Professional Documents
Culture Documents
MitochondrialDz X PDF
Uploaded by
Mircea MoldovanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MitochondrialDz X PDF
Uploaded by
Mircea MoldovanCopyright:
Available Formats
The Physician's Guide to Laboratory Test Selection and Interpretation
Mitochondrial Diseases
Diagnosis
Indications for Testing Children with multiple complex neurologic symptoms or a single neurological symptom with other system involvement Children presenting with lactic acidosis Individuals with clinical symptoms characteristic of a specific mitochondrial disorder Individuals with any progressive multisystem disorder of unknown etiology Asymptomatic, at-risk family members Family history assess inheritance pattern to help direct molecular testing Laboratory Testing Metabolic evaluation generally precedes molecular genetic testing unless a specific disorder is suspected Serum Chemistry panel Liver function studies Pyruvate concentration/lactate Ammonia Creatinine kinase (MM) rarely elevated Plasma acylcarnitine Ketone Fasting glucose Amino acids Coenzyme Q deficient isolated myopathy, cerebellar ataxia, encephalomyopathy, Leigh syndrome Urine Urinalysis Organic acids Amino acids Cerebrospinal fluid Routine studies Lactate acid/pyruvate concentration Amino acids Molecular genetic testing Molecular testing for mtDNA mutations may require testing be performed on DNA extracted from skeletal muscle; nuclear gene mutations and some mtDNA mutations can be detected in DNA from peripheral blood Mitochondrial genome mutation scanning/sequencing Mitochondrial genome duplication/deletion testing DNA testing for nuclear genes associated with mitochondrial disorders Targeted testing for a family-specific mutation in at-risk or symptomatic family members For classic syndrome presentation, genetic testing may be initial testing of choice Imaging Studies CT often normal May demonstrate punctate calcifications May see edema or atrophy (cerebral or cerebellar)
ARUP LABORATORIES | 500 Chipeta Way | Salt Lake City, Utah 84108-1221 | (800) 522-2787 | www.arupconsult.com | www.aruplab.com
20062012 ARUP Laboratories. All Rights Reserved. Mitochondrial Diseases - p. 1 of 9
The Physician's Guide to Laboratory Test Selection and Interpretation
MRI T2 signal that resembles stroke-like lesions Abnormal myelination Other Testing Biochemistry Analysis of electron transport chain activity ATP synthesis measures in fibroblasts Coenzyme Q Biochemical results may suggest genetic testing Complex I deficiency analysis of mitochondrial DNA and nuclear encoded genes Complex II deficiency analysis of SDHA, SDHB, CDHC, SDHD Complex III deficiency analysis of MTCYB, 10 nuclear structural genes, BCS1L Complex IV deficiency analysis of mitochondrial DNA cytochrome coxidase assembly factors (SURF1, SCO1, SCO2, COX10, COX15) Multiple complex deficiencies analysis of mitochondrial DNA and nuclear DNA mitochondrial maintenance and translation genes Coenzyme Q deficiency analysis of CABC1, COQ2, COQ9, PDSS1, PDSS2, ETFDH, APTX Muscle biopsy Light microscopy histochemistry Detection of ragged red fibers (most common in mitochondrial mutations) by Gomori trichrome stains Subsarcolemmal accumulation of mitochondria on muscle pathology Cytochrome coxidase-deficient fibers Electron microscopy Increase in mitochondrial number or size, increased lipid and glycogen droplets, increased mitochondrial matrix Can also perform liver, cardiac, or skin biopsy Neurophysiologic studies Electroencephalography for individuals with suspected encephalopathy or seizures Electromyography/nerve conduction velocity for individuals with limb weakness, sensory issues, or areflexia Electrocardiography/echocardiography Evaluate cardiomyopathy or atrioventricular conduction defects Auditory/ophthalmologic examinations to confirm defects Differential Diagnosis Neurological Children/infants Metabolic diseases Hypothyroidism Muscular dystrophy Developmental delay Lysosomal storage diseases Adults Wilson disease Multiple sclerosis
ARUP LABORATORIES | 500 Chipeta Way | Salt Lake City, Utah 84108-1221 | (800) 522-2787 | www.arupconsult.com | www.aruplab.com
20062012 ARUP Laboratories. All Rights Reserved. Mitochondrial Diseases - p. 2 of 9
The Physician's Guide to Laboratory Test Selection and Interpretation
Coenzyme Q disease Dementia Migraine disorder Parkinson disease Sarcoidosis Vasculidities Connective tissue diseases Infectious fungal, viral Chronic demyelinating disease Paraneoplastic syndrome Stroke Seizure disorder Endocrinological Diabetes mellitus Thyroid disease (hypo/hyper) Autoimmune adrenal disease Hepatic disease Reye syndrome Wilson disease Acute hepatitis B or C Myopathy Dermatomyositis Chronic demyelinating inflammatory polyneuropathy Paraneoplastic syndrome Guillain-Barr syndrome Lactic acidosis Sepsis Polymyositis Inborn errors of metabolism
Clinical Background
Mitochondrial diseases are a group of disorders originating from mutations in nuclear DNA or mitochondrial DNA (mtDNA) and resulting in a wide spectrum of pathological conditions, often with significant neurologic and myelopathic symptoms. Many commonly seen conditions can be classified as discrete clinical syndromes; however, the presentation and severity of the conditions may vary, creating challenges in diagnosis and treatment. Epidemiology Prevalence approximately 1/8,500 Age all ages Sex M:F, equal Inheritance Mitochondrial disorders may be caused by mutations in nuclear DNA or mtDNA Nuclear gene defects may be inherited in an autosomal recessive or autosomal dominant manner mtDNA defects are maternally transmitted mtDNA deletions generally occur de novo mtDNA point mutations and duplications are maternally inherited
ARUP LABORATORIES | 500 Chipeta Way | Salt Lake City, Utah 84108-1221 | (800) 522-2787 | www.arupconsult.com | www.aruplab.com
20062012 ARUP Laboratories. All Rights Reserved. Mitochondrial Diseases - p. 3 of 9
The Physician's Guide to Laboratory Test Selection and Interpretation
Affected individuals with mtDNA mutations often have a mixture of mutated and normal mtDNA within each cell (heteroplasmy) Disease severity and the age of onset are affected by the amount of heteroplasmy and the number and type of cells containing the mtDNA mutation Females with heteroplasmy but no clinical symptoms may have affected offspring Poor genotype/phenotype correlation exists; the same mutation may cause different clinical syndromes Pathophysiology Mitochondria are ubiquitous, complex, intracellular organelles containing non-nuclear DNA Each cell may contain hundreds to thousands of copies of mtDNA Mitochondria are essential in many cell processes, including the generation of adenosine triphosphate during oxidative metabolism Mutations in the mitochondrial genome or in nuclear DNA involved in the respiratory chain principally affect tissues that are heavily dependent on oxidative metabolism (eg, central nervous system, cardiovascular, musculoskeletal) Clinical Presentation Many mitochondrial diseases can be classified as a discrete clinical syndrome based on characteristic clinical features; however, clinical overlap occurs Some mitochondrial disorders only affect a single organ, such as in Leber hereditary optic neuropathy (LHON) and nonsyndromic sensorineural deafness Mitochondrial disorders may present at any age Presentation of nuclear DNA mutations typically occurs in childhood; mtDNA abnormalities are more likely to present in late childhood or adulthood Clinical presentation is highly variable Features of mitochondrial DNA-associated diseases Features of Mitochondrial DNA-Associated Diseases Children Cardiac biventricular hypertrophic cardiomyopathy, rhythm abnormalities, cardiac murmur, sudden death Dermatological erythema, lipomatosis, reticular pigmentation, hypertrichosis, vitiligo, alopecia Endocrine diabetes mellitus, adrenal failure, growth failure, hypothyroidism, hypogonadism, hypoparathyroidism Gastrointestinal vomiting, failure to thrive, dysphagia, GI motility problems, vomiting, pseudoobstruction Hematological anemia, pancytopenia Hepatic hepatic failure (very sensitive to valproate) Musculoskeletal weakness, myopathy Neurological myopathy (proximal > distal, upper extremities > lower), developmental delay, ataxia, spasticity, dystonia, hypotonia, bulbar signs, chorea, seizures, myoclonus, stroke Ophthalmological optic atrophy, retinitis pigmentosa, ptosis, diplopia, cataract Otological sensorineural deafness Renal renal tubular defects (proximal defect renal tubular acidosis most common), nephrotic syndrome, tubulointerstitial nephritis Respiratory central hypoventilation, apnea Adults Cardiac heart failure, conduction block, cardiomyopathy, sudden death Endocrine diabetes, thyroid disease, parathyroid disease Gastrointestinal constipation, irritable bowel syndrome, dysphagia, anorexia, abdominal pain, diarrhea Musculoskeletal rhabdomyolysis, muscle weakness, exercise intolerance
ARUP LABORATORIES | 500 Chipeta Way | Salt Lake City, Utah 84108-1221 | (800) 522-2787 | www.arupconsult.com | www.aruplab.com
20062012 ARUP Laboratories. All Rights Reserved. Mitochondrial Diseases - p. 4 of 9
The Physician's Guide to Laboratory Test Selection and Interpretation
Neurological migraine, stroke, seizures, dementia, myopathy, peripheral neuropathy, ataxia, speech disturbances, bulbar signs, myoclonus, tremor Ophthalmological optic atrophy, cataracts, progressive external ophthalmoplegia, ptosis, pigmentary retinopathy, vision loss, diplopia Otological sensorineural deafness Reproductive pregnancy loss in mid to late gestation, hypogonadism Respiratory respiratory failure, nocturnal hypoventilation, recurrent aspiration, pneumonia Examples of inherited mitochondrial disorders caused by nuclear DNA mutations Autosomal recessive external ophthalmoplegia Hypertrophic cardiomyopathy Myoneurogastrointestinal encephalomyopathy Leigh syndrome Mitochondrial depletion syndrome Dominant optic atrophy Examples of inherited disorders caused by mtDNA mutations Mitochondrial encephalomyopathy, lactic acidosis, and strokelike episodes (MELAS) Myoclonic epilepsy associated with ragged red fibers (MERRF) Neuropathy, ataxia, retinitis pigmentosa/maternally inherited Leigh syndrome Leber hereditary optic neuropathy (LHON) Chronic progressive external ophthalmoplegia Maternally inherited diabetes and deafness Non-syndromic maternally inherited deafness Examples of typically sporadic disorders caused by mtDNA deletions (can be maternally transmitted) Kearns-Sayre syndrome (KSS) Pearson syndrome Presence of substantial intellectual disability or significant dysmorphic features should steer testing toward other disorders
Lab Tests
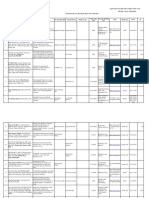
Indications for Laboratory Testing Tests generally appear in the order most useful for common clinical situations. For test-specific information, refer to the test number in the ARUP Laboratory Test Directory on the ARUP Web site at www.aruplab.com. Test Name and Number Mitochondrial Disorders Panel (mtDNA and 108 Nuclear Genes) Sequencing and Deletion/Duplication 2006054 Method: Massive Parallel Sequencing Recommended Use Diagnose mitochondrial disorders caused by mutations within the mitochondrial genome and nuclear genes Limitations Diagnosis of mitochondrial disorders may be tissue specific Nuclear DNA mutations and large deletions/duplications within the mitochondrial genome will not be detected Heteroplasmy levels of <10% will not be detected Follow Up
ARUP LABORATORIES | 500 Chipeta Way | Salt Lake City, Utah 84108-1221 | (800) 522-2787 | www.arupconsult.com | www.aruplab.com
20062012 ARUP Laboratories. All Rights Reserved. Mitochondrial Diseases - p. 5 of 9
The Physician's Guide to Laboratory Test Selection and Interpretation
Mitochondrial Disorders (mtDNA) Sequencing 2006065 Method: Massive Parallel Sequencing
Diagnose mtDNA disorders caused by mutations within the mitochondrial genome
Large deletions/duplications within the mitochondrial genome and nuclear genes will not be detected Heteroplasmy levels of <15% will not be detected Mutation within the nuclear genes will not be detected Large deletions/duplications within the mitochondrial genome and nuclear genes will not be detected Mutation within the mitochondrial genome will not be detected Heteroplasmy levels of <15% will not be detected Point mutation within the mitochondrial genome and nuclear genes will not be detected
Mitochondrial Disorders (108 Nuclear Genes) Sequencing 2006050 Method: Massive Parallel Sequencing Mitochondrial Genome (mtDNA and 108 Nuclear Genes) Deletion/Duplication 2006061
Diagnose mitochondrial disorders caused by mutations within nuclear genes
Diagnose mitochondrial disorders caused by deletions and duplications within the mitochondrial genome and nuclear genes
Method: Exonic Oligonucleotide-based CGH Microarray Ketones, Serum or Plasma Rule out other metabolic disorders 0020034 Method: Visual Identification Lactic Acid, Plasma 0020045 Method: Enzymatic Lactic Acid, CSF 0020516 Method: Enzymatic Pyruvic Acid 0080310 Method: Quantitative Enzymatic
Results may be suggestive of mitochondrial disorders individually or when combined with pyruvic acid Rule out other metabolic disorders
Results may be suggestive of mitochondrial disorders individually or when combined with plasma lactic acid
ARUP LABORATORIES | 500 Chipeta Way | Salt Lake City, Utah 84108-1221 | (800) 522-2787 | www.arupconsult.com | www.aruplab.com
20062012 ARUP Laboratories. All Rights Reserved. Mitochondrial Diseases - p. 6 of 9
The Physician's Guide to Laboratory Test Selection and Interpretation
Carnitine Panel 0081110 Method: Tandem Mass Spectrometry Organic Acids, Urine 0098389 Method: Gas Chromatography/Mass Spectrometry Amino Acids Quantitative, Plasma 0080710 Method: Ion Exchange Chromatography Amino Acids Quantitative, Urine 0080044 Method: Ion Exchange Chromatography Acylcarnitine Quantitative Profile, Plasma 0040033
Rule out other metabolic disorders
Rule out other metabolic disorders
Rule out other metabolic disorders
Rule out other metabolic disorders
Rule out other metabolic disorders
Method: Tandem Mass Spectrometry Glucose, Plasma or Serum Rule out other metabolic disorders 0020024 Method: Quantitative Enzymatic Additional Tests Available Test Name and Number Urinalysis, Complete 0020350 Method: Reflectance Spectrophotometry/Microscopy Mitochondrial Disorders (108 Nuclear Genes) Sequencing and Deletion/Duplication 2006878 Method: Massive Parallel Sequencing/Exonic Oligonucleotide-based CGH Microarray Comments
ARUP LABORATORIES | 500 Chipeta Way | Salt Lake City, Utah 84108-1221 | (800) 522-2787 | www.arupconsult.com | www.aruplab.com
20062012 ARUP Laboratories. All Rights Reserved. Mitochondrial Diseases - p. 7 of 9
The Physician's Guide to Laboratory Test Selection and Interpretation
Mitochondrial Disorders (mtDNA) Sequencing and Deletion/Duplication 2006872 Method: Massive Parallel Sequencing/Exonic Oligonucleotide-based CGH Microarray Guidelines Finsterer J, Harbo HF, Baets J, Van Broeckhoven C, Di Donato S, Fontaine B, De Jonghe P, Lossos A, Lynch T, Mariotti C, Schols L, Spinazzola A, Szolnoki Z, Tabrizi SJ, Tallaksen CM, Zeviani M, Burgunder JM, Gasser T. EFNS guidelines on the molecular diagnosis of mitochondrial disorders.Eur J Neurol. 2009; 16 (12) :1255-1264.
General References Craigen WJ. Mitochondrial DNA mutations: an overview of clinical and molecular aspects.Methods Mol Biol. 2012; 837 :3-15. Haas RH, Parikh S, Falk MJ, Saneto RP, Wolf NI, Darin N, Cohen BH. Mitochondrial disease: a practical approach for primary care physicians.Pediatrics. 2007; 120 (6) :1326-1333. Kisler JE, Whittaker RG, McFarland R. Mitochondrial diseases in childhood: a clinical approach to investigation and management.Dev Med Child Neurol. 2010; 52 (5) :422-433. Koenig MK. Presentation and diagnosis of mitochondrial disorders in children.Pediatr Neurol. 2008; 38 (5) :305-313. Mancuso M, Orsucci D, Coppede F, Nesti C, Choub A, Siciliano G. Diagnostic approach to mitochondrial disorders: the need for a reliable biomarker.Curr Mol Med. 2009; 9 (9) :1095-1107. McFarland R, Taylor RW, Turnbull DM. A neurological perspective on mitochondrial disease.Lancet Neurol. 2010; 9 (8) :829-840. Rahman S, Hanna MG. Diagnosis and therapy in neuromuscular disorders: diagnosis and new treatments in mitochondrial diseases.J Neurol Neurosurg Psychiatry. 2009; 80 (9) :943-953. Scaglia F. Nuclear gene defects in mitochondrial disorders.Methods Mol Biol. 2012; 837 :17-34. Siciliano G, Pasquali L, Mancuso M, Murri L. Molecular diagnostics and mitochondrial dysfunction: a future perspective.Expert Rev Mol Diagn. 2008; 8 (4) :531-549. Tuppen HA, Blakely EL, Turnbull DM, Taylor RW. Mitochondrial DNA mutations and human disease.Biochim Biophys Acta. 2010; 1797 (2) :113-128. References from the ARUP Institute for Clinical and Experimental Pathology Dimmock DP, Zhang Q, onisi-Vici C, Carrozzo R, Shieh J, Tang LY, Truong C, Schmitt E, Sifry-Platt M, Lucioli S, Santorelli FM, Ficicioglu CH, Rodriguez M, Wierenga K, Enns GM, Longo N, Lipson MH, Vallance H, Craigen WJ, Scaglia F, Wong LJ. Clinical and molecular features of mitochondrial DNA depletion due to mutations in deoxyguanosine kinase.Hum Mutat. 2008; 29 (2) :330-331. Dobrowolski SF, Hendrickx AT, van den Bosch BJ, Smeets HJ, Gray J, Miller T, Sears M. Identifying sequence variants in the human mitochondrial genome using high-resolution melt (HRM) profiling.Hum Mutat. 2009; 30 (6) :891-898. Longo N, Schrijver I, Vogel H, Pique LM, Cowan TM, Pasquali M, Steinberg GK, Hedlund GL, Ernst SL, Gallagher RC, Enns GM. Progressive cerebral vascular degeneration with mitochondrial encephalopathy.Am J Med Genet A. 2008; 146 (3) :361-367.
ARUP LABORATORIES | 500 Chipeta Way | Salt Lake City, Utah 84108-1221 | (800) 522-2787 | www.arupconsult.com | www.aruplab.com
20062012 ARUP Laboratories. All Rights Reserved. Mitochondrial Diseases - p. 8 of 9
The Physician's Guide to Laboratory Test Selection and Interpretation
Reviewed by Krautscheid, Patti, MS, LCGC. Genetic Counselor, Molecular Genetics and Special Genetics Laboratories at ARUP Laboratories Longo, Nicola, MD, PhD. Medical Co-Director, Biochemical Genetics at ARUP Laboratories; Professor, Pediatrics and Pathology (Adjunct), University of Utah Mao, Rong, MD. Medical Director, Molecular Genetics, Fragment Analysis and Sequencing at ARUP Laboratories; Assistant Professor of Pathology (Clinical), University of Utah Miller, Christine E., MS, LCGC. Genetic Counselor, Molecular Genetics Laboratory at ARUP Laboratories; Faculty, Graduate Program in Genetic Counseling, University of Utah Pasquali, Marzia, PhD. Medical Director, Newborn Screening Laboratory and Biochemical Genetics Laboratory at ARUP Laboratories; Professor of Pathology (Clinical), University of Utah Related Content Autoimmune Inner Ear Disease Developmental Delay (DD) or Intellectual Disability (ID) Testing - Neurocognitive Impairments N-methyl-D-Aspartate (NMDA) type Glutamate Receptor Autoantibody Disorders - Anti-NMDA-Receptor Encephalitis Seizure Disorders - Epilepsy
Last Update: August 2012
ARUP LABORATORIES | 500 Chipeta Way | Salt Lake City, Utah 84108-1221 | (800) 522-2787 | www.arupconsult.com | www.aruplab.com
20062012 ARUP Laboratories. All Rights Reserved. Mitochondrial Diseases - p. 9 of 9
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Fischer Technical Manual PDFDocument94 pagesFischer Technical Manual PDFMircea Moldovan100% (1)
- Kettlebell Fusion WorkoutDocument2 pagesKettlebell Fusion WorkoutMircea MoldovanNo ratings yet
- FitnessfitnessDocument136 pagesFitnessfitnessSimran MehataNo ratings yet
- BMIDocument2 pagesBMISabita PersaudNo ratings yet
- CBR600RR 2007Document162 pagesCBR600RR 2007Mircea MoldovanNo ratings yet
- Antrenament MatrixDocument1 pageAntrenament MatrixMircea MoldovanNo ratings yet
- The Naked Warrior PDFDocument218 pagesThe Naked Warrior PDFAurel100% (2)
- Principles of Functional ExerciseDocument290 pagesPrinciples of Functional ExercisePedro ManéNo ratings yet
- Caml I GuneyDocument5 pagesCaml I GuneyMircea MoldovanNo ratings yet
- Program Standard IncepatoriDocument2 pagesProgram Standard IncepatoriMircea MoldovanNo ratings yet
- Weekly Meal Planner: Monday Friday Grocery ListDocument1 pageWeekly Meal Planner: Monday Friday Grocery ListMircea MoldovanNo ratings yet
- Keiser Performance Cycling ManualDocument46 pagesKeiser Performance Cycling ManualMircea MoldovanNo ratings yet
- Dietary Guidelines For Americans - 2010Document112 pagesDietary Guidelines For Americans - 2010scribd993No ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Out - 213 - Cil - To - Artefact Extension of Time ApplicationDocument25 pagesOut - 213 - Cil - To - Artefact Extension of Time Applicationkrishna murariNo ratings yet
- Lipid Metabolism - 3rd LectureDocument38 pagesLipid Metabolism - 3rd LectureLe Uyen Nguyen100% (1)
- Corneal Epithelial Proliferation and Thickness in A Mouse Model of Dry EyeDocument7 pagesCorneal Epithelial Proliferation and Thickness in A Mouse Model of Dry EyeAa 1989No ratings yet
- Blood Lecture SlidesDocument144 pagesBlood Lecture Slidesgrace ncubeNo ratings yet
- NT Biology Answers Chapter 16Document8 pagesNT Biology Answers Chapter 16ASADNo ratings yet
- Flashcards For Neet Biology 12 Biotechnology Principles and Processes PDFDocument5 pagesFlashcards For Neet Biology 12 Biotechnology Principles and Processes PDFDeepikaNo ratings yet
- Plowman - 1984 - The Ethnobotany of CocaDocument49 pagesPlowman - 1984 - The Ethnobotany of CocaLuis Flores BlancoNo ratings yet
- HL BIO IB Extended EssayDocument39 pagesHL BIO IB Extended EssayRachel Tan Hui MinNo ratings yet
- How To Increase Dopamine The Motivation MoleculeDocument6 pagesHow To Increase Dopamine The Motivation MoleculeTarik Alic100% (1)
- Pro Clot PCDocument3 pagesPro Clot PCSmithesh TpNo ratings yet
- RBSC2013 Abstract BookDocument138 pagesRBSC2013 Abstract BookPETIENo ratings yet
- Weber Health Assessment in NursingDocument22 pagesWeber Health Assessment in NursingAaron WallaceNo ratings yet
- Causes of Mental IllnessDocument18 pagesCauses of Mental IllnessMonika Joseph0% (1)
- Medical Microbiology Made MemorableDocument113 pagesMedical Microbiology Made MemorableParna Praveen90% (10)
- Agricultural Biotechnology: Ars Main Exam-2012 Memory Based Paper Developed By: Ifas, B-7 Saraswati Nagar, JodhpurDocument3 pagesAgricultural Biotechnology: Ars Main Exam-2012 Memory Based Paper Developed By: Ifas, B-7 Saraswati Nagar, JodhpurDipankar RoyNo ratings yet
- AllergyDocument528 pagesAllergyCristina Ene100% (1)
- Hemostasis, Surgical Bleeding and TransfusionDocument10 pagesHemostasis, Surgical Bleeding and TransfusionCarl Earvin L. FavoritoNo ratings yet
- Early Pregnancy Loss in Emergency MedicineDocument14 pagesEarly Pregnancy Loss in Emergency MedicineMuhammad RezaNo ratings yet
- PRO102 CHARACTERISTICS AND OUTCOMES OF PEDIATRIC HEMOPHILIA A - 2020 - Value inDocument2 pagesPRO102 CHARACTERISTICS AND OUTCOMES OF PEDIATRIC HEMOPHILIA A - 2020 - Value inMichael John AguilarNo ratings yet
- Protein Expression HandbookDocument118 pagesProtein Expression HandbookLuis Arístides Torres SánchezNo ratings yet
- Vpa 25Document11 pagesVpa 25Ada CelisNo ratings yet
- Detection of Sars-Cov-2 Omicron Variant (B.1.1.529) Infection of White-Tailed DeerDocument19 pagesDetection of Sars-Cov-2 Omicron Variant (B.1.1.529) Infection of White-Tailed DeerNational Content DeskNo ratings yet
- Liver Function Tests InterpretationDocument2 pagesLiver Function Tests InterpretationdarrenkongNo ratings yet
- Danh Sach Bai Bao Quoc Te 2020 794Document14 pagesDanh Sach Bai Bao Quoc Te 2020 794Master DrNo ratings yet
- MS ENT Basic Sciences MGR University September 2009 Question Paper With SolutionDocument36 pagesMS ENT Basic Sciences MGR University September 2009 Question Paper With SolutionDr. T. Balasubramanian67% (3)
- Annotated BibliographyDocument10 pagesAnnotated Bibliographyapi-273829037No ratings yet
- Biodiversity, Bioprospecting, Traditional Knowledge, Sustainable Development and Value Added Products: A ReviewDocument8 pagesBiodiversity, Bioprospecting, Traditional Knowledge, Sustainable Development and Value Added Products: A Review075. Hortensa MukudjeyNo ratings yet
- Mangifera IndicaDocument3 pagesMangifera IndicaRajesh KumarNo ratings yet
- Mma DataDocument30 pagesMma DataPau ZalazarNo ratings yet
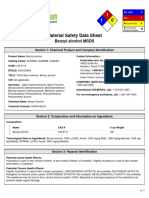
- Benzyl Alcohol (Corrosive)Document6 pagesBenzyl Alcohol (Corrosive)Yojana SonawaneNo ratings yet