Professional Documents
Culture Documents
Pneumonia in Elderly
Uploaded by
Abdi Nusa Persada Nababan0 ratings0% found this document useful (0 votes)
4 views1 pageADC
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentADC
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
4 views1 pagePneumonia in Elderly
Uploaded by
Abdi Nusa Persada NababanADC
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 1
[Pneumonia in the elderly: results of quality improvement
program for a geriatric department in Lower Saxony 2006-
2009].
[Article in German]
Gogol M
1
, Schmidt D, Dettmer-Flgge A, Vaske B.
Author information
Abstract
BACKGROUND:
Is the time to diagnosis and to start antibiotic therapy a major factor contributing to the
outcome in geriatric patients?
METHODS:
In 2006, a program for documentation and improvement for diagnostic and therapeutic
procedures in patients with community-acquiredpneumonia was introduced in German
hospitals. The analyses were performed centrally by an independent board.
SETTING:
Tertiary geriatric department with 70 beds for acute care and rehabilitation in a hospital, also
including a department of neurology and neurological rehabilitation.
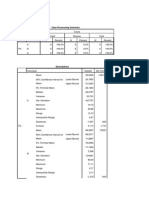
RESULTS:
In Lower Saxony (LS), 81,853 patients were treated between 2006-2009 in
our geriatric department (GD). In LS, 55.3% of the population was male, while 45.2% of the
patients in the GD were male (p=0.063). Throughout an age of 79 years, the distribution was
equal; however in the age groups 80-89 years (LS vs GD: 32.3 vs 47.6%) and >90 years (LS
vs GD: 10.2 vs 15.5%, p<0.001) there were a higher proportion of male patients in the GD.
The proportion of male nursing home patients was 46.8% vs 24.3%, hospital or rehabilitation
unit 6.2% vs 40.5%, and status of confinement to bed was 47% vs 35.1% (LS vs GD,
p<0.001). Delirium caused by pneumonia occurred in 24.4% vs 9.3% and a status of chronic
delirium (dementia) was assessed by 75.6% vs. 90.7% of all cases (LS vs GD, p=0.021).
The distribution about the risk classes 1/2/3 of the CRB-65 score was 14.9/76.9/8.2% in LS
and 3.6/89.3/7.1% in the GD (p=0.011). The time to starting antibiotics (no therapy, <4, 4-8,
and >8 h) was 2.2/83.0/7.6/7.2% in LS and 15.4/47.4/10.3/26.9% in GD patients (p<0.001).
Overall mortality rates did not differ significantly (LS 14.6% vs GD 11.9%, p=0.53).
CONCLUSIONS:
Patients in the GD were older and more functionally dependent. The distribution of the risk
index CRB-65 shows that these patients were at higher risk, were more often cognitively
impaired (not caused by pneumonia), and time to starting antibiotics was longer. However,
none of these differences had an influence on total mortality. The results are limited by the
number of patients, potential differences of the treatment groups, and the quality of data in
general as a result of a quality improvement program.
You might also like
- 2022 Clinical Features and Risk Factors of Mortality in Patients With Posterior Reversible Encephalopathy SyndromeDocument7 pages2022 Clinical Features and Risk Factors of Mortality in Patients With Posterior Reversible Encephalopathy SyndromeSafitri MuhlisaNo ratings yet
- Principales Emergencias Oncológicas en El Cáncer de Pulmón: Un Análisis de Un Único CentroDocument3 pagesPrincipales Emergencias Oncológicas en El Cáncer de Pulmón: Un Análisis de Un Único CentroJoskarla MontillaNo ratings yet
- Pharmaceutical Sciences: Recent Advances and Treatments of Childhood Nephrotic SyndromeDocument3 pagesPharmaceutical Sciences: Recent Advances and Treatments of Childhood Nephrotic SyndromeiajpsNo ratings yet
- Journal Pre-Proof: Clinical Lymphoma, Myeloma and LeukemiaDocument20 pagesJournal Pre-Proof: Clinical Lymphoma, Myeloma and LeukemiaYakobus Antonius SobuberNo ratings yet
- 2881Document7 pages2881Dwi Tantri SPNo ratings yet
- Clinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypeDocument12 pagesClinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypesilviailieNo ratings yet
- Antibiotics 02 00001Document10 pagesAntibiotics 02 00001Jenny AlmagroNo ratings yet
- Art 3A10.1186 2Fcc3188Document174 pagesArt 3A10.1186 2Fcc3188mfhfhfNo ratings yet
- Home Telehealth COPD Study Reduces Healthcare UtilizationDocument10 pagesHome Telehealth COPD Study Reduces Healthcare UtilizationJessyta Benítez OjedaNo ratings yet
- s00432-023-05544-xDocument11 pagess00432-023-05544-xqjhojanjhesielNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document4 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Riri KumalaNo ratings yet
- Rheumatoid Arthritis A Single Center Egyptian Experience CorretedDocument11 pagesRheumatoid Arthritis A Single Center Egyptian Experience CorretedSara EhabNo ratings yet
- Reports of Practical Oncology and Radiotherapy 1 8 (2 0 1 3) S186-S197Document2 pagesReports of Practical Oncology and Radiotherapy 1 8 (2 0 1 3) S186-S197Elisa SalakayNo ratings yet
- Jid 2009113 ADocument9 pagesJid 2009113 AAMELIA.SYAHUTAMINo ratings yet
- Ability of Procalcitonin To Predict Bacterial MeningitisDocument20 pagesAbility of Procalcitonin To Predict Bacterial MeningitisGeorge WinchesterNo ratings yet
- Outcomes of Systemic Lupus Erythematosus in Patients Who DiscontinueDocument7 pagesOutcomes of Systemic Lupus Erythematosus in Patients Who DiscontinueirsyadilfikriNo ratings yet
- Syphilis in Pregnancy - Prevalence at Different Levels of Health Care in DurbanDocument2 pagesSyphilis in Pregnancy - Prevalence at Different Levels of Health Care in DurbanIqaNo ratings yet
- Diagnosis and Features of Hospital-Acquired Pneumonia: A Retrospective Cohort StudyDocument7 pagesDiagnosis and Features of Hospital-Acquired Pneumonia: A Retrospective Cohort Studytitan dheaNo ratings yet
- Encuesta VMP SurvivalDocument5 pagesEncuesta VMP SurvivalMarcelaNo ratings yet
- Guillain-Barré Syndrome: Natural History and Prognostic FactorsDocument7 pagesGuillain-Barré Syndrome: Natural History and Prognostic FactorsAlexandra MardareNo ratings yet
- (2009) Radiographic Improvement and Its Predictors in Patients With Pulmonary TuberculosisDocument6 pages(2009) Radiographic Improvement and Its Predictors in Patients With Pulmonary TuberculosisMohd RahimiNo ratings yet
- Chronic Lymphocytic Leukemia in Young (Comprehensive Analysis of Prognostic Factors and OutcomesDocument40 pagesChronic Lymphocytic Leukemia in Young (Comprehensive Analysis of Prognostic Factors and OutcomesSanti Ayu SNo ratings yet
- Tuberculosis Treatment Outcome Monitoring in England, Wales and Northern Ireland For Cases Reported in 2001Document6 pagesTuberculosis Treatment Outcome Monitoring in England, Wales and Northern Ireland For Cases Reported in 2001A KusyairiNo ratings yet
- Cushing's DiseaseDocument56 pagesCushing's DiseaseDrasmNo ratings yet
- Effect of BMI on complications in thoracic surgeryDocument9 pagesEffect of BMI on complications in thoracic surgeryNoviNo ratings yet
- 1 s2.0 S0360301609016228Document2 pages1 s2.0 S0360301609016228andresNo ratings yet
- Nou 297Document5 pagesNou 297ObamaNo ratings yet
- Shorter Treatment Duration For Selected Patients With Multidrug-Resistant TuberculosisDocument4 pagesShorter Treatment Duration For Selected Patients With Multidrug-Resistant Tuberculosispooja thanekarNo ratings yet
- UntitledDocument26 pagesUntitledAounAbdellahNo ratings yet
- IJMHR: Pneumonia in Diabetics Clinical Profile and OutcomesDocument5 pagesIJMHR: Pneumonia in Diabetics Clinical Profile and OutcomesDanianto WicaksonoNo ratings yet
- 1 s2.0 S2214139123000331 MainDocument6 pages1 s2.0 S2214139123000331 MainHailemariam MebratuNo ratings yet
- PVDI Scientific AbstractsDocument2 pagesPVDI Scientific AbstractsBombinTallerdeTeatroNo ratings yet
- 11 - Manoj Kumar MinjDocument8 pages11 - Manoj Kumar MinjIndah SarihandayaniNo ratings yet
- Cutaneous TB in NigerDocument4 pagesCutaneous TB in NigerRizky ErizkaNo ratings yet
- 33 JMSCRDocument6 pages33 JMSCRVani Junior LoverzNo ratings yet
- Cardiovascular Disease and Its Risk Factors: Frequency in Patients With Chronic Obstructive Pulmonary Disease (COPD)Document5 pagesCardiovascular Disease and Its Risk Factors: Frequency in Patients With Chronic Obstructive Pulmonary Disease (COPD)MJSPNo ratings yet
- Document PDFDocument7 pagesDocument PDFnur fadlilahNo ratings yet
- Tratament of Miastenia GravisDocument9 pagesTratament of Miastenia GravisAndres MardonesNo ratings yet
- Basal Gangila CahngesDocument12 pagesBasal Gangila CahngesJakkani RavikanthNo ratings yet
- The Influence of Body Mass Index On The Long-Term Survival of Patients With Renal Cell Carcinoma After Tumour NephrectomyDocument6 pagesThe Influence of Body Mass Index On The Long-Term Survival of Patients With Renal Cell Carcinoma After Tumour NephrectomyRania AnisNo ratings yet
- j.jalz.2007.10.018Document8 pagesj.jalz.2007.10.018k6fqcwfczfNo ratings yet
- Oncotarget 08 16755Document10 pagesOncotarget 08 16755Ruang GiriNo ratings yet
- Marcadores Sericos para Cole AgudaDocument6 pagesMarcadores Sericos para Cole Agudajessica MárquezNo ratings yet
- Conservative Management and Outcome of Blunt Trauma Abdomen: Original Research ArticleDocument3 pagesConservative Management and Outcome of Blunt Trauma Abdomen: Original Research ArticleBenyamin KalapadangNo ratings yet
- Healthcare UtilisationDocument4 pagesHealthcare UtilisationIvan RomeroNo ratings yet
- HSDC CBC 2015Document5 pagesHSDC CBC 2015Bob sponjaNo ratings yet
- Jof 06 00318Document10 pagesJof 06 00318Robertus RonnyNo ratings yet
- Differences in The Characteristics of Dialysis Patients in Japan Compared With Those in Other CountriesDocument5 pagesDifferences in The Characteristics of Dialysis Patients in Japan Compared With Those in Other CountriesFebyanNo ratings yet
- Scientific Letter: Archivos de Bronconeumología 58 (2022) 520-522Document3 pagesScientific Letter: Archivos de Bronconeumología 58 (2022) 520-522johannaNo ratings yet
- Radiotherapy in Oncological Emergencies Final Results of A Patterns of Care Study in Germany Austria and SwitzerlandDocument10 pagesRadiotherapy in Oncological Emergencies Final Results of A Patterns of Care Study in Germany Austria and SwitzerlandJohnny CshNo ratings yet
- A Randomised Phase II Study of Chemoradiotherapy With or Wi - 2018 - European JoDocument10 pagesA Randomised Phase II Study of Chemoradiotherapy With or Wi - 2018 - European JoFlorin AchimNo ratings yet
- Reviewed FinalDocument10 pagesReviewed FinalTsigereda AberaNo ratings yet
- GuiasddddDocument10 pagesGuiasddddKarla CastilloNo ratings yet
- Guide:Dr - Kadambari Co-Guides:Dr.K.S.Reddy DR - Elangovan Dr. BasuDocument46 pagesGuide:Dr - Kadambari Co-Guides:Dr.K.S.Reddy DR - Elangovan Dr. BasuKishore PriyadharsanNo ratings yet
- Radiologic Findings of PulmonaryDocument6 pagesRadiologic Findings of PulmonaryRiot Riot AdjaNo ratings yet
- 100220080112Document8 pages100220080112Nabil MrhiliNo ratings yet
- Treatmentof Pediatric Acute Lymphoblastic Leukemiaand Recent AdvancesDocument17 pagesTreatmentof Pediatric Acute Lymphoblastic Leukemiaand Recent AdvancesRizkaNo ratings yet
- Makro Skop IsDocument8 pagesMakro Skop IsAbdi Nusa Persada NababanNo ratings yet
- Diameter Luka BakarDocument3 pagesDiameter Luka BakarAbdi Nusa Persada NababanNo ratings yet
- A-V Valves Open Semilunar Valves Closed: Atrial Contraction (Phase 1)Document7 pagesA-V Valves Open Semilunar Valves Closed: Atrial Contraction (Phase 1)Abdi Nusa Persada NababanNo ratings yet
- Macrocarpa (Scheff.) Boerl) AS THE LARVICIDES TOWARDS THIRDDocument9 pagesMacrocarpa (Scheff.) Boerl) AS THE LARVICIDES TOWARDS THIRDAbdi Nusa Persada NababanNo ratings yet
- Case Processing Summary and Descriptive Statistics for MAKROSKOPIS and MIKROSKOPIS DataDocument8 pagesCase Processing Summary and Descriptive Statistics for MAKROSKOPIS and MIKROSKOPIS DataAbdi Nusa Persada NababanNo ratings yet
- Pneumonia in Elderly4Document1 pagePneumonia in Elderly4Abdi Nusa Persada NababanNo ratings yet
- Pneumonia in Elderly4Document1 pagePneumonia in Elderly4Abdi Nusa Persada NababanNo ratings yet
- Lamp IranDocument9 pagesLamp IranAbdi Nusa Persada NababanNo ratings yet
- Pone 0069210 PDFDocument21 pagesPone 0069210 PDFAbdi Nusa Persada NababanNo ratings yet
- Daftar Pustaka: Poisonous Plants. Bogor: Prosea, P. 286-7Document0 pagesDaftar Pustaka: Poisonous Plants. Bogor: Prosea, P. 286-7Abdi Nusa Persada NababanNo ratings yet
- Quality of Care, Process, and Outcomes in Elderly Patients With PneumoniaDocument1 pageQuality of Care, Process, and Outcomes in Elderly Patients With PneumoniaanitacharisNo ratings yet
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Taruhan Europa LeagueDocument1 pageTaruhan Europa LeagueAbdi Nusa Persada NababanNo ratings yet
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)