Professional Documents
Culture Documents
Mother Self-Care: Postpartum Teaching Plan
Mother Self-Care: Postpartum Teaching Plan
Uploaded by
Maemae SumalinogOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mother Self-Care: Postpartum Teaching Plan
Mother Self-Care: Postpartum Teaching Plan
Uploaded by
Maemae SumalinogCopyright:
Available Formats
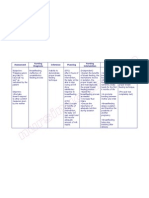
POSTPARTUM TEACHING PLAN
MOTHER SELF-CARE
After Delivery Changes:
The New Beginning
Body returns to normal after labor & delivery
Continued support from healthcare team
o Helps you to relax
o Enables you to learn what to expect
o Helps you gain confidence
o Allows you to be comfortable
Be aware of transitions in which you find yourself, your
baby, & your family
DO NOT hesitate to contact your healthcare provider with
questions or concerns
Normal Changes
Body begins to return to its non-pregnant state
Usually takes 4-6 weeks
The Uterus
Immediately after delivery it is the size of a grapefruit
Takes about 6 weeks to return to its normal size and weight
Afterbirth Pain
Caused by uterus contractions as it shrinks
Most noticeable 3-4 days following delivery
Pronounced during breastfeeding
Helps to shrink uterus & reduce blood loss
Lochia (Vaginal Discharge)
Drainage from birth canal following delivery
Immediately following birth like menstrual flow
3-4 days discharge becomes watery/pale
2nd week its thicker & more yellow
4 weeks discharge decreases
Smells fleshy, musty, or earthy not offensive
Occasional cramping, brief bleeding, passing a clot is
normal
Profuse/persistent bleeding or foul odor notify health care
provider
Birth Canal
Returns to previous condition by end of 3rd week
Pelvic floor muscles return to normal in 6-7 weeks
Kegel exercises help speed healing
Breastfeeding mothers more likely to have vaginal dryness
& discomfort during sex 4-6 months after delivery
Menstrual Cycle
Breast feeding can cause delay
1st period within 7-9 wks
If Nursing within 12 wks or after breast feeding
Bladder
Urinating may initially be difficult following delivery
(catheter may be required)
Try to empty bladder every 3-4 hours
Eliminate large amounts of urine 1st few days after delivery
Bowels
First bowel movement occurs 2-3 days
Possible constipation/hemorrhoids
o Exercise, fiber, and H2O can prevent constipation
If breast feeding consult health care provider before
taking medications (including laxatives)
Bowel Elimination
Maintain normal bowel function by drinking 6-8 glasses of
water daily
Weight Loss
Immediately after delivery common to weigh same or more
than you did prior to delivery
Should occur in postpartum period as bodys fluid levels
return to normal
Muscle and Joints
1st 1-2 days following delivery muscle aches & fatigue
o Shoulders, neck, & arms
Joint stiffness of hands common
Abdominal muscles weak, soft, & flabby
Skin Changes
Disappear gradually several months after childbirth
o Dark line of lower abdomen
o Blotchy appearance of face
Varicose Veins
1st 6 weeks following delivery
o Elevate leg & use elastic support hose
Hemorrhoids
Cold compress, topical ointments, pain medications
Stool softener/laxative
Severe pain may cause constipation
Eye Hemorrhages
Clears by itself within a few weeks
Emotional Changes
Normal to feel overwhelmed
Takes 2-3 months to establish a routine
Ask for/accept help during early postpartum period
Baby Blues & Postpartum Depression
BABY BLUES
Can occur within 1st few days after giving birth
o Impatience, irritability, crying
o Feelings generally come & go quickly
POSTPARTUM DEPRESSION
Can start 2nd or 3rd day after delivery
May take several weeks or months to develop
Many of baby blues symptoms present, but more intense
List of symptoms (pg. 9)
These symptoms are not signs of weakness or inadequacy
Contact health care provider immediately at the onset
of these changes or if you think you are depressed
Self Care Tips:
Getting Around On Your Own
Moving around minimizes the risk of blood clots
Helps with bladder & bowel function
Hygiene & Episiotomy
Change sanitary pads frequently (avoid infection)
Perineum rinsed /cleaned with lukewarm water 2-3 times
daily and after urination/bowel movement
Pat perineum to dry
Washing/wiping front to back (prevent contamination)
POSTPARTUM TEACHING PLAN
Usually require 4 or more weeks to heal
Mothers with a Cesarean Birth
Keep incision dry (instructed by health care team)
Red, swollen, tender, warm to touch/draining notify health
care provider
Bathing/Showers
When client is able to ambulate
Tub baths safe after 2nds day following delivery
Vaginal douching not recommended until check-up
Mothers Warning Signs & Reportable Symptoms
If you experience any of the following, contact your
health care provider immediately (please see list at
bottom of pg. 10)
Rest & Sleep
Fatigue follows delivery, sleep when possible
Use relaxation exercises
Know & understand suggestions to assist you at home (list
on pg. 11)
ASK FOR WHAT YOU NEED
Resuming Sex
Discuss resuming sex with your partner
Vaginal dryness & diminished vaginal lubrication are
expected (use water soluble cream or jelly)
Set aside time for each other (without baby)
If problems persist, contact HCP
Nutrition
Eat extra 300 calories per day (500 if breastfeeding)
Eat well balanced diet from 5 food groups
Find balance between food & physical activity
Know the limits on fats, sugars, & salt
If breastfeeding, avoid tobacco, alcohol, & non-essential
medications (can affect baby)
The New Father
May feel neglected/lonely, keep communication open
Healthy adult relationships important for babys emotional
well-being, as well as your own
FEEDING YOUR NEWBORN
Breastfeeding:
Skin-to-Skin Connection (Kangaroo Care)
Regulates babys temperature, blood sugar, & heart rate
Babies more alert & cry less during this time
Breastfeed better/longer & stay awake during feeding
Benefits of Breastfeeding (see list on pg. 17)
Babys immune system benefits from breastmilk
Anatomy of the Breast
Milk producing cells, milk ducts, nipple, & areola
Nipple stimulated by baby suckling (milk glands produce
milk)
Milk flows from ducts to nipple (let-down)
Let-down sensations/list of causes (pg. 18)
Preparation of the Breast for Nursing
Expose breasts to room air daily, avoid soap nipple/areola
See complete list of guidelines on pg. 19
Nipple Types
pinch test nipples should stand erect, not flat/inward
Supply & Demand
Milk regulated; more removed=more made & vice versa
Breastfeeding Relationship
3 Cs calm, comfortable, & close
Breastfeeding: When & How
Initiate within 1st hour of birth, ask questions, & watch for
early feeding cues
Correct Latch On
Position on breast w/all of nipple & good amount of areola
in mouth
Guideline on pg. 22 for tips/techniques
Burping
Over the shoulder
Lying belly down across your lap
Sitting in your lap with chin supported
Guidelines & Technical Pointers for Frequency & Duration of
Feeding
8-12 feedings/24 hours, approximately every 1-3 hours, &
may cluster feed
Nurse until baby shows signs of being full
Offer both breasts each feeding (stimulates milk
production)
How Do I Know the Baby is Getting Enough to Eat?
Be attentive (know babys signs of hunger & being full)
Weight gain of 4-7 ounces/week = sign of proper feeding
Time of Awareness & Perseverance:
Engorgement
3-4 days postpartum breasts become swollen & heavier, this
lessens in 24-48 hours
Effective treatment measures pg. 25
Expressing Breastmilk
Done manually with hands or with special breast pump
Breast Massage
Key is to trigger the let-down response
Wash hands, relax, warm compress, use pads of fingers
Circular motion from chest to nipple, bend forward &
gently shake breast
Hand Expression
Technique/instructions listed on pg. 26
Sore Nipples
Tenderness expected, should resolve by day 7-10
Usually due to improper positioning & latch-on
DO NOT LET PROBLEM GET WORSE (call health care
provider)
Cracked Nipples
Due to improper positioning & latch-on or traumatic
removal from breast (properly break suction before
removing baby from breast)
Blocked Ducts
Pea-sized lumps under skin of breast & sore to the touch
Causes/treatments listed on pg. 27
Mastitis
Unrelieved persistent blocked duct that becomes inflamed
& breast infection possible (immediate medical attention)
Symptoms/treatment listed on pg. 27 & 28
Dietary Requirements for the Mother
POSTPARTUM TEACHING PLAN
Nursing moms need 500 extra calories/day, drink 6-8
glasses of fluid daily
Supplemental Feedings for Your Baby
Not necessary if milk is well-established & have good
breastfeeding relationship
Storage of Breastmilk
Label & date container, never microwave or boil, throw
away remaining unused breastmilk
Breastfeeding Questions
Are my breasts too small?
Will my breasts leak all the time?
How can I breastfeed if I have had breast surgery?
How can my partner find me attractive?
How can I breastfeed if I am taking certain medications?
Answers to these questions are listed on pg. 30
A Fathers Concern: Note to Dad
Become close to baby (diapering, bathing, cuddling)
Going Back to Work & Continuing to Breastfeed
Pump milk & save, breastfeed when with baby & feed
pumped milk when away from baby
Feeding Choices
Formula from cows milk or soy proteins
Bottle feeding steps/instructions on pg. 32
CARING FOR YOUR NEWBORN
General Care
Regular well-baby exams monitor growth & development
Routine immunizations
Visitors
Do not feel obligated to entertain, keep baby away from
contagious illness, & keep touching of baby by others to
minimum
Weight Loss & Gain
Infants lose 5-8% of birth weight at first, regain birth
weight by day 10, double by 6th month, & triple by 1 year
Sleep Patterns
Infants wake for feedings every 2-3 hours until 6-8 wks old
You sleep when baby sleeps
4-8 wks of age baby may sleep through 1-2 nighttime
feedings
Teething
Most babies begin at 6-7 months (some 2-4 months)
Bowel Function
Changes in number, consistency, & color of stools normal
Constipation is small, firm, pebble-like stool
Contact health care provider if baby has diarrhea
Diaper Rash
Change diaper when baby wets or has bowel movement
Skin Care
Newborn acne common, baby sheds dead skin-leave alone
Sponge Bath
Until circumcision or umbilical cord has healed
Follow steps/instructions on pg. 37-38
Umbilical Cord
Falls off by itself in 1-4 weeks (allow it to do so)
Clean around site with warm water or alcohol
If oozing, foul odor, redness, or fever present contact HCP
Circumcision
Removal of foreskin surrounding head of penis
Apply ointment to tip of penis (each diaper change) for 1st
few days, tip of penis may be red & have yellow crust (do
not wash off)
Contact HCP if notice unusual swelling, oozing, bleeding
Jaundice
Causes yellow appearance of skin & common in newborns
Physiologic jaundice not harmful, usually respond without
medical treatment, & may last up to 1 week
Phototherapy & bililite usually used to treat
Taking Your Babys Temperature
Taken under arm or with ear thermometer
Keeping Your Baby Safe
See list of safety measures on pg. 40
Car Seat Safety
Baby needs car seat for ride home from hospital
Place in middle of back seat
NEVER place rear-facing seat in front seat (airbag)
Rear facing car seat until at least 2 years of age
Keep car window closed & door locked nearest baby
NEVER leave infant/child unattended in car
Immunizations
Protects child from variety of diseases
Begin at birth & must be given prior to 12-18 months
Continue at different times for rest of life
Babys Warning Signs & Reportable Symptoms
BLUE LIP COLOR CALL 911
Yellow skin/eyes, listlessness, temperature of 100 degrees
or more, difficulty breathing
See complete list on pg. 43
Sudden Infant Death Syndrome (SIDS)
Place baby on back to sleep (nighttime & nap)
On firm mattress (not on pillow, waterbed, sofa)
Remove fluffy, soft, loose bedding from crib
Keep babys head & face uncovered while sleeping
Do not let baby become overheated during sleep
Shaken Baby Syndrome
DO NOT SHAKE YOUR BABY
If babys basic needs met & still crying stop, think, reach
out for help
Signs & symptoms of shaken baby syndrome along with
helpful tips if you do become frustrated on pg. 45
POSTPARTUM TEACHING PLAN
You might also like
- Ebook PDF Child Development An Active Learning Approach 3rd Edition PDFDocument41 pagesEbook PDF Child Development An Active Learning Approach 3rd Edition PDFmike.casteel80798% (43)
- Inpatient Obstetric Nurse Exam Prep 2020-2021: A New Study Guide for Certification Including 300 Test Questions and Answers with Full Explanations (RNC-OB)From EverandInpatient Obstetric Nurse Exam Prep 2020-2021: A New Study Guide for Certification Including 300 Test Questions and Answers with Full Explanations (RNC-OB)No ratings yet
- Nursing Care Plan For PostpartumDocument5 pagesNursing Care Plan For PostpartumTheeya Quigao91% (11)
- Nursing Postpartum Care PlanDocument7 pagesNursing Postpartum Care PlanBecky Kipling100% (9)
- 8 Point Postpartum Assessment WorksheetDocument2 pages8 Point Postpartum Assessment WorksheetSoni Ali100% (2)
- Teaching Plan For A Post Partum MotherDocument12 pagesTeaching Plan For A Post Partum Motherpatrickarvin100% (2)
- Maternal-Newborn Nursing DeMYSTiFieD: A Self-Teaching GuideFrom EverandMaternal-Newborn Nursing DeMYSTiFieD: A Self-Teaching GuideNo ratings yet
- DischargeDocument4 pagesDischargePatricia Franco100% (1)
- Bleeding During Pregnancy and Nursing Care PlanDocument17 pagesBleeding During Pregnancy and Nursing Care PlanLizcelle Bihasa86% (7)
- Postpartum Maternal Physical Assessment SummaryDocument6 pagesPostpartum Maternal Physical Assessment SummaryAlyanna Evangelista100% (2)
- ACOG Practice Bulletin No 183 Postpartum-Hemorrhage-2017Document19 pagesACOG Practice Bulletin No 183 Postpartum-Hemorrhage-2017Leslie GuzmanNo ratings yet
- Gravida - The Number of Pregnancies That o Progesterone Deprivation TheoryDocument27 pagesGravida - The Number of Pregnancies That o Progesterone Deprivation TheoryRoshin Tejero100% (1)
- Newborn Careplan 9-15-2011Document17 pagesNewborn Careplan 9-15-2011Brittany Wood100% (1)
- Maternal & Child Practice Exam 9 (Intrapartum)Document29 pagesMaternal & Child Practice Exam 9 (Intrapartum)Lot Rosit100% (1)
- Maternity NursingDocument40 pagesMaternity NursingClarissa Guifaya100% (2)
- Careplan NewBornDocument2 pagesCareplan NewBornVic DangNo ratings yet
- NSVD Case StudyDocument11 pagesNSVD Case StudyMichael UrrutiaNo ratings yet
- Maternal and Child NursingDocument30 pagesMaternal and Child NursingJack Bisarra Sanchez0% (1)
- NCP: Labor Stage 2 (Expulsion)Document15 pagesNCP: Labor Stage 2 (Expulsion)Javie100% (1)
- Maternal ExamsDocument168 pagesMaternal Examshopeyang100% (2)
- Nursing Care Plan Breast Feeding IneffectiveDocument1 pageNursing Care Plan Breast Feeding Ineffectivederic88% (8)
- Practice Test Maternity-Nsg 100 ItemsDocument21 pagesPractice Test Maternity-Nsg 100 ItemsPaul Christian P. Santos, RN100% (21)
- NCP (Acute Pain, Episiotomy)Document6 pagesNCP (Acute Pain, Episiotomy)Jenny AjocNo ratings yet
- BubbleDocument12 pagesBubblekarloeguiareyesNo ratings yet
- PostpartumDocument7 pagesPostpartummaryNo ratings yet
- Postpartum Health TeachingDocument3 pagesPostpartum Health TeachingMarisCachero100% (1)
- Nursing Care PlanDocument7 pagesNursing Care Planrockerespi1283No ratings yet
- Postpartum Care PlanDocument6 pagesPostpartum Care Planallie-jones-6489100% (27)
- Postpartum Health TeachingDocument8 pagesPostpartum Health TeachingMsOrange96% (24)
- Postpartum CareDocument13 pagesPostpartum CareChristian100% (11)
- Nursing Care Plan-OBDocument20 pagesNursing Care Plan-OBPriscilla Paula Benavidez100% (3)
- Health Teaching Plan BreastfeedingDocument4 pagesHealth Teaching Plan Breastfeedingkev mondaNo ratings yet
- Teaching Plan For BreastfeedingDocument2 pagesTeaching Plan For BreastfeedingEmerson Sambo100% (6)
- Patterns of FunctioningDocument5 pagesPatterns of FunctioningMhia Mhi-mhi FloresNo ratings yet
- Maternal and Child Health Nursing TestDocument21 pagesMaternal and Child Health Nursing TestAt Day's Ward50% (2)
- Intrapartum CareDocument14 pagesIntrapartum CareChristian80% (5)
- High Risk NewbornDocument4 pagesHigh Risk NewbornWenn Joyrenz ManeclangNo ratings yet
- Components of LaborDocument5 pagesComponents of LaborJeraldine Lindo100% (4)
- Post Partum CareDocument145 pagesPost Partum Carenickybore100% (2)
- Intrapartum QuizletDocument15 pagesIntrapartum Quizletanon_616227840100% (3)
- Ob MaternityDocument46 pagesOb MaternityJohanna Erazo Padilla100% (1)
- Postpartum NCPDocument20 pagesPostpartum NCPapi-370148988% (34)
- Bubbleshe Assessment: BREASTS 1. Palpate Both Breasts ForDocument3 pagesBubbleshe Assessment: BREASTS 1. Palpate Both Breasts Forallyssa joyNo ratings yet
- Newborn Nursing CareplanDocument7 pagesNewborn Nursing CareplanSamantha MillerNo ratings yet
- Nursing Care Plan - Delivery RoomDocument2 pagesNursing Care Plan - Delivery RoomMarivic Misola100% (5)
- Postpartum Discharge Instructions - Howard County General Hospital, Johns Hopkins MedicineDocument7 pagesPostpartum Discharge Instructions - Howard County General Hospital, Johns Hopkins MedicineA.No ratings yet
- Clinical Week 3 - Teaching Plan - BreastfeedingDocument2 pagesClinical Week 3 - Teaching Plan - Breastfeedingapi-273168705No ratings yet
- Nursing ManagementDocument6 pagesNursing ManagementLoraine CastilloNo ratings yet
- Post Partum PeriodDocument31 pagesPost Partum PeriodMay CaballeroNo ratings yet
- Breast Feeding GettingstartedDocument31 pagesBreast Feeding GettingstartedSunny DemandanteNo ratings yet
- Month by MonthDocument28 pagesMonth by MonthChoi Han KimNo ratings yet
- NCM 107 Postpartum Care Guide QuestionDocument6 pagesNCM 107 Postpartum Care Guide QuestionMiguel LigasNo ratings yet
- Postpartum Period HandoutsDocument8 pagesPostpartum Period HandoutsChared LumbaNo ratings yet
- BreastfeedingDocument3 pagesBreastfeedingER RonNo ratings yet
- Care After Birth & F.planningDocument22 pagesCare After Birth & F.planningbangiidamanNo ratings yet
- Antenatal Info Booklet Intuitive BirthDocument32 pagesAntenatal Info Booklet Intuitive Birthapi-223713414No ratings yet
- Breastfeeding Int School NewDocument56 pagesBreastfeeding Int School NewGI SanadaNo ratings yet
- Discharge InstructionsDocument2 pagesDischarge InstructionsNaneth CadisalNo ratings yet
- Breast Feeding Lecture From Tegrity: How The Breast Prepares For BreastfeedingDocument8 pagesBreast Feeding Lecture From Tegrity: How The Breast Prepares For BreastfeedingStephanie KirknerNo ratings yet
- Problems of Breastfeeding: DR Asmaa Fathy Lecturer of Family MedicineDocument47 pagesProblems of Breastfeeding: DR Asmaa Fathy Lecturer of Family MedicineAbdulla1999 AshrafNo ratings yet
- Common Discomforts in Pregnancy: Childbirth (Also Called Labour, Birth, Partus or Parturition) Is The Culmination of ADocument14 pagesCommon Discomforts in Pregnancy: Childbirth (Also Called Labour, Birth, Partus or Parturition) Is The Culmination of Arocel_44No ratings yet
- BreastfeedingDocument30 pagesBreastfeedingKeith Madarang100% (2)
- What Is The Heart Rate?Document3 pagesWhat Is The Heart Rate?6bigstar9No ratings yet
- SBAR WorksheetDocument3 pagesSBAR Worksheet6bigstar9No ratings yet
- 10 Pharmacology QuestionsDocument4 pages10 Pharmacology Questions6bigstar9No ratings yet
- Cleaning ChecklistDocument1 pageCleaning Checklist6bigstar9No ratings yet
- 9780143783572Document206 pages9780143783572Eloisa VianaNo ratings yet
- Practical Guide To Sovereign Birth - 2021Document6 pagesPractical Guide To Sovereign Birth - 2021Eva TuáNo ratings yet
- (Argumentative Essay) : of Teenage Pregnancy School of Public Health, University of Illinois, Chicago, IL 60680Document4 pages(Argumentative Essay) : of Teenage Pregnancy School of Public Health, University of Illinois, Chicago, IL 60680Dham DoñosNo ratings yet
- Principles and Interpretation of CardiotocographyDocument9 pagesPrinciples and Interpretation of CardiotocographyCKNo ratings yet
- Obstetric Ultrasound ScansDocument6 pagesObstetric Ultrasound ScansMichael Spica RampangileiNo ratings yet
- NCM107 MCN - Pedia Nursing SL Semifinal HandoutsDocument17 pagesNCM107 MCN - Pedia Nursing SL Semifinal HandoutsLillabinNo ratings yet
- Diabetes in PregnancyDocument11 pagesDiabetes in PregnancyAlana CaballeroNo ratings yet
- Heart Disease in PregnancyDocument33 pagesHeart Disease in PregnancyKanishka KonarNo ratings yet
- Infant Assessment FormDocument2 pagesInfant Assessment FormteuuuuNo ratings yet
- NNTDocument36 pagesNNTSamzana ShresthaNo ratings yet
- TS Circ025-2015Document11 pagesTS Circ025-2015zaldusalvaradoNo ratings yet
- Botswana EHSP HLSPDocument147 pagesBotswana EHSP HLSPThembaNo ratings yet
- Prenatal History For Clerks Morning EndorsementDocument18 pagesPrenatal History For Clerks Morning Endorsementherbee.berb14No ratings yet
- The Role of Certified Nurse-Midwives and Certified Midwives in Ensuring Women's Access To Skilled Maternity CareDocument51 pagesThe Role of Certified Nurse-Midwives and Certified Midwives in Ensuring Women's Access To Skilled Maternity Caredamar aulia nissaNo ratings yet
- Job DescriptionDocument2 pagesJob DescriptionVaughn Jovi GabrilloNo ratings yet
- Ethico Legal Considerations and Issues in The Care of Sick Mother and Child QuestionsDocument5 pagesEthico Legal Considerations and Issues in The Care of Sick Mother and Child QuestionsQueeny Anne ApilNo ratings yet
- BucensDocument6 pagesBucensEmily GirardNo ratings yet
- Hiv and PregnancyDocument7 pagesHiv and PregnancyCarlos Manuel Carranza VegaNo ratings yet
- Twin To Twin Transfusion Syndrome (TTTS)Document16 pagesTwin To Twin Transfusion Syndrome (TTTS)Angieda SoepartoNo ratings yet
- Analysis of Cesarean Section Rate - According To Robson's 10-Group ClassificationDocument4 pagesAnalysis of Cesarean Section Rate - According To Robson's 10-Group ClassificationMahavir GemavatNo ratings yet
- Cesearean Section FinalDocument62 pagesCesearean Section FinalsanthiyasandyNo ratings yet
- Maternal+Newborn+Matrix+Packet+KEY Spr+2019+ (MR)Document6 pagesMaternal+Newborn+Matrix+Packet+KEY Spr+2019+ (MR)lisa mornoNo ratings yet
- Epidural Analgesia in Labour CA4054 v5Document25 pagesEpidural Analgesia in Labour CA4054 v5АнастасияПлешкоNo ratings yet
- Ladies Doctor in MadhubaniDocument5 pagesLadies Doctor in MadhubaniShubh ParmarNo ratings yet
- Umbilical Cord Coiling: Case Report and Review of LiteratureDocument4 pagesUmbilical Cord Coiling: Case Report and Review of LiteratureHesti hasanNo ratings yet
- An Exploration of The Postpartum Depression Behaviors Among Select First-Time Mother - FINAL RESEARCH PAPER IRREG 3Document127 pagesAn Exploration of The Postpartum Depression Behaviors Among Select First-Time Mother - FINAL RESEARCH PAPER IRREG 3Hermin TorresNo ratings yet
- Case StudyDocument8 pagesCase StudyJay-ann MendozaNo ratings yet
- Guinea Pig DissertationDocument78 pagesGuinea Pig Dissertationcreatingcreator100% (1)