaces.
The superior ramus unites with the ilium and the ischium.
The inferior ramus joins the ischial ramus.
The body of the pubis bears the pubic crest, a rounded superomedial prominence.
The pubic tubercle, on either side of the pubic crest, is an upward directed elevation on the
body, 1-2 cm lateral to the pubic symphysis.
The superior ramus has a pectineal line (pecten pubis).
The Obturators
Foramen, Membrane, and Internus Muscle:
Foramen: An ovoid aperture surrounded by a continuous rim of bone, derived from pubis, ilium,
and ischium.
Membrane: A fibrous sheath that almost completely encloses the obturator foramen leaving a
small superomedial gap through which pass the obturator nerve and vessels.
Internus Muscle:
A lateral rotator of the femur at the hip joint and is supplied by a branch from the sacral
plexus (nerve to the obturator internus from L5, S2, & S3).
It arises from the pelvic surface of the obturator membrane and the adjoining part of the hip
bone.
The muscle fibers converge to a tendon which leaves the pelvis through the lesser sciatic
foramen to be inserted in the greater trochanter of femur.
Upon the perineal surface of the muscle, the obturator fascia (covering the muscle) form a
tunnel called pudendal canal (Alcock's fascia). It transmits the pudendal nerve and the
internal pudendal vessels. It connects the lesser sciatic foramen to the posterior edge of the
perineal membrane (immediately above the upper edge of the sacrotuberous ligament).
The Acetabulum
A depression on the outer surface of the hip bone which articulates with the hemispherical
head of femur.
It is formed by parts of the ilium, the ischium, and the pubis. The Y-shaped line of fusion is
often visible in the floor of the socket.
The raised circumferential perimeter of the acetabulum is interrupted inferiorly forming the
acetabular notch. This notch in life is spanned by the transverse acetabular ligament.
The Sacrum
It is the fusion of the 5 sacral vertebrae.
It is a wedge-shaped bone with forward concavity.
The upper border (the base): 2 alae, promontory, and the articular surface. It articulates with
L5 via 2 superior articular processes.
The narrow inferior border (apex) articulates with the coccyx.
The sacrum is tilted forward so that it forms an angle with L5 called lumbosacral angle.
Laterally, the sacrum articulates with the 2 iliac bones to form the sacroiliac joints.
The anterior and upper margins of the 1st sacral vertebrae bulge forward (sacral
promontory).
The anterior and posterior surfaces of the sacrum posses on each side 4 foramina for the
passage of the anterior and posterior rami of the upper four sacral nerves.
The vertebral foramina together form the sacral canal.
The lamina of S5, and sometimes those of the 4th, fails to meet in the midline forming the
sacral hiatus.
The sacral canal contains the anterior and posterior roots of the lumbar, sacral, and
coccygeal spinal nerves, the filum terminale, and fibrofatty material. It also contains the
lower part of the subarachnoid space down as far as the lower border of S2.
The pelvic surface:
a. Central part formed by bodies of fused sacral vertebrae separated by transverse
ridges.
b. 4 pairs of anterior sacral foramina.
c. 2 lateral masses.
The dorsal surface:
a. Five sacral crests: median, 2 intermediate and 2 lateral.
b. 4 pairs of dorsal sacral foramina.
c. Inferiorly: 2 sacral cornua. One on each side of the hiatus for the articulation with
the coccygeal cornua.
The Coccyx
It consists of 4 vertebrae fused together to form a small triangular bone.
It articulates at its base with the sacrum.
The coccygeal vertebrae consist of bodies only, but the 1st vertebra possesses a rudimentary
transverse processes and cornua. The cornua project upward to articulate with the sacral
cornua.
Piriformis Muscle
Lateral rotator of the femur at the hip joint.
It is supplied by branches from the sacral plexus.
It arises from the front of the lateral masses of the sacrum.
It passes through the greater sciatic foramen to be inserted into the upper border of the
greater trochanter of the femur.
Ligaments of the pelvis
1. The sacroiliac ligaments: are extremely strong and pass directly anterior and posterior to
the sacroiliac joint. They bind the sacrum to the pelvis. The strong posterior and
interosseous sacroiliac ligaments suspend the sacrum between the two iliac bones. The
anterior sacroiliac ligament is thin and is anterior to the joint.
2. The iliolumbar ligaments: connect the transverse process of L5 to the iliac crest on each
side. Some inferior fibers of this ligament attach to the lateral margin of the sacrum and are
called as:
3. Lumbosacral ligament.
N.B. The iliolumbar and the Lumbosacral ligaments prevent the rotation of L5 on the
sacrum. They also help to prevent the gliding of L5 on the sacrum aided by the presence of
the articular processes between the sacrum and L5.
4. The pubic symphysis: note the superior and inferior pubic (symphyseal=arcuate)
ligaments.
5. The sacrotuberous ligament: it is strong and extends from the lateral part of the sacrum
and coccyx and the posterior inferior iliac spine to the ischial tuberosity.
6. The sacrospinous ligament: it is triangular in shape. It is attached by its base to the sacrum
and coccyx and by its apex to the spine of the ischium.
N.B. The weight of the trunk tends to thrust the upper end of the sacrum downward and rotate
the lower end of the bone upward. This movement is prevented by the sacrotuberous and
sacrospinous ligaments.
N.B. The sacrotuberous and sacrospinous ligaments help to form borders of the greater and
lesser sciatic foramina. The greater sciatic foramen is bounded by these ligaments and the
greater sciatic notch. Similarly, the lesser sciatic foramen is bounded by the lesser sciatic notch
and these 2 ligaments.
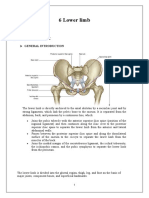
The Pelvis
The pelvis is divided into two compartments by the pelvic inlet (pelvic brim), which is
formed by:
a. Posteriorly: The sacral promontory.
b. Laterally: The iliopectineal line (arcuate line).
c. Anteriorly: The symphysis pubis.
Above the brim is the false pelvis. Below the brim is the true pelvis.
False pelvis
Boundaries:
Anteriorly: the lower part of the anterior abdominal wall.
Laterally: The iliac fossa and iliacus muscle.
Posteriorly: The lumbar vertebrae.
The false pelvis flares out superiorly and is considered part of the abdominal cavity.
True pelvis
It has:
1. Inlet (pelvic brim): forms ~55
o
angle with the horizontal plane.
2. Outlet: is bounded by:
a. Anteriorly: the pubic arch.
b. Laterally: the ischial tuberosities.
c. Posteriorly: the coccyx.
The pelvic outlet does not present a smooth outline but has 3 notches; the pubic arch and the
sciatic notches.
N.B. From an obstetric point of view the sacrotuberous ligaments are considered to form
part of the perimeter of the pelvic outlet. Thus, the outlet is diamond shaped with the
ischiopubic rami and the symphysis pubis in front, and the sacrotuberous ligaments and the
coccyx behind.
3. Cavity: short, curved canal between the inlet and the outlet. It has a shallow anterior wall
and a much deeper posterior wall.
Pelvic Measurements in Obstetrics
The pelvic axes:
Anatomic axis:
o It is an imaginary line joining the central points of the antero-posterior (AP)
diameters from the inlet to the outlet.
o It is C-shaped with the concavity directed forward.
Obstetric axis:
o It is an imaginary line represents the way passed by the head during labour.
o It is J-shaped that passes downward and backward along the axis of the inlet till the
ischial spines where it passes downward and forward along the axis of pelvic outlet.
True Pelvis Measurements
The Pelvic Inlet
Antero-posterior (AP) diameters:
Anatomical AP diameter (true conjugate) =11 cm.
From the tip of the sacral promontory to the upper border of the symphysis
pubis.
Transverse diameters:
Anatomical =13 cm.
It is the largest diameter in the pelvis.
It is between the outermost two points on the iliopectineal lines.
Oblique diameters (arcuate lines):
1. Right oblique =12 cm.
From the right sacroiliac joint to the left iliopectineal eminence.
2. Left oblique =12 cm.
From the right sacroiliac joint to the left iliopectineal eminence.
The Pelvic Outlet
Antero-posterior (AP) diameters:
Anatomical AP diameter =11 cm (9.5-11.5). Varies because of the mobility of the coccyx.
From the tip of the coccyx to the lower border of the symphysis pubis.
Transverse diameters:
1. Bituberous diameter = 11 cm
Between the inner aspects of the ischial tuberosities.
Usually estimated by the size of a closed fist.
2. Bispinous diameter = 10.5 cm
Between the tips of ischial spines.
Sex Differences of the Pelvis
They result from the adaptation of the female pelvis for childbearing.
The stronger muscles in the male are responsible for the thicker bones and more prominent
bony markings.
1. The false pelvis is shallow in females and deep in males.
2. The inlet is transversely oval in females but heart shape in males (because of the
promontory of sacrum).
3. The cavity in females is cylindrical (i.e. with parallel walls) with the distance
between the inlet and the outlet is shorter. In males, it is funnel-like with inwardly
slopping walls.
4. The pelvic outlet is larger in females than in males. The distance between the
ischial tuberosities is longer, the subpubic angle is wider, and the coccyx is more
mobile in females.
5. The ischial tuberosities are everted in females and turned in males.
6. The pubic tubercles are more widely separated in females than in males.
7. The sacrum is shorter, wider, and flatter in females than in males.
8. The greater sciatic notch is wider in females.
9. The sub pubic angle (pubic arch is wider in females):
In males: it is between 55
o
-58
o
(angle between the index and middle fingers).
In females: it is 80
o
-100
o
(angle between the thumb and the index finger).
Varieties of the Female Pelvis
In 1933, Caldwell and Moloy classified female pelves into 4 groups:
I. Gynecoid pelvis: is the typical female pelvis and present in ~40-50%.
II. Android pelvis: is the male or funnel-shaped pelvis with narrow outlet.
III. Platypelloid pelvis:
o The transverse diameters are much greater than the AP diameters (the promontory of
sacrum is pushed forward).
o Sub pubic angle is wide.
IV. Anthropoid pelvis:
o All the AP diameters are greater than the transverse diameters.
Two other varieties can be added to the above:
V. Contracted pelvis.
VI. Asymmetrical pelvis.
Pelvic Walls
Formed by bones and ligaments.
Partly lined with muscles covered with fascia and parietal peritoneum.
They are: anterior, posterior, lateral, and inferior pelvic walls.
Anterior pelvic wall
Formed by the posterior surfaces of the bodies of the pubic bones, the pubic rami, and the
symphysis pubis.
Posterior pelvic wall
Formed by the sacrum, coccyx, and the piriformis muscles and their coverings of parietal
pelvic fascia.
Lateral pelvic walls
Formed by:
a. Hip bone below the pelvic inlet.
b. Obturator membrane.
c. Sacrospinous and sacrotuberous ligaments.
d. Obturator internus muscle and its covering fascia.
Inferior pelvic wall (pelvic floor)
It stretches across the pelvis and divides it into the main pelvic cavity above and the
perineum below.
It is formed by the pelvic diaphragm.
Pelvic Diaphragm
o Formed by levator ani muscles, coccygeus muscles, and their covering fascia.
o It is incomplete anteriorly for the passage of the urethra (and vagina in females).
Levator Ani Muscle
I. Origin:
II.
o The line of origin extends from the pubis to ischial spines and includes a thickened
obturator fascia along the medial surface of the obturator
Internus (the arcus tendineus).
III. Insertion:
o Muscle fibers converge medially to their insertion. The line of insertion extends
from the pubis anteriorly to the coccyx posteriorly.
IV. Perforations:
o Anteriorly: urethral and vaginal orifices (the bulb of the penis in males).
o Posteriorly: the anal orifice.
o In between: the perineal body.
The anal orifice and the coccyx are joined by the thickened anococcygeal raphe.
V. Divisions:
Anterior fibers: 3 parts
1. (the levator prostate or sphincter vagina
Arises from the body of the pubis.
Forms a sling around the prostate or vagina.
Inserts into the perineal body.
Support the prostate (vagina) and stabilize the perineal body.
2. Puborectalis:
Arises from the body of the pubis.
Forms a sling around the junction of the rectum and anal canal
(anorectal junction) to end in the body of the pubis of the opposite
side.
This part is best seen from an outside (exterior) view.
Many fibers blend with the external anal sphincter (prerectal muscle
fibers of luschka)
3. Pubococcygeus:
1. From the body of the pubis and the tendineus arc.
2. Inserts into the anococcygeal body.
Posterior fibers (The iliococcygeus):
Arises from the arcus tendineus and the ischial spine.
Inserts in the coccyx and the anococcygeal body.
V. Actions of levator ani muscles:
A. Support and maintain pelvic viscera in position.
B. Resist the rise in the intrapelvic pressure during straining.
C. Sphincter action on the anorectal junction (vagina).
VI. Nerve Supply:
. Perineal branch of S4.
A. Perineal branch of the pudendal nerve.
Coccygeus Muscle
Small triangular muscle that makes up the lower part of the posterior pelvic wall just below
the piriformis.
It arises from the ischial spine.
Inserts into the lower end of the sacrum (S5) and into the coccyx.
It is the muscle that sways the tail in dogs (wagging the tail).
Nerve supply: a branch of the S4 and S5.
N.B. The piriformis muscle appears to "fill in" the gap between the posterior edge of the coccygeus
and the sacrum, but it is not a true pelvic floor muscle.
Pelvic Fascia
Formed of connective tissue.
Continuous above with the fascia lining the abdominal wall (fascia transversalis).
Continuous below with the fascia of the perineum.
It is divided into parietal and visceral layers:
Parietal layer
Lines the walls.
It is named according to the muscle it overlies, e.g. obturator internus fascia.
The coccygeus and levator ani fascia is the superficial layer of the pelvic fascia.
As the diaphragm becomes deficient anteriorly, it becomes continuous with (or as) the
superior fascia covering the superior surface of the pelvic diaphragm (i.e. in the perineum).
N.B. In many locations, where the parietal fascia comes into contact the bone it fuses with
the periosteum.
Below, in the perineum, it forms the superficial layer of the urogenital diaphragm.
Visceral layer
It is a layer of loose connective tissue.
It covers and supports all the pelvic viscera.
In certain locations, the fascia thickens to form fascial ligaments (e.g. ligaments of the
parametrium).
Pelvic peritoneum
The parietal peritoneum lines the pelvic walls.
It reflects onto the pelvic viscera where it becomes continuous with the visceral peritoneum.
It forms the pouch of Douglas and the vesicouterine pouches.
You might also like
- PelvisDocument35 pagesPelvisAdan ImanNo ratings yet
- Pelvic WallDocument56 pagesPelvic WallYousef El bannaNo ratings yet
- Pelvic Wall-Cont.: Dr:Ahmed Ibrahim Abdi (Nawawi) AnatomistDocument39 pagesPelvic Wall-Cont.: Dr:Ahmed Ibrahim Abdi (Nawawi) AnatomistSAKARIYE MAXAMEDNo ratings yet
- Anatomy of The Female Pelvis FinalDocument209 pagesAnatomy of The Female Pelvis FinalMignot Aniley86% (14)
- The Pelvis IDocument21 pagesThe Pelvis IFaith ChepoghishoNo ratings yet
- Joints of The Lower LimbDocument63 pagesJoints of The Lower LimbEliud MbuteNo ratings yet
- LowerLimbExam NurDocument108 pagesLowerLimbExam Nuralina nguynNo ratings yet
- Anatomy Research Paper PelvisDocument4 pagesAnatomy Research Paper PelvisBasil AdeelNo ratings yet
- Bones of The Pelvis: P. Akabondo Bsc. HB (Unza-Som)Document20 pagesBones of The Pelvis: P. Akabondo Bsc. HB (Unza-Som)Elias KangwaNo ratings yet
- The Female Pelvis: Namasinga JoyceDocument79 pagesThe Female Pelvis: Namasinga JoyceNamaganda NajjatiNo ratings yet
- Subjects: - Introduction - Pelvic Girdle - Pelvic CavityDocument39 pagesSubjects: - Introduction - Pelvic Girdle - Pelvic CavityAshraf SidrahNo ratings yet
- Anatomy of The PelvisDocument149 pagesAnatomy of The PelvisObongsamuel IdiongNo ratings yet
- GRDA Intro Bony PelvisDocument5 pagesGRDA Intro Bony PelvisKingNo ratings yet
- Anatomy of The Female PelvisDocument60 pagesAnatomy of The Female PelvisMignot AnileyNo ratings yet
- 1-25 LLDocument25 pages1-25 LLJames WesNo ratings yet
- Obg Lab ModuleDocument217 pagesObg Lab Moduleaiswarya ppNo ratings yet
- Gross Anatomy Ii (ANAT 104) : Osteology of The Pelvis and Its JointsDocument33 pagesGross Anatomy Ii (ANAT 104) : Osteology of The Pelvis and Its Jointsmirabel mac-peppleNo ratings yet
- Pelvis: The Pelvis/Bony Gridle/Pelvic GridleDocument18 pagesPelvis: The Pelvis/Bony Gridle/Pelvic GridlepreezaNo ratings yet
- Anatomy of The PelvisDocument6 pagesAnatomy of The Pelvisapi-195986134No ratings yet
- Lower LimbpostgDocument79 pagesLower LimbpostgBuya kasahunNo ratings yet
- Gross Anatomy of The Pelvis & Perineum DR Ogedengbe O.ODocument162 pagesGross Anatomy of The Pelvis & Perineum DR Ogedengbe O.OKolawole Adesina KehindeNo ratings yet
- CH 2 Female PelvisDocument80 pagesCH 2 Female PelvisamixnomyNo ratings yet
- ANATOMY I 25.03.20 I Pelvic Girdle, Thigh Bones, Hip JointsDocument34 pagesANATOMY I 25.03.20 I Pelvic Girdle, Thigh Bones, Hip JointsArianna RomanoNo ratings yet
- The Pelvis: By: Raja Basil ADEEL (Ug Code:2103110)Document20 pagesThe Pelvis: By: Raja Basil ADEEL (Ug Code:2103110)Basil AdeelNo ratings yet
- Worku Antomy and Physiology of Reproductive OrganDocument206 pagesWorku Antomy and Physiology of Reproductive OrganMignot AnileyNo ratings yet
- Pedicles Are Short Projections, From The Superior Part of The Vertebral Body To TheDocument3 pagesPedicles Are Short Projections, From The Superior Part of The Vertebral Body To ThebarbacumlaudeNo ratings yet
- Gluteal RegionDocument66 pagesGluteal Regionashley nicholeNo ratings yet
- Lecture 8Document99 pagesLecture 8bolivarsefNo ratings yet
- Pelvis, NOTEDocument358 pagesPelvis, NOTELidiya TeshomeNo ratings yet
- Anatomy of Lower LimbDocument20 pagesAnatomy of Lower LimbDr.Ammar MasoodNo ratings yet
- Maternal Pelvis Fetal Skull PDFDocument13 pagesMaternal Pelvis Fetal Skull PDFAnuradha Maurya100% (2)
- Joints of Lower LimbsDocument12 pagesJoints of Lower LimbsMohammed SheikhNo ratings yet
- 1 Introduction To The Pelvis and The Pelvic Peritoneum DIYADocument38 pages1 Introduction To The Pelvis and The Pelvic Peritoneum DIYAOmotosho DavidNo ratings yet
- Anatomy of Hip and Knee Joint and Popliteal Fossa: Prof. Dr. Nabil KhourDocument49 pagesAnatomy of Hip and Knee Joint and Popliteal Fossa: Prof. Dr. Nabil KhourBadria Al-najiNo ratings yet
- Inguinal Canal and ScrotumDocument55 pagesInguinal Canal and ScrotumAuza Moses IbrahimNo ratings yet
- Anatomy of Knee JointDocument17 pagesAnatomy of Knee JointSiti AisyahNo ratings yet
- Vertebral ColumnDocument64 pagesVertebral ColumnJavin BissoondyalNo ratings yet
- Lower Limb BONESDocument79 pagesLower Limb BONESDr.Kumar Satish Ravi100% (1)
- ANATOMY PELVIS PRESENTATION - CompressedDocument20 pagesANATOMY PELVIS PRESENTATION - CompressedBasil AdeelNo ratings yet
- 9. المحاضرة التاسعة - مادة التشريح العام - المرحلة الاولىDocument6 pages9. المحاضرة التاسعة - مادة التشريح العام - المرحلة الاولىAbdullah TheNo ratings yet
- The Back: Cortez Gomez Lucas VillafuerteDocument53 pagesThe Back: Cortez Gomez Lucas VillafuerteFlorenze Laiza Donor LucasNo ratings yet
- Knee JointDocument49 pagesKnee JointRiaz SialNo ratings yet
- 7pelvic CavityDocument71 pages7pelvic CavityDan MupenziNo ratings yet
- ANA212 - Oesteology of Lower Limbs 2020Document52 pagesANA212 - Oesteology of Lower Limbs 2020osunmuyiwaaNo ratings yet
- Chapter 10 - The Lower Limb: Snell 9 EdDocument138 pagesChapter 10 - The Lower Limb: Snell 9 EdFerjie Angelica DalandaoNo ratings yet
- 6 Lower LimbDocument19 pages6 Lower LimbMOHAMMED BIN BAREKNo ratings yet
- Pdfs/residency/anatomy/ Normal-Anatomy-And-Physiology-Of-The-Female-PelvisDocument34 pagesPdfs/residency/anatomy/ Normal-Anatomy-And-Physiology-Of-The-Female-PelvisMohamed FarahatNo ratings yet
- Review of Anatomy and Physiology of Human ReproductiveDocument68 pagesReview of Anatomy and Physiology of Human Reproductivesavita hanamsagarNo ratings yet
- 1 Lower Limb BONESDocument79 pages1 Lower Limb BONESZaid AbdulqadirNo ratings yet
- Bones of Lower LimbsDocument11 pagesBones of Lower Limbsbasitali khanNo ratings yet
- Seminar On Female Pelvis and Pelvic FloorDocument11 pagesSeminar On Female Pelvis and Pelvic FloorJasmin SabnaNo ratings yet
- Bony Pelvis and Pelvic FloorDocument73 pagesBony Pelvis and Pelvic Floormamai elijahNo ratings yet
- Skeletal System Notes 2023Document16 pagesSkeletal System Notes 2023shinamaejNo ratings yet
- Knee Joint and Popliteal FossaDocument71 pagesKnee Joint and Popliteal FossaEsdras DountioNo ratings yet
- Anatomy 1Document17 pagesAnatomy 1Uljana NasonovaNo ratings yet
- HindlimbDocument60 pagesHindlimbsaikotbau56121No ratings yet
- The Pelvis IiDocument25 pagesThe Pelvis IiFaith ChepoghishoNo ratings yet
- The Influence of Bones and Muscles on FormFrom EverandThe Influence of Bones and Muscles on FormRating: 5 out of 5 stars5/5 (3)