Professional Documents
Culture Documents
1757 1626 0002 0000007983 PDF
1757 1626 0002 0000007983 PDF
Uploaded by
OchaaQOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1757 1626 0002 0000007983 PDF
1757 1626 0002 0000007983 PDF
Uploaded by
OchaaQCopyright:
Available Formats
Open Access
Case report
Pulmonary miliary tuberculosis complicated with tuberculous
spondylitis; an extraordinary rare association: a case report
Eleni Palama1, Christos Golias1,2, Iosif Illiadis2 and
Konstantinos Charalabopoulos2*
Addresses: 1Department of Medicine and Pulmonary Diseases, Grevena State Hospital, 51100 Grevena, Greece
2
Department of Physiology, Clinical Unit, University of Ioannina Medical Faculty, 13 Solomou Street 452 21 Ioannina, Greece
Email: EP - p.edessa@yahoo.gr; CG - chgkolias@hotmail.com; II - iliadis@gmx.com; KC* - kcharala@cc.uoi.gr
* Corresponding author
Received: 27 May 2009 Accepted: 22 August 2009 Published: 8 September 2009
Cases Journal 2009, 2:7983 doi: 10.4076/1757-1626-2-7983
This article is available from: http://casesjournal.com/casesjournal/article/view/7983
2009 Palama et al.; licensee Cases Network Ltd.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0),
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
In the last decade a significant rise in the prevalence of tuberculosis as well as in its extrapulmonary
manifestations is detected worldwide. The central nervous system, the genitourinary tract, the organs
of the abdomen and the skeletal system, are common sites of infection. Misdiagnosis and delay in
treatment are common events. Herein, we present a case of a 78-year-old man non-smoker, with
miliary tuberculosis complicated with tuberculous spondylitis. The patient presented with anemia and
a left shoulder pain, accompanied by rigor and fever 37.5C-38C of one month duration. This entity
is extremely rare, since only two similar cases have been reported in the English literature according
to PubMed search.
Introduction
During the last years it is more than evident that the
prevalence of pulmonary and extrapulmonary tuberculosis
(TB), mainly in western European countries, has risen
significantly. The aetiology of this phenomenon is multifactorial. The main parameters are the development of
drug-resistant strains of Mycobacterium tuberculosis, aging
population demographics, massive refugee waves from
high prevalence for tuberculosis disease territories, increase
in the number of health care workers exposed to the
disease and the rising number of people with immunosuppression [1,2]. Diagnosis of extrapulmonary tuberculosis is often difficult. The genitourinary system is a usual
extrapulmonary location. The most common manifestation of abdominal tuberculosis is lymphadenopathy and
ileocecal involvement is present in 80%-90% of patients.
Central nervous system tuberculosis involvement has
various manifestations, such as meningitis, tuberculoma,
abscess, cerebritis, and miliary tuberculosis. Spinal tuberculosis accounts for approximately 50% of cases of
skeletal tuberculosis [3]. The most common location is
L1 (lumbar) vertebra although more than one vertebral
bodies are typically affected. The disease process most
often begins in the anterior part of the vertebral body
adjacent to the end plate. Later on the disk space is
involved via a number of routes. Potts disease, is a rare
presentation of extrapulmonary tuberculosis that affects
spine, vertebrae and intevertebral joints. The disease is
named after Percivall Pott (1714-1788) description, a
surgeon in London, U.K. The disease is also called
Page 1 of 5
(page number not for citation purposes)
Cases Journal 2009, 2:7983
tuberculous spondylitis and is mostly localized in the
thoracic portion of the spine. Herein, we present a case of
miliary tuberculosis complicated by tuberculous spondylitis, which was confronted by administration of regressive
treatment before the establishment of the definite
diagnosis.
Case presentation
A 78-year-old Caucasian man of Greek origin, 80 kg in
weight, 174 cm in height, non-smoker, was referred to
Grevena State Hospital, Greece, complaining for a left
shoulder pain, which was aggravated by movement. He
also reported rigor and fever between 375 and 38C,
persisting for one month. Ten days before his first
admission, he was examined by an orthopaedic surgeon
and had received analgesic-anti-inflammatory drugs without any clinical improvement. From his personal medical
history, the patient reported multiple medical visits
complaining of persistent cough and abundant purulent
sputum without fever for years. Due to these symptoms he
was subjected to two CT scans of the thorax and one
fiberoptic bronchoscopy without any conclusive results.
For the last two years, he was thought to suffer from
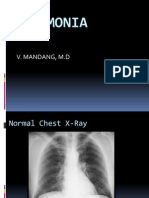
episodes of chronic bronchitis. On admission, a posteroanterior chest radiograph was performed which revealed
multiple diffuse small opacities at both lungs (Figure 1),
which prompted further investigation. Physical examination revealed temperature 38.3C, heart rate 100 beats/min,
18 inspirations/min, and blood pressure 110/60 mmHg.
Auscultation of the lungs was not conclusive; some
fine crackles were audible. White blood cell (WBC)
count was 16.2 109/L, with 86.3% neutrophils, 4.3%
lymphocytes, 7.7% monocytes, 1.6% eosinophils). Platelets
(PLT):512000/mm3, haematocrit (Ht):29.1%, erythrocyte
Figure 1. Postero-anterior chest radiograph revealing
multiple diffuse small opacities at both lungs.
http://casesjournal.com/casesjournal/article/view/7983
sedimentation rate (ESR) 102 mm/h and C-reactive protein
20.97 mg/dl (normal value < 0.8 mg/dl). Biochemical tests
revealed increased transaminases with serum glutamic
oxaloacetic transaminase (SGOT): 132 IU, serum glutamic
pyruvic transaminase (SGPT): 90 IU and hypoalbuminaemia with serum albumins 2.30 g/dL, total protein 5.90 g/dl
and lactate dehydrogenase (LDH): 149 IU/L. Urine test was
normal. Tuberculin skin reaction was negative. Consecutive
blood cultures were negative. Chest computer tomography
(CT) showed lymphadenopathy of the mediastinum, a
mass of smooth consistency laterally to the left at the level
of T2 (thoracic) vertebra, accompanied by osteolytic
erosions of the vertebral bodies of the second to the fifth
thoracic vertebrae (Figure 2). Additionally, multiple bilaterally diffused opacities giving the picture of bud in tree
(Figure 3) and a very small bubble filled with air, were
revealed. The radiologists diagnosis was miliary tuberculosis complicated with tuberculous spondylitis accompanied by a small lung abscess. The abdomen and cerebral
CT were normal. Gram stain and cultures for common
bacteria were taken from sputum secretions. They were
negative for Mycobacterium tuberculosis. Bronchoscopy one
month later was negative for endobronchial mass and non
revelatory for tuberculosis; however, an atrophy of the
mucosa was noted. On cytology, bronchial aspirate was
negative at cultivation for Kochs bacillus; a polymerase
chain reaction (PCR) was also negative. Antituberculous
chemotherapy, with isoniazid, rifampicin, and ethambutol,
was initiated from the first day of admission. After 3 days
of hospitalization, a repeated chest CT revealed improvement of findings. Clinical improvement was noted after the
first week of therapy. Ht increased towards normal limits
Figure 2. CT scan of the thoracic cage-vertebrae showing
(arrow) mass of smooth consistency laterally to the left at the
level of T2 (thoracic) vertebra accompanied by osteolytic
damage (erosions) of the vertebral bodies.
Page 2 of 5
(page number not for citation purposes)
Cases Journal 2009, 2:7983
http://casesjournal.com/casesjournal/article/view/7983
Figure 3. CT scan image of the pulmonary parenchyma
showing multiple bilaterally diffused opacities giving the
picture of bud in tree.
and ESR was significantly decreased. Transaminasemia was
diminished. The patient after his discharged followed
the anti-TB therapy for one year. During this period,
he was followed up periodically by a pneumonologist.
Four months later, chest radiograph and thoracic CT
showed a significant improvement. On the 12th month
of therapy, thoracic CT revealed a complete remission
(Figures 4 and 5).
Discussion
Miliary tuberculosis (or disseminated TB) is a form of
tuberculosis which is characterized by wide dissemination
into the human body and by the tiny size of the lesions
(1-5 mm). It is caused by the widespread hematogenous
dissemination of Mycobacterium tuberculosis. Classic miliary
TB is defined as millet-like (mean 2 mm, range 1-5 mm)
seeding of TB bacilli in the lung, as evidenced on chest
radiography. Miliary TB may occur in an individual organ
(very rare, <5%) or may affect any number of organs
throughout the whole body (>90%), including brain,
lungs, liver, and spleen. It is a complication of 1-3% of all
TB cases [4].
Miliary TB may mimic many diseases. Symptoms including fever, night sweats, weight loss, hematologic abnormalities, cough, pleurisy, dyspnea, and hemoptysis are not
necessarily specific. In some case series, up to 50% of cases
are not diagnosed antemortem. If untreated, the mortality
rate is assumed to be close to 100%, but with early and
appropriate treatment, the mortality rate is reduced to less
than 10%. Therefore, a high index of clinical suspicion is
important to obtain an early diagnosis and to ensure
Figure 4 and 5. CT of the thorax after one year treatment
revealing a healthy patient.
improved clinical outcomes [4]. Early empirical treatment
for possible but not yet definitive miliary TB increases
the likelihood of survival and should never be withheld
while test results are pending.
Skeletal tuberculosis comprises 35% of cases presenting
extrapulmonary tuberculous manifestations. Skeletal
tuberculosis includes entities such as spinal tuberculosis
(Potts disease), articular tuberculosis, Poncets disease
(rare, acute sterile polyarthritis associated with visceral
involvement) and tuberculous osteomyelitis.
Tuberculosis of the spine is an uncommon form of
tuberculosis occurring in less than 1% of patients with
tuberculosis [5,6]. Typical radiographic changes indicative of Potts disease include vertebral destruction and
narrowing of the intervertebral space seen on plain
radiographs. Correlative CT and magnetic resonance
Page 3 of 5
(page number not for citation purposes)
Cases Journal 2009, 2:7983
imaging (MRI) could aid substantially in the diagnosis of
spinal TB due to their ability to show lytic lesions and
adjacent abscess formation. CT scan could be considered
the most useful radiologic tool both for the diagnosis and
determining the extent of the disease. In our patient CT
scan revealed positive findings such as anterior vertebral
body destruction and paraspinal abscess. In addition, the
diagnosis may be confirmed by CT guided needle
aspiration biopsy. The samples obtained are assessed
with stains for acid fast bacilli, culture and histological
examination. It is essential prompt diagnosis to be
established and early treatment to be administered in
order to prevent neurological deficit and irreversible
damage [7,8].
Spinal tuberculosis is a chronic and slowly progresive
disease with prolonged symptomatology. The clinical
history, as well as the presenting condition of the patient,
are important but not always reliable for an immediate
diagnosis. Pain is the most common presenting symptom.
It usually has an insidious onset and may be mechanical in
nature during the initial stages of the disease. Systemic
symptoms arise with progression of disease. Persistent
spinal pain and local tenderness, limitation of spinal
mobility, febrile state, and neurologic complications
including paralytic phenomena, present as the destruction
continues. Other symptoms are reflective of chronic illness
including malaise, weight loss, and fatigue [5]. Diagnosis
is frequently not suspected in patients with no evidence
of extraspinal tuberculosis. The clinical presentation
together with the radiologic appearance of the spine and
a positive tuberculin test may suggest spinal tuberculosis.
The diagnosis must be confirmed by evidence of acid-fast
bacilli from the bone or body fluids. To our best
knowledge, association of miliary tuberculosis and Potts
disease is rather rare with only two cases being reported
in the English literature [8,9]. The physician could easily
miss the diagnosis since this association presents a rare
clinical entity.
Our patient had negative tuberculin skin test as well as
negative sputum cytology and cultivation for Kochs
bacillus after bronchoscopy although he presented pertinacious clinical signs and had rather suspicious radiological findings. The clinical and radiologic features of
extrapulmonary tuberculosis may mimic those of many
diseases. A high index of suspicion is required, especially
in high-risk populations. Although a positive chest radiograph or positive tuberculin skin test supports the
diagnosis, negative results do not exclude the possibility
of extrapulmonary tuberculosis [10].
Anti-TB therapy can minimize morbidity and mortality
but it may be initiated empirically. A negative smear
for acid-fast bacillus, the lack of granulomas on
http://casesjournal.com/casesjournal/article/view/7983
histopathology, and failure to culture Mycobacterium
tuberculosis do not exclude diagnosis. Novel diagnostic
modalities such as adenosine deaminase levels and
polymerase chain reaction method can be useful in certain
forms of extrapulmonary tuberculosis.
In general, the same regimens are used to treat pulmonary
and extrapulmonary tuberculosis, and responses to
antituberculous therapy are similar in patients with
immunosuppressive disease as well as in those without.
Our patient proved to be a potentially easily misdiagnosed case since most of the basic laboratory findings
regarding tuberculosis were negative. Nevertheless, an
empirical initiation of anti-TB treatment based on his
previous and present clinical manifestations was proved
quite beneficial while more extensive laboratory tests
such as CT imaging and CT guided needle aspiration
biopsy were pending.
At present, the treatment of Potts disease remains
controversial. Some advocate conservative treatment with
late spinal fusion and others early spinal fusion followed
by conservative treatment. Surgical treatment should
include anti-TB medication and abscess decompression
[11-13]. Chemotherapy remained the cornerstone in our
patient. During his follow up there was strong evidence of
significant improvement after anti-TB chemotherapy without any neurological deficit or damage been observed.
Conclusion
Tuberculous spondylitis is considered an extremely rare
clinical entity known also as Potts disease. In the era of
modern imaging modalities and effective anti-TB medication, TB appears to be a disease too frequently forgotten
by clinicians and underemphasized by academic scholars.
Misdiagnosis and delay in treatment are common events.
A high degree of suspicion is necessary in order to avoid
delays that may result in irreversible damage and high
mortality rate. In patients presenting with chronic symptomatology of the lungs and suspicious radiological
presentation, the clinicians should proceed to further
clinical and laboratory tests, even if Mantoux test and
sputum cultivation are negative. It is also suggested to
administer treatment before definite diagnosis. Clinicians
should consider Potts disease in the differential diagnosis
of patients with back or shoulder pain and possible
destructive vertebral lesions. Proper diagnosis and anti-TB
treatment with or without surgery will result in cure.
Abbreviations
ESR, erythrocyte sedimentation rate; LDH, lactate dehydrogenase; PCR, polymerase chain reaction; PLT, platelets;
SGOT, serum glutamic oxaloacetic transaminase; SGPT,
serum glutamic pyruvic transaminase; TB, tuberculosis;
WBC, white blood cell.
Page 4 of 5
(page number not for citation purposes)
Cases Journal 2009, 2:7983
http://casesjournal.com/casesjournal/article/view/7983
Consent
Written informed consent was obtained from the patient
for publication of this case report and accompanying
images. A copy of the written consent is available for
review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Authors contributions
EP was involved in patients medical care and in literature
review. CG was involved in patients medical care, in
conception of the report and manuscript preparation. II
was involved in literature review and manuscript editing.
KC was involved in manuscript design and control, being
the supervisor of the team. All authors have read and
approved the final manuscript.
References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
Mehta JB, Dutt A, Harvill L, Mathews KM: Epidemiology of
extrapulmonary tuberculosis: a comparative analysis with
pre-AIDS era. Chest 1991, 99:1134-1138.
Yao DC, Sartoris DJ: Musculoskeletal tuberculosis. Radiol Clin
North Am 1995, 33:679-689.
Moon MS: Tuberculosis of the spine. Spine 1997, 22:1791-1797.
Sharma SK, Mohan A, Sharma A, Mitra DK: Miliary tuberculosis:
new insights into an old disease. Lancet Infect Dis 2005, 5:415-430.
Luzzati R, Giacomazzi D, Danzi MC, Tacconi L, Concia E, Vento S:
Diagnosis, management and outcome of clinically- suspected
spinal infection. J Infect 2009, 58:259-265.
Ramdurg SR, Gupta DK, Suri A, Sharma BS, Mahapatra AK: Spinal
intramedullary tuberculosis: a series of 15 cases. Clin Neurol
Neurosurg 2009, 111:115-118.
Engin G, Acunas B, Acunas G, Tunaci M: Imaging of extrapulmonary tuberculosis. Radiographics 2000, 20:471-488.
Langhorst M, Reeves A, Tarver R, Miller D: Diagnostic case study:
military tuberculosis and Potts disease. Semin Respir Infect 2001,
16:149-151.
Kheir A, Musanda C, Weber P, Colnot F, Bavelele Z, Martinet Y:
Miliary tuberculosis with neurologic involvement: apropos of
a case. Rev Med Interne 1999, 20:1043-1046.
Carette MF, Azencot M, Le Breton C, Breittmayer F, Bigot JM:
Imaging of thoracic tuberculosis. Ann Radiol (Paris) 1994, 37:229238.
Nussbaum ES, Rockswold GL, Bergman TA, Erickson DL,
Seljeskog EL: Spinal tuberculossis: a diagnostic and management challenge. J Neurosurg 1995, 83:243-247.
Rajasekaran S, Shanmugasundaram TK, Parabhakar R,
Dheenadhayalan J, Shetty AP, Shetty DK: Tuberculous lesions of
the lumbosacral region. A 15-year follow-up patients treated
by ambulant chemotherapy. Spine 1998, 23:1163-1167.
Rezai AR, Lee M, Cooper PR, Errico TJ, Koslow M: Modern
management of spinal tuberculosis. Neurosurgery 1995, 36:87-89.
Do you have a case to share?
Submit your case report today
Rapid peer review
Fast publication
PubMed indexing
Inclusion in Cases Database
Any patient, any case, can teach us
something
www.casesnetwork.com
Page 5 of 5
(page number not for citation purposes)
You might also like
- Patient Profile and HistoryDocument3 pagesPatient Profile and Historyrachael89% (19)
- Hydromol Intensive CreamDocument5 pagesHydromol Intensive CreamJesus Carmona VillarrealNo ratings yet
- Running Head: CASE STUDY PAPER 1Document14 pagesRunning Head: CASE STUDY PAPER 1Issaiah Nicolle CeciliaNo ratings yet
- Ginekologi UKDI MANTAP Batch NovemberDocument156 pagesGinekologi UKDI MANTAP Batch NovemberIsmail Eko SaputraNo ratings yet
- Lung Cancer Pathophysio and NCPDocument21 pagesLung Cancer Pathophysio and NCPApple Y.D.No ratings yet
- Appendix Chapter, Sabiston Textbook of SurgeryDocument43 pagesAppendix Chapter, Sabiston Textbook of SurgeryShuo Huang100% (2)
- Delay in Diagnosis of Extra-Pulmonary Tuberculosis by Its Rare Manifestations: A Case ReportDocument5 pagesDelay in Diagnosis of Extra-Pulmonary Tuberculosis by Its Rare Manifestations: A Case ReportSneeze LouderNo ratings yet
- Jurnal Maju DR ArifDocument6 pagesJurnal Maju DR ArifRefta Hermawan Laksono SNo ratings yet
- Coll U 2018 DiagnoseDocument4 pagesColl U 2018 DiagnosevisiniNo ratings yet
- Mediastinal Tuberculous Lymphadenitis Presenting With Insidious Back Pain in A Male Adult: A Case Report and Review of The LiteratureDocument7 pagesMediastinal Tuberculous Lymphadenitis Presenting With Insidious Back Pain in A Male Adult: A Case Report and Review of The Literaturez9tpwgb5nwNo ratings yet
- Cases Journal: Tuberculosis and Venous Thromboembolism: A Case SeriesDocument4 pagesCases Journal: Tuberculosis and Venous Thromboembolism: A Case SeriesDiana Fadly MatondangNo ratings yet
- Pulmonary Balantidium Coli Infection in A Leukemic PatientDocument4 pagesPulmonary Balantidium Coli Infection in A Leukemic PatientNika Dwi AmbarwatiNo ratings yet
- Computed Tomography Findings of Community-Acquired Immunocompetent Patient: A Case ReportDocument4 pagesComputed Tomography Findings of Community-Acquired Immunocompetent Patient: A Case ReportDenta HaritsaNo ratings yet
- Tomographic Findings of Acute Pulmonary Toxoplasmosis in Immunocompetent PatientsDocument5 pagesTomographic Findings of Acute Pulmonary Toxoplasmosis in Immunocompetent Patientshasbi.alginaaNo ratings yet
- F - CMCRep 1 Assy Et Al - 1405Document2 pagesF - CMCRep 1 Assy Et Al - 1405faegrerh5ju75yu34yNo ratings yet
- Up To Date. Tuberculosis Clinical Manifestations and ComplicationsDocument41 pagesUp To Date. Tuberculosis Clinical Manifestations and ComplicationsGuardito PequeñoNo ratings yet
- Multidisciplinary Case-Based Teaching: Prof. S. O 'Neill Dr. D. Royston Dr. S. ShaikhDocument90 pagesMultidisciplinary Case-Based Teaching: Prof. S. O 'Neill Dr. D. Royston Dr. S. Shaikhmynoidanh19No ratings yet
- Rhizomucor Scedosporium: Case ReportDocument6 pagesRhizomucor Scedosporium: Case ReportPaul ColburnNo ratings yet
- Pulmonary Pseudotumoral Tuberculosis in An Old Man: A Rare PresentationDocument3 pagesPulmonary Pseudotumoral Tuberculosis in An Old Man: A Rare PresentationNurhasanahNo ratings yet
- Para-Aortic and Meningitis Tuberculosis: A Case Report: BackgroundDocument10 pagesPara-Aortic and Meningitis Tuberculosis: A Case Report: BackgroundAseta MedikaNo ratings yet
- PROCALCITONINADocument17 pagesPROCALCITONINAaabigutNo ratings yet
- Disseminated Tuberculosis in An AIDS/HIV-Infected Patient: AbstractDocument3 pagesDisseminated Tuberculosis in An AIDS/HIV-Infected Patient: AbstractAmelia Fitria DewiNo ratings yet
- Pulmonary Histoplasmosis Presenting With A Halo Sign On CT in An Immunocompetent PatientDocument2 pagesPulmonary Histoplasmosis Presenting With A Halo Sign On CT in An Immunocompetent PatientSharom R. AlvarezNo ratings yet
- Fungi52 52.9537Document6 pagesFungi52 52.9537Reza PutradinataNo ratings yet
- Radiologic and Clinical Findings in Tuberculous MeningitisDocument6 pagesRadiologic and Clinical Findings in Tuberculous MeningitisAustine OsaweNo ratings yet
- Peritoneal Tuberculosis: ReviewDocument5 pagesPeritoneal Tuberculosis: ReviewEvellyna MeilanyNo ratings yet
- Tuberculosis Mimicking Lung CancerDocument3 pagesTuberculosis Mimicking Lung CancerdyahNo ratings yet
- Case 1: Recurrent Pneumonia in A 15-Year-Old Girl: Article Figures & Data Info & Metrics CommentsDocument7 pagesCase 1: Recurrent Pneumonia in A 15-Year-Old Girl: Article Figures & Data Info & Metrics CommentsJoshua MendozaNo ratings yet
- 51 Uysal EtalDocument4 pages51 Uysal EtaleditorijmrhsNo ratings yet
- Pyothorax-Associated Lymphoma: A Case Report and ReviewDocument10 pagesPyothorax-Associated Lymphoma: A Case Report and ReviewSoukaina SoukainaNo ratings yet
- Pulmonary Tuberculosis in Patients With Chronic Renal Failure at Zagazig University HospitalsDocument6 pagesPulmonary Tuberculosis in Patients With Chronic Renal Failure at Zagazig University HospitalsAnastasia Lilian SuryajayaNo ratings yet
- Cardiac Leptospirosis: Iralphuaborque Md14thbatch Hds DocharlabardaDocument15 pagesCardiac Leptospirosis: Iralphuaborque Md14thbatch Hds DocharlabardaJr. CesingNo ratings yet
- MMC 1Document6 pagesMMC 1ANo ratings yet
- Malignant Mesothelioma Presenting With Unexplained Recurrent Pleurisy EpisodesDocument4 pagesMalignant Mesothelioma Presenting With Unexplained Recurrent Pleurisy EpisodesNurul NingrumNo ratings yet
- Pathophysiological Study of Chronic Necrotizing Pulmonary AspergillosisDocument5 pagesPathophysiological Study of Chronic Necrotizing Pulmonary AspergillosisSyaiful IslamNo ratings yet
- Pneumonia: V. Mandang, M.DDocument44 pagesPneumonia: V. Mandang, M.DMeggy SumarnoNo ratings yet
- Pulmonary Tuberculosis Presenting With Acute Respiratory Distress Syndrome (Ards) : A Case Report and Review of LiteratureDocument5 pagesPulmonary Tuberculosis Presenting With Acute Respiratory Distress Syndrome (Ards) : A Case Report and Review of Literatureamelya asryNo ratings yet
- CytomegaloDocument3 pagesCytomegaloYusi RizkyNo ratings yet
- Crim Em2013-948071Document2 pagesCrim Em2013-948071m.fahimsharifiNo ratings yet
- Potts DiseaseDocument6 pagesPotts DiseaseJefferson ManasanNo ratings yet
- International Journal of Orthopaedics Spinal TuberculosisDocument6 pagesInternational Journal of Orthopaedics Spinal TuberculosisFriyanto Mira MangngiNo ratings yet
- Neumonia Anciano 2014Document8 pagesNeumonia Anciano 2014Riyandi MardanaNo ratings yet
- Hyperimmunoglobulin E (Job's) Syndrome: A Rare Cause of Recurrent Pneumatocele, Lung Abscess and Empyema in ChildhoodDocument5 pagesHyperimmunoglobulin E (Job's) Syndrome: A Rare Cause of Recurrent Pneumatocele, Lung Abscess and Empyema in ChildhoodYan BatlayeriNo ratings yet
- ICU JournalDocument4 pagesICU Journal2080315No ratings yet
- Pulmonary Tuberculosis Literature ReviewDocument5 pagesPulmonary Tuberculosis Literature Reviewafdtvwccj100% (1)
- Pneumothorax: Classification and EtiologyDocument17 pagesPneumothorax: Classification and EtiologyPASMOXNo ratings yet
- A Case of Pulmonary Aspergilloma and ActinomycosisDocument4 pagesA Case of Pulmonary Aspergilloma and ActinomycosisNova PurbaNo ratings yet
- Clinical Features of Medical PneumomediastinumDocument4 pagesClinical Features of Medical PneumomediastinumFerdinando BaehaNo ratings yet
- Jurnal Bahasa InggrisDocument12 pagesJurnal Bahasa InggrisVanessa Angelica SitepuNo ratings yet
- Hemoptysis: A Symptom Not Well Explored in The Primary Care Setting in The Developing WorldDocument4 pagesHemoptysis: A Symptom Not Well Explored in The Primary Care Setting in The Developing WorldAditya RamdaniiNo ratings yet
- Diffuse Large B-Cell Lymphoma Arising From The Lesion ofDocument7 pagesDiffuse Large B-Cell Lymphoma Arising From The Lesion ofFadel AhmadNo ratings yet
- Tuberculosis Spondylitis IIDocument40 pagesTuberculosis Spondylitis IICendraiin MinangkabauNo ratings yet
- Toorthj 6 445Document4 pagesToorthj 6 445Sonia RogersNo ratings yet
- Managing Hemato Oncology Patients in EdDocument6 pagesManaging Hemato Oncology Patients in EdjprakashjjNo ratings yet
- ISM Davit SoesantoDocument14 pagesISM Davit SoesantodavitlieNo ratings yet
- Severe Acute Pancreatitis - A Serious Complication of LeptospirosisDocument3 pagesSevere Acute Pancreatitis - A Serious Complication of LeptospirosisSanda Puspa RiniNo ratings yet
- Gonitis TranslateDocument8 pagesGonitis TranslateYessica DestianaNo ratings yet
- Journal of Medical Case ReportsDocument5 pagesJournal of Medical Case ReportsDumitru RadulescuNo ratings yet
- A Rare Cause of Endocarditis: Streptococcus PyogenesDocument3 pagesA Rare Cause of Endocarditis: Streptococcus PyogenesYusuf BrilliantNo ratings yet
- Case Report: Streptococcus AnginosusDocument4 pagesCase Report: Streptococcus AnginosusIesanu MaraNo ratings yet
- Internal MedicineDocument38 pagesInternal MedicineRoxana Alexandra BogosNo ratings yet
- Infected Pulmonary Infarction Case ReportDocument8 pagesInfected Pulmonary Infarction Case ReportSebastian Felipe Sierra UmañaNo ratings yet
- Clinical Manifestations and Complications of Pulmonary Tuberculosis - UpToDateDocument20 pagesClinical Manifestations and Complications of Pulmonary Tuberculosis - UpToDatedixama9519No ratings yet
- MEningitis TBDocument4 pagesMEningitis TBAlexander TegarNo ratings yet
- Fast Facts: Multiple Sclerosis: A new era of disease modification and treatmentFrom EverandFast Facts: Multiple Sclerosis: A new era of disease modification and treatmentNo ratings yet
- Oc1 PDFDocument8 pagesOc1 PDFIsmail Eko SaputraNo ratings yet
- Sss (2,5 X Kesadaran) + (2 X Muntah) + (2 X Sakit Kepala) + (0,1 X Td. Diastole) - (3 X Ateroma) - 12Document8 pagesSss (2,5 X Kesadaran) + (2 X Muntah) + (2 X Sakit Kepala) + (0,1 X Td. Diastole) - (3 X Ateroma) - 12Ismail Eko SaputraNo ratings yet
- New England Journal Medicine: The ofDocument9 pagesNew England Journal Medicine: The ofIsmail Eko SaputraNo ratings yet
- 686 FullDocument8 pages686 FullIsmail Eko SaputraNo ratings yet
- Report 3Document8 pagesReport 3Ismail Eko SaputraNo ratings yet
- GigiDocument10 pagesGigiIsmail Eko SaputraNo ratings yet
- Managing Hyperglycaemia in People With DKD - Final DraftDocument90 pagesManaging Hyperglycaemia in People With DKD - Final DraftRiched LhyneNo ratings yet
- Breast CancerDocument19 pagesBreast CancerSuresh ThanneruNo ratings yet
- Psoriatic ArthritisDocument33 pagesPsoriatic Arthritisini_etuk100% (1)
- Immunization RecordDocument2 pagesImmunization RecordWillNo ratings yet
- Drug Study and NCPDocument9 pagesDrug Study and NCPDan Dan ManaoisNo ratings yet
- VIRAL MENINGITIS John GreenDocument3 pagesVIRAL MENINGITIS John Greenbradle2005No ratings yet
- Morning Report BangsalDocument9 pagesMorning Report Bangsaltia tamaraNo ratings yet
- Adult Tachycardia With A Pulse Algorithm: Doses/DetailsDocument1 pageAdult Tachycardia With A Pulse Algorithm: Doses/DetailsZakiyahulfahdwNo ratings yet
- Package Leaflet: Information For The User Tamsulosin Hydrochloride 400 Micrograms, Modified-Release Capsule, HardDocument7 pagesPackage Leaflet: Information For The User Tamsulosin Hydrochloride 400 Micrograms, Modified-Release Capsule, HardKahmNo ratings yet
- Tetralogy of FallotDocument3 pagesTetralogy of FallotJohn Mark PocsidioNo ratings yet
- Dyspnea Cardiac Origin STPDocument21 pagesDyspnea Cardiac Origin STPmeiliaNo ratings yet
- Laminitis - Prevention, Diagnosis and Treatment PDFDocument10 pagesLaminitis - Prevention, Diagnosis and Treatment PDFfrankyNo ratings yet
- Sudden Visual Loss - PPTX, EmergencyDocument31 pagesSudden Visual Loss - PPTX, EmergencydesmyyNo ratings yet
- Acute AppendicitisDocument23 pagesAcute AppendicitisPrashant SinghNo ratings yet
- CÂNCER TURBO - Inglês e Português - Report 61 PFIZERDocument49 pagesCÂNCER TURBO - Inglês e Português - Report 61 PFIZERPaulo E MarleneNo ratings yet
- Stroke AssessmentDocument10 pagesStroke AssessmentUzra ShujaatNo ratings yet
- Lab Values and Vital Signs PDFDocument4 pagesLab Values and Vital Signs PDFmike_steven12No ratings yet
- 2021 Dent4060Document14 pages2021 Dent4060Jason JNo ratings yet
- Bino - Lec - Midterm Exam - Yellow - PadDocument11 pagesBino - Lec - Midterm Exam - Yellow - PadDanielle SangalangNo ratings yet
- Cantellops Cueli, N. Soap Note #1 1.14.20Document4 pagesCantellops Cueli, N. Soap Note #1 1.14.20Nicole Juliette CCNo ratings yet
- Drugs Used in Obstetric Emergencies: Vasanthakumari, MSC (N)Document56 pagesDrugs Used in Obstetric Emergencies: Vasanthakumari, MSC (N)revathidadam55555100% (1)
- Level of Breast Cancer Awareness On Fourth-Year FemaleDocument28 pagesLevel of Breast Cancer Awareness On Fourth-Year FemaleLafayette Kirsi NoelNo ratings yet
- Diarrhea in ChildrenDocument6 pagesDiarrhea in ChildrenAdeola AdegboyegaNo ratings yet
- Protein BiosynthesisDocument33 pagesProtein BiosynthesisLucy WijayaNo ratings yet
- GeneticsDocument23 pagesGeneticsmianskNo ratings yet
- Prenatal Cell-Free DNA Screening: Should I Undergo Prenatal Screening For Genetic Conditions?Document2 pagesPrenatal Cell-Free DNA Screening: Should I Undergo Prenatal Screening For Genetic Conditions?Derrick ThompsonNo ratings yet