Professional Documents
Culture Documents
Candidiasis Oral
Candidiasis Oral
Uploaded by
tristiarinaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Candidiasis Oral
Candidiasis Oral
Uploaded by
tristiarinaCopyright:
Available Formats
ORAL PATHOLOGY PP&A 635
Oral Candidiasis:
Clinical Manifestations, Diagnosis,
And Treatment
Karen Rossie, DDS, MS
James Guggenheimer, DDS
C
andidiasis (also known as
candidosis) is caused by an
infection or overgrowth with
the fungus Candida; the species
most commonly involved is
Candida albicans. Candidiasis affects
certain groups of the population, eg,
the debilitated, elderly, infants, denture
wearers, and the immunocompromised,
1
with prevalence of 10% to 15%.
2
Among
the general population, 25% to 75%
are carriers.
3
Oral candidiasis may present
in a number of dissimilar forms.
1,4
The
clinical appearance is influenced by
the severity, chronicity, and location of
the infection. Acute infections tend
to be diffuse and are associated with symp-
toms of soreness or burning. Chronic
infections generally produce fewer symp-
toms and can be diffuse or localized to
certain areas of the mouth. The oral man-
ifestations of candidiasis are varied, but
some major forms can be distinguished;
they may occur separately or in combi-
nation with each other.
ORAL CLINICAL
MANIFESTATIONS
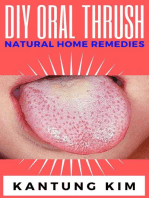
Pseudomembranous Candidiasis
Commonly called thrush or a yeast
infection, this is the most widely recog-
nized form of oral candidiasis (Figure 1),
visible as soft, white, cheesy material
that wipes off, revealing red, inflamed
mucosa. The infection is often acute but
may be chronic, depending upon the
underlying etiologic factors. Following
a course of antibiotics, a typical onset
can be sudden. Often, there are symptoms
of oral soreness or a burning sensation,
distributed diffusely throughout the
oral cavity. Some previous reports have
described an ulcerated surface underlying
the pseudomembrane of candidiasis;
however, candidiasis itself does not typ-
ically produce ulceration. Therefore, if
the underlying mucosa is ulcerated,
another diagnosis should be considered.
The white pseudomembrane overlying
an ulceration can be mistaken for can-
didiasis. However, an ulcer membrane
is more tenacious, and if it is wiped off,
a raw bleeding ulcer bed will be exposed.
There are several other common white
intraoral materials that wipe off and
must, therefore, be distinguished from
candidiasis. These include bacterial plaque
and materia alba (normal sloughing of
epithelial cells), which may accumulate,
particularly on the gingiva in debilitated
patients with poor hygiene. An uncom-
mon reaction to certain mouthwashes
and toothpastes, presenting as a thin
filmy white material, has also been ob-
served. These lesions can vaguely resemble
candidiasis, although they are less thick
and less tenacious.
Erythematous (Atrophic)
Candidiasis
This form of candidiasis presents with
red, inflamed mucosa (Figure 2). Its
appearance is identical to the mucosa,
revealed under the pseudomembranous
form when the white material is wiped
off. The patient complains of a sore, burn-
ing mouth. There may be a little pseu-
domembrane present in the morning,
but it may have sloughed off by the time
the patient presents to the dental office.
Denture Stomatitis (Denture Sore
Mouth)
Denture stomatitis is a form of erythema-
tous candidiasis in which the diffuse red-
ness of the mucosa corresponds to the
area covered by the denture (Figure 3).
It is most evident on the palate and may
occur in acute or chronic form. It is gen-
erally caused by a mixed microflora of
Candida plus bacteria.
5
Frequently, this
form of candidiasis is not an actual in-
fection, since the yeasts or pseudohyphae
Karen Rossie, DDS, MS, is Associate
Professor, Dental Specialty, Oral Medicine,
Department of Oral and Maxillofacial
Pathology, School of Dental Medicine,
University of Pittsburgh, Pittsburgh,
Pennsylvania.
James Guggenheimer, DDS, is Professor,
Dental Specialty, Oral Medicine, Depart-
ment of Oral Medicine and Pathology,
School of Dental Medicine, University of
Pittsburgh, Pittsburgh, Pennsylvania.
Address correspondence to:
Karen Rossie, DDS, MS
University of Pittsburgh
School of Dental Medicine
Department of Oral Medicine
and Pathology
Pittsburgh, PA 15261
Tel: 412-648-8637
Fax: 412-383-9142
22
Oral candidiasis (candidosis) is an infection with multiple manifestations. To prevent prolongation of undiagnosed cases, it is
essential that the dental clinicians have an understanding of the etiology, pathogenesis, and treatment of this disease. The learn-
ing objective of this article is the identification of the various clinical features of candidiasis. The underlying causes of oral can-
didiasis include antibiotic therapy, poor denture hygiene, xerostomia, immune deficiencies, diabetes, and some less common
conditions. Candidal infection may be superimposed on other mucosal diseases and may disguise the underlying disease. The
diagnosis is established using clinical appearance and patient history, and it may require diagnostic tests. A significant segment
of the population carries intraoral Candida, without any symptoms of infection, complicating the use of diagnostic tests.
are not evident in the epithelium of
biopsy specimens.
1
The inflammation
may be a reaction to the mixed micro-
organisms, held in place by the denture.
Median Rhomboid Glossitis
Another form of erythematous (atrophic)
candidiasis, median rhomboid glossitis,
presents as an atrophic area in the midline
dorsal surface of the posterior portion
of the tongue (Figure 4). The atrophy
consists of a loss of the tongue papillae,
particularly the filiform papillae, resulting
in a well-demarcated, localized smooth
area. The intensity of inflammation varies.
Median rhomboid glossitis had previously
been thought to represent a developmen-
tal anomaly; now it is recognized that
most cases are caused by candidal infection.
Evidence includes the presence of the
microorganisms in biopsied lesions and
the resolution of lesions with antifungal
medications. Localization to this area
of the tongue may be due to stasis during
swallowing as it comes in contact with
the palate. While the midline posterior
dorsal tongue is the most common
location for the lesion, it may also occur
in patches elsewhere on the dorsal tongue
and may, therefore, resemble migratory
glossitis (geographic tongue). These
two conditions can be distinguished,
since migratory glossitis generally con-
sists of multiple atrophic patches and
may display a zone of white hyperplasia
at its border with a red inflamed zone
just inside the atrophic area. Occasionally,
this distinction can be problematic, and
a cytologic smear may be required to
demonstrate the presence of Candida.
Localized Palatal Redness
Redness in the middle of the hard palate
is another form of erythematous can-
didiasis, particularly when it corresponds
to median rhomboid glossitis in the
area of the tongue with which it comes
in contact. These localized erythematous
Figure 3. Erythematous candidiasis: Denture stomatitis. The redness of the mucosal tissue
corresponds to the area covered by the denture.
Figure 2. Erythematous candidiasis: Palatal erythema. Note red, inflamed mucosa.
Candidiasis (also known as
candidosis) is caused by an
infection or overgrowth with
the fungus Candida ...
Figure 1. Acute pseudomembranous candidiasis. Note the presence of soft, white,
cheesy material.
636 Vol. 9, No. 6 ORAL PATHOLOGY
patches may be subtle, but they can
confirm a suspected case of candidiasis,
when present.
Angular Cheilitis
This term refers to inflammation at the
corners of the mouth. The clinical signs
and symptoms include redness and sore-
ness, with possible formation of fissures
and crusting ulcers (Figure 5). A mixed
infection of Candida plus certain bacteria
is responsible for the infection.
6
Angular
cheilitis is pronounced in individuals
who have deep skin folds at the angles
of the mouth. This occurs in individuals
with overclosed vertical dimension
(Figure 6). Presumably the fold of skin
provides an ideal environment for the
microorganisms to proliferate. Angular
cheilitis is frequently associated with an
intraoral candidal infection. Occasionally,
perioral skin around the entire mouth
is infected, most often in children.
Chronic Hyperplastic Candidiasis
This uncommon form of candidiasis
involves a white macular or plaque lesion
(leukoplakia) that does not wipe off. It
is often located on the buccal mucosa
just inside the commissures of the lip,
presenting as a speckled white lesion,
which becomes nodular and fissured as
it progresses (Figure 7). Generally, the
candidal infection is superimposed on
an underlying leukoplakia (Figure 8).
Treatment of these lesions with anti-
fungal medications may produce some
improvement but will not accomplish
complete resolution. Infrequently, the
leukoplakia may disappear completely
in response to antifungal therapy, sug-
gesting that the lesion is caused entirely
by the fungus. Nevertheless, candidi-
asis may have a role in carcinogenesis.
7
Leukoplakia lesions that do not resolve
completely with antifungal therapy should
be biopsied to rule out a premalignant
or a malignant condition.
Figure 6. Angular cheilitis associated with denture wearing and closed vertical dimension.
Figure 5. Angular cheilitis following a long course of antibiotic therapy.
It is important
to distinguish between
carriers of Candida ...
and actual infection.
Figure 4. Erythematous candidiasis: Median rhomboid glossitis. An atrophic area is
demonstrated in the midline dorsal surface of the posterior portion of the tongue.
ORAL PATHOLOGY PP&A 637
DIAGNOSTIC TESTS
Tests for the diagnosis of candidiasis
include the cytologic smear or exfoliative
cytology, culture, and KOH (potassium
hydroxide) preparation, designed to detect
the microorganism itself. It is important
to distinguish between carriers of
Candida 25% to 75% of the population
and actual infection.
1
Most carriers do
not have an actual infection. The white
material that wipes off in pseudomem-
branous candidiasis is composed primarily
of numerous candidal microorganisms
in the pseudohyphae or yeast forms.
This material can be removed and tested.
With a chronic infection, the pseudo-
hyphal form becomes embedded in the
superficial layers of the epithelium.
Superficial pseudohyphae can be removed
together with surface epithelial cells by
scraping the surface of a suspected lesion
with a wet tongue depressor. The material
removed is applied to a glass slide that
is sprayed with a cytological fixative and
air dried (Figure 9). The slide is then
stained in a laboratory and examined
microscopically (Figure 10).
The presence of Candida can also
be demonstrated immediately in an
unfixed smear using a technique called
a KOH preparation. The KOH solution
dissolves the epithelial cells but does
not dissolve the Candidamicroorganisms.
The yeasts and pseudohyphae remaining
on the slide can then be microscopically
observed. However, many of the micro-
organisms may be lost during processing
with the KOH technique, and this may
result in a false negative test.
A biopsy may be indicated for chronic
red and/or white lesions, since chronic
candidiasis can resemble the potentially
premalignant or malignant clinical con-
ditions leukoplakia and erythroplakia.
The microscopic appearance includes a
mildly thickened layer of parakeratin,
which may include small microabscesses
Figure 8. White nodular leukoplakia, usually found on buccal mucosa just inside
commissure is an uncommon form of chronic Candida infection.
The causes ... either
alter the balance of normal
oral microflora ... or compromise
the immune system.
Figure 9. Cytologic smear: Applying cytologic scrapings to a glass slide.
Figure 7. White intraoral plaque may have a superimposed Candida infection.
638 Vol. 9, No. 6 ORAL PATHOLOGY
containing neutrophils (Figure 11).
The typical epithelium is hyperplastic
with elongated rete pegs. There is a
mononuclear inflammatory infiltrate
in the lamina propria, consisting pri-
marily of lymphocytes. Staining the
biopsy specimen reveals varying numbers
of pseudohyphae.
ETIOLOGY/PATHOGENESIS
The causes of oral candidiasis either
alter the balance of the normal oral
microflora, alter the oral environment,
or compromise the immune system.
1,2,4,5,7
Some systemic diseases, such as HIV
infection or diabetes mellitus, place
the patient at risk for candidiasis through
more than one mechanism.
Antibiotics, especially the broad spec-
trum group such as tetracycline, are likely
to alter the oral microflora and are a com-
mon cause. Acute pseudomembranous
candidiasis may develop after only a short
course of antibiotics. Histories of lengthy
treatment with antibiotics for resistant
bacterial infections are frequently obtained
from patients with chronic candidiasis.
Dentures are another common ini-
tiator of candidiasis by altering the oral
environment. A mixture of Candida and
other microorganisms can actually live
in the nonpolished inner surfaces of the
denture acrylic.
6
A low degree of saliva increases a
patients risk for candidiasis,
8
particularly
the more severe forms of dry mouth,
such as those caused by several medi-
cations, Sjgrens syndrome, or radiation
therapy that involves the salivary glands.
The milder form of candidiasis seen in
xerostomia is often the atrophic form
in which the patient presents with a red,
burning mouth, and the white pseudo-
membrane may not be present.
Immunosuppression, particularly of
the cell-mediated immune system, such
as occurs with HIV infection, frequently
results in severe, persistent oropharyngeal
Figure 10. Cytologic smear: Microscopic appearance of Candida pseudohyphae in cyto-
logic smear, stained with periodic acid and Schiff reagents.
Figure 11. Microscopic appearance of Candida pseudohyphae invading superficial keratin
in histologic section of infected mucosa, stained with periodic acid and Schiff reagents.
Tests for the diagnosis of
candidiasis include cytologic
smear or exfoliative cytology,
culture, and KOH preparation.
Figure 12. Case 1. Patient at presentation, following 1 month on amoxicillin; the lesions
have been diagnosed as medial rhomboid glossitis.
ORAL PATHOLOGY PP&A 639
candidiasis.
9
Immunosuppressed indi-
viduals can manifest any of the clinical
forms; development of unusual genotypes
of Candida is of particular concern, since
they may be resistant to standard anti-
fungal therapies. Corticosteroid use is
another common cause of immunosup-
pression that may initiate candidiasis.
10
Patients using immunosuppressive med-
ications for long periods include those
with autoimmune diseases and organ
or bone marrow transplant recipients.
Chemotherapeutic medications for treat-
ment of cancer can similarly initiate
candidiasis.
11
A rare disorder called chronic muco-
cutaneous candidiasis is characterized
by persistent oral candidiasis and involve-
ment of the skin and nail beds.
12
These
syndromes are often inherited, but spo-
radic cases may occur.
Non-insulin- and insulin-dependent
diabetes mellitus are associated with
an increased rate of candidiasis and an
increased carrier rate of the micro-
organism.
13
Possible contributing factors,
reported in diabetes, include decreased
neutrophil function, xerostomia, and
increased glucose in the saliva.
14
TREATMENT
Topical treatment of candidiasis can be
administered in the form of a rinse,
troche, or pastille of certain antifungal
medications (eg, clotrimazole, nystatin).
1,10
Medication forms which dissolve slowly,
such as the troche or pastille, can be
more effective than rinses, since they
are in contact with the infected mucosa
over a longer period of time. Patients
with xerostomia may find it difficult to
dissolve topical medications; for them,
a rinse may be more comfortable. Topical
treatment for the adult patient requires
rinsing 4 times per day or dissolving
on a troche or pastille 5 times per day
for 10 days. An initial course of antifungal
medication is typically 10 days; however,
Figure 13. The same patient at initial presentation with erythematous lesion on the
corresponding area of palate.
Figure 15A. Case 2. Patient at presentation, with median rhomboid glossitis. 15B.
Following 2 weeks of treatment with nystatin rinses, the patient demonstrates partial resolu-
tion.
A B
Figure 14. Following 10 days of treatment with nystatin pastilles, the patient demonstrates
partial resolution of median rhomboid glossitis.
The microscopic appearance,
includes a ... layer of parakeratin,
which may include small micro-
abscesses containing neutrophils.
640 Vol. 9, No. 6 ORAL PATHOLOGY
treatment should last at least twice as
long as the time it takes to alleviate signs
and symptoms.
10
A second course of
antifungal medication may be required,
particularly in chronic forms of candidi-
asis. Antifungal rinses may have a high
sugar content, which should be taken
into consideration when prescribed for
long intervals in caries-prone patients.
The new varieties of systemic anti-
fungal medications elicit improved treat-
ment response, have fewer toxic effects,
and are used more frequently.
10
They
include fluconazole, which can be
administered in a single dose of 100 mg
per day (200 mg on the first day) in an
adult for at least 2 weeks.
15
The single
dose may result in improved patient
compliance. The drug is also available in
an oral suspension, but dosage should
be the same as for tablets, due to rapid
and almost complete absorption. There
is some risk of liver toxicity in the
imidazole group of medications (eg,
clotrimazole, itraconazole, fluconazole,
and ketoconazole), and liver function
tests should be obtained periodically.
10
Long-term dosage should be avoided
to limit possible adverse effects.
Mixed infections, such as angular
cheilitis, may benefit from topical medi-
cations (eg, clioquinol) that have antifungal
and antibacterial properties.
15
Cases with-
out a significant bacterial component
may respond well to the above antifungal
medications in cream or ointment form
alone. For angular cheilitis, any intraoral
infection should be treated in conjunction
with the extraoral problem, otherwise
the angles of the mouth may be reinfected.
In cases of denture stomatitis, the
denture and the oral cavity must be
treated in order to avoid reinfection.
10
Dentures should be soaked in commer-
cially available antiseptics or in 0.12%
chlorhexidine gluconate. An effective
disinfectant can be prepared from a
1:50 dilution of sodium hypochlorite
(chlorine bleach) in water. All dentures
should be carefully rinsed with water
prior to reseating. Antifungal ointments
or creams (eg, nystatin, clotrimazole,
or ketoconazole) can also be applied to
the inside of the denture to hold the
medication against the affected area.
Control of any underlying systemic
diseases is an important consideration
in the treatment of oral candidiasis.
Chlorhexidine may be effective for main-
tenance following resolution of an infection
in a patient who is predisposed to recurrent
candidiasis.
10
CASE PRESENTATION
Case 1
A 29-year-old female patient presented
with persistent pain in a carious man-
dibular right second molar. The patient
had periodically taken amoxicillin when-
ever the severity of the symptoms had
increased, and had taken it for 1 week
prior to presentation. There was no
other significant medical history. The
oral examination revealed a slightly
raised, inflamed, and atrophic area in
the posterior central portion of the
tongue (Figure 12). An area of inflam-
mation also involved the vault of the
hard palate (Figure 13). Cytologic smears
from the tongue and palatal lesions
exhibited large numbers of Candida
pseudohyphae.
The diagnosis was candidiasis
(median rhomboid glossitis), apparently
induced by antibiotics. The kissing
lesion of the hard palate was also con-
firmed as candidiasis. The patient was
treated with lozenges (eg, nystatin),
200,000 units held intraorally 4 times
daily and at bedtime (Figure 14). The
tongue and palate lesions had resolved
3 weeks posttreatment.
Case 2
A 72-year-old male patient presented
complaining of soreness and burning of
the tongue. The symptoms had persisted
for 3 weeks. The patient was edentulous
and had complete maxillary and mandibu-
lar dentures. The medical history included
rheumatoid arthritis with considerable
pain and stiffness that had become
increasingly refractory to treatment.
Six months prior to the onset of the oral
symptoms, the patients physician had
prescribed a regimen of prednisone,
10 mg per day, and methotrexate, 2.5 mg
three times per week. Examination of
the oral cavity revealed an erythema-
tous, atrophic strip down the midline of
the dorsal surface of the dorsal tongue
(Figure 15A). The clinical diagnosis was
candidiasis (median rhomboid glossitis)
secondary to the medications; it was
confirmed with cytologic smears. The
patient was placed on a regimen of nys-
tatin pastilles, 200,000 units dissolved
in the mouth 4 times daily and at bed-
time. Two-week follow-up revealed an
improvement of the tongue symptoms
and appearance (Figure 15B).
CONCLUSION
Oral candidiasis is common, but diagnosis
can be confusing, due to the variety of
manifestations which it demonstrates.
Some cases of oral candidiasis may remain
undiagnosed, due to the subtle appear-
ance of the disease to the untrained eye.
Other cases may be misdiagnosed due to
a resemblance to other conditions. Unrecog-
nized cases can result in needless suffering
by the patient, with symptoms that can
be effectively and rapidly alleviated by
antifungal medications. Therefore, dentists
should have an understanding of the many
faces of candidiasis as well as its etiology,
pathogenesis, and treatment.
REFERENCES
1. Allen CM. Diagnosing and managing oral can-
didiasis. J Am Dent Assoc 1992;123(1):77-78.
2. Odds FC. Candida and Candidosis. 2nd ed.
London, England: Balliere Tindall, 1988.
3. Fotos PG, Vincent SD, Hellstein JW. Oral candi-
dosis. Clinical, historical, and therapeutic fea-
tures of 100 cases. Oral Surg Oral Med Oral
Pathol 1992;74(1):41-49.
4. Fotos PG, Hellstein JW. Candida and candidosis.
Epidemiology, diagnosis and therapeutic manage-
ment. Dent Clin North Am 1992;36(4):857-878.
5. Theilade E, Budtz-Jorgensen E. Predominant
cultivable microflora of plaque on removable
dentures in patients with denture-induced stom-
atitis. Oral Microbiol Immunol 1988;3(1):8-13.
6. MacFarlane TW, Helnarska SJ. The microbiology of
angular cheilitis. Br Dent J 1976;140(12):403-406.
7. Field EA, Field JK, Martin MV. Does Candida
have a role in oral epithelial neoplasia? J Med Vet
Mycol 1989;27(5):277-294.
8. Atkinson JC, Wu AJ. Salivary gland dysfunction:
Causes, symptoms, treatment. J Am Dent Assoc
1994;125(4):409-416.
9. Coleman DC, Bennett DE, Sullivan DJ, et al. Oral
Candida in HIV infection and AIDS: New per-
spectives/new approaches. Crit Rev Microbiol
1993;19(2):61-82.
10. Fotos PG, Lilly JP. Clinical management of oral
and perioral candidosis. Dermatol Clin 1996;14
(2):273-280.
11. Rodu B, Griffin IL, Gockerman JP. Oral candidiasis
in cancer patients. South Med J 1984;77(3):312-314.
12. Porter SR, Haria S, Scully C, Richards A. Chronic
candidiasis, enamel hypoplasia, and pigmentary
anomalies. Oral Surg Oral Med Oral Pathol
1992;74(3):312-314.
13. Bartholomew GA, Rodu B, Bell DS. Oral candidi-
asis in patients with diabetes mellitus: A thor-
ough analysis. Diabetes Care 1987;10(5):607-612.
14. Aly FZ, Blackwell CC, Mackenzie DA, et al.
Factors influencing oral carriage of yeasts among
individuals with diabetes mellitus. Epidemiol
Infect 1992;109(3):507-518.
15. Drug Facts and Comparisons, 1996 edition. Facts
and Comparisons, St. Louis, MO: Wolters Kluwer,
1996.
ORAL PATHOLOGY PP&A 641
642 Vol. 9, No. 6 ORAL PATHOLOGY
1. The species of Candida most often responsible for
candidiasis is:
a. Candida candidosis.
b. Candida globrata.
c. Candida tropicalis.
d. Candida albicans.
2. Candidiasis is also commonly called all of the
following EXCEPT:
a. Thrush.
b. Trench mouth.
c. Yeast infection.
d. Candidosis.
3. The following are common oral manifestations of
candidiasis EXCEPT:
a. White material that wipes off.
b. Median rhomboid glossitis.
c. Ulceration.
d. Erythematous mucosa.
4. The pseudomembrane of pseudomembranous
candidiasis is mostly composed of:
a. Pseudohyphae and yeasts.
b. Sloughing epithelium.
c. Fibrin.
d. Necrotic cells.
5. Which of the following diseases is frequently
associated with candidiasis?
a. Osteoporosis.
b. Herpes gingivostomatitis.
c. HIV infection.
d. Colon cancer.
6. If a leukoplakia lesion infected with Candida does
NOT resolve following 4 weeks on an antifungal
medication, the dentist should:
a. Continue antifungal medication for 2 months.
b. Biopsy the lesion.
c. Discontinue antifungal medication and observe
for 6 months.
d. Give an antibiotic.
7. Which of the following medications frequently
contributes to the development of candidiasis?
a. Corticosteroids.
b. Clotrimazole.
c. Insulin.
d. Ibuprofen.
8. A special stain used to demonstrate Candida in
cytologic smears or biopsy specimens is:
a. Acid fast bacillus.
b. Mucicarmine.
c. Periodic acid and Schiff reagents.
d. Alcian blue.
9. Which form of candidiasis is frequently combined
with a bacterial infection?
a. Pseudomembranous candidiasis.
b. Angular cheilitis.
c. Median rhomboid glossitis.
d. Chronic hyperplastic candidiasis.
10. A potentially serious side effect of the imidazole
antifungal medications is:
a. Lichen planus.
b. Renal failure.
c. Diabetes mellitus.
d. Liver toxicity.
To submit your CE Exercise answers, please use the enclosed Answer Card (one for all 4 CE articles) found
opposite page 610, and complete it as follows: 1) Complete the address; 2) Identify the Article/Exercise Number;
3) Place an X in the appropriate answer box for each question for each exercise. Return the completed card.
The 10 multiple-choice questions for this Continuing Education (CE) exercise are based on the article Oral
candidiasis: Clinical manifestations, diagnosis, and treatment by Karen Rossie, DDS, MS, and James Guggenheimer,
DDS. This article is on Pages 635-641. Answers to this exercise will be published in the October 1997 issue of PP&A.
Learning Objectives:
This article describes the various clinical features of oral candidiasis, emphasizing their typical appearance, characteristics, and
locations. The underlying causes and therapy are discussed. Upon reading and completion of this exercise, the reader should have:
Knowledge of signs and symptoms of oral candidiasis, required for establishing an accurate diagnosis.
Ability to treat or refer the patient.
Continuing Education (CE) Exercise No. 22
sm
UTHSCSA
22
You might also like
- Fungal Diseases of The Oral MucosaDocument5 pagesFungal Diseases of The Oral MucosaManar AlsoltanNo ratings yet
- Oral ThrushDocument29 pagesOral ThrushTushar KhuranaNo ratings yet
- CandidiasisDocument20 pagesCandidiasisMoustafa Hazzaa100% (1)
- Candidiasis: International Class MakalahDocument16 pagesCandidiasis: International Class MakalahIrwan AzizNo ratings yet
- Variasi Normal Rongga MulutDocument18 pagesVariasi Normal Rongga MulutRafi Kusuma Ramdhan SukonoNo ratings yet
- Oral Manifestations of Systemic DiseaseDocument10 pagesOral Manifestations of Systemic DiseasedrnainagargNo ratings yet
- Oral Candidiasis: Madhu Priya.MDocument4 pagesOral Candidiasis: Madhu Priya.MinventionjournalsNo ratings yet
- White and Red Lesion Lecture 1 - DR Ameena Ryhan DiajilDocument43 pagesWhite and Red Lesion Lecture 1 - DR Ameena Ryhan Diajilفاطمة احمد غضبان الزياديNo ratings yet
- Red and White Lesions of The Oral Mucosa: DR - Wisam RasoolDocument43 pagesRed and White Lesions of The Oral Mucosa: DR - Wisam RasoolFlorida ManNo ratings yet
- Oral CandidasisDocument39 pagesOral CandidasisArmada Eka FredianNo ratings yet
- Manchas Blancas y RojasDocument16 pagesManchas Blancas y RojasJosué Zuriel OrtizNo ratings yet
- White, Red, and Mixed Lesions of Oral Mucosa A Clinicopathologic Approach To DiagnosisDocument17 pagesWhite, Red, and Mixed Lesions of Oral Mucosa A Clinicopathologic Approach To DiagnosisAlexandra LupuleasaNo ratings yet
- Oral Candidiasis: Etiology and PathogenesisDocument5 pagesOral Candidiasis: Etiology and PathogenesisNovita Indah PratiwiNo ratings yet
- 455.full CandidiasisDocument6 pages455.full CandidiasisIdris Siddiq CuakepNo ratings yet
- A Clinical Approach White LesionDocument5 pagesA Clinical Approach White LesionTirta KusumaNo ratings yet
- 961 Atharav CandidiasisDocument25 pages961 Atharav CandidiasisDevender MittalNo ratings yet
- Angular Chelitis - StatPearls - NCBI BookshelfDocument15 pagesAngular Chelitis - StatPearls - NCBI Bookshelfmichaelarchangelus7No ratings yet
- Fungal Infection, FinalDocument26 pagesFungal Infection, FinalFatima TagNo ratings yet
- Icd 10Document59 pagesIcd 10Hendra PranotogomoNo ratings yet
- Cabt 10 I 1 P 1Document5 pagesCabt 10 I 1 P 1Hanifah Nailul AmaniaNo ratings yet
- Candidiasis MucosalDocument112 pagesCandidiasis MucosalTara Sefanya KairupanNo ratings yet
- Oral Candidiasis An Overview and Case ReportDocument7 pagesOral Candidiasis An Overview and Case ReportPutri NingrumNo ratings yet
- Haider OralllllllllllllllllllllllDocument13 pagesHaider OralllllllllllllllllllllllAli YehyaNo ratings yet
- Oral CandidiasisDocument4 pagesOral CandidiasisAnish RajNo ratings yet
- Fungal OriginDocument1 pageFungal OriginAnnaNo ratings yet
- Applied Sciences: The Pseudolesions of The Oral Mucosa: Di Diagnosis and Related Systemic ConditionsDocument8 pagesApplied Sciences: The Pseudolesions of The Oral Mucosa: Di Diagnosis and Related Systemic Conditionssiti baiq gadishaNo ratings yet
- ContempClinDent111-3628383 - 100443 HIVDocument5 pagesContempClinDent111-3628383 - 100443 HIVthomas purbaNo ratings yet
- Common Oral Lesions: by Joseph Knight, PA-CDocument7 pagesCommon Oral Lesions: by Joseph Knight, PA-CAnonymous k8rDEsJsU1No ratings yet
- Stomatitis. Aetiology and A Review. Part 2. Oral Diseases Caused Candida SpeciesDocument7 pagesStomatitis. Aetiology and A Review. Part 2. Oral Diseases Caused Candida SpeciesIzzahalnabilah_26No ratings yet
- Ulcers and Vesicles2Document24 pagesUlcers and Vesicles2Kelly MayerNo ratings yet
- Department of Oral Medicine and Radiology: Seminar OnDocument26 pagesDepartment of Oral Medicine and Radiology: Seminar OnPatriciaXavier100% (1)
- Oral UlcerationDocument10 pagesOral Ulcerationمحمد حسنNo ratings yet
- Candidiasis (Candidosis)Document17 pagesCandidiasis (Candidosis)h8j5fnyh7dNo ratings yet
- Lecture 1: Bacterial&fungal Infection With Damage of Mucouse of Oral CavityDocument35 pagesLecture 1: Bacterial&fungal Infection With Damage of Mucouse of Oral CavityParisa PourkhosrowNo ratings yet
- Pediatric Oral MedicineDocument17 pagesPediatric Oral MedicinebanyubiruNo ratings yet
- Oral Findings in Secondary Syphilis: Zela Puteri Nurbani 1506668694Document15 pagesOral Findings in Secondary Syphilis: Zela Puteri Nurbani 1506668694adnanfananiNo ratings yet
- Ojsadmin, 1464Document6 pagesOjsadmin, 1464Akun MoontonNo ratings yet
- At-A-Glance: KandidiasisDocument19 pagesAt-A-Glance: Kandidiasisketty putriNo ratings yet
- Oral Candidiasis An Opportunistic Infection A ReviewDocument5 pagesOral Candidiasis An Opportunistic Infection A ReviewDino JalerNo ratings yet
- Pathogenesis and Treatment of Oral CandidosisDocument20 pagesPathogenesis and Treatment of Oral CandidosiselisabethpriskaNo ratings yet
- Candidiasis MedscapeDocument36 pagesCandidiasis MedscapesummiyaNo ratings yet
- RKDF Dental College Bhopal: Department of PeriodonticsDocument40 pagesRKDF Dental College Bhopal: Department of Periodonticsananya saxenaNo ratings yet
- Candida-Associateddenturestomatitis - Aetiologyand Management: Areview - Part2.Oraldiseasescausedby Candida SpeciesDocument7 pagesCandida-Associateddenturestomatitis - Aetiologyand Management: Areview - Part2.Oraldiseasescausedby Candida SpeciesDentist HereNo ratings yet
- Oral Mucosal Lesions in Children: Upine PublishersDocument3 pagesOral Mucosal Lesions in Children: Upine PublishersbanyubiruNo ratings yet
- Approach To Oral LesionsDocument53 pagesApproach To Oral LesionsUmut YücelNo ratings yet
- Lip LesionsDocument4 pagesLip LesionsGhada AlqrnawiNo ratings yet
- Candida Info UptodateDocument40 pagesCandida Info UptodateRamona RahimianNo ratings yet
- MoniliasisDocument2 pagesMoniliasis4gen_7100% (1)
- Contents:: Infectious DiseasesDocument87 pagesContents:: Infectious DiseasesdrnainagargNo ratings yet
- CandidiasisDocument6 pagesCandidiasisNabrazz SthaNo ratings yet
- Diagnosis and Treatment of Oral CandidosisDocument7 pagesDiagnosis and Treatment of Oral CandidosisYerly Ramirez MuñozNo ratings yet
- 3 Benign Inflammatory LesionsDocument8 pages3 Benign Inflammatory LesionsalbaablyNo ratings yet
- A. What Is Perio-Endo Lesion?Document6 pagesA. What Is Perio-Endo Lesion?Emeka NnajiNo ratings yet
- Oral CandidiasisDocument3 pagesOral CandidiasisGoutham MkNo ratings yet
- 588 Article+Text 1884 1 10 20220107Document9 pages588 Article+Text 1884 1 10 20220107Dave PutraNo ratings yet
- 39 Ahmed EtalDocument6 pages39 Ahmed EtaleditorijmrhsNo ratings yet
- CandidiasisDocument51 pagesCandidiasisLincy JohnyNo ratings yet
- b.8 Oral CandidiasisDocument14 pagesb.8 Oral Candidiasisbryamjbriceno100% (1)
- Fixed Appliances - Open Coiled Space Regainer - Jackscrew Space Regainer - Gerber Space RegainerDocument19 pagesFixed Appliances - Open Coiled Space Regainer - Jackscrew Space Regainer - Gerber Space RegainertristiarinaNo ratings yet
- Prosthetic TreatmentDocument23 pagesProsthetic Treatmenttristiarina0% (1)
- Research ArticleDocument11 pagesResearch ArticletristiarinaNo ratings yet
- Polishing Amalgam RestorationsDocument39 pagesPolishing Amalgam RestorationsMuad AbulohomNo ratings yet
- Perbedaan Jumlah Actinobacillus Actino Mycetem Comitans Pada Periodontitis Agresif Berdasarkan Jenis KelaminDocument1 pagePerbedaan Jumlah Actinobacillus Actino Mycetem Comitans Pada Periodontitis Agresif Berdasarkan Jenis KelamintristiarinaNo ratings yet
- Nteraksi Obat Dalam Praktek Edokteran Igi: Drg. Yayun Siti Rochmah SPBMDocument29 pagesNteraksi Obat Dalam Praktek Edokteran Igi: Drg. Yayun Siti Rochmah SPBMtristiarinaNo ratings yet
- Partial Odontectomy BrochureDocument2 pagesPartial Odontectomy BrochuretristiarinaNo ratings yet