Professional Documents
Culture Documents
Blood Disorders: Minerva A. Cobus
Blood Disorders: Minerva A. Cobus
Uploaded by
matrixtrinityOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Blood Disorders: Minerva A. Cobus
Blood Disorders: Minerva A. Cobus
Uploaded by
matrixtrinityCopyright:
Available Formats
BLOOD DISORDERS
Minerva A. Cobus
Overview of
Hematological System
Bone Marrow
Contained inside of the bone,
occupies interior of spongy and
center of long bones
4-5% of total body weight
Primary function is Hematopoiesis-
formation of blood cells
Bone Marrow
2 kinds:
a. Red marrow (functioning)
a. Carries out hematopoiesis
b. Found in ribs, vertebral column, other flat
bones
b. Yellow marrow
a. Red marrow that has changed to fat;
found in long bones
b. Does not contribute to hematopoiesis
Blood
Composed of plasma (55%) and
cellular components (45%)
Hematocrit
a. reflects portion of blood composed of
RBC
Plasma
Liquid part of blood; yellow in color
Consist of serum (liquid portion of
plasma) and fibrinogen
Contains plasma proteins such as:
a. Albumin: largest plasma proteins,
involve in regulation of intravascular
plasma volume and maintenance of
osmotic pressure
Plasma
b. Serum globulins:
a. Alpha role in transport of steroids, lipids,
bilirubin
b. Beta: role in transport of iron and copper
c. Gamma: role in immune response,
function of antibodies
c. Fibrinogen, prothrombin, plasminogen-
for coagulation
Cellular Components
Erythrocytes RBCs responsible for
oxygen transport
Normal 12-18 g Hgb/100cc blood;
men- 14-18 g; women 12-14g
Average life span- 120 days
Leukocytes- protection from bacteria
and other foreign substances
Cellular Components
Thrombocytes essential factor in
coagulation via adhesion,
aggregation, and plug formation
Diagnostic Test
Blood
Complete CBC: WBC; Hgb and Hct;
platelet and reticulocyte count
Coagulation studies: PT; PTT; (FSP)
fibrin split products; Lee-white clotting
(whole blood clotting time)
Blood Chemistry: BUN; creatinine; uric
acid
Urine and stool
Urinalysis
Hematest
Bence-Jones protein assay (urine)
Radiologic
Chest x-ray
Radionuclide scans (bone scan)
Bone marrow aspiration and biopsy
Puncture of the iliac crest (preferred
site), vertebrae body, sternum, or tibia
(in infants) to collect tissue from bone
marrow
Purpose: study cells involved in blood
production
Nursing care:
Confirm consent
Allay anxiety
Position client and assist physician to
maintain sterile field
Immediately after aspiration, apply
pressure to the site for at least 5
minutes and longer, if necessary
Send specimen to the laboratory.
Sickle Cell test
Sickledex
No hemoglobin S present
Routine screening test for cell, trait
or disorder; does not distinguish
between them
Hemoglobin Electrophoresis
Separates various hemoglobins and
allows for identification of specific
problem
Differentiates between traitor
disorder in sickle cell anemia
Diagnosis of thalassemia and
hemolytic anemia
Fibrin Split Products
Fibrinolysis occurs in intravascular
coagulation
Abnormally high levels in DIC
Schilling Test
Normal excretion is 10-40% of oral
dose of the radioactive B12
Stage 1-is a 24-hour urine test after
a dose of radio labeled B12
Stage 2-is a second 24-hour urine to
determine response to intrinsic
factor; distinguishes between
pernicious anemia and
malabsorption.
BLOOD COMPONENT
THERAPY
Plasma Components and
Products
Consist of:
Fresh frozen plasma
Cryoprecipitate
Fresh Frozen Plasma
Plasma which is separated from whole
blood and frozen within 6 hours of
phlebotomy.
Content:
-plasma protein
-all coagulation factors ( include labile F V
+ F VIII)
Storage and shelf life:
- storage at -18C
- deep freeze at -40C can be kept for 2
year
FFP
Properties:
-1 unit volume: 200 ml
- pediatric : 50-100 ml
Administration :
- thawed in 37C water bath
- administer within half an hour after
thawing
( activity of labile F V, V III is rapidly
lost)
FFP
Definite indications:
1) Replacement for isolated factor
deficiencies (specific factor not available
eg: F V)
2) Immediate reversal warfarin effect.
3) Replacement of coagulation factors in:
DIVC.
4) Inherited def of inhibitors of coagulation
eg: Anti thrombin III, protein C, protein S.
FFP
Conditional uses (FFP only indicated in
the presence of bleeding and disturbed
coagulation):
- Massive transfusion
- Liver disease
- Cardiopulmonary bypass surgery
- Special pediatric indications eg: severe
sepsis
FFP
Contraindication:
- estimated as many 73% are used without
justification
- 1) volume expander
- 2) nutritional source of protein +
immunoglobulin
- 3) Urticaria + anaphylactoid reaction or
previous severe reaction to plasma
FFP
Dose + Administration:
- ABO compatible with recipient blood cell
+ without regard to Rh type
- Cross matching not required
- Amount used depend on clinical situation
eg: DIVC case: 2 units for adult
paediatric: 10-20 mls /kg
- efficacy assessed with PT, aPTT
Platelets
Will raise recipient's platelet count by
10,000 u/liter
Pooled from 4-8 units of whole blood
Albumin Preparation
Protein solution containing
predominantly albumin prepared by
fractionation of large pools of
plasma.
Properties:
1) Albumin solution
2) Plasma protein fraction
Albumin solution
Available in 5% and 25% solution.
Contain 96% albumin and 4% globulin +
other plasma protein.
Pooled plasma product and is heat treated
to inactivate viral activity.
5% solution: osmotically + oncotically
equivalent to plasma
25% solution; markedly hyperoncotic.
Shelf life: 5 years at 2-10C.
Plasma Protein Fraction
Prepared the same manner as
albumin.
Differences: albumin content 80 to
85%
Stored at room temperature for 3
years or at 1-6C for 5 years.
Administration:
- albumin + PPF do not contain ABO
antigen or Ab compatibility not
required
Albumin preparation
Indication (both):
Volume expansion and colloid replacement
for patients in hypovolemic shock, burn,
undergoing retroperitoneal surgery in
which large volume of protein-rich fluid
may pool in the bowel.
Indication for PPF: parallel those for 5%
albumin.
Albumin solution not indicated to correct
nutritional def (enteric, parenteral,
hyperalimentation > appropriate)
Factor VIII Concentrate
FVIII concentrate or antihemophilic
Factor (AHF) specific treatment for
F VIII def (hemophilia A)
Prepared fr large donor pools of
plasma
Pooled plasma is fractionated ,
lyophilized + stored at 1-6C
Heat treated to reduce risk of
transfusion transmitted disease.
Factor IX Concentrate
2 heat treated , lyophilized
concentrates of F IX:
1) Factor IX complex
2) Pure Factor IX concentrate
F IX complex (Prothrombin
complex) Contain factor II, VII,
IX and X
F IX concentrate: contain 20-30 %
F IX, trace amount of F II, VII, X.
Factor IX concentrate
Indication:
1) Hemophilia B
2) Haemophilia A with inhibitors
Contraindication:
-Fac IX complex a/w thromboses and
episode of DIC.
- Adverse effect also seen in
Haemophilia A with inhibitors
Autologous Transfusion
Therapeutic benefit:
1) Safe (risk of TTD eliminated)
2) No alloimmunization
Conserves blood banks limited
homologous blood supply
Either be:
1) Perioperative Hemodilution
2) Intraoperative Salvage
3) Postoperative Blood Salvage
Perioperative Hemodilution
Eg: Cardiopulmonary bypass surgery
Withdraw 1/> units of blood
preoperatively + replace with crystalloid /
colloid solution normovolemic,
hemodiluted state
Results in improved blood flow in pt
circulation + loss of < red cell
Labelled properly (pt name, RN,date/time
phlebotomy)
Reinfuse within 8 hr: reliable source of plt,
coag factors.
Intraoperative Salvage
Blood-containing fluid aspirated fr op
site, centrifuge or washed and reinfused
through a filter during op/post op.
Vascular procedure large amount of
blood pool in body cavities.
Collection device washes with 0.9%
saline + transfuse immediately or
stored at room temperature for 6 hrs or
at 1-6C for 24 hrs.
Complication: hemolysis, DIVC, air
embolism
Postoperative Blood Salvage
Within first 24-48 hrs after surgery in pt
actively bleeding in closed site (chest,
joint cavity)
Contraindicated if evidence of infection or
malignant tumor cell at site
Blood collected into sterile container,
labelled and filtered.
Reinfuse within 6 hours, to minimize
proliferation of bacteria
Nursing Care during
Blood Transfusion
1. Assess client for history of previous
blood transfusion and any adverse
reactions.
2. Ensure that pt. has an 19 or 19
gauge IV catheter in place
3. Use .0% sodium chloride
4. At least 2 nurses should verify the
blood component
5. Take baseline v/s
6. Start transfusion at slow rate
7. Stay w/ the client for the 1
st
15
mins; continue monitor v/s
8. Maintain prescribe transfusion rate:
1. Whole blood: approx 3-4 hours
2. RBCs: approx 2-4 hours
3. FFP: as quickly as possible
4. Cryoprecipitate: rapid infusion
9. Monitor for adverse reactions
10. Document the following:
1. Blood component unit number
2. Date infusion starts and ends
3. Type of component and amount
transfused
4. Client reaction and v/s
Transfusion Reaction
1. Hemolytic Reaction with in 15 min
a. S/sx headache, lumbar or sternal
pain, dyspnea, restlessness, fever,
chills, heat along veins, renal
shutdown
b. Intervention stop transfusion, obtain
1
st
voided urine specimen, send blood
unit and client blood sample to lab,
continue saline IV
Transfusion Reaction
2. Allergic Reaction with in 30 min
a. S/sx uticaria [hives], laryngeal edema,
dyspnea, sever-shortness of breath
b. Intervention stop transfusion, administer
antihistamine and/or epinephrine.
3. Febrile Reaction with in 15 90 min
a. S/sx fever, chills, flushing, headache, N &
V, palpitations
b. Intervention treat temperature, keep client
covered and warm during transfusion,
administer antipyretic medication.
ANEMIAS
Decreased availability of oxygen
to the tissues
Kinds:
Iron Deficiency Anemia
Aplastic Anemia
Folate Deficiency Anemia
Pernicious Anemia
Hemolytic Anemia
Sickle Cell Anemia
ANEMIAS
Causes
Acute / chronic blood loss
Inadequate dietary intake of
vitamins / minerals needed for rbc
production
Decreased rbc production by the
bone marrow
Increased destruction of rbc
Increased demands of vitamins /
minerals needed for rbc production
COMMON CLINICAL
MANIFESTATIONS
Pallor
Easy fatigability
Weakness
Anorexia
Weight loss
SOB
Headache /
Dizziness
Tachycardia /
palpitations
Syncope
Brittle hair and
nails
Paresthesia
Cold sensitivity
Amenorrhea
Iron-deficiency Anemia
Chronic microcytic, hypochromic
anemia caused by either
inadequate absorption or excessive
loss of iron.
Risk Factors:
a. Women between 15-45 y/o
b. Common in infants whose primary diet
is milk
c. Heavy flow during menses
Assessment:
a. Mild cases usually asymptomatic
b. Palpitations, dizziness, and cold
sensitivity
c. Dyspnea, weakness
d. Laboratory findings:
a. RBCs small and pale
b. HGB markedly decreased
c. Hct decreased
d. Serum iron decreased
Nursing Interventions
Promote rest
Provide good oral care
Provide good skin care.
Diet: Iron rich foods
Organ meals
Beans
Green, leafy vegetables
Raisins
a. Monitor for s/sx of bleeding
b. Provide adequate rest
c. Explain all diagnostic procedure
d. Administer iron preparation
COLLABORATIVE MANAGEMENT
Medical Management
Iron Supplement
Oral
Ferrous Sulfate
Ferrous Gluconate
Ferrous Fumarate
Parenteral: Iron Dextran (Imferon)
Oral iron should be given p.c.
Oral liquid iron to be administered with straw
Vitamin C increases iron absorption
X administer with milk, antacid
Imferon : Z track (deep IM)
Do not massage site of injection
Iron salts change color of stool to dark green
or black
Oxygen therapy
Blood transfusion as needed
FOLATE DEFICIENCY ANEMIA
(MEGALOBLASTIC ANEMIA)
Causes
Poor dietary intake
Rarely eat uncooked
(raw) fruits and
vegetables
Alcoholism
Chronic malnutrition
Pregnancy
Anorexia nervosa
Malabsorption
Malignancy
Prolonged TPN
Chronic
hemodialysis
Assessment
Cracked lips, sore
tongue
Same as Pernicious
Anemia
Collaborative
Management
Well balanced diet
Folic acid 1mg. / day
PERNICIOUS ANEMIA
Macrocytic, hyperchromic anemia
Causes
Gastric surgery
Crohns disease
Pathophysiology
INTRINSIC FACTOR production
VITAMIN B12 absorption
RBC production
DNA synthesis in maturing RBC
(megaloblastic cells)
Impairment of integrity of cells
(mouth, stomach, anus, vagina, axon of
neurons)
DIAGNOSTIC TESTS
Tubeless Gastric Analysis
blue
HCl is present
(-) Pernicious Anemia
X blue
(-) HCL Achlorhydria
(+) Pernicious Anemia
Collect urine specimen
Diagnex blue / Azuressin tablet
DIAGNOSTIC TEST
Schillings Test
Most definitive diagnostic test
Oral radioactive Vitamin B12
IM nonradioactive Vitamin 12
Collect 24 hour urine specimen
Decreased excretion of Vitamin
B12 in the urine
(+) Pernicious Anemia
COLLABORATIVE
MANAGEMENT
Vitamin B12 IM
Daily: 7 days
Weekly: 10 weeks
Monthly: LIFETIME (100mg/Mo)
Hydrochloric acid p.o. for 1 week
Iron therapy
Blood transfusion as needed
Physical examination every six
months
*At risk for Gastric Cancer
APLASTIC ANEMIA
Hypoplasia of the bone
marrow
Fat replaces bone
marrow
PANCYTOPENIA
Anemia
Leukopenia
Thrombocytopenia
Causes
Congenital
Acquired
Idiopathic
Infections
Medications
Heavy metals
Hepatitis
Diagnostic tests
Bone marrow
aspiration /
biopsy
Adult
Posterior Iliac
Crest
Prone Position
Brief , sharp
pain
Child
Tibia
Side lying
position
COLLABORATIVE
MANAGEMENT
Medical Management
Bone marrow transplantation
Immunosuppressive therapy
(Antithymocyte Globulin ATG)
Central line 7 10 days
Blood transfusion as necessary
Stool softeners; high fiber diet
NURSING INTERVENTIONS
Assess for signs and symptoms of
infection, tissue hypoxia and
bleeding
Frequent rest periods
Good oral care
Use soft bristled toothbrush /
soft swabs
Male clients
Use electric razor
NURSING INTERVENTIONS
X ASA administration
Reverse / Protective Isolation
Practice asepsis
X fresh fruits / fresh flowers in the
patients unit
Limit visitors
X allow persons with signs and
symptoms of infection to visit
Hemolytic Anemia
Cause often unknown
Characterize by increased rate of
RBC destruction
Assessment:
Pallor, slight jaundice
Hematuria
Melena
Medical Mngt:
Folic acid supplements
BT
Corticosteroids in
autoimmune types of
anema
Intervention
Monitor for s/sx of
hypoxia
If jaundice and
associated pruritus are
present , avoid soap.
Frequent turning
Sickle Cell Anemia
Characterized by the sickling effect
of the erythrocytes
Predominantly a problem of children.
Asymptomatic until 4-6 mons of age.
Autosomal Recessive
Pathologic changes results from:
Increased blood
viscosity
Increased red cell
destruction 6 20
days life span
Types of Crisis
1. Vaso-occlusive severe pain,
thrombotic; caused by stasis of
blood w/ clumping of cells in the
microcirculation
2. Splenic sequestration life
threatening crisis, death can occur
w/in hours; pooling of large amount
of blood in the spleen and liver
3. Aplastic diminished production
and increased destruction of RBC.
Intervention
Pain control
Promote hydration 4 6 liters/day, folic
acid supplement
Control anxiety
Bedrest
BT
Genetic counseling
Prevent infection
Discharge planning and home care.
DISORDERS AFFECTING THE
RBCS
Polycythemia
rbc and hgb production
Compensatory response to chronic hypoxia
Hypoxia
Erythropoietin production by the kidneys
Stimulation of the bone marrow to rbc
production
DISORDERS AFFECTING THE
RBCS
Polycythemia Vera
Hyperplasia of the bone marrow
rbc (erythrocytosis); wbc (leukocytosis);
platelets (thrombocytosis)
Cause is unknown; associated with genetics
Pathophysiology
rbc, wbc, platelets
blood viscosity
thromboembolism
organ
infiltration
Hepatomegaly
Splenomegaly
Arthralgia
Cerebral hypoxia
capillary
overdistention
Rupture
Hemorrhage
Hypovolemia
POLYCYTHEMIA VERA
Signs and Symptoms
Headache
Dizziness
Blurred vision
Fatigue
Hepato-splenomegaly
COLLABORATIVE MANAGEMENT
fluid intake
Monitor for signs and symptoms of bleeding
Monitor for signs and symptoms of
thromboembolism
Angina
Claudication
Thrombophlebitis
Pruritus
Administer antihistamine to decrease pruritus
Administer analgesic as ordered
Therapeutic phlebotomy
Chemotherapy
Radiation therapy (Na Phosphate / IV)
Patient teaching : Avoid high altitude
Disseminated Intravascular
Coagulation
Hallmarks:
Excessive clotting, followed by
dissolution
Presentation:
Cutaneous oozing, petechiae, cyanosis,
N/V, oliguria, bleeding from GI tract
Causes:
Damage to endothelium
Release of tissue thromboplastin
Activation of Factor X
Disseminated Intravascular Coagulation
Tests/Therapies
TESTS:
Platlets
Prothrombin
Time
Fibrin
THERAPIES
Supportive
Fresh-frozen
plasma,
platelets, or
packed red
cells
Heparin
Intervention:
Watch out for bleeding problems
Provide emotional support
You might also like
- Endocrine DisordersDocument77 pagesEndocrine Disordersahmad100% (2)
- Child With Blood DisorderDocument126 pagesChild With Blood DisorderSivabarathy100% (1)
- Types of AnemiaDocument9 pagesTypes of AnemiaShine Reyes MackieNo ratings yet
- WelcomeDocument103 pagesWelcomeLyka BernalNo ratings yet
- Anemia: Presented byDocument36 pagesAnemia: Presented byParmvir Singh100% (1)
- Acute Cardiac AlterationsDocument38 pagesAcute Cardiac AlterationsJoyce SiosonNo ratings yet
- HYDROCEPHALUSDocument63 pagesHYDROCEPHALUSAjeng Aristiany Rahawarin100% (2)
- Acid-Base Balance PDFDocument3 pagesAcid-Base Balance PDFjanet roosevelt100% (2)
- Acid-Base Balance PDFDocument10 pagesAcid-Base Balance PDFinah krizia lague100% (1)
- Management of Patient With AnemiaDocument58 pagesManagement of Patient With AnemiaDoaa HussainNo ratings yet
- Dyspnea: Ahammed Naseem Roll No: 3 Second Year BSC Nursing Al-Mas College of NursingDocument19 pagesDyspnea: Ahammed Naseem Roll No: 3 Second Year BSC Nursing Al-Mas College of NursingNaseem Bin YoosafNo ratings yet
- Coagulation DisordersDocument14 pagesCoagulation Disorderssusan_grace123No ratings yet
- Nephrotic Syndrome: Prepared by Dr. Kawsar Ahmed Intern Dr. (TMMCH)Document26 pagesNephrotic Syndrome: Prepared by Dr. Kawsar Ahmed Intern Dr. (TMMCH)GENERAL sharpNo ratings yet
- Umbilical Artery CatheterizationDocument11 pagesUmbilical Artery CatheterizationRhaq Sheldon-CoelhoNo ratings yet
- Renal Failure in ChildrenDocument43 pagesRenal Failure in Childrendennyyy175No ratings yet
- Fluids and Electrolytes-2Document82 pagesFluids and Electrolytes-2Jem Loterte100% (1)
- New Fluid and Electrolytes Therapy Toyinoriginali2againDocument55 pagesNew Fluid and Electrolytes Therapy Toyinoriginali2againt.baby100% (1)
- NCM 102 Pedia Nervous, Hema,,Renal, SkeletalDocument178 pagesNCM 102 Pedia Nervous, Hema,,Renal, SkeletalMika SamsonNo ratings yet
- RicketsDocument5 pagesRicketsNader SmadiNo ratings yet
- ErythropoisisDocument47 pagesErythropoisisDisha SuvarnaNo ratings yet
- EndocrineDocument12 pagesEndocrineAna FelNo ratings yet
- Fluid and Electrolytes Lecture NotesDocument85 pagesFluid and Electrolytes Lecture NotesVince Peliño De MesaNo ratings yet
- Maternity Nursing 2Document133 pagesMaternity Nursing 2Rick100% (1)
- Abnormalities of PuerperiumDocument70 pagesAbnormalities of PuerperiumYasmin SharmaNo ratings yet
- Pediatric G.I Disorders FinalDocument53 pagesPediatric G.I Disorders FinalRashid Hussain0% (1)
- Anaemia in Pregnancy: By-Dr. Soumya.p (2nd Yr PG) Mod - Dr. Rita. D (Professor and Hod)Document98 pagesAnaemia in Pregnancy: By-Dr. Soumya.p (2nd Yr PG) Mod - Dr. Rita. D (Professor and Hod)SoumyaNo ratings yet
- Endocrine Disorders TableDocument6 pagesEndocrine Disorders TablebarbaraNo ratings yet
- Fluid, Electrolyte, and Acid-Base BalanceDocument42 pagesFluid, Electrolyte, and Acid-Base BalanceRichelene Mae CanjaNo ratings yet
- Vital Signs: Aurora Roslin Samosa, Man RNDocument57 pagesVital Signs: Aurora Roslin Samosa, Man RNAlexander DontonNo ratings yet
- Medical Surgical NursingDocument66 pagesMedical Surgical Nursing04eden100% (3)
- Congenital Anomalies of KidneDocument7 pagesCongenital Anomalies of KidneSanthosh.S.U100% (2)
- Nephrotic and Nephritic SyndromesDocument27 pagesNephrotic and Nephritic SyndromesJoshua Smith100% (1)
- 5 Bleeding Disorders PPT EditedDocument87 pages5 Bleeding Disorders PPT EditedFrances Isabella OlasimanNo ratings yet
- MenstruationDocument37 pagesMenstruationJoy JarinNo ratings yet
- Fluids Electrolytes - Acid-Base BalanceDocument11 pagesFluids Electrolytes - Acid-Base BalanceJhosita Flora Laroco100% (1)
- Empyema 171013100219Document23 pagesEmpyema 171013100219Mahmoud Abdel MoneimNo ratings yet
- Principles of Fluid Therapy On The Basis ofDocument29 pagesPrinciples of Fluid Therapy On The Basis ofhendrytzNo ratings yet
- MeningitisDocument12 pagesMeningitisFaith Vaughn100% (2)
- Fluids & Electrolyte NewDocument154 pagesFluids & Electrolyte NewMaria Visitacion100% (2)
- Thalassemia PDFDocument88 pagesThalassemia PDFshabrinaerin100% (1)
- IV FluidsDocument47 pagesIV FluidsMuvenn Kannan100% (1)
- Body Fluids-1: Fluid Compartments of The Body Fluid and Electrolyte CompositionDocument33 pagesBody Fluids-1: Fluid Compartments of The Body Fluid and Electrolyte CompositionMan LingNo ratings yet
- Disorders of The Genitourinary SystemDocument49 pagesDisorders of The Genitourinary SystemYemaya84No ratings yet
- Diagnostic TestingDocument10 pagesDiagnostic TestingVrindha Vijayan100% (1)
- Increased Intracranial PressureDocument34 pagesIncreased Intracranial PressureshykitijaNo ratings yet
- Neurologic System: Carolyn Jarvis Physical Examination and Health Assessment Fourth EditionDocument37 pagesNeurologic System: Carolyn Jarvis Physical Examination and Health Assessment Fourth Edition03152788100% (1)
- Eyes and Ears DisordersDocument36 pagesEyes and Ears Disordersjeshema100% (4)
- Neurological SystemDocument10 pagesNeurological SystemManelle SingzonNo ratings yet
- Enzymes of Clinical SignificanceDocument65 pagesEnzymes of Clinical SignificancepaulaOrialNo ratings yet
- Q. List Different Functions of The Kidney: (A) Homeostatic FunctionDocument42 pagesQ. List Different Functions of The Kidney: (A) Homeostatic Functionramadan100% (4)
- Respiratory System DisordersDocument353 pagesRespiratory System Disordersይደግ አብነውNo ratings yet
- Hepatic EncephalopathyDocument3 pagesHepatic EncephalopathySuhas KandeNo ratings yet
- Nursing Management in Abdominal SurgeryDocument19 pagesNursing Management in Abdominal Surgeryejguy7777100% (2)
- Anomalies of Skeletal System-1Document44 pagesAnomalies of Skeletal System-1Meena Koushal100% (1)
- Hemorrhagic Disease of The NewbornDocument2 pagesHemorrhagic Disease of The NewbornsucirahmiiiiiiNo ratings yet
- Leukemia in Children: 1 Rahul Dhaker, Asst. Professor, RCNDocument41 pagesLeukemia in Children: 1 Rahul Dhaker, Asst. Professor, RCNRahul DhakerNo ratings yet
- Disseminated Intravascular Coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandDisseminated Intravascular Coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Acute Respiratory Distress Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandAcute Respiratory Distress Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Infant Jaundice, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandInfant Jaundice, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Critical ThinkingDocument6 pagesCritical ThinkingmatrixtrinityNo ratings yet
- Intelligence in PsychologyDocument29 pagesIntelligence in PsychologymatrixtrinityNo ratings yet
- Stress and Illness: Castillo, Justine GDocument19 pagesStress and Illness: Castillo, Justine GmatrixtrinityNo ratings yet
- Group Number: Case Title: Year and Section: Group Members: 1. 5. 2. 6. 3. 7. 4. 8Document1 pageGroup Number: Case Title: Year and Section: Group Members: 1. 5. 2. 6. 3. 7. 4. 8matrixtrinityNo ratings yet
- antepartumTEST1 MOSBYDocument14 pagesantepartumTEST1 MOSBYmatrixtrinity50% (2)
- Antepartumtest2 LippincottDocument7 pagesAntepartumtest2 Lippincottmatrixtrinity100% (1)
- Distinguishing Features of Anthropology - Characteristics 1-5 6.78 What Are The3 Unique Approaches of AnthropologyDocument2 pagesDistinguishing Features of Anthropology - Characteristics 1-5 6.78 What Are The3 Unique Approaches of AnthropologymatrixtrinityNo ratings yet
- Intestinal Obstruction5Document4 pagesIntestinal Obstruction5matrixtrinityNo ratings yet
- Socio - GENDER, ETHNICITY AND RACEDocument22 pagesSocio - GENDER, ETHNICITY AND RACEmatrixtrinity100% (1)
- Cardio DiseasesDocument17 pagesCardio DiseasesmatrixtrinityNo ratings yet
- Intestinal Obstruction Wit Pic2Document2 pagesIntestinal Obstruction Wit Pic2matrixtrinityNo ratings yet
- Blood ComponentDocument33 pagesBlood Componentmatrixtrinity100% (1)
- Cardiovascular Physio Logic ProcessDocument35 pagesCardiovascular Physio Logic ProcessmatrixtrinityNo ratings yet
- What Is Intestinal ObstructionDocument5 pagesWhat Is Intestinal ObstructionmatrixtrinityNo ratings yet
- Cerebrovascular Accidents: Rochee P. Benito, RNDocument23 pagesCerebrovascular Accidents: Rochee P. Benito, RNmatrixtrinityNo ratings yet
- Circulatory System: Rochi Paraon Benito, RN Infection Control NurseDocument15 pagesCirculatory System: Rochi Paraon Benito, RN Infection Control NursematrixtrinityNo ratings yet
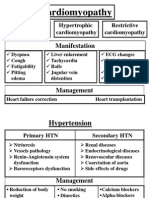
- Cardiomyopathy 02Document2 pagesCardiomyopathy 02matrixtrinityNo ratings yet
- Cardiovascular Therapeutic ManagementDocument15 pagesCardiovascular Therapeutic ManagementmatrixtrinityNo ratings yet
- Burns and Environmental EmergenciesDocument33 pagesBurns and Environmental EmergenciesmatrixtrinityNo ratings yet
- Nutritional Requirements in Pregnancy and LactationDocument12 pagesNutritional Requirements in Pregnancy and LactationPatrick nyawiraNo ratings yet
- Pharm MCQ BookDocument11 pagesPharm MCQ BookanojanNo ratings yet
- Therapeutic Interchange ListDocument29 pagesTherapeutic Interchange ListНазарій ЛавровськийNo ratings yet
- Anaemia in Pregnancy-MaklapDocument34 pagesAnaemia in Pregnancy-MaklapBronson KaturkanaNo ratings yet
- Parenteral Iron TherapyDocument31 pagesParenteral Iron TherapyEmmanuel Kissiedu Antiri100% (1)
- Lecture 29-AnemiaDocument35 pagesLecture 29-AnemiaBini JaminNo ratings yet
- CKD My PharmacotherapyDocument7 pagesCKD My PharmacotherapyJA TongNo ratings yet
- Oral Iron ProductsDocument2 pagesOral Iron ProductsOlga BabiiNo ratings yet
- An Approach To Anemic PatientDocument79 pagesAn Approach To Anemic PatientHussain AzharNo ratings yet
- OB Hematologic DiseasesDocument2 pagesOB Hematologic DiseasespreciousjemNo ratings yet
- Spectrophotometric Method For Quantitative Determination of Iron III From Iron Polymaltose ComplexDocument6 pagesSpectrophotometric Method For Quantitative Determination of Iron III From Iron Polymaltose ComplexAde MuchlasNo ratings yet
- Iron Nutrition and Lead ToxicityDocument32 pagesIron Nutrition and Lead ToxicityChibueze EzeokaforNo ratings yet
- Drug Study Ferrous SulfateDocument2 pagesDrug Study Ferrous SulfatePauline AnesNo ratings yet
- LP 1 I NCM 107 RLE I CARE OF PREGNANT WOMAN StudentsDocument28 pagesLP 1 I NCM 107 RLE I CARE OF PREGNANT WOMAN StudentsNaomi Anne AsuntoNo ratings yet
- Obs-UM - Paper - 1Document16 pagesObs-UM - Paper - 1Muhammad Abbas AliNo ratings yet
- Iron SucroseDocument3 pagesIron SucroseAtul KumarNo ratings yet
- Ferrous Sulfate Syrup InsertDocument6 pagesFerrous Sulfate Syrup InsertPrincess TiongsonNo ratings yet
- Tratamiento de Anemia Por Deficiencia de Hierro en Ancianos Nuevos ParadigmasDocument11 pagesTratamiento de Anemia Por Deficiencia de Hierro en Ancianos Nuevos ParadigmasCarlos OlivoNo ratings yet
- Agen HematinikDocument77 pagesAgen HematinikErinaGeraldiNo ratings yet
- What Causes Iron-Deficiency Anemia?Document54 pagesWhat Causes Iron-Deficiency Anemia?Zaia Raymond FlumoNo ratings yet
- Iron Dextran Drug StudyDocument5 pagesIron Dextran Drug StudySofronio OmboyNo ratings yet
- COMPILATIONSSSSDocument976 pagesCOMPILATIONSSSSANNooonynmousNo ratings yet
- Physiological C-WPS OfficeDocument15 pagesPhysiological C-WPS OfficeGwagsiGlennNo ratings yet
- Liposomal IronDocument6 pagesLiposomal IronPiyush KhetrapalNo ratings yet
- Deficiency Iron AnemiaDocument9 pagesDeficiency Iron AnemiaNadia Puspita DewiNo ratings yet
- AGA Technical Review On GI Evaluation of Iron Deficiency AnemiaDocument10 pagesAGA Technical Review On GI Evaluation of Iron Deficiency AnemiaElena ChNo ratings yet
- Anemia During PregnancyDocument7 pagesAnemia During Pregnancydita fNo ratings yet
- 813-Article Text-1261-1-10-20180214Document5 pages813-Article Text-1261-1-10-20180214dwiky ramaNo ratings yet
- Vi. Drug Study: Source: 2011 Lippincott's Nursing Drug GuideDocument8 pagesVi. Drug Study: Source: 2011 Lippincott's Nursing Drug GuideDarNo ratings yet
- KU - Lesson 4A - DRUGS USED IN ANAEMIADocument60 pagesKU - Lesson 4A - DRUGS USED IN ANAEMIAchristine gisembaNo ratings yet