Professional Documents
Culture Documents
Kuliah 1 HHD Hipertensi
Uploaded by
Dita Wahyu RahmanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Kuliah 1 HHD Hipertensi
Uploaded by
Dita Wahyu RahmanCopyright:
Available Formats
Hypertension Heart Disease
APEKS:SIC V
Mid claviculer
The World Health Organization (WHO)
estimates that 20% of the worlds
current adult population has
hypertension
Prevalence of hypertension
Awareness, Treatment and Control of
High Blood Pressure in Canada
Patients unaware of their high blood pressure 43%
Aware but not treated and not controlled 22%
Treated but not controlled 21%
Treated and controlled 13%
Joffres et al. Am J Hypertens 2001; 14(11):1099-1105
43%
22%
21%
13%
Trends in the awareness, treatment and
control of hypertension in the U.S.
Awareness 51.0% 73.0% 68.4%
Treated 31.0% 55.0% 53.6%
Controlled 10.0% 29.0% 27.6%
NHANES II
1976-80
NHANES III
(Phase I)
1988-91
NHANES III
(Phase II)
1991-94
Controlled BP = SBP <140 mmHg and DBP <90 mmHg
Adapted from Burt et al. 1995
Causes of Resistant Hypertension
Efficacy of
medications
Patient compliance:
Side effects
Convenience
Lack of symptoms
Patient education
Cost
Failure to treat to
target
MD Reluctance
Accurate blood pressure
measurements
Secondary Causes
Sleep apnea
Renal vascular HTN
Endocrine causes
Chronic renal failure
Rx Drugs (NSAIDS, steroids)
White-coat HTN
Pseudo-hypertension
Vasoactive substances
(non-Rx)
Relctnce: enggan Rstant : mlawan
Diseases Attributable to Hypertension
Hypertension
Heart failure
Stroke
Coronary heart disease
Myocardial infarction
Left ventricular
hypertrophy
Aortic aneurysm
Retinopathy
Peripheral vascular disease
Hypertensive
encephalopathy
Chronic kidney failure
Cerebral hemorrhage
All
Vascular
Adapted from: Dustan et al. Arch Intern Med 1996; 156:1926-1935
Hypertension Optimal Treatment (HOT) study
9.9
10.0
9.3
24.4
18.6
11.9
0
5
10
15
20
25
30
90 mmHg 85 mmHg 80 mmHg
Target DBP group
Major CV
events per
1000 patient
years
All patients (n=18 790)
Diabetics (n=1501)
Lancet 1998;351:17551762
Intensive BP-lowering decreases cardiovascular risk in patients with
hypertension, especially among those with diabetes
UKPDS: relative risk reduction with tight
versus less tight blood pressure control
Any diabetes-
related endpoint
Diabetes-related
deaths
Stroke Microvascular
disease
24% P<0.005
32% P<0.05
44% P<0.05
37% P<0.01
Tight control (n=758)
Less tight control (n=390)
Deterioration in
visual acuity
47% P<0.005
BMJ 1998;317:703713
Tight BP control decreases morbidity and mortality in patients with diabetes
BP targets
BP targets in guidelines are becoming
more stringent
Coexistent cardiovascular risk factor
profile is important
The relationship between BP and mortality
is not dictated by a J-shaped curve
Strngt : ktat,kras
Initial Assessment
Target organ damage
Overall cardiovascular risk
Rule out secondary and often curable
causes
Target end-organs should be assessed
by history and physical examination
Components of Risk Stratification
Target Organ Damage/Clinical Cardiovascular Disease
Brain
Heart
Kidneys
Eyes
Arteries
Adapted from: JNC VI. Arch Intern Med 1997;157: 2413-46
Components of Risk Stratification
Major Cardiovascular Risk Factors
Hypertension
Age
Smoking
Dyslipidemia
Diabetes
Family history
Obesity
> 45 years Male
> 55 years Female (Postmenopausal)
CAD <65 Female
CAD <55 Male
Adapted from: JNC VI. Arch Intern Med 1997;157: 2413-46
14
Stratification of risk to quantity prognosis
Other risk factor and
disease history
Normal
SBP 120-
129
DBP 80-84
High normal
SBP 130-
139
DBP 85-89
Grade 1
SBP140-
159
DBP 90-99
Grade 2
SBP 160-
179
DBP 100-
109
Grade 3
SBP > 180
DBP >
110
No other risk factors Average
risk
Average
risk
Low added
risk
Moderate
added risk
High
added risk
1 2 risk factors Low added
risk
Low added
risk
Moderate
added risk
Moderate
added risk
Very high
added risk
3 or more risk factors or
TOD or DM
Moderate
added risk
High added
risk
High added
risk
High added
risk
Very high
added risk
ACC High added
risk
Very high
added risk
Very high
added risk
Very high
added rsik
Very
added risk
Blood pressure (mm Hg)
2003 ESH-ESC
Effectively reduces BP
Maintains BP control over 24 h with
once-a-day dosing
Effective in all hypertensive patients
No adverse effects
No negative metabolic side effects
Affordable
The ideal antihypertensive agent
Persistent use of monotherapy
Obsession with first line therapy
Poor recognition of the importance and efficacy
of combination therapy
Lack of advice on most appropriate drugs to
use in combination
BP monotherapy: BP fall <10%
Statin therapy: Cholesterol fall 30-40%
Clinical Practice:
Most people with hypertension are treated with monotherapy
Clinical Evidence:
Most people in clinical trials are treated with combination
therapy
HOT: percentage of patients requiring
combination therapy to achieve target DBP
90 mmHg
37.1%
62.9%
85 mmHg
31.7%
68.3%
80 mmHg
26.1%
73.9%
Combination therapy
Monotherapy
Target DBP group
The lower the target DBP, the greater the need for combination therapy
HOT:Hypertesion Optimal Treatment
Advantages of combination therapy
Additive antihypertensive efficacy (due to
complementary mechanisms of action)
Higher patient response rates
Simple titration and dosing schedules
Maintained or improved tolerability
Improved patient compliance
Cost effective
Drug Action
- vasodilatation
RAS Activation
SNS Activation
-Vasoconstriction
- Sodium retention
RAS = renin-angiotensin system
SNS = sympathetic nervous system
24
Thiazide
Lowers Blood
Pressure
Natriuretic
Activates
Renin Angiotensin
System
Reduces antihypertensive effect
25
Reduce Adverse Effects of Drug Therapy:
ACE inhibition or
Angiotensin Receptor Blockers
Retain potassium
Thiazide
Diuretics
Excrete Potassium
Combination
Prevents hypokalaemia of thiazide therapy
Limits hyperkalaemia of RAS(r angt sys) blockade
26
27
28
29
WHAT IS THE IDEAL WAY OF CONTROLLING BP?
The new therapeutic window in hypertension
100
80
60
40
20
0
100
80
60
40
20
0
Efficacy (%)
Freedom from
side effects (%)
Dose
Man Int Veld AJ. J Hypert, 1997
IDEAL treatment
Traditional
30
31
32
ACE-I = angiotensin-converting enzyme inhibitor; ARB = angiotensin-receptor blocker;
BB = beta blocker; CCB, = calcium channel blocker.
Chobanian AV et al. JAMA. 2003;289:2560-2572.
Drug(s) for the compelling
indications; other
antihypertensive drugs
(diuretics, ACE-I, ARB,
BB, CCB) as needed
Drug(s) for the compelling
indications; other
antihypertensive drugs
(diuretics, ACE-I, ARB, BB,
CCB) as needed
BP Classification
Lifestyle
Modification
Initial Drug Therapy
Without Compelling
Indication
With Compelling
Indication
Normal
<120/80 mm Hg
Prehypertension
120-139/80-89 mm Hg
Stage 1 hypertension
140-159/90-99 mm Hg
Stage 2 hypertension
160/100 mm Hg
Encourage
Yes
Yes
Yes
No drug indicated Drug(s) for the compelling
indications
Thiazide-type diuretics
for most; may consider
ACE-I, ARB, BB, CCB, or
combination
2-drug combination for most
(usually thiazide-type diuretic
and ACE-I, ARB, BB, or
CCB)
33
BP target of <140/90 mm Hg for patients with uncomplicated
hypertension without compelling indications
BP target of <130/80 mm Hg for patients with diabetes
Combinations of 2 or more drugs are usually needed
to achieve target BP goal
BP target of <130/80 mm Hg for patients with chronic renal
disease*
Combinations of 3 or more drugs are often needed
to reach target BP goal
*Chronic kidney disease = GFR <60 mL/min per 1.73 m
2
or presence of albuminuria
(>300 mg/d or 200 mg/g creatinine).
Chobanian AV et al. JAMA. 2003;289:2560-2572.
American Diabetes Association. Diabetes Care. 2003;26(Suppl 1):S33-S50.
Guidelines Committee. J Hypertens. 2003;21:1011-1053.
34
Most patients with hypertension will require 2 or
more antihypertensive drugs to achieve BP goals
According to baseline BP and presence or absence
of complications, therapy can be initiated either
with a low dose of a single agent or with a low-dose
combination of 2 agents
When BP is >20/10 mm Hg above goal,
consideration should be given to initiating 2 drugs,
either as separate prescriptions or in fixed-dose
combinations, one of which should be a thiazide-
type diuretic
Chobanian AV et al. JAMA. 2003;289:2560-2572.
Guidelines Committee. J Hypertens. 2003;21:1011-1053.
35
Easy as ABC D
A = ACE-Inhibitor or Angiotensin Receptor Blocker
B = - Blocker
C = Calcium Channel Blocker
D = Diuretic (thiazide)
Adapted from : Better blood pressure control: how to combine drugs
Journal of Human Hypertension (2003) 17, 81-86 www.bhsoc.org
36
A or B
Inhibit the
Renin-Angiotensin
System
C or D
Do not inhibit the
Renin-Angiotensin
System
More Effective
In Younger
More Effective
In Older
Adapted from : Better blood pressure control: how to combine drugs
Journal of Human Hypertension (2003) 17, 81-86 www.bhsoc.org
Younger
Or Diabetes
( 55yrs)
Older
(55yrs)
or Black
A or B C or D
1.
A or (B) + C or D
2.
A or (B) + C + D
3.
A or (B) + C + D + other 4.
Adapted from : Better blood pressure control: how to combine drugs
Journal of Human Hypertension (2003) 17, 81-86 www.bhsoc.org
38
39
Recommended Combinations
1. ACE inhibitors / AIIRA Diuretics
2. ACE inhibitors / AIIRA Calcium antagonists
3. ACE inhibitors / AIIRA Beta-blockers
(Special condition)
4. Beta-Blockers Diuretics
5. Beta-Blockers Calcium Antagonists
SUMMARY
COMBINATION THERAPY IN HTN
MANAGEMENT IS LOGIC AND
EVIDENCE BASED
MAXIMIZE EFFECT, MINIMIZE SIDE
EFFECT
COMBINATION THERAPY IN HTN
INCREASE COMPLIANCE
THE END
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Kuliah 1 HHD HipertensiDocument41 pagesKuliah 1 HHD HipertensiDita Wahyu RahmanNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Kuliah 1 Hiv, Aids, OpportDocument61 pagesKuliah 1 Hiv, Aids, OpportDita Wahyu RahmanNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Islam Perspective On Heart DiseaseDocument39 pagesIslam Perspective On Heart DiseaseDita Wahyu RahmanNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
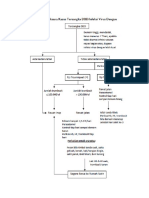
- Pathway DF DHFDocument4 pagesPathway DF DHFDita Wahyu RahmanNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Kuliah 1 HHD HipertensiDocument41 pagesKuliah 1 HHD HipertensiDita Wahyu RahmanNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Curriculum PhysicsDocument4 pagesThe Curriculum PhysicsDita Wahyu RahmanNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Stroke 2010 Bath 732 8Document8 pagesStroke 2010 Bath 732 8Dita Wahyu RahmanNo ratings yet
- Ce 15403Document18 pagesCe 15403Dita Wahyu RahmanNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Kuliah 1 HHD HipertensiDocument41 pagesKuliah 1 HHD HipertensiDita Wahyu RahmanNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Growth Chart For Boys Birth To 36 MonthsDocument2 pagesGrowth Chart For Boys Birth To 36 MonthsCarlos TejedaNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Stroke 2010 Bath 732 8Document8 pagesStroke 2010 Bath 732 8Dita Wahyu RahmanNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Stroke 2010 Hassan 1673 8Document7 pagesStroke 2010 Hassan 1673 8Dita Wahyu RahmanNo ratings yet
- Topic Tree EmergenciesDocument1 pageTopic Tree EmergenciesDita Wahyu RahmanNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- CDC-wfa Boys 2 To 20 YearsDocument1 pageCDC-wfa Boys 2 To 20 YearsDita Wahyu RahmanNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- CDC-wfa Girls Birth To 36 MonthDocument1 pageCDC-wfa Girls Birth To 36 MonthDita Wahyu RahmanNo ratings yet
- UII Gram Pos Spore-FormDocument30 pagesUII Gram Pos Spore-FormDita Wahyu RahmanNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Kuliah 1 HHD HipertensiDocument41 pagesKuliah 1 HHD HipertensiDita Wahyu RahmanNo ratings yet
- Evidence Based Medicine 0705Document32 pagesEvidence Based Medicine 0705Dita Wahyu RahmanNo ratings yet
- Brain Death AdultsDocument4 pagesBrain Death AdultsTcacolate Telsa ElizsabethNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)