Professional Documents
Culture Documents
Cystectomy - Surgical MNGT (Case Pres)
Cystectomy - Surgical MNGT (Case Pres)
Uploaded by
Mel RodolfoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cystectomy - Surgical MNGT (Case Pres)
Cystectomy - Surgical MNGT (Case Pres)
Uploaded by
Mel RodolfoCopyright:
Available Formats
SURGICAL MANAGEMENT
CYSTECTOMY
Cystectomy is a medical term for surgical removal of all or part of the urinary bladder. It
may also be rarely used to refer to the removal of a cyst, or the gallbladder. The most common
condition warranting removal of the urinary bladder is bladder cancer.
[1]
After the bladder has been
removed, an Ileal conduit urinary diversion is necessary. An alternative to this method is to
construct a pouch from a section of ileum or colon, which can act as a form of replacement bladder,
storing urine until the patient desires to release it, which can be achieved by either abdominal
straining or self catheterisation. Future treatment for this condition may involve a full replacement
with an artificial bladder.
Mayo surgeons most commonly perform a cystectomy to treat bladder cancer that has spread into
the bladder wall. They may also perform a cystectomy to treat recurring superficial or treatment-
resistant bladder cancer, as well as other conditions. Options may include:
Partial cystectomy. In this procedure, also called a segmental cystectomy, surgeons remove the
tumor and only a portion of the bladder. Doctors perform this procedure when your bladder will
likely be able to continue to work normally.
Radical cystectomy. In a radical cystectomy, surgeons remove your entire bladder. This is more
common than a partial procedure because bladder cancer is often found when the disease is so
advanced that partial removal isn't possible. For men, radical cystectomy usually involves
removing the bladder, prostate and glands that help produce semen (seminal vesicles). For
women, radical cystectomy usually involves removing the uterus, ovaries and sometimes part of
the vagina. If you undergo this surgery, you may also have lymph nodes removed for
examination. Removal of the lymph nodes has been shown to improve survival for people
undergoing cystectomy.
For both radical and partial cystectomy, surgeons can perform the procedure using one of these
methods:
Traditional (open) procedure. Surgeons use a traditional abdominal incision.
Minimally invasive robotic surgery. During robotic surgery, the surgeon uses a computer that
remotely controls small instruments attached to a robot, with improved precision. The surgeon
works while viewing highly magnified 3-D images of your body on a monitor. Use of several
smaller incisions can decrease scarring and speed recovery.
http://www.mayoclinic.org/cystectomy/types.html
BILATERAL TUBAL LIGATION
What is a Bilateral Tubal Ligation?
A Bilateral Tubal Ligation (BTL) is a surgical procedure that involves blocking the fallopian tubes to
prevent the ovum (egg) from being fertilized. It can be done by cutting, burning or removing
sections of the fallopian tubes or by placing clips on each tube.
When is it used?
A BTL is used when a woman wants to prevent pregnancy. It is considered a permanent form of
birth control, although in some cases it can be reversed. There can be damage to the tubes after
reversal, so this decision should not be made quickly.
How do I prepare for a BTL?
You will have this procedure in the outpatient surgery center or in the main hospital if you have just
delivered a baby. You will not be able to eat or drink anything after midnight the day before your
surgery. This procedure is done laparoscopically or immediately following a cesarean section. If you
are taking any medications, you should discuss these with your doctor to see when you should stop
them.
What happens during the procedure?
You will be given general anesthesia which will put you to sleep. One incision will be made in the
umbilicus (belly button) and three small incisions will be made in the lower abdomen. Gas is
pumped into the abdomen in order to help Dr. Hardy see the uterus, ovaries and fallopian tubes. A
laparoscope is a telescopic instrument that is used to locate the fallopian tubes. Once the tubes are
exposed, a small section of each tube is cut free and removed. The severed ends are ligated
burned with a cautery tool or clips may be placed on each tube. The skin is closed with sutures
that will dissolve and steristrips on the outside that may be removed after 1 week.
What happens after the procedure?
You will be moved to the recovery room while the anesthesia is wearing off. Your pain will be
controlled with pain medications and any side effects will be addressed. You will be able to go home
that day if you were scheduled for an outpatient surgery. If you have this procedure done after
delivery, you will be discharged according to your postpartum care.
You may experience pain that radiates to your shoulder. This is caused from the gas that was used
during the procedure. You may use an electric heating pad, drink warm beverages and walk to help
alleviate this pain. You may bathe and shower as usual. You may wash the incision gently with mild
unscented soap.
You will be given prescription pain medication to use for 2 to 7 days after the procedure. A stool
softener may also help alleviate or prevent constipation. You will be given 2 weeks to recover from
the procedure. Avoid sex or exercising until your postoperative appointment. You may resume
driving after you are not taking any narcotic pain medication
What are the benefits of this procedure?
You do not have the risks associated with hormones for birth control.
You have a more permanent form of birth control.
http://www.atlanticobgyn.com/bilateral-tubal-ligation/
PROCEDURE
Tubal ligation is considered major surgery requiring the patient to undergo general anesthesia. It is
advised that women should not undergo this surgery if they currently have or have had a history of
bladder cancer. After the anesthesia takes effect, a surgeon will make a small incision at each side
of, but just below the navel in order to gain access to each of the 2 fallopian tubes. With traditional
tubal ligation, the surgeon severs the tubes, and then ties (ligates) them off thereby preventing the
travel of eggs to the uterus. Other methods include using clips or rings to clamp them shut, or
severing and cauterizing them. Tubal ligation is usually done in a hospital operating-room setting.
The corresponding male surgical sterilization procedure known as Vasectomy is considered minor
surgery done with local anesthesia and typically done in an out-patient setting.
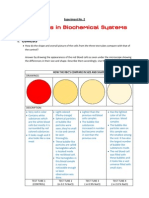
TUBAL LIGATION METHODS
Bipolar Coagulation. The most popular method of laparoscopic female sterilization, this method
uses electrical current to cauterize sections of the fallopian tube.
Monopolar Coagulation. Less common than Bipolar Coagulation, Monopolar Coagulation uses
electrical current to cauterize the tube together, but also allows radiating current to further damage
the tubes as it spreads from the coagulation site. Many cases involve a cutting of the tubes after the
procedure.
Fimbriectomy. By removing a portion of the fallopian tube closest to the ovary, fimbriectomy
eliminates the ovarys ability to capture eggs and transfer them to the uterus.
Irving Procedure. This procedure calls for placing two ligatures (sutures) around the fallopian
tube and removing the segment of tubing between the ligatures. Then to complete the procedure,
the ends of the fallopian tubes are connected to the back of the uterus and the connective tissue
respectively.
Tubal Clip. The tubal clip (Filshie Clip or Hulka Clip) technique involves the application of a
permanent clip onto the fallopian tube. Once applied and fastened, the clip disallows transference of
eggs to the ovary.
Tubal Ring. The silastic band or tubal ring method involves a doubling over of the fallopian tubes
and application of a silastic band to the tube.
Pomeroy Tubal Ligation. In this method of tubal ligation, a loop of tube is strangled with a
suture. Usually, the loop is cut and the ends cauterized or burned. This type of tubal ligation is
often referred to as cut, tied, and burned.
Essure Tubal Ligation. In this method of tubal ligation, two small metal and fiber coils are placed
in the fallopian tubes. After insertion, scar tissue forms around the coils, blocking off the fallopian
tubes and preventing sperm from reaching the egg.
Adiana Tubal Ligation. In this method of tubal ligation, two small silicone pieces that were placed
in the fallopian tubes. During the procedure, the health care provider heated a small portion of each
fallopian tube and then inserted a tiny piece of silicone into each tube. After the procedure, scar
tissue formed around the silicone inserts, blocking off the fallopian tubes and preventing sperm
from reaching the egg. The procedure can no longer be performed due to a lawsuit and judgment
brought by the company responsible for Essure.
[10]
http://en.wikipedia.org/wiki/Tubal_ligation
Prepared by:
BERNAFLOR N. PIELAGO
BSN III-B
HYSTERECTOMY
Abdominal hysterectomy is a surgical procedure that removes your uterus through an incision in
your lower abdomen. Your uterus or womb is where a baby grows if you're pregnant. A
partial hysterectomy removes just the uterus, and a total hysterectomy removes the uterus and the
cervix.
Sometimes a hysterectomy includes removal of one or both ovaries and fallopian tubes, a procedure
called total hysterectomy with salpingo-oophorectomy (sal-ping-go-o-of-uh-REK-tuh-me).
Hysterectomy can also be performed through an incision in the vagina (vaginal hysterectomy) or by
a laparoscopic or robotic surgical approach which uses long, thin instruments passed through
small abdominal incisions. Abdominal hysterectomy may be recommended over other types of
hysterectomy if you have a large uterus or if your doctor wants to check other pelvic organs for
signs of disease.
Types of Hysterectomies:
Total Hysterectomy involves removing both the body of the uterus and the cervix, which is
the lower part of the uterus. Hysterectomy can be abdominally, vaginally and
laparoscopically.
Total Abdominal Hysterectomy with Bilateral Salpingo-Oophorectomy involves removing the
uterus, cervix, bilateral fallopian tubes and ovaries.
Subtotal Hysterectomy only the upper part of the uterus is removed, but the cervix is not.
Tubes and ovaries may or may not be removed.
Radical Hysterectomy is reserved for serious disease such as cancer. The entire uterus and
usually both tubes and ovaries as well as the pelvic lymph nodes are removed through the
abdomen. Since cancer is unpredictable, other organs or parts of other systems are
sometimes removed as well.
Purpose
After a Hysterectomy, a woman can no longer have children and menstruation stops. If you
have cancer of the uterus or ovaries or hemorrhage (uncontrollable bleeding) of the uterus,
this operation may save your life. The operation is done as a treatment and to improve the
quality of life:
Complications
Bleeding
Infection
Blood clots
Damage to organs
Hernia formation
Large scars
Reaction to the anesthesia
What to expect before the procedure
You must be admitted a day before the scheduled procedure
Consents must be secured
Nothing by mouth for 8 hours prior to the time of the procedure
If ordered by the physician, cleaning or fleet enema will be given for further bowel
preparation.
You will also meet with the anesthesiologist to go over details of the method of anesthesia
to be used.
Insertion of Intravenous Line
You will undergo diagnostic exams as ordered by the physician like Complete blood count,
blood typing and urinalysis.
Pre-operative medicines and antibiotics will be administered.
Instructions regarding change of gown, removal of jewelries, dentures, contact lenses, hair
accessories, nail polish, and make up will be given.
An hour before the scheduled operation, you will be wheeled down to the delivery room.
Abdominoperineal prep (shaving) will be done.
What to expect during the procedure
Prior to the time of operation, you will be wheeled in to the operating room where a
surgical nurse will do the necessary preparations such as placement of cardiac leads,
hooking to the cardiac monitor, oxygen administration thru nasal cannula, and placement of
leggings
Before the procedure, for verification that the right patient and right procedure will be
done, Signing in will be called, wherein you will be asked to state in your full name, date of
birth, name of your surgeon and anesthesiologist, as well as the procedure to be done.
After the induction of anesthesia, a curtain will be raised over your mid section and you
arms will be outstretched in order for the anesthesiologist and nurse to have access to your
I.V.
A Foley catheter will be inserted. This is not a painful procedure, and if you have an
anesthesia in you won't feel it at all.
Once a sufficient level of anesthesia has been reached, the initial cut into the skin will be
made. The surgeon will then explore the abdominal cavity for disease or trauma.
Alternatively, samples of various tissues and/or fluids may be removed for further analysis.
What to expect after the procedure
After the surgeon closes, you will be wheeled into recovery where you will be observed for
two hours as the anesthetic wears off.
You will be hooked to the cardiac monitor to check your vital signs, and you will also be
hooked to the oxygen.
Since Hysterectomy is a major operation, discomfort and pain from the surgical incision are
greatest during the first few days after surgery, but medicine is available to reduce these
symptoms.
Post-operative medicines will be given to you. Depending upon the nature of your surgery
and your doctor's assessment of your pain, you probably will be given a pain drip to address
the pain.
Turning from side to side is advised. A tight abdominal binder is applied to support the
incision.
The foley catheter will remain until further orders.
Nothing per mouth as ordered by the physician/s, usually for 24 hours or after passed out
of flatus.
After the recovery period, you will be examined and will be transferred to your room if
there are no complications.
Discharge instructions will be given to you by your bedside nurse.
At Home:
During the first two weeks, avoid tiring activities such as lifting of heavy objects.
Slowly increase your activities. Begin with light chores, short walks, and some driving.
Depending on your job, you may be able to return to work.
To promote healing, eat a diet rich in fruits and vegetables.
Try to avoid constipation by:
o Eating high-fiber foods
o Drinking plenty of water
o Using stool softeners if needed
Take proper care of the incision site. This will help to prevent an infection.
Follow your doctor's instructions
When to call your doctor
After you leave the hospital, contact your doctor if any of the following occurs:
Fever or chills
Redness, swelling, increasing pain, excessive bleeding, or any discharge from the incision
site
Increasing pain or pain that does not go away
Your abdomen becomes swollen or hard to the touch
Diarrhea or constipation that lasts more than 3 days
Bright red or dark black stools
Dizziness or fainting
Nausea and vomiting
Cough, shortness of breath, or chest pain
Pain or difficulty with urination
Swelling, redness, or pain in your leg
TOTAL ABDOMINAL HYSTERECTOMY WITH AND WITHOUT BILATERAL SALPINGO-
OOPHORECTOMY
Total abdominal hysterectomy is utilized for benign and malignant disease where removal of the
internal genitalia is indicated. The operation can be performed with the preservation or removal of
the ovaries on one or both sides. In benign disease, the possibility of bilateral and unilateral
oophorectomy should be thoroughly discussed with the patient. Frequently, in malignant disease,
no choice exists but to remove the tubes and ovaries, since they are frequent sites of
micrometastases.
In general, the modified Richardson technique of intrafascial hysterectomy is used.
The purpose of the operation is to remove the uterus through the abdomen, with or without
removing the tube and ovaries.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5811)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Experiment No. 2Document5 pagesExperiment No. 2Berna Pielago67% (6)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- PE (Basic Steps)Document6 pagesPE (Basic Steps)Berna Pielago100% (7)
- SeaWorld Orca MothersDocument6 pagesSeaWorld Orca MotherswithoutmethereisnouNo ratings yet
- Case Study HELLPDocument7 pagesCase Study HELLPJovirtNo ratings yet
- Summary Evaluation of Laboratory WorksDocument2 pagesSummary Evaluation of Laboratory WorksBerna PielagoNo ratings yet
- Health Perception and Management PatternDocument3 pagesHealth Perception and Management PatternBerna PielagoNo ratings yet
- T5R1Document1 pageT5R1Berna PielagoNo ratings yet
- Health Perception and Management PatternDocument3 pagesHealth Perception and Management PatternBerna PielagoNo ratings yet
- Bed Making TesdaDocument5 pagesBed Making TesdaSusan JilhanoNo ratings yet
- Introduction To Modern NursingDocument44 pagesIntroduction To Modern NursingHarold AngelesNo ratings yet
- Basic Statistics PDFDocument89 pagesBasic Statistics PDFdivyaNo ratings yet
- Malala Yousufzai Discharged From Birmingham Hospital - NHS Press ReleaseDocument2 pagesMalala Yousufzai Discharged From Birmingham Hospital - NHS Press ReleasestoryfulNo ratings yet
- Braket H4Document32 pagesBraket H4leonor maria zamora montes100% (1)
- Puberty PDFDocument6 pagesPuberty PDFjoshNo ratings yet
- Aula 4 - The Effect of An Electronic SBAR Comunication Toll PDFDocument5 pagesAula 4 - The Effect of An Electronic SBAR Comunication Toll PDFGabriela AfonsoNo ratings yet
- Casualty RimaDocument4 pagesCasualty RimariskyNo ratings yet
- Part B - Health Facility Briefing & Design 157Document27 pagesPart B - Health Facility Briefing & Design 157John Dryden Pillos ClerigoNo ratings yet
- Trauma Care ManualDocument348 pagesTrauma Care Manualsdavis76100% (3)
- Introduction Review, Asking Question, GrammarDocument24 pagesIntroduction Review, Asking Question, GrammarNonny Tentia MNo ratings yet
- Volume 3 Issue 2 2023: Newport International Journal of Public Health and Pharmacy (Nijpp)Document11 pagesVolume 3 Issue 2 2023: Newport International Journal of Public Health and Pharmacy (Nijpp)KIU PUBLICATION AND EXTENSIONNo ratings yet
- Tetanus - The DiseaseDocument6 pagesTetanus - The Diseasemanjunath mamathaNo ratings yet
- Peter Bellezza DPM, MS Midori Higashi DPM Jeffrey Christensen, DPM, FACFASDocument1 pagePeter Bellezza DPM, MS Midori Higashi DPM Jeffrey Christensen, DPM, FACFASbaoNo ratings yet
- My CV Dec2018Document6 pagesMy CV Dec2018Bader AlqattanNo ratings yet
- 001 Laboratory Scope of ServiceDocument5 pages001 Laboratory Scope of ServiceMichael FernandezNo ratings yet
- Paediatric OrthopaedicDocument77 pagesPaediatric Orthopaedicdr_asalehNo ratings yet
- Discover The Positive Effects Prenatal Yoga: About The Holistic CenterDocument2 pagesDiscover The Positive Effects Prenatal Yoga: About The Holistic CenterJerico RelopezNo ratings yet
- (1890) Oil of Dog (Ambrose Bierce)Document3 pages(1890) Oil of Dog (Ambrose Bierce)StelioPassarisNo ratings yet
- Lecture Notes Sp13 PDFDocument198 pagesLecture Notes Sp13 PDFFlorentina GasttiNo ratings yet
- EndosDocument8 pagesEndosAli ZainNo ratings yet
- Root Canal Sealers / Orthodontic Courses by Indian Dental AcademyDocument51 pagesRoot Canal Sealers / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Trends & Issues in MSN NursingDocument41 pagesTrends & Issues in MSN NursingRajesh Sharma100% (3)
- What Is An Intravenous Pyelogram (IVP) ? How Should I Prepare?Document4 pagesWhat Is An Intravenous Pyelogram (IVP) ? How Should I Prepare?vindictive666No ratings yet
- List of Occupation-AustraliaDocument7 pagesList of Occupation-AustraliaBipinNo ratings yet
- P ArtographDocument17 pagesP ArtographPrincess RoseNo ratings yet
- Choosing Your Positions During Labour and Birth:: A Decision Aid For Women Having A Vaginal BirthDocument21 pagesChoosing Your Positions During Labour and Birth:: A Decision Aid For Women Having A Vaginal BirthCatur ErtyNo ratings yet
- Genetics of Mucopolysaccharidosis Type II Treatment & Management Medical CareDocument5 pagesGenetics of Mucopolysaccharidosis Type II Treatment & Management Medical CareBoNo ratings yet