Professional Documents
Culture Documents
Abg 1
Abg 1
Uploaded by
Phillip MartinezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Abg 1
Abg 1
Uploaded by
Phillip MartinezCopyright:
Available Formats
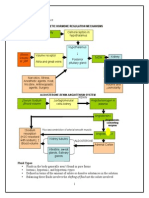
ABG INTERPRETATION
ABG Interpretation
First, does the patient have an acidosis or an
alkalosis
Second, what is the primary problem
metabolic or respiratory
Third, is there any compensation by the
patient respiratory compensation is
immediate while renal compensation takes
time
ABG Interpretation
It would be extremely unusual for either the
respiratory or renal system to
overcompensate
The pH determines the primary problem
After determining the primary and
compensatory acid/base balance, evaluate
the effectiveness of oxygenation
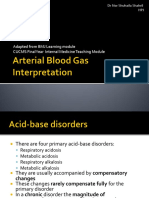
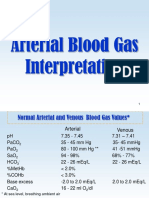
Normal Values
pH 7.35 to 7.45
paCO
2
36 to 44 mm Hg
HCO
3
22 to 26 meq/L
Abnormal Values
pH < 7.35
Acidosis (metabolic
and/or respiratory)
pH > 7.45
Alkalosis (metabolic
and/or respiratory)
paCO
2
> 44 mm Hg
Respiratory acidosis
(alveolar hypoventilation)
paCO
2
< 36 mm Hg
Respiratory alkalosis
(alveolar hyperventilation)
HCO
3
< 22 meq/L
Metabolic acidosis
HCO
3
> 26 meq/L
Metabolic alkalosis
Putting It Together - Respiratory
So
paCO
2
> 44 with a pH < 7.35 represents a respiratory
acidosis
paCO
2
< 36 with a pH > 7.45 represents a respiratory
alkalosis
For a primary respiratory problem, pH and paCO
2
move in the opposite direction
For each deviation in paCO
2
of 10 mm Hg in either
direction, 0. 08 pH units change in the opposite
direction
Putting It Together - Metabolic
And
HCO
3
< 22 with a pH < 7.35 represents a
metabolic acidosis
HCO
3
> 26 with a pH > 7.45 represents a
metabolic alkalosis
For a primary metabolic problem, pH and
HCO
3
are in the same direction, and paCO
2
is also in the same direction
Compensation
The bodys attempt to return the acid/base
status to normal (i.e. pH closer to 7.4)
Primary Problem Compensation
respiratory acidosis metabolic alkalosis
respiratory alkalosis metabolic acidosis
metabolic acidosis respiratory alkalosis
metabolic alkalosis respiratory acidosis
Expected Compensation
Respiratory acidosis
Acute the pH decreases 0.008 units for
every 1 mm Hg increase in paCO
2
; HCO
3
0.1-1 mEq/liter per 10 mm Hg paCO
2
Chronic the pH decreases 0.003 units for
every 1 mm Hg increase in paCO
2
; HCO
3
1.1-3.5 mEq/liter per 10 mm Hg paCO
2
Expected Compensation
Respiratory alkalosis
Acute the pH increases 0.008 units for
every 1 mm Hg decrease in paCO
2
; HCO
3
0-2 mEq/liter per 10 mm Hg paCO
2
Chronic - the pH increases 0.017 units for
every 1 mm Hg decrease in paCO
2
; HCO
3
2.1-5 mEq/liter per 10 mm Hg paCO
2
Expected Compensation
Metabolic acidosis
paCO
2
= 1.5(HCO
3
) + 8 (2)
paCO
2
1-1.5 per 1 mEq/liter HCO
3
Metabolic alkalosis
paCO
2
= 0.7(HCO
3
) + 20 (1.5)
paCO
2
0.5-1.0 per 1 mEq/liter HCO
3
Classification of primary acid-base
disturbances and compensation
Acceptable ventilatory and metabolic acid-base
status
Respiratory acidosis (alveolar hypoventilation) -
acute, chronic
Respiratory alkalosis (alveolar hyperventilation) -
acute, chronic
Metabolic acidosis uncompensated,
compensated
Metabolic alkalosis uncompensated, partially
compensated
Acute Respiratory Acidosis
paCO
2
is elevated and pH is acidotic
The decrease in pH is accounted for entirely
by the increase in paCO
2
Bicarbonate and base excess will be in the
normal range because the kidneys have not
had adequate time to establish effective
compensatory mechanisms
Acute Respiratory Acidosis
Causes
Respiratory pathophysiology - airway
obstruction, severe pneumonia, chest
trauma/pneumothorax
Acute drug intoxication (narcotics, sedatives)
Residual neuromuscular blockade
CNS disease (head trauma)
Chronic Respiratory Acidosis
paCO
2
is elevated with a pH in the
acceptable range
Renal mechanisms increase the excretion of
H
+
within 24 hours and may correct the
resulting acidosis caused by chronic
retention of CO
2
to a certain extent
Chronic Respiratory Acidosis
Causes
Chronic lung disease (BPD, COPD)
Neuromuscular disease
Extreme obesity
Chest wall deformity
Acute Respiratory Alkalosis
paCO
2
is low and the pH is alkalotic
The increase in pH is accounted for entirely
by the decrease in paCO
2
Bicarbonate and base excess will be in the
normal range because the kidneys have not
had sufficient time to establish effective
compensatory mechanisms
Respiratory Alkalosis
Causes
Pain
Anxiety
Hypoxemia
Restrictive lung
disease
Severe congestive
heart failure
Pulmonary emboli
Drugs
Sepsis
Fever
Thyrotoxicosis
Pregnancy
Overaggressive
mechanical ventilation
Hepatic failure
Uncompensated Metabolic
Acidosis
Normal paCO
2
, low HCO
3
, and a pH less
than 7.30
Occurs as a result of increased production
of acids and/or failure to eliminate these
acids
Respiratory system is not compensating by
increasing alveolar ventilation
(hyperventilation)
Compensated Metabolic Acidosis
paCO
2
less than 30, low HCO
3
, with a pH
of 7.3-7.4
Patients with chronic metabolic acidosis are
unable to hyperventilate sufficiently to
lower paCO
2
for complete compensation to
7.4
Elevated AG
Metabolic Acidosis
Causes
Ketoacidosis - diabetic, alcoholic, starvation
Lactic acidosis - hypoxia, shock, sepsis,
seizures
Toxic ingestion - methanol, ethylene glycol,
ethanol, isopropyl alcohol, paraldehyde,
toluene
Renal failure - uremia
Normal AG Metabolic Acidosis
Causes
Renal tubular acidosis
Post respiratory
alkalosis
Hypoaldosteronism
Potassium sparing
diuretics
Pancreatic loss of
bicarbonate
Diarrhea
Carbonic anhydrase
inhibitors
Acid administration
(HCl, NH
4
Cl, arginine
HCl)
Sulfamylon
Cholestyramine
Ureteral diversions
Effectiveness of Oxygenation
Further evaluation of the arterial blood gas
requires assessment of the effectiveness of
oxygenation of the blood
Hypoxemia decreased oxygen content of blood -
paO
2
less than 60 mm Hg and the saturation is less
than 90%
Hypoxia inadequate amount of oxygen available
to or used by tissues for metabolic needs
Mechanisms of Hypoxemia
Inadequate inspiratory partial pressure of
oxygen
Hypoventilation
Right to left shunt
Ventilation-perfusion mismatch
Incomplete diffusion equilibrium
Assessment of Gas Exchange
Alveolar-arterial O
2
tension difference
A-a gradient
PAO
2
-PaO
2
PAO
2
= FIO
2
(PB - PH
2
O) - PaCO
2
/RQ*
arterial-Alveolar O
2
tension ratio
PaO
2
/PAO
2
arterial-inspired O
2
ratio
PaO
2
/FIO
2
P/F ratio
*RQ=respiratory quotient= 0.8
Assessment of Gas Exchange
ABG A-a grad
PaO
2
PaCO
2
RA 100%
Low FIO
2
N* N
Alveolar hypoventilation N N
Altered gas exchange
Regional V/Q mismatch /N/ N/
Intrapulmonary R to L shunt N/
Impaired diffusion N/ N
Anatomical R to L shunt
(intrapulmonary or intracardiac) N/
* N=normal
Summary
First, does the patient have an acidosis or an
alkalosis
Look at the pH
Second, what is the primary problem metabolic
or respiratory
Look at the pCO
2
If the pCO
2
change is in the opposite direction of the
pH change, the primary problem is respiratory
Summary
Third, is there any compensation by the
patient - do the calculations
For a primary respiratory problem, is the pH
change completely accounted for by the change
in pCO
2
if yes, then there is no metabolic compensation
if not, then there is either partial compensation or
concomitant metabolic problem
Summary
For a metabolic problem, calculate the expected
pCO
2
if equal to calculated, then there is appropriate
respiratory compensation
if higher than calculated, there is concomitant
respiratory acidosis
if lower than calculated, there is concomitant
respiratory alkalosis
Summary
Next, dont forget to look at the
effectiveness of oxygenation, (and look at
the patient)
your patient may have a significantly increased
work of breathing in order to maintain a
normal blood gas
metabolic acidosis with a concomitant
respiratory acidosis is concerning
Case 1
Little Billy got into some of dads
barbiturates. He suffers a significant
depression of mental status and respiration.
You see him in the ER 3 hours after
ingestion with a respiratory rate of 4. A
blood gas is obtained (after doing the
ABCs, of course). It shows pH = 7.16,
pCO
2
= 70, HCO
3
= 22
Case 1
What is the acid/base abnormality?
1. Uncompensated metabolic acidosis
2. Compensated respiratory acidosis
3. Uncompensated respiratory acidosis
4. Compensated metabolic alkalosis
Case 1
Uncompensated respiratory acidosis
There has not been time for metabolic
compensation to occur. As the barbiturate
toxicity took hold, this child slowed his
respirations significantly, pCO
2
built up in
the blood, and an acidosis ensued.
Case 2
Little Suzie has had vomiting and diarrhea for
3 days. In her moms words, She cant
keep anything down and shes runnin out.
She has had 1 wet diaper in the last 24
hours. She appears lethargic and cool to
touch with a prolonged capillary refill time.
After addressing her ABCs, her blood gas
reveals: pH=7.34, pCO
2
=26, HCO
3
=12
Case 2
What is the acid/base abnormality?
1. Uncompensated metabolic acidosis
2. Compensated respiratory alkalosis
3. Uncompensated respiratory acidosis
4. Compensated metabolic acidosis
Case 2
Compensated metabolic acidosis
The prolong history of fluid loss through diarrhea
has caused a metabolic acidosis. The mechanisms
probably are twofold. First there is lactic acid
production from the hypovolemia and tissue
hypoperfusion. Second, there may be significant
bicarbonate losses in the stool. The body has
compensated by blowing off the CO
2
with
increased respirations.
Case 3
You are evaluating a 15 year old female in the ER who was brought in by
EMS from school because of abdominal pain and vomiting. Review of
system is negative except for a 10 lb. weight loss over the past 2
months and polyuria for the past 2 weeks. She has no other medical
problems and denies any sexual activity or drug use. On exam, she is
alert and oriented, afebrile, HR 115, RR 26 and regular, BP 114/75,
pulse ox 95% on RA. Exam is unremarkable except for mild
abdominal tenderness on palpation in the midepigastric region and
capillary refill time of 3 seconds. The nurse has already seen the
patient and has sent off routine blood work. She hands you the
result of the blood gas. pH = 7.21 pCO
2
=
24 pO
2
= 45 HCO
3
= 10
BE = -10 saturation = 72%
Case 3
What is the blood gas interpretation?
Uncompensated respiratory acidosis with severe
hypoxia
Uncompensated metabolic alkalosis
Combined metabolic acidosis and respiratory
acidosis with severe hypoxia
Metabolic acidosis with respiratory compensation
Case 3
Metabolic acidosis with respiratory compensation
This is a patient with new onset diabetes mellitus
in ketoacidosis. Her pulse oximetry saturation and
clinical examination do not reveal any respiratory
problems except for tachypnea which is her
compensatory mechanism for the metabolic
acidosis. The nurse obtained the blood gas sample
from the venous stick when she sent off the other
labs.
You might also like
- ABG InterpretationDocument31 pagesABG Interpretationɹǝʍdןnos100% (12)
- Arterial Blood Gas Analysis - making it easyFrom EverandArterial Blood Gas Analysis - making it easyRating: 4.5 out of 5 stars4.5/5 (4)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Acid Base Balancing ActDocument6 pagesAcid Base Balancing ActjohnkuysNo ratings yet
- Fluid & ElectrolyteDocument26 pagesFluid & Electrolytesanjana bhatia100% (1)
- Arterial Blood GasDocument55 pagesArterial Blood GasRathis Dasan100% (1)
- Acid - Base Balance & Abg AnalysisDocument71 pagesAcid - Base Balance & Abg AnalysisMohan KrishnaNo ratings yet
- Abg PPT NewDocument69 pagesAbg PPT NewMalaka Atapattu100% (3)
- Arterial Blood Gases: Mike Runyon, MD July 15, 2010Document46 pagesArterial Blood Gases: Mike Runyon, MD July 15, 2010mamiraliNo ratings yet
- Lecture 2 - Fluid & Electrolyre Balance 2021Document28 pagesLecture 2 - Fluid & Electrolyre Balance 2021عمار عاشورNo ratings yet
- Blood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSIDocument39 pagesBlood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSISalsabila RahmaNo ratings yet
- Acid Base BalanceDocument45 pagesAcid Base BalanceSameer Ul BashirNo ratings yet
- Abg Interpretation: Marc D. Berg, MD - Devos Children'S Hospital Rita R. Ongjoco, Do - Sinai Hospital of BaltimoreDocument41 pagesAbg Interpretation: Marc D. Berg, MD - Devos Children'S Hospital Rita R. Ongjoco, Do - Sinai Hospital of BaltimoreArianne PulidoNo ratings yet
- Arterial Blood Gases: A Step by Step GuideDocument19 pagesArterial Blood Gases: A Step by Step GuideKathleen Ann50% (2)
- Acid Base Disorders - Lecture 45Document14 pagesAcid Base Disorders - Lecture 45yassin mostafaNo ratings yet
- Acid-Base DisordersDocument35 pagesAcid-Base DisordersAnonymous eson90100% (2)
- Saumya Gupta Moderator: Dr. Vishal GuptaDocument41 pagesSaumya Gupta Moderator: Dr. Vishal Guptaimranqazi11No ratings yet
- ABG MMHG InterpretationDocument92 pagesABG MMHG InterpretationManmeet SNo ratings yet
- ABGS Arterial Blood GasesDocument27 pagesABGS Arterial Blood GasesMuhammad asif samiNo ratings yet
- Acid Base Disorders For Vet. StudentsDocument43 pagesAcid Base Disorders For Vet. StudentsAli H. Sadiek أ.د. علي حسن صديق100% (2)
- Acid Base 2013Document60 pagesAcid Base 2013Belial ZaheuerNo ratings yet
- Acid Base Balance: Carol Johns, MSN, RNDocument36 pagesAcid Base Balance: Carol Johns, MSN, RNkatrinasdNo ratings yet
- AbgDocument8 pagesAbgprecillathoppilNo ratings yet
- ABG Interpretation: - Mark Lee R. TagalaDocument31 pagesABG Interpretation: - Mark Lee R. TagalappsavidalandNo ratings yet
- Acid-Base Balance: Acidosis & AlkalosisDocument30 pagesAcid-Base Balance: Acidosis & AlkalosisrathanNo ratings yet
- Blood Gas Analysis-IH 2014Document26 pagesBlood Gas Analysis-IH 2014ismaangrianiNo ratings yet
- Acid-Base Balance: Graciela Lou F. Mana-Ay, RN, ManDocument68 pagesAcid-Base Balance: Graciela Lou F. Mana-Ay, RN, ManKeshia Joyce LimNo ratings yet
- Arterial Blood GasDocument48 pagesArterial Blood GaslovianettesherryNo ratings yet
- Acid Base Disorders: Mr. Ahmed Alnaji Mbchb. Mrcs 1+2 Palestinian Board G. Surgery European Gaza HospitalDocument60 pagesAcid Base Disorders: Mr. Ahmed Alnaji Mbchb. Mrcs 1+2 Palestinian Board G. Surgery European Gaza Hospitalpt.mahmoudNo ratings yet
- Moderator: Dr. R. K. Yadav (MD) Presented By: Ashish JaisawalDocument47 pagesModerator: Dr. R. K. Yadav (MD) Presented By: Ashish Jaisawalimranqazi11No ratings yet
- Arterial Blood GasesDocument28 pagesArterial Blood Gases091Nurul Nur AkmalNo ratings yet
- Acid-Base Imbalances: Dr. Emmanuel Sandy Department of Chemical Pathology Comahs-UslDocument49 pagesAcid-Base Imbalances: Dr. Emmanuel Sandy Department of Chemical Pathology Comahs-UslVivian Kamara100% (1)
- Blood Gas Analysis: - Arterial Blood Gases MeasuresDocument39 pagesBlood Gas Analysis: - Arterial Blood Gases Measuresapi-19641337No ratings yet
- Abg AnalysisDocument43 pagesAbg AnalysisHakuna MatataNo ratings yet
- Arterial Blood Gas AnalysisDocument46 pagesArterial Blood Gas AnalysisMedi - LecturesNo ratings yet
- Arterial Blood Gas AnalysisDocument32 pagesArterial Blood Gas AnalysisPervinNo ratings yet
- Arterial Blood Gas Analysis Learning Objectives:: Introduction/ OverviewDocument5 pagesArterial Blood Gas Analysis Learning Objectives:: Introduction/ OverviewjanorberteNo ratings yet
- Acid+base+disordersDocument32 pagesAcid+base+disordersWizzy Akor100% (1)
- Hand Out 2 NCM 103 PrelimDocument3 pagesHand Out 2 NCM 103 PrelimLouisa Marie MirandaNo ratings yet
- The Acid Base Balance: Faculty of Medicine Anesthesia and Intensive Care DepartmentDocument36 pagesThe Acid Base Balance: Faculty of Medicine Anesthesia and Intensive Care DepartmentCamelia A. ParuschiNo ratings yet
- Blood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSIDocument39 pagesBlood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSIIQBAL HAKKIKINo ratings yet
- Fluid, Electrolytes, Acid Base BalanceDocument18 pagesFluid, Electrolytes, Acid Base Balanceashdmb217100% (5)
- Arterial Blood Gas Analysis Workshop: Key Teaching ObjectivesDocument8 pagesArterial Blood Gas Analysis Workshop: Key Teaching ObjectivesBayan Abu AlrubNo ratings yet
- Jill Getchell, BS, CCP, LCP, LPNDocument115 pagesJill Getchell, BS, CCP, LCP, LPNapi-301270014No ratings yet
- ABGs InterpretationDocument33 pagesABGs InterpretationHamza DossaNo ratings yet
- Blood Gas Analysis CMEDocument12 pagesBlood Gas Analysis CMEpierhot_11No ratings yet
- Acid Base BalanceDocument40 pagesAcid Base BalanceAyman LatifNo ratings yet
- MPhill Acid Base DisorderDocument28 pagesMPhill Acid Base DisorderUsamaNo ratings yet
- Arterial Blood Gas AnalysisDocument39 pagesArterial Blood Gas AnalysisDick-Jay BustamanteNo ratings yet
- ABIDocument27 pagesABIekramNo ratings yet
- Acid-Base Balance PDFDocument10 pagesAcid-Base Balance PDFinah krizia lague100% (1)
- Acid Base DisordersDocument33 pagesAcid Base DisordersShre RanjithamNo ratings yet
- Interpreting ABG - An Interative Session: Dr. Manjunath Patil Professor, Dept. of Anaesthesiology J.N.Medical CollegeDocument31 pagesInterpreting ABG - An Interative Session: Dr. Manjunath Patil Professor, Dept. of Anaesthesiology J.N.Medical CollegeMadhan Mohan Reddy KatikareddyNo ratings yet
- Arterial Blood Gas AnalysisDocument24 pagesArterial Blood Gas AnalysisDeepika PatelNo ratings yet
- Arterial Blood GasesDocument13 pagesArterial Blood GasesLemuel QueNo ratings yet
- Acid Base ImbalanceDocument50 pagesAcid Base ImbalanceDian Pratiwi BurnamaNo ratings yet
- ABG AnalysisDocument57 pagesABG AnalysisHardik RathodNo ratings yet
- Acid Base Disorders: Hasan Al-Dorzi, MD Pulmonary and Critical Care Consultant, Intensive Care DepartmentDocument47 pagesAcid Base Disorders: Hasan Al-Dorzi, MD Pulmonary and Critical Care Consultant, Intensive Care DepartmentAmjaSaudNo ratings yet
- Acid Base Imbalance 2Document26 pagesAcid Base Imbalance 2Female calmNo ratings yet
- Acid Base BalanceDocument69 pagesAcid Base BalanceAli AttarNo ratings yet
- Arterial Blood Gases Easyas: InterpretingDocument5 pagesArterial Blood Gases Easyas: Interpretingoccam1132No ratings yet
- Metabolic Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandMetabolic Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- TyphoidDocument2 pagesTyphoidjtalan9No ratings yet
- 1) Guide LinesDocument5 pages1) Guide Linesjtalan9No ratings yet
- FLH105 TaperlocDocument16 pagesFLH105 Taperlocjtalan9No ratings yet
- E T IntubationDocument15 pagesE T Intubationjtalan9No ratings yet
- Arterial Blood Gas InterpretationDocument69 pagesArterial Blood Gas InterpretationostuffeNo ratings yet
- Arterial Blood Gas AnalysisDocument28 pagesArterial Blood Gas Analysishendra_darmawan_4No ratings yet
- Synthesis 3 Jay VillasotoDocument6 pagesSynthesis 3 Jay VillasotoJay VillasotoNo ratings yet
- Blood Gas AnalysisDocument39 pagesBlood Gas Analysisjtalan9No ratings yet
- Acid-Base BalanceDocument47 pagesAcid-Base BalanceEmmanuel RocksonNo ratings yet
- Clinical Enzymology: Enzyme Classification and NomenclatureDocument27 pagesClinical Enzymology: Enzyme Classification and NomenclaturePatrick DazaNo ratings yet
- Acid Base BalanceDocument44 pagesAcid Base BalanceKenny JapNo ratings yet
- Electrolytes Used in Acid-Base TheraphyDocument30 pagesElectrolytes Used in Acid-Base TheraphySuresh ThanneruNo ratings yet
- Arterial Blood Gas InterpretationDocument65 pagesArterial Blood Gas InterpretationDaniel AryanNo ratings yet
- Primer On Clinical Acid-Base Problem Solving - DisAMon 2004Document41 pagesPrimer On Clinical Acid-Base Problem Solving - DisAMon 2004Ashley100% (1)
- Cardiac Biomarkers: Cardiac Enzymes and BiomarkerDocument21 pagesCardiac Biomarkers: Cardiac Enzymes and Biomarkeranamika sharmaNo ratings yet
- BSAVA - Interpretation of Arterial Blood Gas - VINDocument5 pagesBSAVA - Interpretation of Arterial Blood Gas - VINvetthamilNo ratings yet
- Common Complications of Iv TherapyDocument63 pagesCommon Complications of Iv TherapyFrancis James RigodonNo ratings yet
- Acid-Base Balance: Graciela Lou F. Mana-Ay, RN, ManDocument68 pagesAcid-Base Balance: Graciela Lou F. Mana-Ay, RN, ManKeshia Joyce LimNo ratings yet
- NIV ProformaDocument10 pagesNIV ProformaWael N Sh GadallaNo ratings yet
- Hydrogen Hydroxide: Acid-Base Balance Overview of Acids and Bases DescriptionDocument15 pagesHydrogen Hydroxide: Acid-Base Balance Overview of Acids and Bases DescriptionElisha WorworNo ratings yet
- Dwnload Full Nursing A Concept Based Approach To Learning Volume 1 2nd Edition Pearson Test Bank PDFDocument36 pagesDwnload Full Nursing A Concept Based Approach To Learning Volume 1 2nd Edition Pearson Test Bank PDFmichaelcalhounjtypaegbnk100% (12)
- Arterial Blood Gas InterpretationDocument9 pagesArterial Blood Gas InterpretationSunny AghniNo ratings yet
- Rhythm QRS Duration Atrial Rate QT Interval Ventricular Rate QRS Axis (Compute)Document10 pagesRhythm QRS Duration Atrial Rate QT Interval Ventricular Rate QRS Axis (Compute)Luis PadillaNo ratings yet
- CopdDocument47 pagesCopdNingshesil Ny HermantNo ratings yet
- Internal Medicine - Phase 3: Important Legal InformationDocument19 pagesInternal Medicine - Phase 3: Important Legal InformationClaire YabaNo ratings yet
- Laboratory ValuesDocument12 pagesLaboratory ValuesJaney Co100% (2)
- Practice Test Questions Downloaded From FILIPINO NURSES CENTRALDocument5 pagesPractice Test Questions Downloaded From FILIPINO NURSES CENTRALFilipino Nurses CentralNo ratings yet
- Physioex 8Document4 pagesPhysioex 8Dayanna MartínezNo ratings yet
- Disorders of Acid Base BalanceDocument1 pageDisorders of Acid Base BalanceLyn Domingo EllaquezNo ratings yet
- اسئلة وزارة الصحة للالتحاق ببرنامج الاقامة والامتيازDocument68 pagesاسئلة وزارة الصحة للالتحاق ببرنامج الاقامة والامتيازAhmad HamdanNo ratings yet
- Clinical Manifestations and Diagnosis of Obesity Hypoventilation Syndrome - UpToDateDocument26 pagesClinical Manifestations and Diagnosis of Obesity Hypoventilation Syndrome - UpToDateacesacesNo ratings yet
- Overview of Child Health NursingDocument22 pagesOverview of Child Health NursingnatalieshirleyNo ratings yet
- Sas 18Document4 pagesSas 18Sistine Rose Labajo100% (1)