Professional Documents
Culture Documents
Surgical Vacuum Drains
Surgical Vacuum Drains
Uploaded by
obonk2880 ratings0% found this document useful (0 votes)
13 views9 pagesjurnal
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentjurnal
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
13 views9 pagesSurgical Vacuum Drains
Surgical Vacuum Drains
Uploaded by
obonk288jurnal
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 9
Surgical Vacuum Drains:
Types, Uses, and
Complications
RAJARAMAN DURAI, MD, MRCS; PHILIP C.H. NG, MD, FRCS
1.2
ABSTRACT
High- and low-pressure vacuum drains are commonly used after surgical procedures.
High-pressure vacuum drains (ie, sealed, closed-circuit systems) are efcient and
allow for easy monitoring and safe disposal of the drainage. Low-pressure vacuum
drains use gentle pressure to evacuate excess uid and air, and are easy for patients
to manage at home because it is easy to reinstate the vacuum pressure. Perioperative
nurses should be able to identify the various types of commonly used drains and their
surgical applications. Nurses should know how to care for drains, how to reinstate
the vacuum pressure when necessary, and the potential complications that could
result from surgical drain use. AORN J 91 (February 2010) 266-271. AORN, Inc,
2010
Key words: surgical drains, four-channel vacuum drains, low-pressure vacuum
drains, high-pressure vacuum drains, negative pressure.
D
rains are commonly used after surgical
procedures and can be classied as either
active or passive.
1
Active drains use neg-
ative pressure to remove accumulated uid from a
wound. Passive drains depend on the higher pres-
sure inside the wound in conjunction with capil-
lary action and gravity to draw uid out of a
wound (ie, the difference in pressure between the
inside and the outside of the wound forces the
uid out of the wound).
Passive drains, such as a Penrose drain, do not
require special attention; the dressing is changed
when it becomes saturated, or, if the drain is at-
tached to a reservoir, then the reservoir is emptied
or changed when it is full. Active drains, how-
ever, do require special maintenance. The collec-
tion reservoir of an active drain expands as it col-
lects uid drainage by exchanging negative
pressure for uid. The drain becomes ineffective
if the vacuum is lost. This article provides infor-
mation on the various types of commonly used
vacuum drains, nursing care of drains, methods to
reinstate a drains vacuum pressure, and potential
complications of drain use.
indicates that continuing education contact
hours are available for this activity. Earn the con-
tact hours by reading this article, reviewing the
purpose/goal and objectives, and completing the
online examination and learner evaluation at http://
www.aornjournal.org/ce. The contact hours for this
article expire February 28, 2013.
266 AORN Journal February 2010 Vol 91 No 2 AORN, Inc, 2010
USE OF DRAINS
Drains are used both prophylactically and thera-
peutically. The most common use is prophylactic
after surgery to prevent the accumulation of uid
(eg, blood, pus) or air. In any surgery in which a
dead space (eg, a cavity) is created, the body has
a natural tendency to ll this space with uid or
air. Use of a prophylactic drain is not routinely
recommended after clean surgical procedures,
2,3
although some articles claim that use of drains
results in seroma reduction,
4,5
and results of re-
search have shown that use of vacuum drains may
not inuence the outcome after tissue expander
use in breast surgery.
6
Surgical drains commonly
are used after procedures on the thyroid,
2
breast,
7
and axillary area as well as after abdominal pro-
cedures and joint replacements.
8,9
Vacuum drains
may be used to drain perirectal wounds,
10
and
certain special vacuum drains (ie, endoluminal)
are available to treat anastomotic leaks that may
occur after intestinal resection and anastomosis.
11,12
DRAIN INSERTION
Typically, when a drain is required, it is inserted
at the end of a surgical procedure. Frequently, the
drain is inserted through a separate hole a few
centimeters from the main incision to decrease the
risk of a postoperative wound infection. There are
two methods to insert a vacuum-type drain. The
rst method is used with drains that have a sharp
trocar attached to the tube. The surgeon uses the
trocar with some drains attached to pierce the
skin from the inside of the wound at the desired
site and pulls the attached tube out through the
stab wound. The surgeon places the inner end of
the tube at the required site and detaches the tro-
car. The surgeon may secure the drain to the skin
with a stay-stitch. After the wound is closed, the
scrub person connects the tube to the reservoir.
Suction may be attached to the reservoir to facili-
tate wound drainage.
The second method for drain insertion is used
when a trocar is not attached to the drainage tube.
In this case, the surgeon uses a forceps to pierce
the abdominal wall from the inside of the wound
and pushes the forceps through the subcutaneous
tissue. He or she then incises the overlying skin
with a scalpel. The surgeon opens the tip of the
forceps to grasp the end of the drain tube and
pulls the drain into the wound to the desired loca-
tion. The surgeon may secure the tube to the pa-
tients skin with a stay-stitch. The scrub person
connects the tube to the reservoir after the wound
is closed.
Vacuum drains are classied according to the
degree of pressure used. Typical bottled vacuum
drains (eg, Redi-vac) use high negative pressure.
Bulb-shaped suction devices (eg, Jackson-Pratt)
and collapsible four-channel vacuum drains (eg,
J Vac, Blake) use low negative pressure.
HIGH-NEGATIVE-PRESSURE DRAINS
High-pressure bottled vacuum drains have the
advantages of being sealed, closed-circuit systems
that allow for easy monitoring and safe disposal
of the drainage. These systems consist of a clear,
plastic reservoir with a rubber cap that has indica-
tor wings to monitor the presence of vacuum
pressure and an opening in which to connect the
drainage tube. When a vacuum is present in the
system, the wings on the rubber cap are close
together; the wings are apart if the vacuum is
lost. The end of the drainage tube that is inserted
into the wound has multiple openings on its inner
side through which uid can be evacuated from
the wound. The wound should be closed before
the clamps on the drain are opened; otherwise the
vacuum will be lost as the tube sucks in atmo-
spheric air.
Although the patients condition and type of
surgical procedure indicate appropriate monitoring
times and documentation of drainage volumes, the
amount of drainage typically is measured two to
four hours after surgery and every six hours
thereafter. Occasionally, the surgeon may decide
to clamp the tube for a couple of hours if it
drains too much (eg, more than 100 mL an
hour).
13
This may occur after some procedures,
SURGICAL VACUUM DRAINS www.aornjournal.org
AORN Journal 267
such as joint replacements. Once every 24 hours,
the nurse should mark the drainage reservoir bot-
tle and record the volume of drainage collected in
24 hours.
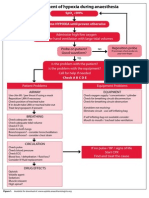
Reinstating Vacuum Pressure
When the vacuum is lost, the drain will not func-
tion, so the tube has to be connected to a new
bottle or the vacuum must be reinstated by one of
the following methods. A clinician removes the
bottle from the drainage tube and loosens the
plastic attachment. In method #1 (ie, the suction-
tube method), the clinician connects the plastic
tube of the suction machine to the white plastic
attachment of the vacuum bottle and turns on the
suction machine (Figure 1). In method #2 (ie, the
reverse Yankauer suction method), the clinician
inserts the tip of a Yankauer suction catheter into
the suction machine tube. The clinician then holds
the connection end of the Yankauer suction cathe-
ter tightly against the white plastic attachment of
the vacuum bottle and turns on the suction ma-
chine. In both methods, when the rubber cap
shows evidence of enough vacuum pressure in the
bottle, the clinician clamps the plastic attachment
on the drainage tube to retain the vacuum pres-
sure, then the clinician disconnects the suction
machine tubing.
LOW-NEGATIVE-PRESSURE DRAINS
Low-pressure vacuum drains have a plastic bulb-
shaped reservoir and a silicone drainage tube,
with multiple side holes at the end that is inserted
into the wound. When the bulb is compressed, air
is forced out, which creates negative pressure in
the system. Low-negative-pressure drains work
gently to evacuate excess uid and air.
It is easy to educate the patient so that he or
she can care for a bulb-type, low-pressure vac-
uum drain at home without help. Removing the
plug from the exit valve allows the bulb to in-
ate. The amount of drainage is easily quantied
with the measurement marks on the side of the
bulb. The patient empties the contents into a dis-
posable container or cup by squeezing the bulb
reservoir, then the patient squeezes the bulb again
and replaces the cap, thus recreating the negative
pressure. The patient can also be instructed on
Figure 1. One method to reinstate the pressure in a
high-pressure bottled vacuum drain is to attach the
plastic tube (arrow) to the suction unit and then
release and close the valve when appropriate.
Figure 2. A four-channel vacuum drain ready for
insertion.
February 2010 Vol 91 No 2 DURAING
268 AORN Journal
how to remove the drain at home without assis-
tance, if necessary.
A four-channel vacuum drain is a type of low-
pressure drain; the primary difference is the size
and shape of the reservoir.
14
The drain tube is
soft and exible,
15
and the reservoir is foldable
with two outlets (Figure 2). One outlet is used for
connecting to two drains and another outlet is
used for emptying the contents. The drainage tube
has four tiny lumina that join to form a single
lumen. The advantage of a four-channel vacuum
drain is that it is unlikely to become occluded by
the omentum because of the tiny size of the
holes. The disadvantage is that the holes may not
be large enough to evacuate larger particles of
tissue or blood clots.
After the surgeon inserts the drain by using
one of the two methods previously described, the
scrub person connects the drain tube to the outlet
adaptor. The scrub person folds or bends the res-
ervoir into a U shape by pressing both thumbs on
the marked areas in the middle part of the reser-
voir, which releases the locking system (Figure
3). The scrub person removes the plug from the
exit valve and repeats the procedure by bending
the reservoir to create vacuum pressure. The
scrub person then reseals the reservoir with the
plug. The scrub person may have to repeat this
process several times until all the air is removed
from the reservoir. On the postoperative nursing
unit, the nurse monitors drain output and empties
the reservoir when required. A vacuum is easily
visible by the undistended or unfolded appearance
of the reservoir. The bag will appear larger when
the vacuum is lost.
DRAIN REMOVAL
The negative pressure in the reservoir should be
released by removing the plug from the exit
valve, and the bulb or reservoir should be discon-
nected before the drain is removed. After cutting
the stay-stitch, if there is one, the nurse or patient
smoothly pulls out the drain. Drain removal can
be painful for some patients, so the patient may
wish to take an oral analgesic before removing
the drain. After removing the drain, the nurse or
patient should clean the drain-tube site with anti-
septic and a small dry cotton swab. If the site is
oozing, then the nurse can apply a gauze dressing.
If there is a large quantity of drainage, then the
nurse can apply a stoma bag.
COMPLICATIONS OF VACUUM DRAINS
Although drains serve an important function, there
are potential complications with their use. Some of
these complications include the following:
BreakageDrains are made of strong silicone
or polyvinyl chloride plastic and, therefore,
are not likely to break, but breakage can oc-
cur.
16
Laparoscopy may be required if part of
a drain breaks off inside the patients abdo-
men during removal.
17
Figure 3. To use a four-channel vacuum drain, the
clinician bends the reservoir into a U by pressing
both thumbs on the marked spots to release the
lock.
SURGICAL VACUUM DRAINS www.aornjournal.org
AORN Journal 269
Difculty in removalIf a drain remains in-
serted for a long period of time, it may be-
come difcult to remove. On occasion, the
drain has been stitched to the wound during
closure of deeper layers. The nurse should
report any difculty encountered during drain
removal to the surgeon. The wound may need
to be temporarily opened to remove the drain.
Inadvertent removalDrains may get tangled
in the patients other lines (eg, IV tubing,
electrocardiogram leads) or become tangled in
clothing or linen and accidentally be pulled
out. This might cause bleeding or pain.
InfectionAlthough one purpose of surgical
drains is to evacuate excessive uid accumula-
tion to prevent bacterial proliferation, drains
can increase the risk of infection via retro-
grade bacterial migration. Typically, drains are
removed when they are draining a negligible
amount (eg, less than 25 mL per day; less
than 1 mL per hour) to minimize this risk.
OcclusionDrain tubes can become occluded
by blood clot, tissue, or the omentum. This can
lead to the formation of a hematoma and subse-
quent discomfort and increased risk for infection.
PainDrain sites can be painful and may pre-
vent the patient from lying on the side where the
drain is inserted. Furthermore, some patients are
apprehensive about moving with a drain in place
after surgery; lack of movement can potentially
increase the risk of postoperative immobility
complications (eg, venous thrombosis).
Unsightly scarA drain site is left to heal by
secondary intention so the site may form a
puckering scar. When possible, the surgeon
may place the drain in a skin crease to help
improve cosmesis.
18
Visceral perforationDrains left in place for a
long period of time can erode into the bowel
and lead to visceral perforation.
19
SUMMARY
Perioperative nurses need to know the surgical
uses of high- and low-pressure vacuum drainage
systems as well as potential complications of sur-
gical drain use. Understanding how to create the
negative pressure vacuum will help nurses pro-
vide better drain care and better patient education.
Knowing how to recreate the negative pressure in
a high-pressure reservoir is particularly useful
when an underlled high-pressure vacuum drain
bottle loses its vacuum pressure. Low-pressure
vacuum drains have the advantages of easy emp-
tying and easy recreation of the gentle, negative
low-pressure vacuum, and they are easy for pa-
tients to manage at home.
Editors note: Redi-vac is a trademark of
Atrium Medical, Hudson, NH. Jackson-Pratt is
a registered trademark of Cardinal Health, Dub-
lin, OH. J Vac and Blake are registered
trademarks of Ethicon, St Louis, MO.
References
1. Durai R, Mownah A, Ng PC. Use of drains in surgery:
a review. J Perioper Pract. 2009;19(6):180-186.
2. Suslu N, Vural S, Oncel M, et al. Is the insertion of
drains after uncomplicated thyroid surgery always nec-
essary? Surg Today. 2006;36(3):215-218.
3. Kumar M, Yang SB, Jaiswal VK, Shah JN, Shreshtha
M, Gongal R. Is prophylactic placement of drains nec-
essary after subtotal gastrectomy? World J Gastroen-
terol. 2007;13(27):3738-3741.
4. Ismail M, Garg M, Rajagopal M, Garg P. Impact of
closed-suction drain in preperitoneal space on the inci-
dence of seroma formation after laparoscopic total ex-
traperitoneal inguinal hernia repair. Surg Laparosc En-
dosc Percutan Tech. 2009;19(3):263-266.
5. Chowdri NA, Qadri SA, Parray FQ, Gagloo MA. Role
of subcutaneous drains in obese patients undergoing
elective cholecystectomy: a cohort study. Int J Surg.
2007;(6):404-407. Epub June 8, 2007.
6. McCarthy CM, Disa JJ, Pusic AL, Mehrara BJ, Cord-
eiro PG. The effect of closed-suction drains on the inci-
dence of local wound complications following tissue
expander/implant reconstruction: a cohort study. Plast
Reconstr Surg. 2007;119(7):2018-2022.
7. Barton A, Blitz M, Callahan D, Yakimets W, Adams
D, Dabbs K. Early removal of postmastectomy drains is
not benecial: results from a halted randomized con-
trolled trial. Am J Surg. 2006;191(5):652-656.
8. Sundaram RO, Parkinson RW. Closed suction drains do
not increase the blood transfusion rates in patients un-
dergoing total knee arthroplasty. Int Orthop. 2007;31
(5):613-616. Epub September 1, 2006.
9. Kumar S, Penematsa S, Parekh S. Are drains required
following a routine primary total joint arthroplasty? Int
Orthop. 2007;31(5):593-596. Epub October 11, 2006.
February 2010 Vol 91 No 2 DURAING
270 AORN Journal
10. Durai R, Ng PC. Perirectal abscess following procedure
for prolapsed haemorrhoids successfully managed with
a combination of VAC sponge and Redivac systems.
Tech Coloproctol. 2009;13(4):307-309. Epub July 14,
2009.
11. Weidenhagen R, Gruetzner KU, Wiecken T, Spelsberg
F, Jauch KW. Endoluminal vacuum therapy for the
treatment of anastomotic leakage after anterior rectal
resection. Rozhl Chir. 2008;87(8):397-402.
12. Richterich JP, Heigl A, Muff B, Luchsinger S,
Gutzwiller JP. Endo-SPONGE: a new endoscopic treat-
ment option in colonoscopy. Gastrointest Endosc. 2008;
68(5):1019-1022. Epub June 4, 2008.
13. Brueggemann PM, Tucker JK, Wilson P. Intermittent
clamping of suction drains in total hip replacement re-
duces postoperative blood loss: a randomized, con-
trolled trial. J Arthroplasty. 1999;14(4):470-472.
14. Tsuda Y, Takemura T, Shimamura Y, Iwasa S. Useful-
ness of silicone Blake drains after cardiac surgery [in
Japanese]. Kyobu Geka. 2003;56(12):1017-1019.
15. Rayatt SS, Dancey AL, Jaffe W. Soft uted silicone
drains: a prospective, randomized, patient-controlled
study. Plast Reconstr Surg. 2005;115(6):1605-1608.
16. Campbell W, Wallace W, Gibson E, McCallion K.
Intra-abdominal drain fracture following pancreatic ne-
crosectomy. Ir J Med Sci. Epub ahead of print April 9,
2009.
17. Bharathan R, Dexter S, Hanson M. Laparoscopic re-
trieval of retained Redivac drain fragment. J Obstet
Gynaecol. 2009;29(3):263-264.
18. Dhar V, Townsley R, Black M, Laccourreye O. Thy-
roid surgery: the sub-mental drain. J Laryngol Otol.
2009;123(7):786. Epub October 17, 2008.
19. Carter P. Perforation of the bowel by suction drains.
Br J Surg. 1993;80(1):129.
Rajaraman Durai, MD, MRCS, is a specialist
registrar at University Hospital Lewisham,
London, UK. Dr Durai has no declared aflia-
tion that could be perceived as a potential con-
ict of interest in publishing this article.
Philip C.H. Ng, MD, FRCS, is a consultant
surgeon for the Department of Surgery at Uni-
versity Hospital Lewisham, London, UK.
Dr Ng has no declared afliation that could be
perceived as a potential conict of interest in
publishing this article.
SURGICAL VACUUM DRAINS www.aornjournal.org
AORN Journal 271
CONTINUING EDUCATION PROGRAM
1.2
Surgical Vacuum Drains: Types,
Uses, and Complications
PURPOSE
To educate perioperative nurses about the use of surgical vacuum drains.
OBJECTIVES
1. Differentiate between passive and active drains.
2. Identify uses of surgical drains.
3. Discuss how drains are inserted.
4. Explain how to reinstate vacuum pressure.
5. Describe low-pressure vacuum drains.
6. Identify complications associated with drain use.
The Examination and Learner Evaluation are printed here for your convenience. To
receive continuing education credit, you must complete the Examination and
Learner Evaluation online at http://www.aorn.org/CE.
QUESTIONS
1. Passive drains
a. use negative pressure to remove accumulated
uid from a wound.
b. depend on the higher pressure inside the
wound in conjunction with capillary action and
gravity to draw uid out of a wound.
c. use the sodium-potassium pump to exchange
sodium ions across the cell membrane with
potassium, which draws uid out of the
wound.
2. The collection reservoir of an active drain ex-
changes negative pressure for uid, so if the vac-
uum is lost, the drain becomes ineffective.
a. true b. false
3. The most common use of drains is to
a. introduce medication such as antibiotics into
the surgical wound after surgery.
b. decrease postoperative pain.
c. prevent the accumulation of uid or air
postoperatively.
d. monitor pressure inside the wound.
4. Use of a prophylactic drain is routinely recom-
mended after clean surgical procedures.
a. true b. false
5. When a surgeon inserts a drain with an attached
trocar, he or she pierces the skin from the outside
of the wound at the desired site and pulls the at-
tached tube in through the stab wound.
a. true b. false
EXAMINATION
272 AORN Journal February 2010 Vol 91 No 2 AORN, Inc, 2010
6. When a surgeon inserts a drain without an at-
tached trocar, the surgeon
1. uses a forceps to pierce the abdominal wall
from the inside of the wound.
2. pushes the forceps through the subcutaneous
tissue.
3. incises the overlying skin with a scalpel.
4. grasps the end of drain tube with the forceps
and pulls it into the wound.
5. secures the tube to the patients skin with a
stay-stitch.
a. 2 and 3 b. 1, 4, and 5
c. 2, 3, 4, and 5 d. 1, 2, 3, 4, and 5
7. If vacuum pressure is lost in a high-pressure bot-
tled vacuum drain, the vacuum can be reinstated
by using the ___________________ method.
1. reverse Yankauer suction
2. suction camshaft
3. suction tube
4. inversion suction
a. 1 and 3 b. 2 and 4
c. 1, 2, and 3 d. 1, 2, 3, and 4
8. The advantages of bulb-type, low-pressure vac-
uum drains include that
1. they can easily be cared for by the patient at
home without help.
2. the amount of drainage is easy to quantify.
3. the patient can be instructed on how to remove
the drain without assistance at home.
4. they work gently to evacuate excess uid and
air.
a. 1 and 2 b. 3 and 4
c. 1, 2, and 3 d. 1, 2, 3, and 4
9. The advantage of a four-channel vacuum drain is
that it
a. can evacuate larger particles of tissue or blood
clots.
b. can be used in multiloculated cavities.
c. is unlikely to become occluded by the
omentum.
d. has a higher negative-pressure vacuum.
10. Potential complications of drain use include
1. breakage or occlusion.
2. difcult or inadvertent removal.
3. electrolyte imbalance.
4. infection.
5. pain or unsightly scar.
6. visceral perforation.
a. 1, 3, and 5 b. 2, 3, 4, and 6
c. 1, 2, 4, 5, and 6 d. 1, 2, 3, 4, 5, and 6
The behavioral objectives and examination for this program were prepared by Rebecca Holm, RN, MSN, CNOR, clinical editor,
with consultation from Susan Bakewell, RN, MS, BC, director, Center for Perioperative Education. Ms Holm and Ms Bakewell
have no declared afliations that could be perceived as potential conicts of interest in publishing this article.
CE EXAMINATION www.aornjournal.org
AORN Journal 273
CONTINUING EDUCATION PROGRAM
1.2
Surgical Vacuum Drains: Types,
Uses, and Complications
T
his evaluation is used to determine the extent to
which this continuing education program met
your learning needs. Rate the items as described
below.
OBJECTIVES
To what extent were the following objectives of this
continuing education program achieved?
1. Differentiate between passive and active
drains. Low 1. 2. 3. 4. 5. High
2. Identify uses of surgical drains.
Low 1. 2. 3. 4. 5. High
3. Discuss how drains are inserted.
Low 1. 2. 3. 4. 5. High
4. Explain how to reinstate vacuum pressure.
Low 1. 2. 3. 4. 5. High
5. Describe low-pressure vacuum drains.
Low 1. 2. 3. 4. 5. High
6. Identify complications associated with drain
use. Low 1. 2. 3. 4. 5. High
CONTENT
7. To what extent did this article increase your
knowledge of the subject matter?
Low 1. 2. 3. 4. 5. High
8. To what extent were your individual objectives
met? Low 1. 2. 3. 4. 5. High
9. Will you be able to use the information from
this article in your work setting? 1. Yes 2. No
10. Will you change your practice as a result of
reading this article? (If yes, answer question
#10A. If no, answer question #10B.)
10A. How will you change your practice (Select all
that apply)
1. I will provide education to my team regard-
ing why the change is needed.
2. I will work with management to change
and/or implement a policy and procedure.
3. I will plan an informational meeting with
physicians to seek their input and acceptance
of the need for the change.
4. I will implement the change and evaluate the
effect of the change at regular intervals until
the change is incorporated as best practice.
5. Other:
10B. If you will not change your practice as a result
of reading this article, why? (Select all that
apply)
1. The content of the article is not relevant to
my practice.
2. I do not have enough time to teach others
about the purpose of the needed change.
3. I do not have management support to make a
change.
4. Other:
11. Our accrediting body requires that we verify the
time you needed to complete the 1.2 continuing
education contact hour (72-minute) program:
This program meets criteria for CNOR and CRNFA recertication, as well as other continuing education requirements.
AORN is accredited as a provider of continuing nursing education by the American Nurses Credentialing Centers Commission on Accreditation.
AORN recognizes these activities as continuing education for registered nurses. This recognition does not imply that AORN or the American Nurses Credentialing Center
approves or endorses products mentioned in the activity.
AORN is provider-approved by the California Board of Registered Nursing, Provider Number CEP 13019. Check with your state board of nursing for acceptance of this
activity for relicensure.
Event: #10007; Session: #4000 Fee: Members $6, Nonmembers $12
The deadline for this program is February 28, 2013.
A score of 70% correct on the examination is required for credit. Participants receive feedback on incorrect answers. Each
applicant who successfully completes this program will be able to print a certicate of completion.
LEARNER EVALUATION
274 AORN Journal February 2010 Vol 91 No 2 AORN, Inc, 2010
You might also like
- Sarrafian's Anatomy - Foot & Ankle - 3rdDocument779 pagesSarrafian's Anatomy - Foot & Ankle - 3rdOrto Mesp100% (16)
- ADD-00058826 ARCHITECT CC-IA Traceability Uncertainty Brochure PDFDocument21 pagesADD-00058826 ARCHITECT CC-IA Traceability Uncertainty Brochure PDFhm07100% (2)
- Surgical Wound ClassificationDocument1 pageSurgical Wound Classificationgeclear323No ratings yet
- The Newcastle Upon Tyne Hospitals NHS Foundation Trust Count ProcedureDocument42 pagesThe Newcastle Upon Tyne Hospitals NHS Foundation Trust Count ProcedureGina AprianaNo ratings yet
- Apraxia TreatmentDocument80 pagesApraxia Treatmentaalocha_25100% (1)
- Suction Machine: Surgical Students 5 Semester 5 BatchDocument12 pagesSuction Machine: Surgical Students 5 Semester 5 BatchIhteshamNo ratings yet
- Intraoperative CareDocument5 pagesIntraoperative CareraffineeNo ratings yet
- Catalago de AspiradoresDocument20 pagesCatalago de AspiradoresGomez, Francisco (AJR)No ratings yet
- Suction Machine GuidelinesDocument3 pagesSuction Machine GuidelinesSandip RajpurohitNo ratings yet
- Thoracic TraumaDocument24 pagesThoracic TraumaOmar MohammedNo ratings yet
- Minimal Invasive Surgery, Robotic, Natural Orifice Transluminal EndoscopicDocument59 pagesMinimal Invasive Surgery, Robotic, Natural Orifice Transluminal EndoscopicKahfi Rakhmadian KiraNo ratings yet
- Mastectomy/ Modified Radical Mastectomy: IndicationsDocument6 pagesMastectomy/ Modified Radical Mastectomy: IndicationsNANDAN RAINo ratings yet
- Skin Integrity and Wound CareDocument47 pagesSkin Integrity and Wound CareCHALIE MEQUNo ratings yet
- Foley Catheter CareDocument6 pagesFoley Catheter Carefreddie27No ratings yet
- Ecmo Review 2Document11 pagesEcmo Review 2Anonymous ZUaUz1wwNo ratings yet
- Orthopedic EmergenciesDocument75 pagesOrthopedic EmergenciesAlex beharuNo ratings yet
- Surgical DrainsDocument2 pagesSurgical DrainsSalim Mwaffaq AlhalholyNo ratings yet
- Staged Abdominal Re-Operation For Abdominal TraumaDocument7 pagesStaged Abdominal Re-Operation For Abdominal TraumaNovrianda Eka PutraNo ratings yet
- Facial InjuriesDocument61 pagesFacial InjuriesafifrspmNo ratings yet
- Surgical Infections Surgical Infections: HistoryDocument7 pagesSurgical Infections Surgical Infections: Historyjc_sibal13No ratings yet
- Adaptability (CS) - WPS OfficeDocument21 pagesAdaptability (CS) - WPS OfficeMalde KhuntiNo ratings yet
- Ot PDFDocument27 pagesOt PDFZain ShariffNo ratings yet
- Alterations in The Surgical Patient Updated 2010Document122 pagesAlterations in The Surgical Patient Updated 2010zorrotranNo ratings yet
- Cardiac Monitor, ECG and CauterizationDocument28 pagesCardiac Monitor, ECG and CauterizationGlaiza Mae Olivar-ArguillesNo ratings yet
- Supraglottic Airway Devices A Review in A New Era of Airway Management 2155 6148 1000647Document9 pagesSupraglottic Airway Devices A Review in A New Era of Airway Management 2155 6148 1000647Riris SihotangNo ratings yet
- History of FluorosDocument2 pagesHistory of FluorosEvi DianNo ratings yet
- Management of Hypoxia During AnaesthesiaDocument5 pagesManagement of Hypoxia During AnaesthesiaNurhafizahImfista100% (1)
- Ivc FilterDocument15 pagesIvc FilterashishNo ratings yet
- Atls SpineDocument11 pagesAtls SpineRonald David EvansNo ratings yet
- Operating TheatreDocument26 pagesOperating TheatreStephen Pilar PortilloNo ratings yet
- Initial Assessment and ManagementDocument8 pagesInitial Assessment and ManagementAlvin De LunaNo ratings yet
- Suction SystemsDocument11 pagesSuction SystemscatatanNo ratings yet
- Introduction To Trauma: LSU Medical Student Clerkship, New Orleans, LADocument31 pagesIntroduction To Trauma: LSU Medical Student Clerkship, New Orleans, LAnandangNo ratings yet
- Fumigation in Operation TheatresDocument22 pagesFumigation in Operation TheatresUtkarsh RaiNo ratings yet
- Surgical Drains and TubesDocument3 pagesSurgical Drains and TubesYusra ShaukatNo ratings yet
- 03 Anaesthesia Machine PDFDocument0 pages03 Anaesthesia Machine PDFjuniorebindaNo ratings yet
- Liver Segments Explained With MnemonicDocument13 pagesLiver Segments Explained With Mnemonicmyat252100% (1)
- 2020-07-07 Reconstructive Ladder FlapDocument96 pages2020-07-07 Reconstructive Ladder FlapTonie AbabonNo ratings yet
- 15Document21 pages15Tyson Easo JonesNo ratings yet
- AERB Guidelines RadiologyDocument4 pagesAERB Guidelines RadiologyTejinder100% (1)
- Percutaneous Nephrostomy: Last Updated: January 3, 2003Document5 pagesPercutaneous Nephrostomy: Last Updated: January 3, 2003Alicia EncinasNo ratings yet
- Post Op CareDocument7 pagesPost Op CareJeraldien Diente TagamolilaNo ratings yet
- Type of DialysisDocument11 pagesType of DialysisGail Leslie HernandezNo ratings yet
- Aspirador QuirurgicoDocument20 pagesAspirador QuirurgicoStanley LozaNo ratings yet
- Infection Control in ORDocument10 pagesInfection Control in ORaaminah tariqNo ratings yet
- Basic Chest X-Ray Interpretation (5minutes Talk) : DR - Alemayehu (ECCM R1)Document35 pagesBasic Chest X-Ray Interpretation (5minutes Talk) : DR - Alemayehu (ECCM R1)Alex beharuNo ratings yet
- Flap Reconstruction of The Abdominal WallDocument8 pagesFlap Reconstruction of The Abdominal WallDian AdiNo ratings yet
- Sudan Communicable Disease ProfileDocument123 pagesSudan Communicable Disease ProfileGalaleldin AliNo ratings yet
- Report in Respiratory SuctioningDocument29 pagesReport in Respiratory SuctioningWendy EscalanteNo ratings yet
- Post Cardiac Arrest CareDocument20 pagesPost Cardiac Arrest CareJayita Gayen Dutta100% (1)
- Mic Cabg Procedure PDFDocument12 pagesMic Cabg Procedure PDFprofarmah6150No ratings yet
- Atls MedscapeDocument5 pagesAtls MedscapeCastay GuerraNo ratings yet
- Ot PDFDocument11 pagesOt PDFAnukrit McgregorNo ratings yet
- 06 List of Day Care ProceduresDocument4 pages06 List of Day Care Proceduresanurag1309No ratings yet
- Planning An Operation Theatre ComplexDocument4 pagesPlanning An Operation Theatre ComplexRaviraj PisheNo ratings yet
- Pneumatic Tube Systems For Hospitals Englisch LowDocument5 pagesPneumatic Tube Systems For Hospitals Englisch LowVincent P Nam100% (1)
- Pneumonectomy Management PDFDocument6 pagesPneumonectomy Management PDFMurali BalaNo ratings yet
- Intravenous CannulationDocument9 pagesIntravenous CannulationjeorjNo ratings yet
- Anterior AbdominalDocument9 pagesAnterior AbdominalTAMBAKI EDMONDNo ratings yet
- Mesentric IschemiaDocument27 pagesMesentric Ischemiawalid ganodNo ratings yet
- Indications of JP DrainsDocument9 pagesIndications of JP DrainsDelbrynth MitchaoNo ratings yet
- Wound Drain Tube Management v2Document17 pagesWound Drain Tube Management v2PriyaNo ratings yet
- Care of DrainsDocument28 pagesCare of DrainschandhomepcNo ratings yet
- Electrical in Medical LocationDocument32 pagesElectrical in Medical LocationengrrafNo ratings yet
- Beat Tonsil BookDocument19 pagesBeat Tonsil BookXheni MeleNo ratings yet
- Auratus Hybrid Striped Bass, Morone Hybrid Saxatilis M. Chrysops and Ocellated River Stingray, Potamotrygon MotoroDocument7 pagesAuratus Hybrid Striped Bass, Morone Hybrid Saxatilis M. Chrysops and Ocellated River Stingray, Potamotrygon MotoroMiguel Ángel Gallego DomínguezNo ratings yet
- Northern Trust - Whiteabbey Hospital Site PlanDocument1 pageNorthern Trust - Whiteabbey Hospital Site PlanFloyd PriceNo ratings yet
- OBG Picture Based Discussion 01Document48 pagesOBG Picture Based Discussion 01Dheeraj Nandal0% (1)
- American Society of Hematology 2018 Guidelines For Management of Venous Thromboembolism Optimal Management of Anticoagulation TherapyDocument35 pagesAmerican Society of Hematology 2018 Guidelines For Management of Venous Thromboembolism Optimal Management of Anticoagulation TherapyBladimir CentenoNo ratings yet
- Procedure Sick Bay 2017Document6 pagesProcedure Sick Bay 2017Syed FareedNo ratings yet
- Botanic Drugs 1917 PDFDocument408 pagesBotanic Drugs 1917 PDFUkefácil Ukelele FacilónNo ratings yet
- Health Belief ModelDocument3 pagesHealth Belief ModelPrem Deep100% (1)
- Massage in The Ear or AuriculoterapyDocument4 pagesMassage in The Ear or Auriculoterapytelemasajes100% (3)
- Comer Emergency Department (ED) Clinical Guidelines: Diabetic Ketoacidosis (DKA) - Moderately Severe To SevereDocument6 pagesComer Emergency Department (ED) Clinical Guidelines: Diabetic Ketoacidosis (DKA) - Moderately Severe To SevereChristelle Malaluan CalumpitNo ratings yet
- CNS Case PresentationDocument9 pagesCNS Case Presentation073-NAGULAN SHIVAKUMARNo ratings yet
- PIS DR SamiDocument1 pagePIS DR SamiSami HassanNo ratings yet
- ConvoDocument44 pagesConvoLun Ding0% (1)
- Food Preservation - Pasteurization 13.02.17Document13 pagesFood Preservation - Pasteurization 13.02.17Shania Moesha AlexanderNo ratings yet
- Jugal Kishore's CardrepertoryDocument26 pagesJugal Kishore's Cardrepertorydipgang7174No ratings yet
- Suspension ExamplesDocument3 pagesSuspension ExamplesOula HatahetNo ratings yet
- Botox Issues ReferenceList Pacesetter April 2020Document16 pagesBotox Issues ReferenceList Pacesetter April 2020Amr Mohamed GalalNo ratings yet
- Docking Dan Modifikasi Struktur Senyawa Baru Turunan ParasetamolDocument5 pagesDocking Dan Modifikasi Struktur Senyawa Baru Turunan ParasetamolRiki AfriyadiNo ratings yet
- SOP 5 Template Standard Operating Procedure For Prescribing A Controlled Drug and The CollectioDocument5 pagesSOP 5 Template Standard Operating Procedure For Prescribing A Controlled Drug and The CollectioMarianne HilarioNo ratings yet
- KHS Investigation Report 07 24 12Document10 pagesKHS Investigation Report 07 24 12sunnews820No ratings yet
- Mercury Drugs Vs Judge de LeonDocument2 pagesMercury Drugs Vs Judge de LeonSherwinBriesNo ratings yet
- Manajemen Terpadu Dislipidemia PDFDocument25 pagesManajemen Terpadu Dislipidemia PDFregina fristasariNo ratings yet
- Bessette, Absolon, and Coralie M. Rousseau. Scoliosis: Causes, Symptoms and Treatment, Nova Science PublishersDocument183 pagesBessette, Absolon, and Coralie M. Rousseau. Scoliosis: Causes, Symptoms and Treatment, Nova Science PublishersDaniel MitevNo ratings yet
- Answer 2Document21 pagesAnswer 2bakesami100% (1)
- Medical EthicsDocument3 pagesMedical EthicsJona MagudsNo ratings yet
- Pidato Bahasa InggrisDocument12 pagesPidato Bahasa InggrisAlltopAmriya100% (1)