Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
7 viewsCounselling: E.G.S Missed Miscarriage - Counsel Laparoscopy - Counsel Nuchal Translucency - Councel
Counselling: E.G.S Missed Miscarriage - Counsel Laparoscopy - Counsel Nuchal Translucency - Councel
Uploaded by
SohailKhandental
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You might also like
- Clinical Skills Review: Scenarios Based on Standardized PatientsFrom EverandClinical Skills Review: Scenarios Based on Standardized PatientsRating: 4 out of 5 stars4/5 (10)
- Nac OsceDocument1,089 pagesNac OsceVikrantNo ratings yet
- Nursing Process Lecture NotesDocument16 pagesNursing Process Lecture NotesReden Ocampo100% (17)
- Revision Notes For MRCP 2 PACESDocument356 pagesRevision Notes For MRCP 2 PACESMohd Shuaib Ar0% (1)
- IV WorkbookDocument51 pagesIV WorkbookAndreea Gheorghiu0% (1)
- The Chicago Review Press NCLEX-RN Practice Test and ReviewFrom EverandThe Chicago Review Press NCLEX-RN Practice Test and ReviewRating: 4 out of 5 stars4/5 (20)
- Management of School of NursingDocument35 pagesManagement of School of Nursingkujur mamta100% (1)
- Handouts-IV Therapy Documentation PDFDocument12 pagesHandouts-IV Therapy Documentation PDFTony DemaguilNo ratings yet
- Process of Care and Model of Good CareDocument52 pagesProcess of Care and Model of Good Carekhangsiean89100% (1)
- Cu - Case Study FormatDocument6 pagesCu - Case Study FormatJenny Turado Arbitrario67% (3)
- DocxDocument6 pagesDocxLeo Sandy Ambe CuisNo ratings yet
- D75 14Document8 pagesD75 14JorgeCalvoLara100% (2)
- Fortis AnalysisDocument27 pagesFortis Analysisrahul kNo ratings yet
- Final - MQC Presentation-Standing OrdersDocument29 pagesFinal - MQC Presentation-Standing OrdersElisya Nurri SyaniNo ratings yet
- Osce Top TipsDocument20 pagesOsce Top TipsNeace Dee FacunNo ratings yet
- SOAP Progress NotesDocument11 pagesSOAP Progress NotesShan SicatNo ratings yet
- Questions and Answers for the Specialty Recruitment AssessmentFrom EverandQuestions and Answers for the Specialty Recruitment AssessmentRating: 2 out of 5 stars2/5 (5)
- The AOA Guide:: How To Succeed in The Third-Year ClerkshipsDocument25 pagesThe AOA Guide:: How To Succeed in The Third-Year Clerkshipshector100% (1)
- Tsra Intern Survival Guide 9 12Document44 pagesTsra Intern Survival Guide 9 12johntheuglyllamaNo ratings yet
- SecondCheckingGuidance NorthWestLondonDocument7 pagesSecondCheckingGuidance NorthWestLondonCherryNo ratings yet
- Jobfit Work Fitness Assessment Protocol 230421Document17 pagesJobfit Work Fitness Assessment Protocol 230421Ronni Untung HNo ratings yet
- Nursing ProcessDocument52 pagesNursing ProcessDzon LornaNo ratings yet
- Nursing Documentation, Record Keeping and Written CommunicationDocument14 pagesNursing Documentation, Record Keeping and Written CommunicationAnil PabbaNo ratings yet
- Nursing ProcessDocument14 pagesNursing Processrubycorazon_ediza100% (1)
- The Problem Oriented Medical RecordDocument32 pagesThe Problem Oriented Medical RecordPriscila TanuwidjajaNo ratings yet
- American Association For Medical Transcription 100 Sycamore Avenue, Modesto, CA 95354-0550 - 800-982-2182Document5 pagesAmerican Association For Medical Transcription 100 Sycamore Avenue, Modesto, CA 95354-0550 - 800-982-2182JijoNo ratings yet
- Performance Assessment What You Can ExpectDocument8 pagesPerformance Assessment What You Can ExpectvikrameyeNo ratings yet
- NCP and CNPDocument37 pagesNCP and CNPDen TupasNo ratings yet
- Activity 7.3fDocument4 pagesActivity 7.3fMashaal FasihNo ratings yet
- Busyspr MRCPDocument38 pagesBusyspr MRCPNasir AyubNo ratings yet
- Nicu DoccumentationDocument17 pagesNicu Doccumentationchaarvi100% (1)
- Records and ReportDocument4 pagesRecords and ReportAnusikta PandaNo ratings yet
- EvaluationDocument12 pagesEvaluationapi-338166933No ratings yet
- Case Study FormatDocument6 pagesCase Study FormatMark Jefferson LunaNo ratings yet
- MedicalTemplates Making Medical Documentation Simple and PainlessDocument35 pagesMedicalTemplates Making Medical Documentation Simple and Painlesse-MedTools100% (8)
- Organization Name Occupational Health Service: OrganizatitionaDocument16 pagesOrganization Name Occupational Health Service: OrganizatitionaSA RAINo ratings yet
- Focus Charting 2Document65 pagesFocus Charting 2Ella Caro100% (1)
- 2012 Orthopaedics POMR TemplateDocument5 pages2012 Orthopaedics POMR TemplatecryzallNo ratings yet
- On Going Professional PracticeDocument56 pagesOn Going Professional PracticeAnita Sriwaty PardedeNo ratings yet
- Jobfit Work Fitness Assessment Protocol - May 2016 PDFDocument16 pagesJobfit Work Fitness Assessment Protocol - May 2016 PDFsafiyaNo ratings yet
- Defensible Documentation Quick ReferenceDocument3 pagesDefensible Documentation Quick ReferencecderdnaseNo ratings yet
- Midterms - HA LabDocument17 pagesMidterms - HA LabMa. Daniela De la CernaNo ratings yet
- FAQs 011922Document6 pagesFAQs 011922salyouhaNo ratings yet
- Documentation: VN230 Vocational Nursing Spring 2007Document44 pagesDocumentation: VN230 Vocational Nursing Spring 2007brendz_pontelaNo ratings yet
- Bets - DunningrDocument5 pagesBets - DunningrYhr YhNo ratings yet
- What Is Perinatal Audit?Document5 pagesWhat Is Perinatal Audit?dreamblitzNo ratings yet
- SOAP Notes: HistoryDocument5 pagesSOAP Notes: HistoryRajveerNo ratings yet
- Clerking PatientsDocument7 pagesClerking PatientsJx ChamNo ratings yet
- Resume Joey Takemasa Russell RRT RCPDocument3 pagesResume Joey Takemasa Russell RRT RCPapi-625837402No ratings yet
- Case PresentationDocument15 pagesCase PresentationmaymymayNo ratings yet
- Supportive Supervision Plan & ChecklistsDocument50 pagesSupportive Supervision Plan & ChecklistsJennifer Pearson-Paredes100% (1)
- How To Write A Standard Operating ProcedureDocument3 pagesHow To Write A Standard Operating ProcedureTharj ImamNo ratings yet
- Nausea and Vomiting (Full)Document33 pagesNausea and Vomiting (Full)Kang Opik TaufikNo ratings yet
- Adult Post Operative CareDocument5 pagesAdult Post Operative CareDian Cahyo WibowoNo ratings yet
- Case Study FormatDocument3 pagesCase Study FormatPeter John CaballejosNo ratings yet
- Chanakya - Round 1 CasesDocument12 pagesChanakya - Round 1 CasesAnny MonuNo ratings yet
- The Standard Guidelines (Non-Psych)Document5 pagesThe Standard Guidelines (Non-Psych)Isiakpona AdaNo ratings yet
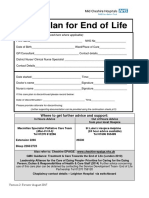
- Care Plan For End of Life Mid Cheshire Hospital Foundation TrustDocument23 pagesCare Plan For End of Life Mid Cheshire Hospital Foundation TrustJoseph HardyNo ratings yet
- Examples of SBARDocument5 pagesExamples of SBARAnonymous C4huq0No ratings yet
- Apss VapDocument14 pagesApss VapRoxanA BocaNo ratings yet
- Bmjopen 2020 039976.reviewer CommentsDocument5 pagesBmjopen 2020 039976.reviewer CommentscderosasNo ratings yet
- Family Nurse Practitioner Certification Exam Premium: 4 Practice Tests + Comprehensive Review + Online PracticeFrom EverandFamily Nurse Practitioner Certification Exam Premium: 4 Practice Tests + Comprehensive Review + Online PracticeNo ratings yet
- Jaypee PublisherDocument20 pagesJaypee PublisherSohailKhanNo ratings yet
- Free Fetal DNA: Prof KhaledDocument15 pagesFree Fetal DNA: Prof KhaledSohailKhanNo ratings yet
- Jaypee PublisherDocument20 pagesJaypee PublisherSohailKhanNo ratings yet
- Pelvic Pain Story of PatientDocument23 pagesPelvic Pain Story of PatientSohailKhanNo ratings yet
- Jaypee PublisherDocument20 pagesJaypee PublisherSohailKhanNo ratings yet
- Jaypee PublisherDocument20 pagesJaypee PublisherSohailKhanNo ratings yet
- Astec1 PDFDocument29 pagesAstec1 PDFSohailKhanNo ratings yet
- Dental DecksDocument84 pagesDental Deckspriyaedwin56% (9)
- Internship Report ON Import Operations of NRB Bank LimitedDocument29 pagesInternship Report ON Import Operations of NRB Bank LimitedRashel MahmudNo ratings yet
- Generate Birth Horoscope, Tamil Jathagam, Tamil Birth Jathakam, South and North Indian Style Horoscope Software PDFDocument4 pagesGenerate Birth Horoscope, Tamil Jathagam, Tamil Birth Jathakam, South and North Indian Style Horoscope Software PDFShanmugam S100% (1)
- Image Processing Using PythonDocument2 pagesImage Processing Using Pythonabhay4meggiNo ratings yet
- Wise Transaction Invoice 288018792 135067666 enDocument2 pagesWise Transaction Invoice 288018792 135067666 enBeytullah UzelNo ratings yet
- ZXDU68 B451 V6.0R20M02 DC Power System Quick Installation GuideDocument7 pagesZXDU68 B451 V6.0R20M02 DC Power System Quick Installation GuideVictor ArticaNo ratings yet
- STIEBEL ELTRON Produktkatalog 2018 VMW Komplett KleinDocument276 pagesSTIEBEL ELTRON Produktkatalog 2018 VMW Komplett KleinsanitermNo ratings yet
- QuestionsDocument49 pagesQuestionsGitika TiwariNo ratings yet
- Compound Interest CalculationDocument2 pagesCompound Interest Calculationbilalak1990No ratings yet
- Switched Reluctance Motors: Control Techniques Using Freescale SolutionsDocument3 pagesSwitched Reluctance Motors: Control Techniques Using Freescale SolutionsHassan SouleymanNo ratings yet
- Induction MotorsDocument179 pagesInduction MotorsMuhammed MifthahNo ratings yet
- Structure of A Flat Hierarchy File For Loading Using A PSADocument6 pagesStructure of A Flat Hierarchy File For Loading Using A PSAapi-3849717No ratings yet
- Lec08. Jquery and AJAX IntroductionDocument64 pagesLec08. Jquery and AJAX IntroductionNixon PeraltaNo ratings yet
- Ermanometry PDFDocument2 pagesErmanometry PDFLakishaNo ratings yet
- Sat. Com (R20) Unit-3Document11 pagesSat. Com (R20) Unit-3kavuri indulakshmiNo ratings yet
- DI Test 76: Archives Forums B-Schools Events MBA VocabularyDocument4 pagesDI Test 76: Archives Forums B-Schools Events MBA VocabularycomploreNo ratings yet
- Midterm s02 SolnsDocument13 pagesMidterm s02 SolnsMuhammad Harun Al RasyidNo ratings yet
- Value Added Tax-Day2Document22 pagesValue Added Tax-Day2Brian Reyes GangcaNo ratings yet
- BonjourDocument23 pagesBonjouramit nigamNo ratings yet
- TLP 521-4Document9 pagesTLP 521-4andrewNo ratings yet
- Professional Engrg in Nigeria-1Document4 pagesProfessional Engrg in Nigeria-1mykekeysNo ratings yet
- Allied Services - 7Document9 pagesAllied Services - 7asaSNo ratings yet
- GU-612 - v3.1 - Guidelines - Incident Investigation and Reporting v1Document185 pagesGU-612 - v3.1 - Guidelines - Incident Investigation and Reporting v1rwerwerw100% (3)
- GV-POE2401 User Manual (POE2401-A-EN)Document48 pagesGV-POE2401 User Manual (POE2401-A-EN)Stiven RomezNo ratings yet
- Alumni Management System Using Android and MYSQLDocument10 pagesAlumni Management System Using Android and MYSQLgayathriNo ratings yet
- 0900 - 1081 - 00 C500 D6 (QSX15G9 With PCC3201)Document2 pages0900 - 1081 - 00 C500 D6 (QSX15G9 With PCC3201)ibrahemNo ratings yet
- Arti Kode Engine: D375A-5 SAA6D170E-3Document17 pagesArti Kode Engine: D375A-5 SAA6D170E-3Akbar WijayaNo ratings yet
- CoP Step by Step Procedures PDFDocument5 pagesCoP Step by Step Procedures PDFThird MateNo ratings yet
Counselling: E.G.S Missed Miscarriage - Counsel Laparoscopy - Counsel Nuchal Translucency - Councel
Counselling: E.G.S Missed Miscarriage - Counsel Laparoscopy - Counsel Nuchal Translucency - Councel
Uploaded by
SohailKhan0 ratings0% found this document useful (0 votes)
7 views10 pagesdental
Original Title
details
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentdental
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
7 views10 pagesCounselling: E.G.S Missed Miscarriage - Counsel Laparoscopy - Counsel Nuchal Translucency - Councel
Counselling: E.G.S Missed Miscarriage - Counsel Laparoscopy - Counsel Nuchal Translucency - Councel
Uploaded by
SohailKhandental
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 10
Counselling
Explain procedure without medical jargon
Use pictures if possible
Interpreter if necessary
Explain benefit and alternatives
Explain serious (death and serious trauma) and frequent risks (infection
+ pain)
Give information leaflet and time to ask questions
E.g.s
Missed miscarriage counsel
Laparoscopy - counsel
Nuchal translucency - councel
ABDOMINAL HYSTERECTOMY FOR HEAVY PERIODS
Audit
A dynamic process that compares clinical practices with a gold standard practice and
possibly suggests change to practice that should be implemented and re-audited to
complete the loop.
1.Standard (RCOG grade A):
2 MARKs
2.EXPLAIN will involve consultant in charge for audit / audit dept / midwives etc to
formulate any other questions / standards to look at with e.g. s
4 marks
3.Then draw up an audit form to fill in (? Use FORMIC software to analyse data sheets)
ask medical records for notes via audit dept if possible. Store notes carefully and extract
information onto the forms pre-prepared.
2 MARKs
Then enter data onto computer / keep data confidential i.e. initials and hosp no only
4.Use Access/excel and powerpoint to present the data and see how measure up to the
standard.
1 MARK
5.Disseminate the recommendations from the audit presentation to all in DEPT and set a
date for the re-audit process / audit cycle.
1 MARK
Standards
Agreed practice
Disseminate
User
Audit
Effect Change
Critical appraisal
Usually a leaflet / patient information
Is it easy to read / non jargon
? simple diagrams
? available in other languages
? does it explain diagnosis / alternative treatments and address pros and cons
does it give a contact number if questions required ?
? who constructed the info leaflet and when will it be updated
Prioritization
Labour ward board
Gynae emergencies and Obs emergencies
Gynae OPD letters and op lists
Make use of all staff and facilities you have available
Midwife can suture episiotomies, put in venflons
SHO may be career SHO ERPCs / assess obstetric patients
Spr ask off going Spr to stay around to help if really busy
Cons ask advice but the examiner wants to know you can prioritise
OPD WHEN TO SEE if suspect cancer 2 WEEK WAIT RULE
URGENT Vs routine
Op lists consultant should really be present
Risk management
How to reduce clinical risk (CNST)
LEVEL 1 10%
LEVEL 2 20%
LEVEL 3 30%
Fill in clinical risk forms
How to make a protocol / guideline
Set format see e.g.
Evidence based (NICE or RCOG)
Review date
Essex Rivers Healthcare NHS Trust
Directorate of Women, Children and Families
Maternity Services
Title of Guideline
Introduction Aims and objectives etc
Body
Structured and progressive framework
Clinical guidelines may be in Table format- including a column for the ACTION and a
column for the RATIONALE but alternatively may be in bullet points
All headings as section breaks
Action
Rationale
Put up IV fluid To maintain circulating volume
References
Harvard referencing (instructions to follow on Harvard System)
As agreed by Obstetric Division (if it is a medical issue)
Head of Midwifery (if it is a midwifery issue only)
------------------------------------------- ---------------------------------------
Anne Ferris Consultant Obstetrician
Head of Midwifery Lead Consultant Delivery Suite
If non medical signed by Head of Midwifery
Date of guideline: (Month and Year)
Review date: (usually 3years later, Month and Year)
Compiled by:
You might also like
- Clinical Skills Review: Scenarios Based on Standardized PatientsFrom EverandClinical Skills Review: Scenarios Based on Standardized PatientsRating: 4 out of 5 stars4/5 (10)
- Nac OsceDocument1,089 pagesNac OsceVikrantNo ratings yet
- Nursing Process Lecture NotesDocument16 pagesNursing Process Lecture NotesReden Ocampo100% (17)
- Revision Notes For MRCP 2 PACESDocument356 pagesRevision Notes For MRCP 2 PACESMohd Shuaib Ar0% (1)
- IV WorkbookDocument51 pagesIV WorkbookAndreea Gheorghiu0% (1)
- The Chicago Review Press NCLEX-RN Practice Test and ReviewFrom EverandThe Chicago Review Press NCLEX-RN Practice Test and ReviewRating: 4 out of 5 stars4/5 (20)
- Management of School of NursingDocument35 pagesManagement of School of Nursingkujur mamta100% (1)
- Handouts-IV Therapy Documentation PDFDocument12 pagesHandouts-IV Therapy Documentation PDFTony DemaguilNo ratings yet
- Process of Care and Model of Good CareDocument52 pagesProcess of Care and Model of Good Carekhangsiean89100% (1)
- Cu - Case Study FormatDocument6 pagesCu - Case Study FormatJenny Turado Arbitrario67% (3)
- DocxDocument6 pagesDocxLeo Sandy Ambe CuisNo ratings yet
- D75 14Document8 pagesD75 14JorgeCalvoLara100% (2)
- Fortis AnalysisDocument27 pagesFortis Analysisrahul kNo ratings yet
- Final - MQC Presentation-Standing OrdersDocument29 pagesFinal - MQC Presentation-Standing OrdersElisya Nurri SyaniNo ratings yet
- Osce Top TipsDocument20 pagesOsce Top TipsNeace Dee FacunNo ratings yet
- SOAP Progress NotesDocument11 pagesSOAP Progress NotesShan SicatNo ratings yet
- Questions and Answers for the Specialty Recruitment AssessmentFrom EverandQuestions and Answers for the Specialty Recruitment AssessmentRating: 2 out of 5 stars2/5 (5)
- The AOA Guide:: How To Succeed in The Third-Year ClerkshipsDocument25 pagesThe AOA Guide:: How To Succeed in The Third-Year Clerkshipshector100% (1)
- Tsra Intern Survival Guide 9 12Document44 pagesTsra Intern Survival Guide 9 12johntheuglyllamaNo ratings yet
- SecondCheckingGuidance NorthWestLondonDocument7 pagesSecondCheckingGuidance NorthWestLondonCherryNo ratings yet
- Jobfit Work Fitness Assessment Protocol 230421Document17 pagesJobfit Work Fitness Assessment Protocol 230421Ronni Untung HNo ratings yet
- Nursing ProcessDocument52 pagesNursing ProcessDzon LornaNo ratings yet
- Nursing Documentation, Record Keeping and Written CommunicationDocument14 pagesNursing Documentation, Record Keeping and Written CommunicationAnil PabbaNo ratings yet
- Nursing ProcessDocument14 pagesNursing Processrubycorazon_ediza100% (1)
- The Problem Oriented Medical RecordDocument32 pagesThe Problem Oriented Medical RecordPriscila TanuwidjajaNo ratings yet
- American Association For Medical Transcription 100 Sycamore Avenue, Modesto, CA 95354-0550 - 800-982-2182Document5 pagesAmerican Association For Medical Transcription 100 Sycamore Avenue, Modesto, CA 95354-0550 - 800-982-2182JijoNo ratings yet
- Performance Assessment What You Can ExpectDocument8 pagesPerformance Assessment What You Can ExpectvikrameyeNo ratings yet
- NCP and CNPDocument37 pagesNCP and CNPDen TupasNo ratings yet
- Activity 7.3fDocument4 pagesActivity 7.3fMashaal FasihNo ratings yet
- Busyspr MRCPDocument38 pagesBusyspr MRCPNasir AyubNo ratings yet
- Nicu DoccumentationDocument17 pagesNicu Doccumentationchaarvi100% (1)
- Records and ReportDocument4 pagesRecords and ReportAnusikta PandaNo ratings yet
- EvaluationDocument12 pagesEvaluationapi-338166933No ratings yet
- Case Study FormatDocument6 pagesCase Study FormatMark Jefferson LunaNo ratings yet
- MedicalTemplates Making Medical Documentation Simple and PainlessDocument35 pagesMedicalTemplates Making Medical Documentation Simple and Painlesse-MedTools100% (8)
- Organization Name Occupational Health Service: OrganizatitionaDocument16 pagesOrganization Name Occupational Health Service: OrganizatitionaSA RAINo ratings yet
- Focus Charting 2Document65 pagesFocus Charting 2Ella Caro100% (1)
- 2012 Orthopaedics POMR TemplateDocument5 pages2012 Orthopaedics POMR TemplatecryzallNo ratings yet
- On Going Professional PracticeDocument56 pagesOn Going Professional PracticeAnita Sriwaty PardedeNo ratings yet
- Jobfit Work Fitness Assessment Protocol - May 2016 PDFDocument16 pagesJobfit Work Fitness Assessment Protocol - May 2016 PDFsafiyaNo ratings yet
- Defensible Documentation Quick ReferenceDocument3 pagesDefensible Documentation Quick ReferencecderdnaseNo ratings yet
- Midterms - HA LabDocument17 pagesMidterms - HA LabMa. Daniela De la CernaNo ratings yet
- FAQs 011922Document6 pagesFAQs 011922salyouhaNo ratings yet
- Documentation: VN230 Vocational Nursing Spring 2007Document44 pagesDocumentation: VN230 Vocational Nursing Spring 2007brendz_pontelaNo ratings yet
- Bets - DunningrDocument5 pagesBets - DunningrYhr YhNo ratings yet
- What Is Perinatal Audit?Document5 pagesWhat Is Perinatal Audit?dreamblitzNo ratings yet
- SOAP Notes: HistoryDocument5 pagesSOAP Notes: HistoryRajveerNo ratings yet
- Clerking PatientsDocument7 pagesClerking PatientsJx ChamNo ratings yet
- Resume Joey Takemasa Russell RRT RCPDocument3 pagesResume Joey Takemasa Russell RRT RCPapi-625837402No ratings yet
- Case PresentationDocument15 pagesCase PresentationmaymymayNo ratings yet
- Supportive Supervision Plan & ChecklistsDocument50 pagesSupportive Supervision Plan & ChecklistsJennifer Pearson-Paredes100% (1)
- How To Write A Standard Operating ProcedureDocument3 pagesHow To Write A Standard Operating ProcedureTharj ImamNo ratings yet
- Nausea and Vomiting (Full)Document33 pagesNausea and Vomiting (Full)Kang Opik TaufikNo ratings yet
- Adult Post Operative CareDocument5 pagesAdult Post Operative CareDian Cahyo WibowoNo ratings yet
- Case Study FormatDocument3 pagesCase Study FormatPeter John CaballejosNo ratings yet
- Chanakya - Round 1 CasesDocument12 pagesChanakya - Round 1 CasesAnny MonuNo ratings yet
- The Standard Guidelines (Non-Psych)Document5 pagesThe Standard Guidelines (Non-Psych)Isiakpona AdaNo ratings yet
- Care Plan For End of Life Mid Cheshire Hospital Foundation TrustDocument23 pagesCare Plan For End of Life Mid Cheshire Hospital Foundation TrustJoseph HardyNo ratings yet
- Examples of SBARDocument5 pagesExamples of SBARAnonymous C4huq0No ratings yet
- Apss VapDocument14 pagesApss VapRoxanA BocaNo ratings yet
- Bmjopen 2020 039976.reviewer CommentsDocument5 pagesBmjopen 2020 039976.reviewer CommentscderosasNo ratings yet
- Family Nurse Practitioner Certification Exam Premium: 4 Practice Tests + Comprehensive Review + Online PracticeFrom EverandFamily Nurse Practitioner Certification Exam Premium: 4 Practice Tests + Comprehensive Review + Online PracticeNo ratings yet
- Jaypee PublisherDocument20 pagesJaypee PublisherSohailKhanNo ratings yet
- Free Fetal DNA: Prof KhaledDocument15 pagesFree Fetal DNA: Prof KhaledSohailKhanNo ratings yet
- Jaypee PublisherDocument20 pagesJaypee PublisherSohailKhanNo ratings yet
- Pelvic Pain Story of PatientDocument23 pagesPelvic Pain Story of PatientSohailKhanNo ratings yet
- Jaypee PublisherDocument20 pagesJaypee PublisherSohailKhanNo ratings yet
- Jaypee PublisherDocument20 pagesJaypee PublisherSohailKhanNo ratings yet
- Astec1 PDFDocument29 pagesAstec1 PDFSohailKhanNo ratings yet
- Dental DecksDocument84 pagesDental Deckspriyaedwin56% (9)
- Internship Report ON Import Operations of NRB Bank LimitedDocument29 pagesInternship Report ON Import Operations of NRB Bank LimitedRashel MahmudNo ratings yet
- Generate Birth Horoscope, Tamil Jathagam, Tamil Birth Jathakam, South and North Indian Style Horoscope Software PDFDocument4 pagesGenerate Birth Horoscope, Tamil Jathagam, Tamil Birth Jathakam, South and North Indian Style Horoscope Software PDFShanmugam S100% (1)
- Image Processing Using PythonDocument2 pagesImage Processing Using Pythonabhay4meggiNo ratings yet
- Wise Transaction Invoice 288018792 135067666 enDocument2 pagesWise Transaction Invoice 288018792 135067666 enBeytullah UzelNo ratings yet
- ZXDU68 B451 V6.0R20M02 DC Power System Quick Installation GuideDocument7 pagesZXDU68 B451 V6.0R20M02 DC Power System Quick Installation GuideVictor ArticaNo ratings yet
- STIEBEL ELTRON Produktkatalog 2018 VMW Komplett KleinDocument276 pagesSTIEBEL ELTRON Produktkatalog 2018 VMW Komplett KleinsanitermNo ratings yet
- QuestionsDocument49 pagesQuestionsGitika TiwariNo ratings yet
- Compound Interest CalculationDocument2 pagesCompound Interest Calculationbilalak1990No ratings yet
- Switched Reluctance Motors: Control Techniques Using Freescale SolutionsDocument3 pagesSwitched Reluctance Motors: Control Techniques Using Freescale SolutionsHassan SouleymanNo ratings yet
- Induction MotorsDocument179 pagesInduction MotorsMuhammed MifthahNo ratings yet
- Structure of A Flat Hierarchy File For Loading Using A PSADocument6 pagesStructure of A Flat Hierarchy File For Loading Using A PSAapi-3849717No ratings yet
- Lec08. Jquery and AJAX IntroductionDocument64 pagesLec08. Jquery and AJAX IntroductionNixon PeraltaNo ratings yet
- Ermanometry PDFDocument2 pagesErmanometry PDFLakishaNo ratings yet
- Sat. Com (R20) Unit-3Document11 pagesSat. Com (R20) Unit-3kavuri indulakshmiNo ratings yet
- DI Test 76: Archives Forums B-Schools Events MBA VocabularyDocument4 pagesDI Test 76: Archives Forums B-Schools Events MBA VocabularycomploreNo ratings yet
- Midterm s02 SolnsDocument13 pagesMidterm s02 SolnsMuhammad Harun Al RasyidNo ratings yet
- Value Added Tax-Day2Document22 pagesValue Added Tax-Day2Brian Reyes GangcaNo ratings yet
- BonjourDocument23 pagesBonjouramit nigamNo ratings yet
- TLP 521-4Document9 pagesTLP 521-4andrewNo ratings yet
- Professional Engrg in Nigeria-1Document4 pagesProfessional Engrg in Nigeria-1mykekeysNo ratings yet
- Allied Services - 7Document9 pagesAllied Services - 7asaSNo ratings yet
- GU-612 - v3.1 - Guidelines - Incident Investigation and Reporting v1Document185 pagesGU-612 - v3.1 - Guidelines - Incident Investigation and Reporting v1rwerwerw100% (3)
- GV-POE2401 User Manual (POE2401-A-EN)Document48 pagesGV-POE2401 User Manual (POE2401-A-EN)Stiven RomezNo ratings yet
- Alumni Management System Using Android and MYSQLDocument10 pagesAlumni Management System Using Android and MYSQLgayathriNo ratings yet
- 0900 - 1081 - 00 C500 D6 (QSX15G9 With PCC3201)Document2 pages0900 - 1081 - 00 C500 D6 (QSX15G9 With PCC3201)ibrahemNo ratings yet
- Arti Kode Engine: D375A-5 SAA6D170E-3Document17 pagesArti Kode Engine: D375A-5 SAA6D170E-3Akbar WijayaNo ratings yet
- CoP Step by Step Procedures PDFDocument5 pagesCoP Step by Step Procedures PDFThird MateNo ratings yet