Professional Documents
Culture Documents
Ulcers and Vesicles2
Uploaded by
Kelly MayerOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ulcers and Vesicles2
Uploaded by
Kelly MayerCopyright:
Available Formats
Ulcers and Vesicles Ulcers are lesions of skin or mucosa in which the entire layer of epithelium is necrotic, missing
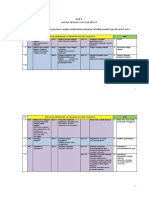
or abraded away. Most are painful. The lesion is generally gray centrally with an erythematous halo. While some ulcers originate as vesicles or bullae, others begin initially as ulcers, never having passed through a vesiculobullous stage. The configuration of the ulcer is highly germane to the diagnosis. Three configurations most often seen are: round or oval, shallow and symmetrical, irregularly marginated, and deep with rolled margins. Additionally, these ulcers may occur as solitary lesions or in multiples. Although not foolproof, the following table lists the most likely diagnoses for various ulcerative lesions: Table 1 - Configuration of Ulcers Round Shallow Multiple Herpes, Varicella-Zoster, Coxsackievirus, Aphthous Ulcers Focal Aphthous Ulcer, Denture Ulcer Irregular Shallow Multiple Agranulocytosis Focal TraumaticFocal Deep, Rolled Margins Squamous Cancer, Granulomatous Infection, Necrotizing Sialometaplasia Most of the lesions listed above can be diagnosed on the basis of clinical features alone or with the aid of laboratory studies that include culture, CBC or specific antibody titers. The viral ulcers all begin as vesicles
and are generally accompanied by fever. Each viral disease is diagnosed on the basis of lesion distribution. Primary herpetic gingivostomatitis is characterized by fever, malaise, oral pain, gingival erythema with ulceration and movable mucosal vesicles that pop to become ulcers and lymphadenopathy of cervical nodes. The labial, buccal and sublingual mucous membranes are usually involved (Figure 1). Herpes labialis affects either the upper or lower lips or sometimes both (Figure 2). The lesions represent recurrences from awakening of trigeminal ganglion latent herpes virus infections. Classically, the lesions evolve as vesicles with a tendency for clustering into groups that ulcerate, coalesce and after four to five days become crusted. After 12 days, healing occurs and the virus is inactivated immunologically, only to recur at a future date. The chief stimuli that reactivate the latent virus include intense sun exposure to the lips, emotional anxiety episodes and trauma from stretching the lips. Recurrent intraoral herpes of the palatal gingiva is typified by clusters of ulcers; a history of antecedent vesicles may be obtained from the patient (Figure 3). A history of recurrent episodes is usually gleaned. Herpes infections are treated with acyclovir, analgesics and palliative anesthetic mouth rinses. Figure 1: Primary Herpetic Gingivo Stomatitis
QuickTime and a decompressor are needed to see this picture.
QuickTime and a decompressor are needed to see this picture.
Figure 2 Recurrent herpes Labialis
Figure 3 Recurrent intraoral herpes In contrast to herpes simplex induced ulcers, coxsackievirus ulcers do not regularly recur; unlike herpes group viruses, coxsackies are not latent QuickTime and a within host neurons. In hand, foot and mouth decompressor are needed to see this picture. disease, ulcers are present anywhere in the mouth; however, unlike primary herpes, the gingiva is rarely or minimally affected. Characteristically, intact vesicles are identifiable on the hands and feet. The trunk is not involved. In another coxsackie infection known as herpangina, the lesions are limited to the oropharynx and soft palate. Other enteric viruses and coxsackies can cause mucosal ulcers that resemble aphthae; yet unlike aphthae, the patients are febrile and suffer malaise. Coxsackie-induced ulcers are widespread without a tendency for focal clustering. There are no antivirals available for coxsackievirus infections. Anesthetic mouth rinses and analgesics can be prescribed as needed.
Recurrent aphthous stomatitis (RAS) is often mistaken for a herpes infection and many practitioners are under the mistaken impression that the common canker sore is indeed a herpes virus induced lesion. In fact, the etiology of RAS remains enigmatic. Immunologic mechanisms underlie the pathogenesis; however, the instigating antigen that triggers the response remains unknown. Patients prone to develop RAS are usually young and the lesions recur from monthly to once or twice annually. The lesions never go through a vesicular stage. They ulcerate from their inception and are found on loose movable mucosa, with gingival or palatal involvement being very rare QuickTime and a (Figure 4). Patients with one to three ulcers can be treated with decompressor are needed to see this picture. silver nitrate impregnated sticks, electrocautery or laser therapy. Multiple lesions are managed with tetracycline oral rinses and palliative mouth rinses. Figure 4 Recurrent Aphtous Stomatitis Focal shallow ulcers may also represent aphthae, although trauma from a rubbing denture flange or even cheek or lip biting can produce a shallow ulcer. Traumatic ulcers will heal in 10 days when the irritant is eliminated. When a suspected traumatic ulcer does not resolve after removal of an irritant, biopsy should be performed to rule out cancer or a specific inflammatory lesion. While most traumatic ulcers are oval, some show an irregular outline. When irregularly marginated ulcers are observed and there is no history of a traumatic episode, agranulocytosis may be suspected. Agranulocytic ulcers are often large and may be multifocal. When located on the alveolar ridge or gingiva, sequestration of the bone underlying the ulcer may occur. Agranulocytosis may be idiopathic; yet, in most instances of oral ulcers secondary to decreased neutrophils, the ulcers are encountered by patients taking anticancer chemotherapeutic agents. Indeed, the occurrence of oral ulcers in a patient undergoing chemotherapy is a sign of dangerous drug toxicity that may quickly predispose to secondary infection or death. When oral ulcers are encountered, consultation with the patient's treating physician should be undertaken immediately. Focal deep ulcers with rolled margins are indicative of cancer or granulomatous inflammation from mycobacteria or deep invasive fungi. A single large ulcer in the soft palate could represent a salivary tumor, yet may also be a manifestation of minor salivary gland necrosis, a lesion often mistaken for cancer both clinically and microscopically and referred to as necrotizing sialometaplasia. All deep ulcers with rolled borders should be biopsied to reach a definitive diagnosis. Bullous/Erosive Lesions Mucosal lesions that evolve through desquamation of all or a portion of the surface epithelium are immunologic diseases that lead to erosions and bulla formation. In reality, intact bullae are rarely seen in the mouth, because blisters are easily broken, leaving broad areas of desquamation or erosion. Both humoral (immunoglobulin) and T-cell mediated immune mechanisms underlie these processes. Histopathologic diagnosis is augmented by immunofluorescence studies; therefore, biopsy should include the procurement of
a formalin fixed specimen, as well as an unfixed sample to be placed in immunofluorescence transport media to allow frozen sections and immunostaining. Four more common bullous/erosive oral diseases can be grouped according to clinical features and site predilection (Table 2): Table 2 - Common bullous/erosive lesions Buccal mucosa with associated white stria erosive lichen planus Gingival and ocular erosions mucous membrane pemphigoid Soft palate erosions pemphigus vulgaris Hemorrhagic lesions of the lips erythema multiforme The most frequently encountered oral erosive/desquamative disease is erosive lichen planus. In the erosive form of the disease, mucosal burning pain or a feeling of rawness is the chief complaint. Cutaneous lesions, if present, are usually located on the forearms and ankles as pruritic, scaly keratotic plaques overlying a violacious base. The oral lesions are red and ulcerated (Figure 5). They are usually localized to the buccal mucosa and mandibular vestibule, although other sites, particularly the gingiva, may be involved. White lacy foci usually accompany the red and erosive lesions, being "Stria of Wickham". The disease has no known etiology in the majority of cases; however, in some patients, medications cause the disease, which is then referred to as a lichenoid drug eruption. The chief drugs include antimalarials, antihypertensives and gold salts. Lichen planus-like lesions are sometimes associated with cinnamon and outdated corroding dental amalgams that are in direct contact with the lesions. Most cases, however, are idiopathic and patients tend to have lesions throughout their lives. The severity of symptoms is often accentuated by stress and anxiety. Biopsy should be performed to confirm the diagnosis and immunofluorescence studies disclose the presence of fibrinogen along the basement membrane. Topical steroids are the treatment of choice, reserving short-term systemic steroids for more severe episodes.
Figure 5 Erosive lichen planus
QuickTime and a decompressor are needed to see this picture.
After lichen planus, mucous membrane pemphigoid is the second most common oral bullous/desquamative disease. Postmenopausal - f-females are predilected 5:1 to males and
the lesions always affect the attached gingiva (Figure 6). Extragingival lesions occur anywhere in the mouth, yet are not seen in the absence of gingival desquamation. About 10% of patients will manifest conjunctival lesions (ocular, cicatricial pemphigoid). Skin lesions are not observed, except in one variant in which patients may have bullae of the face and scalp. Immunofluorescent staining shows deposition of complement and immunoglobulins along the basement membrane. Topical steroids occluded with a soft acrylic splint that extends over the attached gingiva offers the best method of control. The disease persists for many years and the etiology is unknown.
Figure 6: Mucous Membrane Pemphigoid While pemphigus vulgaris is potentially a fatal autoimmune disease, it is quite rare. Oral lesions may QuickTime and a decompressor precede skin bullae by up to six months and the oral are needed to see this picture. lesions may be the first sign of the disease. Once skin involvement occurs, there is a potential for septicemia and fluid/electrolyte imbalance, both of which may cause death. Oral lesions are extremely painful and may occur anywhere, although the soft palate is the most common. Biopsy is required for definitive diagnosis and immunofluorescent staining shows pericellular staining with complement and immunoglobulins, yielding a fishnet appearance. Systemic steroids are usually required to contain this incurable, yet controllable disease. Of all the oral bullous/desquamative diseases, only erythema multiforme (EM) has an identifiable etiology. The disease may affect skin, oral, ocular and genital mucosa as a result of allergy to sulfa drugs. Antibiotic sulfas and hypoglycemic sulfonylurea compounds are the chief precipitators. In allergic patients, lesions develop in one to two days. On the skin they may appear as bull's eye target lesions with a red center surrounded by a pale halo with an outer erythematous ring or they may be bullous. Oral lesions classically involve the lips as hemorrhagic ulcers and bullae, while intraoral lesions of a similar QuickTime and a decompressor nature occur as well (Figure 7). When oral, ocular, genital and skin are needed to see this picture. lesions occur together, the disease is referred to as erythema multiforme major, or Steven's-Johnson syndrome. The histology is nonspecific; importantly, immunostaining discloses the presence of perivascular immune complexes with complement fixation. Some cases are recurrent and are associated with the formation of immune complexes to herpes virus. In these instances, the EM outbreak is preceded by either recurrent orolabial or genital herpes lesions. Sulfa-associated EM can be managed by withdrawal of the drug and prescription of systemic prednisone. Postherpetic EM can be prevented by prescribing daily acyclovir. Figure 7 Erythema multiform The decision to prescribe topical versus systemic steroids for oral erosive diseases is generally based upon the
extent and severity of disease. Severe erosions with extensive lesions and significant pain usually warrant a seven to 10 day course of prednisone or Medrol. Less severe disease or maintenance therapy is usually managed with topical fluocinonide or clobetasol gels applied to lesional areas four to six times daily for seven days and then retreated as needed. Erythematous Lesions Erythema of the mucous membranes connotes an inflammatory reaction. Red lesions of the oral cavity may therefore represent infections, irritations or allergic reactions. Early carcinomatous transformation may appear red because the precancerous changes are accompanied by an inflammatory response in the underlying connective tissue. Location and configuration are of utmost consideration in the differential diagnosis of red mucosal lesions. In this context, red lesions are grouped as follows (Table 3): Table 3 - Red Lesions Diffuse hard palate Erythematous (atrophic) candidiasis Multifocal circinate, tongue, buccal mucosa/lips Benign migratory glossitis, Erythema migrans Focal velvety patch, soft palate, oral floor, ventral tongue Erythroplakia, Chemical injury mucositis Multifocal velvety patches Erythematous candidiasis, Multiple erythroplakias, Allergic stomatitis Perhaps the most common oral red lesion is erythematous candidiasis. In HIV infected patients the lesions can occur anywhere in the mouth. The most common form is localized to the hard palate in patients with old, illfitting dentures (Figure 8). The diagnosis can often, yet not always, be confirmed with a smear positive for mycelia using a PAS stain. Even when a smear is negative, topical nystatin treatment should be undertaken along with a soft reline. Once the erythema has resolved, a permanent reline, rebase or new denture can be fabricated. The fiery red appearance has been attributed to an allergic reaction to candida antigens and the organisms may actually accumulate within the pores of denture acrylic.
Figure 8 Erythematous Candidiasis Red lesions with a circinate (C-shaped) pattern with a white rim and a history of resolution QuickTime and a followed by recurrence at another site are benign decompressor lesions of unknown etiology. Benign migratory are needed to see this picture. glossitis or geographic tongue affects the dorsal tongue and occasionally the lateral and ventral tongue (Figure 9). The filiform papillae are shed, leaving a bald red focus with reddened fungiform papillae. Pain is uncommon. The extraglossal counterpart is erythema migrans or erythema areata migrans. No treatment is needed and the diagnosis is usually made clinically.
Figure 9 Benign Migratory Glossitis
A focal red lesion of oral mucosa with no history of migration and no QuickTime and a identifiable etiology should arouse suspicion of precancer, particularly decompressor among tobacco users. Such lesions are common on the soft palate and are needed to see this picture. floor of the mouth, being termed erythroplakias. Erythroplakic lesions may also have a white keratotic component that gives them the appellation speckled erythroplakias or speckled leukoplakias (Figure 10). Red plaques have a high probability of harboring premalignant cells (dysplasia, carcinoma-in-situ, early invasive squamous cell carcinoma). Hence, all require immediate biopsy.
Figure 10 Erythroplakia with ulcerations
QuickTime and a decompressor are needed to see this picture.
Multifocal erythematous lesions are seen in the aforementioned bullous erosive diseases, candidiasis and multifocal field cancerization. Clinical diagnosis is impossible, necessitating biopsy.
White Lesions - 1
White mucosal lesions are due to increased thickness of the epithelium (hyperorthokeratosis, hyperparakeratosis, acanthosis), the presence of ulceration with a gray-white pseudomembrane or surface mycelia from a candida infection. Clinically, white lesions may be categorized as follows (Table 4): Table 4 - White Lesions Flat smooth corrugated or verrucous plaques Leukoplakias Lace-like or striated Lichen planus, Lupusery thematosus, Hairy leukoplakia Oval shallow with a red halo Various ulcerative diseases (see section above) Diffuse widespread, buccal mucosa Genokeratoses Curdled milk-like plaques that may be rubbed away Candidiasis Idiopathic leukoplakias are white lesions of oral mucosa that do not rub away, have no readily apparent etiologic factors other than tobacco use and do not correspond to a specific disease characterized by a white appearance (Figure 11a, b). Often, white patches occur in the buccal mucosa in cheek chewers or under the flange of ill-fitting dentures (Figure 12). Some oral pathologists classify such lesions as leukoplakias. They simply represent a callous from irritation and here are referred to as frictional keratoses, because all are characterized by a benign thickening of the keratin layer. Frictional keratoses are not known to progress to cancer, while idiopathic leukoplakias have the potential for malignant transformation. An idiopathic keratosis has a 20% chance of harboring premalignant cell changes and those in the floor of the mouth harbor a 40% chance for such changes. Thus, all idiopathic leukoplakias warrant biopsy. The progression from benign hyperpara or hyperorthokeratosis to cancer usually progresses through well defined stages (Table 5): Table 5 - Stages from hyperkeratosis to cancer Hyperkeratosis
No cytologic atypia on biopsy Mild dysplasia Atypical cells confined to basal layer Moderate dysplasia Atypical cells in lower half of epithelium Severe dysplasia Atypical cells in most of epithelium Carcinoma-in-situ Atypical cells in all layers of epithelium Carcinoma Invasion of connective tissue Figure 11a leukoplakia Figure 11b leukoplakia
QuickTime and a decompressor are needed to see this picture.
QuickTime and a decompressor are needed to see this picture.
Figure 12 Denture Keratons
QuickTime and a decompressor are needed to see this picture.
Most, yet not all, idiopathic leukoplakias are associated with
tobacco use. Malignant transformation in leukoplakia occurs more often with smoking rather than smokeless tobacco (i.e.: snuff, chewing tobacco). Some of these white lesions have a corrugated, rough or granular surface and tend to occur in older females; tobacco use is frequently not a factor (Figure 13). Such lesions have specific verrucous features histologically and are referred to as proliferative verrucous leukoplakia (PVL). This disease is problematical because surgical excision is usually not effective and recurrences are common. Many cases eventually progress to squamous cell carcinoma or variant forms, with an exophytic papillary appearance (verrucous carcinoma, papillary variant of squamous cancer). Laser surgery has become a preferred method of treating these lesions and their recurrences.
Figure 13 Proliferative Verrulous Leukoplakia
QuickTime and a decompressor are needed to see this picture.
White Lesions - 2 Lichen planus, lupus erythematosus and hairy leukoplakia are white lesions of oral mucosa that show a lacy pattern or a fringe-like periphery. Lichen planus has already been discussed with erosive lesions. The nonerosive form is characterized by asymptomatic white lesions most often located in the buccal mucosa and vestibule bilaterally (Figure 14). The lacy pattern is characteristic and referred to as "Stria of Wickham". This asymptomatic form is also known as the reticular form of lichen planus and requires no treatment. Many reticular forms may progress to the painful erosive variant. Figure 14 Lichen Planus
QuickTime and a decompressor are needed to see this picture.
Lupus erythematosus is an autoimmune disease of skin and internal organs, affecting primarily young women. When oral lesions are present, they may mimic lichen planus. Usually, the histology is suggestive; yet, immunofluorescence is often helpful. Furthermore, serologic tests for antinuclear antibodies (ANA) and antiDNA antibodies support the diagnosis. If such a diagnosis is rendered, referral to an internist is recommended because
the oral lesions are only a manifestation of a more widespread, often serious disease. Hairy leukoplakia occurs in HIV seropositive patients, although a few cases have been reported in patients with other immunocompromised states. White lesions occur on the lateral tongue with vertically oriented stria resembling "sage" hairs. Biopsy shows a benign parakeratosis and the diagnosis is confirmed by special stains (DNA in situ hybridization) for the causative agent--Epstein Barr virus or Western blot for HIV positivity. The lesions are asymptomatic and usually do not require any treatment, although they recede with acyclovir therapy. This unusual form of leukoplakia serves as a precedent marker for AIDS. White sponge nevus is an inherited genokeratosis that is a dominant trait, meaning that many family members may be affected. The lesions are characteristically diffuse and bilateral, involving the entire buccal mucosa (Figure 15). The lateral and ventral tongue may also be affected. The buccal mucosal lesions are thick and show curtain-like folds. Histologically, the diagnosis is not always readily made and therefore the clinical findings are important to secure a definitive diagnosis. Once the diagnosis is made, no treatment is necessary because the lesions are asymptomatic and do not progress to carcinoma. Leukoedema is another diffuse white lesion of the buccal mucosa that occurs in African Americans. Typically, the white appearance is lost when the mucosa is stretched; biopsy is not required.
Figure 15 White Sponge Nevus The pseudomembranous form of candidiasis is a white lesion with unique features. The lesions are multiple and papular or speckled, giving the appearance of curdled milk (Figure 16). They can usually be rubbed away with gauze. This fungal infection occurs after antibiotic therapy and is common among diabetics and immunocompromised patients. In the latter, the underlying cause may be HIV infection or leukemia, lymphoma or chemotherapy patients. The clinical diagnosis is confirmed by taking a smear on a glass slide, fixing it in alcohol and having it stained in the oral pathology laboratory for the presence of hyphae. Topical nystatin pastilles or clotrimazole troches are usually effective, as are the systemic antifungals such as ketaconazole or fluconazole. In the immunocompromised patient, recurrence after cessation of antifungals is common, necessitating long-term therapy. Figure 16 Pseudomembranous Candidiasis
QuickTime and a decompressor are needed to see this picture.
QuickTime and a decompressor are needed to see this picture.
Pigmentations Three primary pigments in oral mucosa include: foreign metals or graphite tattoos, melanin, and hemosiderin. Metals are traumatically introduced into the submucosa. Melanin pigments are synthesized by melanocytes and hemosiderin pigment is the result of hemorrhage and degradation of red blood cell hemoglobin within the submucosal connective tissues. These pigmentations may be flat or raised, focal or multifocal (Table 6): Table 6 - Shapes of pigmentation lesions Focal macules Amalgam and graphite tattoos, Melanotic macule, Ephilis. Focal nodules Nevi, Melanoma, Hematoma. Diffuse and multifocal Peutz-Jehger syndrome,
Physiologic pigmentation, Melanoma, Addison's disease. A focal pigmented blue or gray spot of the oral mucosa is usually an amalgam tattoo (Figure 17). Often, they will show up as radio-opaque flecks on a dental film; however, if the metal particles are small, no radiographic evidence can be observed. Biopsy is usually indicated in such instances, although follow-up to ensure no increase in size may be pursued. Graphite tattoos result from jamming a lead pencil into the oral tissues and are usually seen in the palate. These tattoos cause no harm and do not necessarily need to be removed unless the diagnosis is in doubt. Melanotic macules and ephilis (freckle) tend to occur on the lower lip, yet can also be found intraorally (Figure 18). They represent accumulation of melanin pigment in the basal layer of the epithelium and do not progress to melanoma. They are usually brown. Early melanomas may show this appearance; biopsy diagnosis is therefore mandatory. Figure 17 Amalgam Tatoo Figure 18 Oral Pigmented Melanotic Macule
QuickTime and a decompressor are needed to see this picture.
QuickTime and a decompressor are needed to see this picture.
Nevi and melanoma may be flat; most are pigmented and raised. They may appear black or brown (Figure 19). Nevi are benign and, once excised, they do not tend to recur. Melanomas are extremely rare in the oral cavity; when they occur, the anterior maxillary gingiva or alveolar ridge are the favored sites. The lesion may be huge or a single, darkly painted nodule. Alternatively, some are red or pink with only scattered foci of pigmentation. The adjacent mucosa often shows macular pigmentations with intervening foci of pale, depigmented mucosa. Any lesion with the aforementioned features should be considered malignant melanoma unless proven otherwise by biopsy. Figure 19 Nevus Racial or physiologic pigmentation is multifocal and diffuse, involving the facial gingiva as well as other sites (Figure 20). African Americans and dark-skinned Caucasians as well as Asians, may be affected. Such changes are present for many years without any change in size and are considered normal. Multiple foci of pigmentation with a history of perioral distribution should arouse suspicion of the Peutz-Jegher syndrome. The lesions are brown or black and small, appearing as many dark freckles. Similar lesions occur on the palms of the hands.
QuickTime and a decompressor are needed to see this picture.
These lesions are an oral marker of benign intestinal polyposis and patients may give a history of bowel disorder (upset stomach, diarrhea, constipation). Recent onset of cutaneous as well as diffuse or spotty oral brown pigmentation may herald the onset of Addision's disease (adrenal insufficiency). As the adrenal cortex becomes affected, steroid levels drop and the pituitary secretes ACTH, a hormone that has melanocyte stimulating properties. Patients with Addison's disease are hypotensive and hypoglycemic. Focal Nodular Swellings Mucosal nodules are represented by proliferation of submucosal connective tissues, cysts or growths of adnexa, such as salivary tissues or gingival odontogenic tissues. These growths may be due to granulation tissue proliferation or hyperplasias of various connective tissues in response to irritation (reactive proliferations), developmental cysts, mucoceles, benign neoplasms and malignant neoplasms. Certain entities tend to occur in specific locations with the more commonly encountered lesions below (Table 7): Table 7 - Locations of Mucosal Lesions Gingiva/Sulcus Reactive proliferations, Dental abscess, Peripheral odontogenic cysts, Kaposi's sarcoma Buccal Mucosa Fibrous hyperplasia, Mesenchymal neoplasms, Salivary tumors Lips Mucoceles, Salivary tumors Floor of the mouth Mucoceles (ranulas), Dermoid cyst Lateral tongue Carcinoma
Dorsal tongue Fibrous hyperplasia (fibroma), Connective tissue tumors Palate Tori, Dental abscess, Salivary gland tumors, Kaposi's sarcoma Most swellings of the gingiva are reactive proliferations that evolve in response to some irritant lodged in the gingival sulcus. As a group, these reactive proliferations occur commonly during pregnancy. The pyogenic granuloma is the most common and tends to appear fiery red, emanating from the interdental papilla (Figure 21). Peripheral fibroma, ossifying fibroma and giant cell granuloma are the other members of this group of hyperplasias. All are treated by excision with root planing. Before jumping to the conclusion that a gingival mass is reactive, pulp testing must be performed because the mass may represent a parulis associated with a necrotic tooth (Figure 22). Periodontal probing should be performed and if a deep pocket exists and purulent exudate is expressed, a periodontal abscess is the cause of the swelling. A red mass resembling pyogenic granuloma in an HIV positive patient is most likely Kaposi's sarcoma, an AIDS-associated malignancy of vascular endothelial cells.
Figure 21 Pyogenic Granuloma
Figure 22 Peralis QuickTime and a decompressor are needed to see this picture.
QuickTime and a decompressor are needed to see this picture.
Focal fibrous hyperplasia is the most common buccal mucosa and lip nodular swelling. These so-called traumatic fibromas are dome shaped, smooth and of normal color (Figure 23). They merely represent a hyperplasia of the connective tissue that results from trauma. Biopsy should be performed to rule out a true neoplastic process. Specifically, salivary gland tumors can arise in the buccal mucosa and lips, as can nerve sheath tumors, vascular tumors and lipomas (Figure 24). When the mass is fluctuant or has a history of increasing and decreasing in size, mucocele is the probable diagnosis. Mucoceles arise from traumatic severage of the minor salivary ducts with resultant accumulation of mucous secretions in the connective tissues. Mucoceles are usually seen on the lower lip, while salivary tumors tend to arise in the upper lip.
Figure 23 Focal Fibrous Hyperplasia
Figure 24: Varix QuickTime and a decompressor are needed to see this picture.
QuickTime and a decompressor are needed to see this picture.
While most swellings of the dorsal tongue are traumatic fibromas or connective tissue tumors such as granular cell tumor, angioma or nerve sheath tumor, the lateral border is a frequent site for squamous cell carcinoma. The cancers appear as nodules and are often ulcerated. Biopsy should be performed if they do not resolve in 10 days. If the nodule is located at the lateral base of the tongue, the lesion is probably hyperplastic lingual tonsilar tissue. Biopsy is indicated here if the swelling shows progressive enlargement. Midline hard nodules of the palate are invariably tori. When a mass in the palate is off the midline, palatal abscess and salivary tumor are the chief considerations in the differential diagnosis. Palatal abscess is confirmed when adjacent to a necrotic tooth with an apical radiolucency and incision yields pus. The most common site in the mouth for salivary neoplasia is the palate. Pleomorphic adenoma is most common and may be soft or firm (Figure 25). The odds for adenocarcinoma in the palate are as high as for pleomorphic adenoma. All such masses must be biopsied. Pleomorphic adenomas are treated with simple excision, while salivary malignancies usually require a partial maxillectomy with fabrication of an obturating maxillary prosthesis. Nodules of the palate that are purple or red may represent Kaposi's sarcoma, a lesion associated with AIDS (Figure 26). Figure 25 Pleomorphic Adenoma QuickTime and a decompressor are needed to see this picture. QuickTime and a decompressor are needed to see this picture.
Figure 26 Kaposis Sarcoma
Multiple and Papillary Swellings Multiple nodular swellings of the gingiva include leukemia, drug-induced hyperplasias and fibromatosis gingiva, an inherited condition; multiple swellings of the sulcus are generally denture-induced hyperplasias
and papillary swellings may be viral-induced papillomas, inflammatory papillary hyperplasia from denture irritation or papillary forms of neoplasia (Table 8). Table 8 - Multiple and Papillary Swellings Diffuse, multifocal gingival enlargement Dilantin, Cyclosporin and calcium channel blocker-induced hyperplasia, Leukemic infiltrate, Fibromatosis gingivae Multiple nodules, vestibule Denture fibrous hyperplasia Palatal papillary lesions Denture papillomatosis Focal papillary lesions Papilloma, Verruca, Condyloma Diffuse papillary lesions Proliferative verrucous leukoplakia, Verrucous carcinoma, Papillary form of squamous cell carcinoma Diffuse gingival enlargement occurs in patients taking specific drugs. These include dilantin, cyclosporin and calcium channel blockers, all which stimulate gingival fibroblasts to undergo hyperplasia (Figures 27a, 27b). Recall that dilantin is used to control grand mal epilepsy; cyclosporin is an immunosuppressive agent used in transplant patients; calcium channel blockers are employed in the management of coronary heart disease and hypertension. Hyperplasia is minimized by appropriate prophylaxis and home care. Once present, gingivectomy is the only treatment and recurrence should be anticipated. In leukemia, malignant white cells leave the circulation and may infiltrate the gingival tissues. Such patients are usually children who present with pallor, malaise and often have petechia of the mucosa and skin. A complete blood count should be performed in suspected cases. Lastly, a rare familial disease may be the underlying cause, fibromatosis gingivae.
Figure 27 Dilantin or Cyclosporin Hyperplasia Denture hyperplasia may occur in the vestibule or palate. Ill-fitting dentures resting on resorbed ridges impinge upon the sulcus, resulting in physical irritation. This irritation will induce hyperplasia of the submucosal fibroblasts, resulting in multinodular swellings that may be fissured (epulis fissuratum). These hyperplastic tissues must be excised before fabricating a new prosthesis. When denture irritation occurs in the palate, usually a consequence of negative pressure, the palatal vault undergoes papillary hyperplasia. The vault has the appearance of a cobblestone street as multiple small papules arise and become confluent (Figure 28). Neither of these lesions has any precancerous potential. QuickTime and a decompressor are needed to see this picture. Figure 28 Papillary Hyperplasia Focal masses with a papillary surface occur in viral-induced benign growth that represent the oral counterpart of the common skin wart. The papillomavirus group of viruses are responsible. Papillomas are common on the lips, buccal mucosa, soft palate and ventral tongue. When multiple papillomas are seen, one should suspect orogenital transmission. Oral venereal warts are termed condylomas (Figure 29). The vermilion border of the lip may be the site for the common wart (verruca vulgaris). These lesions may be spread from the hands and fingers to the lips. Figure 29 Condyloma Recall from the previous discussion on leukoplakias that a verrucous form occurs, termed proliferative verrucous leukoplakia. Such lesions begin as white plaques but may progressively enlarge into diffuse multinodular and papillary growths. Eventually, they may transform into verrucous carcinomas or papillary variants of squamous cell carcinoma. The former tend to be papillary and white, whereas the latter may lose the white keratotic character. QuickTime and a decompressor are needed to see this picture.
QuickTime and a decompressor are needed to see this picture.
Your answer was incorrect. CLOSE [X] Focal masses with a papillary surface occur in viral-induced benign growths that represent the oral counterpart of the common skin wart. The papillomavirus group of viruses are responsible. Papillomas are common on the lips, buccal mucosa, soft palate and ventral tongue. When multiple papillomas are seen, one should suspect orogenital transmission. Oral venereal warts are termed condylomas (Figure 29). The
vermilion border of the lip may be the site for the common wart (verruca vulgaris). These lesions may be spread from the hands and fingers to the lips.
Summary Since the dentist is on the front line of defense for the identification and treatment of lesions of the oral cavity, we must be ready to accept the challenge. This presentation was designed to reacquaint the practicing dentist with some of the most common soft tissue lesions that may be encountered in a dental practice. Soft tissue mucosal diseases were conveniently grouped into seven different lesion forms for ease of identification. Specific disease processes occurring under the general form categories were discussed relative to varying etiopathognesis. 1) White stria accompanying red erosive lesions in the buccal mucosa is typical for: pemphigoid pemphigus herpes candidiasis lichen planus 2) White lesions of the lateral tongue with vertical striations may be a harbinger of: diabetes HIV infection lichenplanus cancer When multiple papillomas are seen in the oral mucosa, the following lesion should be suspected: condyloma denture papillomatosis verruca vulgaris 4) The treatment of choice for multiple aphthae is: tetracycline oral suspension topical steroids penicillin erythromycin oral rinse acyclovir Recurrent aphthous stomatitis (RAS) is often mistaken for a herpes infection and many practitioners are under the mistaken impression that the common canker sore is indeed a herpes virus induced lesion. In fact, the etiology of RAS remains enigmatic. Immunologic mechanisms underlie the pathogenesis; however, the instigating antigen that triggers the response remains unknown. Patients prone to develop RAS are usually young and the lesions recur from monthly to once or twice annually. The lesions never go through a vesicular stage. They ulcerate from their inception and are found on loose movable mucosa, with gingival or palatal
involvement being very rare (Figure 4). Patients with one to three ulcers can be treated with silver nitrate impregnated sticks, electocautery or laser therapy. Multiple lesions are managed with tetracycline oral rinses and palliative mouth rinses. The most likely cause of a focal pigmented spot in the palate of long duration is: graphite tattoo melanoma amalgam tattoo melanotic macule coxsackievirus infection A focal pigmented blue or gray spot of the oral mucosa is usually an amalgam tattoo (Figure 17). Often, they will show up as radio-opaque flecks on a dental film; however, if the metal particles are small, no radiographic evidence can be observed. Biopsy is usually indicated in such instances, although follow-up to ensure no increase in size may be pursued. Graphite tattoos result from jamming a lead pencil into the oral tissues and are usually seen in the palate. These tattoos cause no harm and do not necessarily need to be removed unless the diagnosis is in doubt. Melanotic macules and ephilis (freckle) tend to occur on the lower lip, yet can also be found intraorally (Figure 18). They represent accumulation of melanin pigment in the basal layer of the epithelium and do not progress to melanoma. They are usually brown. Early melanomas may show this appearance; biopsy diagnosis is therefore mandatory. The most common nodular mass of the buccal mucosa is: Hemangioma mucocele nerve sheath tumor Pyogenic granuloma traumatic fibroma Salivary gland tumors appear as masses, most frequently located in the: tongue gingiva buccal mucosa palate Focal fibrous hyperplasia is the most common buccal mucosa and lip nodular swelling. These so-called traumatic fibromas are dome shaped, smooth and of normal color (Figure 23). They merely represent a hyperplasia of the connective tissue that results from trauma. Biopsy should be performed to rule out a true neoplastic process. Specifically, salivary gland tumors can arise in the buccal mucosa and lips, as can nerve sheath tumors, vascular tumors and lipomas (Figure 24). When the mass is fluctuant or has a history of increasing and decreasing in size, mucocele is the probable diagnosis. Mucoceles arise from traumatic severage of the minor salivary ducts with resultant accumulation of mucous secretions in the connective tissues. Mucoceles are usually seen on the lower lip, while salivary tumors tend to arise in the upper lip. Most of the oral bullous-desquamative-erosive diseases respond to: steroids
penicillin nystatin calcium channel blockers NSAIDs Leukoplakias occurring in females who do not smoke and which show a rough or warty appearance are termed: candidiasis frictional keratoses lichen planus verrucous carcinoma proliferative verrucous leukoplakia Leukoplakias in general have a _____ percent chance of precancerous change while those in the floor of the mouth have a _____ percent chance. 5%, 90% 10%, 50% 20%, 40% Gingival masses arising from the interdental papilla are usually: sarcomas salivary tumors melanomas reactive proliferations Diffuse erythema of the hard palate in a denture wearer is most likely: candidiasis physical irritation precancerous Desquamative lesions of the gingiva and basement membrane immunofluorescent for immunoglobulins and complement are classic features of: mucous membrane pemphigoid desquamative candidiasis pemphigus vulgaris erythema multiforme coxsackievirus infection Curdled milk multifocal white spots that rub away in a patient who recently was on a course of antibiotics are typical for: herpes simplex leukoplakia
candidiasis erosive lichen planus lupus erythematosis All multifocal red lesions should be biopsied because: precancerous change is likely they cannot be diagnosed clinically most are immunologic diseases that require biopsy for diagnosis Multifocal erythematous lesions are seen in the aforementioned bullous erosive diseases, candidiasis and multifocal field cancerization. Clinical diagnosis is impossible, necessitating biopsy.
A pigmented mass in the anterior alveolar ridge is suspicious for: multiple myeloma pigmented candidiasis graphite tattoo ephilis malignant melanoma A patient with fever, lymphadenopathy, mucosal and gingival vesiculoulcerative lesions suffers from: varicella Zoster hairy leukoplakia recurrent herpes primary herpes (primary herpetic stomatitis) allergic stomatitis Most of the lesions listed above can be diagnosed on the basis of clinical features alone or with the aid of laboratory studies that include culture, CBC or specific antibody titers. The viral ulcers all begin as vesicles and are generally accompanied by fever. Each viral disease is diagnosed on the basis of lesion distribution. Primary herpetic gingivostomatitis is characterized by fever, malaise, oral pain, gingival erythema with ulceration and movable mucosal vesicles that pop to become ulcers and lymphadenopathy of cervical nodes. The labial, buccal and sublingual mucous membranes are usually involved (Figure 1). Herpes labialis affects either the upper of lower lips or sometimes both (Figure 2). The lesions represent recurrences from awakening of trigeminal ganglion latent herpes virus infections. Classically, the lesions evolve as vesicles with a tendency for clustering into groups that ulcerate, coalesce and after four to five days become crusted. After 12 days, healing occurs and the virus is inactivated immunologically, only to recur at a future date. The chief stimuli that reactivate the latent virus include intense sun exposure to the lips, emotional anxiety episodes and trauma from stretching the lips. Recurrent intraoral herpes of the palatal gingiva is typified by clusters of ulcers; a history of antecedent vesicles may be obtained from the patient (Figure 3). A history of recurrent episodes is usually gleaned. Herpes infections are treated with acyclovir, analgesics and palliative anesthetic mouth rinses. A focal erythematous velvety lesion in the soft palate of a smoker is at high risk for:
candidiasis erosive lichen planus sarcoma dysplasia syphilis A fluctuant mass of the lower lip is usually a _____, while a mass in the upper lip is more likely to be a _ ____. hemangioma, fibroma mucocele, salivary tumor fibroma, squamous cell carcinoma mucocele, hemangioma Focal fibrous hyperplasia is the most common buccal mucosa and lip nodular swelling. These so-called traumatic fibromas are dome shaped, smooth and of normal color (Figure 23). They merely represent a hyperplasia of the connective tissue that results from trauma. Biopsy should be performed to rule out a true neoplastic process. Specifically, salivary gland tumors can arise in the buccal mucosa and lips, as can nerve sheath tumors, vascular tumors and lipomas (Figure 24). When the mass is fluctuant or has a history of increasing and decreasing in size, mucocele is the probable diagnosis. Mucoceles arise from traumatic severage of the minor salivary ducts with resultant accumulation of mucous secretions in the connective tissues. Mucoceles are usually seen on the lower lip, while salivary tumors tend to arise in the upper lip. A febrile patient with oral hand and foot vesiculoulcerative lesions has: rhabdovirus coxsackievirus varicella herpes simplex HIV infection http://www.adaceonline.org/index.aspx?sec=olce&sub=cmain&ce_id=1028§ion_id=21
You might also like
- Oral Ulceration Causes and DiagnosisDocument10 pagesOral Ulceration Causes and Diagnosisمحمد حسنNo ratings yet
- Ulcerations of The Oral Cavity Infection Causing Oral UlcerationDocument17 pagesUlcerations of The Oral Cavity Infection Causing Oral UlcerationSebastian QuinteroNo ratings yet
- نور الهدى?Document16 pagesنور الهدى?nooraalhuda99No ratings yet
- Ulcerative Vesicular Bullous Lesions 1Document32 pagesUlcerative Vesicular Bullous Lesions 1Mustafa AliNo ratings yet
- RKDF Dental College Bhopal: Department of PeriodonticsDocument40 pagesRKDF Dental College Bhopal: Department of Periodonticsananya saxenaNo ratings yet
- Oral PathologyDocument18 pagesOral Pathologyمنتظر منشد دعاشNo ratings yet
- COLGATE Oral - Lesions - BookDocument89 pagesCOLGATE Oral - Lesions - BookVijetha RaiNo ratings yet
- Oral Ulcerative LesionsDocument34 pagesOral Ulcerative LesionsAhmed NajmNo ratings yet
- Guide to diagnosing and managing oral ulcersDocument10 pagesGuide to diagnosing and managing oral ulcersMazaya Haekal IINo ratings yet
- Ch04oral MedicineDocument35 pagesCh04oral MedicineNaleena JosephNo ratings yet
- A Clinical Approach White LesionDocument5 pagesA Clinical Approach White LesionTirta KusumaNo ratings yet
- Lecture 1: Bacterial&fungal Infection With Damage of Mucouse of Oral CavityDocument35 pagesLecture 1: Bacterial&fungal Infection With Damage of Mucouse of Oral CavityParisa PourkhosrowNo ratings yet
- Skin Diseases Affecting The VulvaDocument7 pagesSkin Diseases Affecting The VulvaNoraNo ratings yet
- Common Oral Lesions: by Joseph Knight, PA-CDocument7 pagesCommon Oral Lesions: by Joseph Knight, PA-CAnonymous k8rDEsJsU1No ratings yet
- Medicine Notes Dr. Fatima and Dr. Rowida2Document38 pagesMedicine Notes Dr. Fatima and Dr. Rowida2qbnc8727s5No ratings yet
- Common Oral Mucosal Diseases Chapter 1Document8 pagesCommon Oral Mucosal Diseases Chapter 1Nidya PutriNo ratings yet
- Ilovepdf MergedDocument22 pagesIlovepdf MergedSRO oONo ratings yet
- Tugas Jurnal Blok 12Document7 pagesTugas Jurnal Blok 12Astasia SefiwardaniNo ratings yet
- Pediatric Mucosal DiseasesDocument45 pagesPediatric Mucosal DiseasesAZZAHRA KARYA BULAN IRIANDANo ratings yet
- Oral Manifestations Ofviral InfectionsDocument5 pagesOral Manifestations Ofviral InfectionsNur Adha AtjoNo ratings yet
- Lichen Planus Guide: Symptoms, Diagnosis and TreatmentDocument17 pagesLichen Planus Guide: Symptoms, Diagnosis and TreatmentRahma Tya Anwar0% (1)
- Oral UlcerationDocument29 pagesOral UlcerationMINI DHABANo ratings yet
- Lesi Multipel Akut (Infeksi Virus & Bakteri)Document19 pagesLesi Multipel Akut (Infeksi Virus & Bakteri)Icha AnviniNo ratings yet
- LP 160610182350Document25 pagesLP 160610182350Karthik TNo ratings yet
- Oral UlcersDocument141 pagesOral UlcersKamal-Eldin Ahmed Abou-Elhamd100% (1)
- Otolaryngologic Manifestations of HIV Infection: ReviewsDocument6 pagesOtolaryngologic Manifestations of HIV Infection: ReviewsSo NicNo ratings yet
- Oral Ulcers & Vesiculobullous Lesions GuideDocument54 pagesOral Ulcers & Vesiculobullous Lesions GuideAbbas Qahtan JameelNo ratings yet
- Carranza Edisi 11 Hal 84-87Document11 pagesCarranza Edisi 11 Hal 84-87erninurhayatiNo ratings yet
- Oral Manifestations of Viral Infections: CPD ArticleDocument4 pagesOral Manifestations of Viral Infections: CPD ArticleAlvionita AnggrainyNo ratings yet
- Viral Infections: Presented By: Fatimah Zahraa Ahmed Supervised By: DR - RafilDocument31 pagesViral Infections: Presented By: Fatimah Zahraa Ahmed Supervised By: DR - Rafilfatimah zahraaNo ratings yet
- Diagnosis of Periodontal Manifestations of Systemic DiseasesDocument13 pagesDiagnosis of Periodontal Manifestations of Systemic DiseaseskochikaghochiNo ratings yet
- Vesiculobullous Diseases of the Oral MucosaDocument73 pagesVesiculobullous Diseases of the Oral MucosaAARYANo ratings yet
- Dermatology RevisionDocument6 pagesDermatology RevisionLedia EssamNo ratings yet
- Herpes Zoster (Shingles) : Muhammad Abdullah Dept. of Dermatology DHQ Hospital FaisalabadDocument26 pagesHerpes Zoster (Shingles) : Muhammad Abdullah Dept. of Dermatology DHQ Hospital FaisalabadwaleedNo ratings yet
- Patient With Single Ulcer: Traumatic Injuries Causing Solitary UlcerationsDocument3 pagesPatient With Single Ulcer: Traumatic Injuries Causing Solitary UlcerationshusseinNo ratings yet
- Show Infetious Diseases IDocument18 pagesShow Infetious Diseases Iريام الموسويNo ratings yet
- Syphilis: DR Muniba SaleemDocument45 pagesSyphilis: DR Muniba SaleemAbdur RehmanNo ratings yet
- Painfulorallesions: Istvan A. HargitaiDocument13 pagesPainfulorallesions: Istvan A. HargitaiAlejandro Ln CNo ratings yet
- Erythema MultiformeDocument5 pagesErythema MultiformeNicco MarantsonNo ratings yet
- Long-Standing Oral Ulcers: Proposal For A New S-C-D Classification System'Document14 pagesLong-Standing Oral Ulcers: Proposal For A New S-C-D Classification System'Tegar Subeqi MochammadNo ratings yet
- Cutaneous TB ReviewDocument7 pagesCutaneous TB ReviewMusdalifah MimousNo ratings yet
- Integumen Viral InfectionDocument34 pagesIntegumen Viral InfectionNissa KeyssaNo ratings yet
- Behcet's Disease (Adamantiades Syndrome) : DefinitionDocument9 pagesBehcet's Disease (Adamantiades Syndrome) : DefinitionNuzairah AynoorNo ratings yet
- Bacteriology, Histopathology, Sequelae and Pathogenesis of Oral Mucosal LesionsDocument24 pagesBacteriology, Histopathology, Sequelae and Pathogenesis of Oral Mucosal LesionsVijetha RaiNo ratings yet
- Aphthous Stomatitis - Background, Pathophysiology, EpidemiologyDocument8 pagesAphthous Stomatitis - Background, Pathophysiology, EpidemiologyRizalRyamizardNo ratings yet
- Human Immunodeficiency Virus AND Acquired Immunodeficiency SyndromeDocument59 pagesHuman Immunodeficiency Virus AND Acquired Immunodeficiency SyndromeJose Joy IdicullaNo ratings yet
- Superficial Skin Infections and The Use of Topical and Systemic Antibiotics in General PracticeDocument4 pagesSuperficial Skin Infections and The Use of Topical and Systemic Antibiotics in General Practicepeter_mrNo ratings yet
- Viral Infections of the Oral CavityDocument154 pagesViral Infections of the Oral CavityrizwanNo ratings yet
- Oral Findings in Secondary Syphilis: Zela Puteri Nurbani 1506668694Document15 pagesOral Findings in Secondary Syphilis: Zela Puteri Nurbani 1506668694adnanfananiNo ratings yet
- Muco-Cutaneous & Aphthous UlcerDocument7 pagesMuco-Cutaneous & Aphthous Ulcerربيد احمد مثنى يحيى كلية طب الاسنان - جامعة عدنNo ratings yet
- Viral Skin Infections: Verrucae ValgarusDocument14 pagesViral Skin Infections: Verrucae Valgarusمسلم هاشم منافNo ratings yet
- Enfermedades InmunologicasDocument14 pagesEnfermedades InmunologicasKarina OjedaNo ratings yet
- Haider OralllllllllllllllllllllllDocument13 pagesHaider OralllllllllllllllllllllllAli YehyaNo ratings yet
- Traslate Bab 8 TopazianDocument87 pagesTraslate Bab 8 TopazianAnonymous bLf4glCRffNo ratings yet
- PV 1Document4 pagesPV 1Aing ScribdNo ratings yet
- Arduino 2017Document8 pagesArduino 2017neetika guptaNo ratings yet
- Red and White Oral Mucosa Lesions CausesDocument43 pagesRed and White Oral Mucosa Lesions Causesفاطمة احمد غضبان الزياديNo ratings yet
- Candida-Associateddenturestomatitis - Aetiologyand Management: Areview - Part2.Oraldiseasescausedby Candida SpeciesDocument7 pagesCandida-Associateddenturestomatitis - Aetiologyand Management: Areview - Part2.Oraldiseasescausedby Candida SpeciesDentist HereNo ratings yet
- Skin Lichen Planus, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandSkin Lichen Planus, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Dsce High YieldDocument29 pagesDsce High YieldLorenzini Grant50% (2)
- Electromagnetic Radiation Therapy Effect On Dimensional Stability of Denture Bases and Its Oral Health Impact On Daily PerformanceDocument10 pagesElectromagnetic Radiation Therapy Effect On Dimensional Stability of Denture Bases and Its Oral Health Impact On Daily PerformanceIJAR JOURNALNo ratings yet
- Oral Chemical Burns Caused by Topical Application of Policresulen A Case ReportDocument4 pagesOral Chemical Burns Caused by Topical Application of Policresulen A Case Reportrahmania alikhlashNo ratings yet
- SLS Dan SARDocument1 pageSLS Dan SARNia DamayantiNo ratings yet
- PPK DOKTER GIGI EDIT Bareng (23102014) .2 PDFDocument10 pagesPPK DOKTER GIGI EDIT Bareng (23102014) .2 PDFeatmyfleasNo ratings yet
- ArticlesDocument6 pagesArticlesmeena syedNo ratings yet
- Herpetic StomatitisDocument21 pagesHerpetic StomatitisZulfahmi RizkiNo ratings yet
- Nickel Allergy and Orthodontics, A Review and Report of Two CasesDocument5 pagesNickel Allergy and Orthodontics, A Review and Report of Two CasesRockey ShrivastavaNo ratings yet
- 9780323080323 (1)Document51 pages9780323080323 (1)nsahai06No ratings yet
- CANCERDocument63 pagesCANCERTrixie Marie Sabile AbdullaNo ratings yet
- Epidemiology and Etiology of Denture Stomatitis: KeywordsDocument10 pagesEpidemiology and Etiology of Denture Stomatitis: Keywordsluthfia choirunnisaNo ratings yet
- Oral Uleration: Thilanka Umesh SugathadasaDocument37 pagesOral Uleration: Thilanka Umesh SugathadasaJuhiJahan AmanullahNo ratings yet
- Oral Manifestations of Systemic Diseases A Review, 2014 PDFDocument9 pagesOral Manifestations of Systemic Diseases A Review, 2014 PDFDwi Indah LestariNo ratings yet
- COVID-19 AstraZeneca Vaccine Analysis PrintDocument65 pagesCOVID-19 AstraZeneca Vaccine Analysis PrintcorreaNo ratings yet
- Essentials of Business Law 10th Edition Liuzzo Solutions Manual Full Chapter PDFDocument37 pagesEssentials of Business Law 10th Edition Liuzzo Solutions Manual Full Chapter PDFquandiendjv100% (14)
- A Colour Handbook of Oral Medicine - M. Lewis, R. Jordan (Manson, 2004) WW PDFDocument177 pagesA Colour Handbook of Oral Medicine - M. Lewis, R. Jordan (Manson, 2004) WW PDFAdrian Tirla100% (1)
- Acj Case Diagnosis Frameworks - March 2018 - EnglishDocument14 pagesAcj Case Diagnosis Frameworks - March 2018 - EnglishKritarth Pandey0% (1)
- OSMFDocument20 pagesOSMFAl RawdhaNo ratings yet
- Handbook Oral Medicine PDFDocument217 pagesHandbook Oral Medicine PDFpretty100% (1)
- Ulcerative, Vesicular, andDocument117 pagesUlcerative, Vesicular, andvanshikaNo ratings yet
- Pub - Clinical Outline of Oral Pathology Diagnosis and T PDFDocument755 pagesPub - Clinical Outline of Oral Pathology Diagnosis and T PDFT100% (1)
- Alimentary Pathology 1 Intro Oral CavityDocument41 pagesAlimentary Pathology 1 Intro Oral CavityCourtney SandsNo ratings yet
- Brookes (2020), Current Uses of Chlorhexidine For Management of Oral Disease: A Narrative ReviewDocument10 pagesBrookes (2020), Current Uses of Chlorhexidine For Management of Oral Disease: A Narrative ReviewPhuong ThaoNo ratings yet
- Approach To Oral LesionsDocument53 pagesApproach To Oral LesionsUmut YücelNo ratings yet
- Kenalogin OrabasepasteDocument4 pagesKenalogin OrabasepasteAndi Muhammad Imam RNo ratings yet
- Oral Medicine PPDocument32 pagesOral Medicine PPHanin AbukhiaraNo ratings yet
- Oral Medicine MCQs CollectionDocument47 pagesOral Medicine MCQs CollectionBharti KahiNo ratings yet
- Management of Herpangina: Denta, Jurnal Kedokteran GigiDocument5 pagesManagement of Herpangina: Denta, Jurnal Kedokteran GigirizadNo ratings yet
- Oral Manifestations of Nutritional Disorders2Document33 pagesOral Manifestations of Nutritional Disorders2Yeoh Wen LiNo ratings yet
- Denture Induced StomatitisDocument15 pagesDenture Induced StomatitisSaroash SadruddinNo ratings yet