Professional Documents
Culture Documents
DD Iicc AA: Sepsis Diagnosis and Management: Work in Progress
Uploaded by
IecHa RizkaMaulidaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
DD Iicc AA: Sepsis Diagnosis and Management: Work in Progress
Uploaded by
IecHa RizkaMaulidaCopyright:
Available Formats
CASI CLINICI
MINERVA ANESTESIOL 2006;72:87-96
M IN CO E R PY V A RI M GH E D T IC
Severe sepsis is a common disease process in the critically ill and is associated with substantial morbidity and mortality. Continuing research has provided considerable insight into the pathophysiology of sepsis over recent years, enabling various aspects of the sepsis response to be targeted. Discoveries related to the link between coagulation and inflammation have been particularly exciting, leading to the development of recombinant activated protein C. This review will discuss current definitions of sepsis, describe new approaches to classification and diagnosis of patients with sepsis, present recommendations for management, and briefly highlight areas of ongoing and future research. Key words: Sepsis, diagnosis - Sepsis, therapy Intensive care.
Sepsis diagnosis and management: work in progress
J. L. VINCENT, A. M. HABIB, C. VERDANT, A. BRUHN
Deparment of Intensive Care, Erasme Hospital Free University of Brussels, Brussels, Belgium
Definitions of sepsis
Sepsis vs infection
ecent years have seen great advances in our understanding of the pathophysiology of sepsis and as a result new treatments have become available and more are being developed. In addition, progress has been made in techniques to facilitate the diagnosis of sepsis. In this article we will discuss the recent advances in the diagnosis and management of this important and common problem.
Address reprint requests to: Prof J. L. Vincent, Erasme Hospital, Route de Lennik 808, 1070 Brussels, Belgium. E-mail: jlvincen@ulb.ac.be
The words sepsis and infection are often used as synonyms, but they are distinct entities. Infection is a microbiological event, caused by bacteria, fungi, viruses etc., while sepsis is the host response to that infection, characterized by the release of many mediators and by a constellation of clinical and laboratory features (Table I), none of which are specific for sepsis. Whenever possible, infection should be defined by the organ primarily infected and the type(s) of microorganisms (e.g., a lung infection due to Pneumococcus or a urinary tract infection due to E. coli). While the presence of infection is essential for a diagnosis of sepsis, sometimes the source of infection cannot be identified, and sometimes the bacteriology remains negative. In some patients with sepsis, the causative infection may never be identified at all; this does not mean the patient does not have an infection, and hence cannot have sepsis, just that we are unable to locate or identify it. To help to rule out an infection, an objective measure such as the
A
Vol. 72, N. 3 MINERVA ANESTESIOLOGICA
87
VINCENT
SEPSIS DIAGNOSIS AND MANAGEMENT
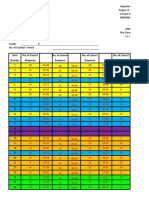
TABLE I.Common clinical and laboratory features of sepsis.
Fever/hypothermia Increased cardiac output/low systemic vascular resistance Increased oxygen consumption Unexplained tachycardia Unexplained tachypnea/respiratory alkalosis Altered white blood cell count Increased C-reactive protein levels Increased procalcitonin levels Unexplained hyperglycemia Unexplained lactic acidosis Unexplained respiratory dysfunction (acute lung injury) Thrombocytopenia/disseminated intravascular coagulation Unexplained disorientation or confusion Unexplained alteration in liver function tests Unexplained alteration in renal function Capillary leak syndrome
M I CO NE R PY V A RI M GH E D T
PREDISPOSING FACTORS infection probability score, which weights 6 variables [temperature, heart rate, respiratory rate, white blood cell count, C-reactive protein (CRP), sequential organ failure assessment score (SOFA)] to make a composite score, may be useful.1 New concepts In the most recent International Sepsis Consensus Conference,2 the 29 experts charged with providing a conceptual and a practical framework to define the systemic inflammatory response to infection came to the following conclusions: first, that the concepts of sepsis (the host response to an infection), severe sepsis (sepsis associated with organ dysfunction) and septic shock (sepsis plus arterial hypotension despite adequate fluid resuscitation), as defined in the 1991 North American Consensus Conference,3 remain useful to clinicians and researchers, but that they do not allow for precise staging or prognostication of the host response to infection. Second, that while the concept of systemic inflammatory response syndrome (SIRS) remains useful as a concept, the diagnostic criteria for SIRS published in 1992 3 are too sensitive and non-specific, and an expanded list of signs and symptoms of sepsis may better reflect the clinical response to infection.
88
MINERVA ANESTESIOLOGICA
In view of these conclusions, the participants introduced the PIRO (predisposing factors, infection, response, organ dysfunction) concept,2 a suggested means of staging sepsis, rather like many cancers are staged using the tumor, nodes, metastases (TNM) system. Using the emerging PIRO model could aid physicians in better characterizing heterogeneous groups of septic patients, providing insight into the continuum of sepsis, and improve the understanding and management of severe sepsis and septic shock.
Predisposing factors 4 include individual characteristics, such as age, chronic diseases, prolonged immunodepressant medications, etc., that may influence a patients response to infection and/or indicate which therapies are likely to be most effective in that patient. Increasingly, the role an individuals genetic make-up may have on the development of sepsis and the severity of disease when it develops are being explored and various polymorphisms have been shown to influence the risk of infection and/or of mortality from sepsis.5 Single nucleotide polymorphisms, microsatellite, insertion and deletion polymorphisms are all forms of genetic variation that can characterize an individuals risk for sepsis, organ dysfunction, or death.6 A polymorphism of the tumor necrosis factor- (TNF-) gene, the TNF-2 allele, is associated with increased serum levels of TNF and a greater risk of mortality from septic shock.7 A polymorphism within the intron 2 of the interleukin-1 receptor antagonist (IL-1ra) gene (IL-1RN*2) has been associated with reduced IL-1ra production and increased mortality rates.8 Polymorphisms in the Toll-like receptor (TLR) and interferon- genes have also been identified influencing susceptibility to sepsis.9, 10 Advances in genetics technology have now allowed investigators to design glass slides (chips) with minute quantities of short, gene-specific nucleotides. These genespecific probe nucleotides, ideally one for each gene in the genome, are arrayed onto the chip surface to produce a DNA microar-
IC
Marzo 2006
SEPSIS DIAGNOSIS AND MANAGEMENT
VINCENT
INFECTION Characteristics of the particular infection, such as site (e.g., lung versus urinary tract), responsible organism(s) (e.g., Gram-negative versus Gram positive, MRSA versus MSSA), severity, can have an effect on the host response and outcome, and may influence choice of treatment.11 However, while few would argue that an E. coli urinary tract infection is likely to be less life-threatening than a meningococcal meningitis, classifying the relative importance of infections on outcome is difficult. Using a systematic literature review and surveying 510 articles describing the outcome of infections, categorized by microorganism and site of infection, Cohen et al.12 recently generated specific risk codes for bacteremia, meningitis, pneumonia, skin and soft tissue infections, peritonitis, and urinary tract infections. For each infection site and organism, a two-digit code was generated according to the mortality rate associated with that infection (from 1: 5% to 4: >30%), and the level of evidence available to support the mortality risk (level A representing evidence from more than 5 studies with more than 100 patients, through to level E insufficient evidence from case reports). They suggested this system be termed the grading system for site and severity of infection (GSSSI) and although it needs to be validated, this could be a useful means of better characterizing the different risks associated with infections caused by different organisms in different sites.12 The timing of onset of infection may also influence outcomes. A recent study showed that patients who developed septic shock within 24 h of ICU admission were more severely ill, but had better outcomes than patients who developed septic shock later during their ICU stay.13
M I CO NE R PY V A RI M GH E D T
ORGAN DYSFUNCTION
Vol. 72, N. 3 MINERVA ANESTESIOLOGICA
Organ dysfunction in severe sepsis is not a simple present or not variable, but a continuous spectrum involving many organs and varying with time and treatment.16 The degree of organ involvement can be assessed with various scoring systems, one of the most commonly used being the SOFA score.17 Diagnosis of sepsis
Sepsis represents a major diagnostic problem for the intensivist and considerable effort is being concentrated on finding a sensitive and specific diagnostic marker; many have been suggested 18-22 and a non-exhaustive list of proposed markers of sepsis is shown in Table II. Studies have shown that early therapy is critical in improving outcomes from sepsis,23, 24 and the identification of a marker that would allow a clear diagnosis of sepsis would certainly help improve outcomes in these patients. Procalcitonin (PCT) and CRP are 2 candidate markers of sepsis that have received a lot of attention. CRP is an acute phase protein that was first described in the early 1930s. CRP levels are widely used as a relatively non-specific marker of inflammation, and many studies have demonstrated increased CRP levels in patients with sepsis.25-27 Concentrations above 10 mg/dL on admission have been associated with particularly
IC
ray. These can be used to generate an expression profile, the transcriptome, for the cell or tissue of interest.6 Genomics and the broader field of proteomics are likely to become increasingly routinely used in patient management.
RESPONSE The degree of host response can be assessed according to the presence or absence of various clinical and laboratory features and to the degree of elevation of, for example, white cell count, CRP, procalcitonin (PCT) etc.14 The host response will vary between patients and over time in the same patient. Volk et al. described an early hyperinflammatory phase followed by immunoparalysis based on the level of HLA-DR monocyte surface expression in septic patients.15 Improving our assessment of the host response could help direct therapies more appropriately.
89
VINCENT
SEPSIS DIAGNOSIS AND MANAGEMENT
TABLE II.Some of the suggested markers of sepsis.
White blood cell count C-reactive protein Procalcitonin Endotoxin Cytokines IL-1, IL-2, IL-4, IL-6, IL-8, IL-10, TNF, IFN-, PAF TNF-receptors IL-1 receptor antagonist, IL-1 receptors Complement factors Endothelin-1 ICAM-1, VCAM-1 Phospholipase A2 PGE2 Nitrates/nitrites Lactoferrin Elastase Neopterin
M I CO NE R PY V A RI M GH E D T
high mortality rates, and increasing or persistently high levels indicated a poor prognosis, while declining values were associated with a more favorable prognosis.28 PCT was described more recently as a potential marker of infection and is not yet routinely measured in many hospital laboratories. PCT may be superior to CRP in discriminating infectious from other inflammatory diseases. In addition, PCT has more rapid kinetics, being produced and cleared more rapidly than CRP, so may be better able to identify infection early and to follow disease progress.29, 30 Indeed several studies have shown that PCT levels are correlated with the severity of sepsis as measured by the APACHE II or sequential organ failure assessment scores.20, 29, 31, 32 Importantly, none of the markers currently available is specific to sepsis, and a diagnosis of sepsis cannot conclusively be made on the basis of the presence of any one item; however, the presence of several features can help increase the diagnostic likelihood in a patient with a suggestive clinical picture. The results of ongoing studies into markers of sepsis, such as the The Genetic and Inflammatory Markers of Sepsis (GenIMS) study, are eagerly awaited. The rapid and accurate identification of the nature of the infection is also of critical importance. As an example, identifying fungal or resistant organism more rapidly would notably improve the
90
MINERVA ANESTESIOLOGICA
The management of sepsis can be considered in 3 sections: treatment of infection, hemodynamic resuscitation and organ support, and modulation of the host response. Treatment of infection The source of infection must be identified wherever possible and eliminated by surgical removal of an infected focus when applicable, and appropriate antimicrobial therapy must be started without delay. If the causative microorganism(s) is unknown, empiric antibiotics should be started based on the likely culprit and local antibiotic patterns of prevalence and resistance. Patients who receive appropriate antibiotics have a better outcome than those who are initially treated with an ineffective antibiotic,33-35 yet a recent study of septic ICU patients found that in as many as 1/3 of patients the first line choice of antibiotic was inappropriate.36 Infectious disease specialists who are familiar with local hospital and community pathogens and resistance patterns should be involved in antimicrobial selection decisions in all patients with severe sepsis.34
Hemodynamic resuscitation
Another basic aspect of the management of the patient with severe sepsis or septic shock is optimal resuscitation, essentially involving administration of sufficient fluids, and vasoactive agents when required. Usually the criteria for starting resuscitation include: mean arterial pressure <65 mmHg, mixed venous oxygen saturation (SvO2) <70%, urine output <0.5 mL/kg/h, blood lactate concentration >1.5 mEq/L, or a worsening of the peripheral capillary circulation. The choice of one fluid type over another and the ideal endpoint of fluid resuscitation have generated considerable debate and a discussion of these aspects is beyond the remit of this paper.
IC
Management
appropriateness of antimicrobial treatment strategies.
Marzo 2006
SEPSIS DIAGNOSIS AND MANAGEMENT
VINCENT
M I CO NE R PY V A RI M GH E D T
Modulation of the host response DROTRECOGIN ALFA (ACTIVATED) The development and licensing of drotrecogin (activated), recombinant activated protein C, marked a turn-up on the rather downward sloping history of anti-sepsis therapeutics, in which multiple immunomodulatory agents have fallen to the wayside as one after another clinical trial failed to show that they had any beneficial effect on outcome. With indications that the coagulation system was keenly involved in the pathogenesis of sepsis, the spotlight fell on mediators of the coagulation pathway and their potential ability to influence sepsis outcomes. The Protein C Worldwide Evaluation in Severe Sepsis (PROWESS) study was a multicenter, randomized, controlled trial involving 1 690 patients from 164 centers in 11 countries.41 Given at a dose of 24 g/kg of body weight/h for 96 h, drotrecogin (activated) reduced mortality rates from 30.8% in the placebo group to 24.7% in the treatment group, which equated to one additional life saved for every
Vol. 72, N. 3 MINERVA ANESTESIOLOGICA
Fluid resuscitation should be commenced as early as possible in the course of septic shock (even before ICU admission).23 Requirements for fluid infusion may be difficult to determine, and such decisions can be facilitated by repeated fluid challenges. A fluid challenge comprises 4 components: the type of fluid to be administered (e.g., natural or artificial colloids, crystalloids); the rate of fluid infusion (e.g., 500 to 1 000 mL over 30 min); the endpoints (e.g., mean arterial pressure >70 mmHg, heart rate <110 beats/min); the safety limits (e.g., central venous pressure not higher than 15 mmHg). The choice of vasoactive agent has also been the subject of considerable debate with conflicting opinions in particular regarding the supremacy of dopamine or norepinephrine.37, 38 Current guidelines recommend either drug as a first-line agent,39, 40 and a randomized, controlled, double-blinded clinical trial comparing the 2 drugs is currently underway in Europe.
16 patients treated. Drotrecogin (activated)-treated patients also showed significantly faster resolution of cardiovascular and respiratory dysfunction and significantly slower onset of hematological organ dysfunction than patients who received placebo.42 Apart from an increased risk of bleeding, mostly associated with invasive procedures, there were no other safety concerns with drotrecogin (activated) in the PROWESS study. A further prospective study was conducted in 361 centers to confirm these findings and provide additional safety data. This study, ENHANCE, enrolled 2 375 adult patients and treated them with the same dose of drotrecogin (activated) as in the PROWESS study.24 The results confirmed the efficacy and safety of drotrecogin (activated). A further analysis of the safety profile of drotrecogin (activated) in more than 6 500 patients who had received the drug in clinical trials or commercially reported that 43% of bleeding events that occurred in patients who received drotrecogin (activated) were procedurerelated, and that severe thrombocytopenia and meningitis may be risk factors for serious bleeding events in patients receiving the drug.43 As a result of the inherent risk of bleeding, drotrecogin (activated) use is contraindicated in patients with active internal bleeding, recent hemorrhagic stroke, intracranial or intraspinal surgery, or severe head trauma, trauma with an increased risk of life-threatening bleeding, presence of an epidural catheter, and intracranial neoplasm or mass lesion or evidence of cerebral herniation. If a surgical procedure is necessary during treatment, the infusion should be stopped 2 h prior to the intervention and restarted 12 h after adequate hemostasis has been obtained. Drotrecogin (activated) is expensive, but in cost-effectiveness analyses, it has been shown to be comparable to other accepted ICU interventions.44, 45 Children were not included in the PROWESS study, suggested that results from open label studies and although drotrecogin (activated) has the same pharmacokinetics, pharmacodynamic effects, and safety profile in the pediatric population,46 a phase III randomized controlled trial in children with
IC
91
VINCENT
SEPSIS DIAGNOSIS AND MANAGEMENT
M I CO NE R PY V A RI M GH E D T
STEROIDS In a randomized controlled trial conducted in 19 ICUs across France and including 300 patients with septic shock, patients with relative adrenal insufficiency (as assessed by non-response to a corticotrophin test) were treated with hydrocortisone (50 mg i.v. every 6 h) and fludrocortisone (50 g per os daily) or placebo for 7 days. Treated patients had a reduced mortality compared to non-responders treated with placebo (53% vs 63%, hazard ratio 0.67, 95% CI 0.47-0.95, P=0.02).48 In a recent meta-analysis of randomized studies in patients with severe sepsis or septic shock treated with corticosteroids, overall use of corticosteroids did not significantly affect mortality.49 However, with longer courses (>5 days) of lower dose corticosteroids (300 mg hydrocortisone or equivalent), mortality at 28 days and hospital mortality were reduced.49 Another meta-analysis reached similar conclusions.50 Nevertheless, some questions remain unanswered, including the optimal test for adrenal insufficiency and whether the results can be extrapolated to patients with severe sepsis not in shock. It is not entirely clear whether steroids treat sepsis per se, or enhance hemodynamic support. Indeed, studies have indicated that steroids can increase the response to adrenergic agents. At present, steroid use in sepsis should be administered only in the presence of shock. The future As our understanding of the pathophysiology of sepsis improves, in particular the
92
MINERVA ANESTESIOLOGICA
severe sepsis has recently been discontinued for lack of efficacy. Drotrecogin (activated) is currently licensed for use in adult patients with severe sepsis and a high risk of mortality (e.g., as assessed by the APACHE II score). This decision is supported by the recent Administration of Drotrecogin alfa [activated] in Early Severe Sepsis (ADDRESS) study that failed to show effectiveness of drotrecogin (activated) in patients with less severe disease.
New anti-endotoxin agents Endotoxin (lipopolysaccharide, LPS) is a component of the Gram-negative bacterial cell wall and is a key initiator of sepsis. Once in the circulation, endotoxin binds to LPS binding protein (LBP), and the LPS-LPB complex interacts with CD14 on the surface of monocytes and macrophages resulting in cellular activation. The LPS-LPB complex can also interact with soluble CD14 and this can then interact with another receptor on the endothelial cell, which itself lacks surface CD14. LPS can also form complexes with serum lipoproteins, including low density lipoproteins (LDL), high density lipoproteins (HDL), and apolipoprotein A, which provide a means of eliminating LPS from the circulation.51 In acute illness, lipoprotein levels are reduced,52, 53 this reducing LPS clearance. Recent studies have indicated that intensive insulin therapy to maintain blood glucose levels less than 6.1 mmol/L improved outcomes predominantly by reducing deaths from sepsis-induced multiple organ failure.54 The incidence of nosocomial infections was also reduced. A further study from Van den Berghe et al. noted that intensive insulin therapy also increases HDL and LDL levels and multivariate analysis suggested that it was this change in lipid levels, rather than an effect on glucose levels, that contributed to the beneficial effects of this approach on mortality and morbidity.55 Replacing lipoproteins may therefore represent a novel method of treating sepsis. Experimental studies in human volunteers and animal models did indeed show that HDL reduced flu-like symptoms during endotoxemia, and blocked the endotoxin-induced release of TNF, IL-6 and IL-8. Interestingly, HDL administration also reduced CD14 expression on monocytes.56 In a porcine model of sepsis, an emulsion
IC
mechanisms of cell-to-cell signaling and the importance of apoptosis, more potential therapeutic targets become apparent. Here we will briefly mention just some of the many agents under research, focusing on those that are, or are almost, at the clinical trial stage.
Marzo 2006
SEPSIS DIAGNOSIS AND MANAGEMENT
VINCENT
M I CO NE R PY V A RI M GH E D T
Macrophage migration inhibitory factor (MIF) By modulating the expression of TLR4, the signal-transducing molecule in the LPS receptor complex, macrophage migration inhibitory factor (MIF) induces the production of various pro-inflammatory mediators.61 MIF levels are raised in patients with sepsis 62, 63 and correlate with outcome,63 and animal studies have demonstrated improved survival with MIF neutralization.62, 64 High-mobility group B-1 protein High-mobility group B-1 protein (HMGB1) acts as a late mediator of systemic inflammation, and is released from endotoxin-stimulated macrophages some 8-12 h after the release of the early cytokines. HMGB1 induces the activation of transcription factors and the release of pro-inflammatory mediators by monocytes and endothelial cells.65, 66 In animal models of sepsis, anti-HMGB1 antibodies, even when given late after sepsis induction, improved survival and reduced sepsis-induced organ injury.67 Ethyl pyruvate, which inhibits HMGB1 production in vivo, also improved survival in a mouse model of sepsis.68 Unlike many animal models when the onset of sepsis is determined artificially, in patients the onset is often difficult to define and many patients will be diagnosed relatively late, making the longer time-frame of HMGB1 of particular interest as it may be effective even when targeted later in the sepsis process. Hemoperfusion strategies Blood purification systems have been proposed for the treatment of sepsis based on the
Vol. 72, N. 3 MINERVA ANESTESIOLOGICA
of phospholipid, the predominant lipid in HDL, lowered serum endotoxin and TNF- levels significantly, preserved cardiac output and ejection fraction, and attenuated increases in systemic and pulmonary vascular resistances.57 A clinical trial with this phospholipid emulsion is ongoing. Other anti-endotoxin strategies currently undergoing clinical testing include anti-CD14 antibodies,58 extracorporeal endotoxin absorption,59 and lipid A analogs.60
rationale that by removing inflammatory mediators, this strategy could improve outcomes. However, hemoperfusion per se removes all mediators both good and bad and may not be beneficial in all patients at all times. Some studies have suggested that coupled plasma filtration adsorption (CPFA) improves blood pressure and restores immune function in patients with septic shock 69, 70 However, further study is needed to determine which technique may be most beneficial, and at present hemofiltration is not recommended unless there is co-existing renal failure.39
Severe sepsis and septic shock are still associated with high mortality rates, but progress is being made. Early diagnosis is vital in improving outcomes and development of more effective markers of sepsis will help in allowing treatments to be instituted as early as possible in the disease process. Appropriate infection control strategies and adequate haemodynamic stabilization remain essential, but must now be combined with drotrecogin alfa (activated) if there is no contraindication, and other immunomodulatory strategies as they become available. It is unlikely that one agent will ever be discovered to cure all patients with sepsis, just as one antibiotic cannot treat all infections, and one chemotherapy drug is not active against all cancers. Sepsis treatment must be seen as a package, with different patients requiring different packages, and the package contents varying with time in the same patient. Attempts to characterize patients, such as the PIRO system, will help in identifying which therapies are best given to which patients and when, and as new interventions undergo clinical testing, treatment protocols must be adapted accordingly. This is a rapidly moving field, very much a work in progress, and the success of drotrecogin (activated) has given new impetus to the search for effective diagnostic and therapeutic strategies in patients with sepsis.
IC
Conclusions
93
VINCENT
SEPSIS DIAGNOSIS AND MANAGEMENT
Riassunto
Diagnosi di sepsi e sua gestione: attuali progressi La sepsi grave un processo patologico comune nel paziente criticamente ammalato ed associata ad una sostanziale morbidit e mortalit. In questi ultimi anni la continua ricerca ha fornito notevoli dati sulla fisiopatologia della sepsi, evidenziando vari aspetti della risposta alla sepsi che devono essere colpiti. Le scoperte relative alla correlazione tra coagulazione e infiammazione sono state particolarmente eccitanti, consentendo lo sviluppo della proteina C attivata ricombinante. Questa revisione discuter le attuali definizioni di sepsi, descriver i nuovi approcci alla classificazione e alla diagnosi dei pazienti con sepsi e presenter le raccomandazioni per la gestione, inoltre discuter brevemente le attuali aree di ricerca e quelle future. Parole chiave: Sepsi, diagnosi - Sepsi, terapia - Terapia intensiva.
References
1. Peres-Bota D, Melot C, Lopes Ferreira F, Vincent JL. Infection probability score (IPS): a simple method to help assess the probability of infection in critically patients. Crit Care Med 2003;31:2579-84. 2. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 2003;31:1250-6. 3. Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA et al. Definition for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 1992;101:1644-55. 4. Angus DC, Burgner D, Wunderink R, Mira JP, Gerlach H, Wiedermann CJ et al. The PIRO concept: P is for predisposition. Crit Care 2003;7:248-51. 5. Lin MT, Albertson TE. Genomic polymorphisms in sepsis. Crit Care Med 2004;32:569-79. 6. Cobb JP, OKeefe GE. Injury research in the genomic era. Lancet 2004;363:2076-83. 7. Appoloni O, Dupont E, Andrien M, Duchateau J, Vincent JL. Association of TNF2, a TNF promoter polymorphism, with plasma TNF levels and mortality in septic shock. Am J Med 2001;110:486-8. 8. Arnalich F, Lopez-Maderuelo D, Codoceo R, Lopez J, Solis-Garrido LM, Capiscol C et al. Interleukin-1 receptor antagonist gene polymorphism and mortality in patients with severe sepsis. Clin Exp Immunol 2002;127:331-6. 9. Lorenz E, Mira JP, Cornish KL, Arbour NC, Schwartz DA. A novel polymorphism in the toll-like receptor 2 gene and its potential association with staphylococcal infection. Infect Immun 2000;68:6398-401. 10. Stassen NA, Leslie-Norfleet LA, Robertson AM, Eichenberger MR, Polk HC Jr. Interferon-gamma gene polymorphisms and the development of sepsis in patients with trauma. Surgery 2002;132:289-92. 11. Vincent JL, Opal S, Torres A, Bonten M, Cohen J, Wunderink R. The PIRO concept: I is for infection. Crit Care 2003;7:252-5. 12. Cohen J, Cristofaro P, Carlet J, Opal S. New method of classifying infections in critically ill patients. Crit Care Med 2004;32:1510-26.
13. Roman-Marchant O, Orellana-Jimenez CE, De Backer D, Melot C, Vincent JL. Septic shock of early or late onset: does it matter? Chest 2004;126:173-8. 14. Gerlach H, Dhainaut JF, Harbarth S, Reinhart K, Marshall JC, Levy M. The PIRO Concept: R is for response. Crit Care 2003;7:256-9. 15. Volk HD, Reinke P, Krausch D, Zuckermann H, Asadullah K, Mller JM et al. Monocyte deactivation rationale for a new therapeutic strategy in sepsis. Intensive Care Med 1996;22:S474-81. 16. Vincent JL, Wendon J, Groeneveld J, Marshall JC, Streat S, Carlet J. The PIRO Concept: O is for organ dysfunction. Crit Care 2003;7:260-4. 17. Vincent JL, de Mendona A, Cantraine F, Moreno R, Takala J, Suter P et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicentric, prospective study. Crit Care Med 1998;26:1793-800. 18. Pinsky MR, Vincent JL, Deviere J, Alegre M, Schandene L, Kahn RJ et al. Serum cytokine levels in human septic shock: relation to multiple-systems organ failure and mortality. Chest 1993;103:565-75. 19. Marty C, Misset B, Tamion F, Fitting C, Carlet J, Cavaillon JM. Circulating interleukin-8 concentrations in patients with multiple organ failure of septic and nonseptic origin. Crit Care Med 1994;22:673-9. 20. Ugarte H, Silva E, Mercan D, de Mendona A, Vincent JL. Procalcitonin as a marker of infection in the intensive care unit. Crit Care Med 1999;27:498-504. 21. Gibot S, Kolopp-Sarda MN, Bene MC, Cravoisy A, Levy B, Faure GC et al. Plasma level of a triggering receptor expressed on myeloid cells-1: its diagnostic accuracy in patients with suspected sepsis. Ann Intern Med 2004;141:9-15. 22. Marshall JC, Foster D, Vincent JL, Cook DJ, Cohen J, Dellinger RP et al. Diagnostic and prognostic implications of endotoxemia in critical illness: results of the MEDIC study. J Infect Dis 2004;190:527-34. 23. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001;345:1368-77. 24. Vincent JL, Bernard GR, Beale R, Putersen C, Dhairant JF et al. Drotrecogin alfa (activated) treatment in severe sepsis from the global open-label trial ENHANCE: further evidence for survival and safety and implications for treatment. Crit Care Med 2005;33:2266-77. 25. Pvoa P, Almeida E, Moreira P, Fernandes A, Mealha R, Arago A et al. C-reactive protein as an indicator of sepsis. Intensive Care Med 1998;24:1052-6. 26. Yentis SM, Soni N, Sheldon J. C-reactive protein as an indicator of resolution of sepsis in the intensive care unit. Intensive Care Med 1995;21:602-5. 27. Smith RP, Lipworth BJ, Cree IA, Spiers EM, Winter JH. C-reactive protein. A clinical marker in communityacquired pneumonia. Chest 1995;108:1288-91. 28. Lobo SM, Lobo FR, Bota DP, Lopes-Ferreira F, Soliman HM, Melot C et al. C-reactive protein levels correlate with mortality and organ failure in critically ill patients. Chest 2003;123:2043-9. 29. Meisner M, Tschaikowsky K, Palmaers T, Schmidt J. Comparison of procalcitonin (PCT) and C-reactive protein (CRP) plasma concentrations at different SOFA scores during the course of sepsis and MODS. Crit Care (Lond) 1999;3:45-50. 30. Castelli GP, Pognani C, Meisner M, Stuani A, Bellomi D, Sgarbi L. Procalcitonin and C-reactive protein during systemic inflammatory response syndrome, sepsis and organ dysfunction. Crit Care 2004;8:R234-42. 31. Claeys R, Vinken S, Spapen H, ver Elst K, Decochez K, Huyghens L et al. Plasma procalcitonin and C-reactive
M I CO NE R PY V A RI M GH E D T
94
MINERVA ANESTESIOLOGICA
IC
Marzo 2006
SEPSIS DIAGNOSIS AND MANAGEMENT
VINCENT
33.
50.
34.
51. 52.
M I CO NE R PY V A RI M GH E D T
35. 53. 36. 54. 37. 38. 55. 39. 56. 40. 57. 41. 58. 42. 59. 43. 60. 44. 61. 45. 62. 46. 63. 64. 47. 65. 48.
Vol. 72, N. 3 MINERVA ANESTESIOLOGICA
IC
32.
protein in acute septic shock: clinical and biological correlates. Crit Care Med 2002;30:757-62. Luzzani A, Polati E, Dorizzi R, Rungatscher A, Pavan R, Merlini A. Comparison of procalcitonin and C-reactive protein as markers of sepsis. Crit Care Med 2003;31: 1737-41. Hanon FX, Monnet DL, Sorensen TL, Molbak K, Pedersen G, Schonheyder H. Survival of patients with bacteraemia in relation to initial empirical antimicrobial treatment. Scand J Infect Dis 2002;34:520-8. Byl B, Clevenbergh P, Jacobs F, Struelens MJ, Zech F, Kentos A et al. Impact of infectious diseases specialists and microbiological data on the appropriateness of antimicrobial therapy for bacteremia. Clin Infect Dis 1999;29:60-6. Valles J, Rello J, Ochagavia A, Garnacho J, Alcala MA. Community-acquired bloodstream infection in critically ill adult patients: impact of shock and inappropriate antibiotic therapy on survival. Chest 2003;123: 1615-24. Malacarne P, Rossi C, Bertolini G. Antibiotic usage in intensive care units: a pharmaco-epidemiological multicentre study. J Antimicrob Chemother 2004;54:221-4. Vincent JL, De Backer D. My initial vasopressor agent in septic shock is dopamine rather than norepinephrine. Crit Care 2003;7:6-8. Sharma VK, Dellinger RP. The International Sepsis Forums controversies in sepsis: my initial vasopressor agent in septic shock is norepinephrine rather than dopamine. Crit Care 2003;7:3-5. Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J et al. Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 2004;32:858-73. Hollenberg SM, Ahrens TS, Annane D, Astiz ME, Chalfin DB, Dasta JF et al. Practice parameters for hemodynamic support of sepsis in adult patients: 2004 update. Crit Care Med 2004;32:1928-48. Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A et al. Recombinant human protein C Worldwide Evaluation in Severe Sepsis (PROWESS) study group. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 2001;344:699-709. Vincent JL, Angus DC, Artigas A, Kalil A, Basson BR, Jamal HH et al. Effects of drotrecogin alfa (activated) on organ dysfunction in the PROWESS trial. Crit Care Med 2003;31:834-40. Bernard GR, Macias WL, Joyce DE, Williams MD, Bailey J, Vincent JL. Safety assessment of drotrecogin alfa (activated) in the treatment of adult patients with severe sepsis. Crit Care 2003;7:155-63. Angus DC, Linde-Zwirble WT, Clermont G, Ball DE, Basson BR, Ely EW et al. Cost-effectiveness of drotrecogin alfa (activated) in the treatment of severe sepsis. Crit Care Med 2003;31:1-11. Neilson AR, Burchardi H, Chinn C, Clouth J, Schneider H, Angus D. Cost-effectiveness of drotrecogin alfa (activated) for the treatment of severe sepsis in Germany. J Crit Care 2003;18:217-27. Barton P, Kalil AC, Nadel S, Goldstein B, OkhuysenCawley R, Brilli RJ et al. Safety, pharmacokinetics, and pharmacodynamics of drotrecogin alfa (activated) in children with severe sepsis. Pediatrics 2004;113: 7-17. Abraham E, Latesia PF, Garg R, Levy H, Talwar D, Trzaskoma BL et al. Drotrecogin alfa (activated) for adults with severe sepsis and a low risk of death. N Engl J Med 2005;333:1332-41. Annane D, Sebille V, Charpentier C, Bollaert PE, Francois B, Korach JM et al. Effect of treatment with low doses
49.
of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 2002;288:862-71. Annane D, Bellissant E, Bollaert PE, Briegel J, Keh D, Kupfer Y. Corticosteroids for severe sepsis and septic shock: a systematic review and meta-analysis. BMJ 2004;329:480. Epub 2004 Aug 02. Minneci PC, Deans KJ, Banks SM, Eichacker PQ, Natanson C. Meta-analysis: the effect of steroids on survival and shock during sepsis depends on the dose. Ann Intern Med 2004;141:47-56. Lynn WA. Anti-endotoxin therapeutic options for the treatment of sepsis. J Antimicrob Chemother 1998;41 Suppl A:71-80. Gordon BR, Parker TS, Levine DM, Saal SD, Wang JC, Sloan BJ et al. Low lipid concentrations in critical illness: implications for preventing and treating endotoxemia. Crit Care Med 1996;24:584-9. van Leeuwen HJ, Heezius EC, Dallinga GM, van Strijp JA, Verhoef J, van Kessel KP. Lipoprotein metabolism in patients with severe sepsis. Crit Care Med 2003;31: 1359-66. Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M et al. Intensive insulin therapy in the critically ill patient. N Engl J Med 2001;345: 1359-67. Mesotten D, Swinnen JV, Vanderhoydonc F, Wouters PJ, Van den Berghe G. Contribution of circulating lipids to the improved outcome of critical illness by glycemic control with intensive insulin therapy. J Clin Endocrinol Metab 2004;89:219-26. Pajkrt D, Doran JE, Koster F, Lerch PG, Arnet B, van der Poll T et al. Antiinflammatory effects of reconstituted high-density lipoprotein during human endotoxemia. J Exp Med 1996;184:1601-8. Goldfarb RD, Parker TS, Levine DM, Glock D, Akhter I, Alkhudari A et al. Protein-free phospholipid emulsion treatment improved cardiopulmonary function and survival in porcine sepsis. Am J Physiol Regul Integr Comp Physiol 2003;284:R550-7. Reinhart K, Gluck T, Ligtenberg J, Tschaikowsky K, Bruining A, Bakker J et al. CD14 receptor occupancy in severe sepsis: results of a phase I clinical trial with a recombinant chimeric CD14 monoclonal antibody (IC14). Crit Care Med 2004;32:1100-8. Reinhart K, Meier-Hellmann A, Beale R, Forst H, Boehm D, Willatts S et al. Open randomized phase II trial of an extracorporeal endotoxin adsorber in suspected Gramnegative sepsis. Crit Care Med 2004;32:1662-8. Lynn M, Rossignol DP, Wheeler JL, Kao RJ, Perdomo CA, Noveck R et al. Blocking of responses to endotoxin by E5564 in healthy volunteers with experimental endotoxemia. J Infect Dis 2003;187:631-9. Calandra T, Froidevaux C, Martin C, Roger T. Macrophage migration inhibitory factor and host innate immune defenses against bacterial sepsis. J Infect Dis 2003;187 Suppl 2:S385-90. Calandra T, Echtenacher B, Roy DL, Pugin J, Metz CN, Hultner L et al. Protection from septic shock by neutralization of macrophage migration inhibitory factor. Nat Med 2000;6:164-70. Bozza FA, Gomes RN, Japiassu AM, Soares M, CastroFaria-Neto HC, Bozza PT et al. Macrophage migration inhibitory factor levels correlate with fatal outcome in sepsis. Shock 2004;22:309-13. Bozza M, Satoskar AR, Lin G, Lu B, Humbles AA, Gerard C et al. Targeted disruption of migration inhibitory factor gene reveals its critical role in sepsis. J Exp Med 1999;189:341-6. Andersson U, Wang H, Palmblad K, Aveberger AC, Bloom O, Erlandsson-Harris H et al. High mobility group 1 protein (HMG-1) stimulates proinflammatory
95
VINCENT
SEPSIS DIAGNOSIS AND MANAGEMENT
M I CO NE R PY V A RI M GH E D T
96
MINERVA ANESTESIOLOGICA
Marzo 2006
IC
cytokine synthesis in human monocytes. J Exp Med 2000;192:565-70. 66. Fiuza C, Bustin M, Talwar S, Tropea M, Gerstenberger E, Shelhamer JH et al. Inflammation-promoting activity of HMGB1 on human microvascular endothelial cells. Blood 2003;101:2652-60. 67. Yang H, Ochani M, Li J, Qiang X, Tanovic M, Harris HE et al. Reversing established sepsis with antagonists of endogenous high-mobility group box 1. Proc Natl Acad Sci U S A 2004;101:296-301. 68. Ulloa L, Ochani M, Yang H, Tanovic M, Halperin D,
Yang R et al. Ethyl pyruvate prevents lethality in mice with established lethal sepsis and systemic inflammation. Proc Natl Acad Sci U S A 2002;99:12351-6. 69. Ronco C, Brendolan A, Lonnemann G, Bellomo R, Piccinni P, Digito A et al. A pilot study of coupled plasma filtration with adsorption in septic shock. Crit Care Med 2002;30:1250-5. 70. Formica M, Olivieri C, Livigni S, Cesano G, Vallero A, Maio M et al. Hemodynamic response to coupled plasmafiltration-adsorption in human septic shock. Intensive Care Med 2003;29:703-8.
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hanumaan Bajrang Baan by JDocument104 pagesHanumaan Bajrang Baan by JAnonymous R8qkzgNo ratings yet
- Branding Assignment KurkureDocument14 pagesBranding Assignment KurkureAkriti Jaiswal0% (1)
- Item AnalysisDocument7 pagesItem AnalysisJeff LestinoNo ratings yet
- Mendoza - Kyle Andre - BSEE-1A (STS ACTIVITY 5)Document1 pageMendoza - Kyle Andre - BSEE-1A (STS ACTIVITY 5)Kyle Andre MendozaNo ratings yet
- KV3000 Programming TutorialDocument42 pagesKV3000 Programming TutorialanthonyNo ratings yet
- Topic 6Document6 pagesTopic 6Conchito Galan Jr IINo ratings yet
- Company Profile ESB Update May 2021 Ver 1Document9 pagesCompany Profile ESB Update May 2021 Ver 1Nakaturi CoffeeNo ratings yet
- Review Questions & Answers For Midterm1: BA 203 - Financial Accounting Fall 2019-2020Document11 pagesReview Questions & Answers For Midterm1: BA 203 - Financial Accounting Fall 2019-2020Ulaş GüllenoğluNo ratings yet
- Assignment File - Group PresentationDocument13 pagesAssignment File - Group PresentationSAI NARASIMHULUNo ratings yet
- AMUL'S Every Function Involves Huge Human ResourcesDocument3 pagesAMUL'S Every Function Involves Huge Human ResourcesRitu RajNo ratings yet
- Java Magazine JanuaryFebruary 2013Document93 pagesJava Magazine JanuaryFebruary 2013rubensaNo ratings yet
- Pigeon Racing PigeonDocument7 pagesPigeon Racing Pigeonsundarhicet83No ratings yet
- Group 2 Lesson 2 DramaDocument38 pagesGroup 2 Lesson 2 DramaMar ClarkNo ratings yet
- Allen F. y D. Gale. Comparative Financial SystemsDocument80 pagesAllen F. y D. Gale. Comparative Financial SystemsCliffordTorresNo ratings yet
- Grope Assignment 1Document5 pagesGrope Assignment 1SELAM ANo ratings yet
- Basics of An Model United Competition, Aippm, All India Political Parties' Meet, Mun Hrishkesh JaiswalDocument7 pagesBasics of An Model United Competition, Aippm, All India Political Parties' Meet, Mun Hrishkesh JaiswalHRISHIKESH PRAKASH JAISWAL100% (1)
- National Rural Employment Guarantee Act, 2005Document17 pagesNational Rural Employment Guarantee Act, 2005praharshithaNo ratings yet
- Full Download Test Bank For Health Psychology Well Being in A Diverse World 4th by Gurung PDF Full ChapterDocument36 pagesFull Download Test Bank For Health Psychology Well Being in A Diverse World 4th by Gurung PDF Full Chapterbiscuitunwist20bsg4100% (18)
- MELC5 - First ObservationDocument4 pagesMELC5 - First ObservationMayca Solomon GatdulaNo ratings yet
- Green Campus Concept - A Broader View of A Sustainable CampusDocument14 pagesGreen Campus Concept - A Broader View of A Sustainable CampusHari HaranNo ratings yet
- Zoonotic Diseases From HorsesDocument12 pagesZoonotic Diseases From HorsesSandra Ximena Herreño MikánNo ratings yet
- Advanced Financial Accounting and Reporting Accounting For PartnershipDocument6 pagesAdvanced Financial Accounting and Reporting Accounting For PartnershipMaria BeatriceNo ratings yet
- AI in HealthDocument105 pagesAI in HealthxenoachNo ratings yet
- HDFC Bank-Centurion Bank of Punjab: Presented By: Sachi Bani Perhar Mba-Ib 2010-2012Document40 pagesHDFC Bank-Centurion Bank of Punjab: Presented By: Sachi Bani Perhar Mba-Ib 2010-2012Sumit MalikNo ratings yet
- Foucault, M.-Experience-Book (Trombadori Interview)Document11 pagesFoucault, M.-Experience-Book (Trombadori Interview)YashinNo ratings yet
- Annals of The B Hand 014369 MBPDocument326 pagesAnnals of The B Hand 014369 MBPPmsakda HemthepNo ratings yet
- LBST 2102 Final EssayDocument9 pagesLBST 2102 Final Essayapi-318174977No ratings yet
- Duterte Vs SandiganbayanDocument17 pagesDuterte Vs SandiganbayanAnonymous KvztB3No ratings yet
- Role of Commodity Exchange in Agricultural GrowthDocument63 pagesRole of Commodity Exchange in Agricultural GrowthSoumyalin Santy50% (2)
- Ev Wireless Charging 5 PDFDocument27 pagesEv Wireless Charging 5 PDFJP GUPTANo ratings yet