Professional Documents
Culture Documents
Hyperimmunoglobulin E (Job's) Syndrome: A Rare Cause of Recurrent Pneumatocele, Lung Abscess and Empyema in Childhood
Uploaded by
Yan BatlayeriOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hyperimmunoglobulin E (Job's) Syndrome: A Rare Cause of Recurrent Pneumatocele, Lung Abscess and Empyema in Childhood
Uploaded by
Yan BatlayeriCopyright:
Available Formats
CASE REPORT
Hyperimmunoglobulin E (Jobs) Syndrome: A Rare Cause of Recurrent Pneumatocele, Lung Abscess and Empyema in Childhood
evval Eren, MD1; Akn E. Balc, MD1; Refik lk, MD1; Mehmet Bonak, MD2; M. Nesimi Eren, MD1
1 Department
of Thoracic and Cardiovascular Surgery, Faculty of Medicine, Dicle University, Diyarbakr, of Pediatrics, Faculty of Medicine, Dicle University, Diyarbakr, Turkey
Turkey
2Department
Abstract
The hyperimmunoglobulin E (HIE) or Jobs syndrome is a rare and complex disorder characterized by recurrent staphylococcal lung infections with abscess and pneumatocele formation and chronic eczematoid dermatitis in childhood. Laboratory evaluation reveals consistent elevation of circulating immunoglobulin E levels. This article describes a case of HIE (Jobs) syndrome as a cause of recurrent lung infections with abscess, pneumatocele formation and empyema necessitating tube thoracostomy.
Key words: hyperimmunoglobulin E, Jobs syndrome, recurrent lung abscess, pneumatocele, empyema, eczematoid skin lesions, bone fractures
Introduction
Hyperimmunoglobulin E (HIE) syndrome or Jobs syndrome is a rare and complex disorder characterized by extremely high levels of serum immunoglobulin (Ig) E, recurrent severe staphylococcal lung infections with pneumatocele formation, staphylococcal skin abscess or chronic eczematoid dermatitis (1-6). Patients may also have coarse facial features (5), mild eozinophilia, mucocutaneous candidiasis (7), empyema (8), recurrent bone fractures that may be seen with osteoporosis (9) and variable polymorphonuclear (PMN) leukocyte chemotactic abnormalities have also been reported in this syndrome (3,6). The syndrome was first described in 1966 by Davis et al. (1). Since then, over 150 cases have been described, mainly children (5). We report a case of hyperimmunoglobulin E (Jobs) syndrome who presented with recurrent staphylococcal lung abscess, pneumatoceles and empyema during childhood necessitating recurrent antistaphylococcal antibiotic therapy and drainage by closed tube thoracostomy.
Correspondence: Dr. evval Eren, Dicle niversitesi, Tp Fakltesi Gs Cerrahisi ve Kardiyovaskler Cerrahi Anabilim Dal, Diyarbakr, Trkiye e-Mail: Sevval@dicle.edu.tr
Case Report
A 9-year-old girl was referred to the thoracic surgery unit for evaluation of recurrent bilaterally staphylococcal lung abscess, pneumatoceles and right thoracic empyema.
68
Turkish Respiratory Journal, August 2002, Vol.3, No.2
History revealed that she had a lung infection and pustular skin lesions localized on the neck at the age of 6 months. The patient was treated with an antibiotic. During the succeeding 7 years she had multiple episodes of bronchitis or pneumonia, eczematoid skin lesions on the face, back, buttocks, arms and legs, middle ear infections, sinusitis and candidal infections of the mouth and groin. She was allergic to a wide variety of environmental agents including soap, fur, toys, fuzzy, dust, and feathers. Neither his parents nor her sibling had the same problem. At 4 years of age, she was hospitalized because of bilaterally distal humerus fractures, resulting from a mild trauma. At the age of 8 years she had a high fever with chills, generalized malaise, fatique, dyspnea and a productive cough. Cultures of sputum and thoracentesis identified Staphylococcus aureus as the offending organism. The patient was treated with intravenous administration of an antistaphylococcal antibiotic and drainage by closed tube thoracostomy
with complete resolution of the empyema. Three months later the diagnosis of Hyper-Ig E was established with a large pneumatocele in the right upper lobe (Fig-1). The serum Ig E level was 20.000 U/mL (normal: 0.0-60 U/mL). Sputum specimens grew Staphylococcus aureus. Initial attempts at another institution to manage the infection by antistaphylococcal antibiotic and subsequently by percutaneous catheter drainage of the pneumatocele were succesful. On admisson (at the age of 9 years) physical examination revealed a girl with dark brown hair and normal growth for her age. Patient had 39 C fever with productive cough. There were multiple skin scars over the face, back, buttocks and extremities (Fig-2). There was no adenopathy appreciated on physical examination. Breath sounds over the right lower lung markedly diminished and had bilaterally diffuse coarse ronchy. The liver and spleen were not enlarged.
Figure 1. Chest CT scan demonstrating large pneumatocele in the right upper lobe.
Figure 3. Chest X-ray on admission showing bilaterally lung abscess, pneumatoceles and patcy areas of consolidation.
Figure 2. Showing eczematoid skin lesions of the lower extremities.
Figure 4. Radiography of the left upper extremity revealing scatris of distal humerus fracture.
Turkish Respiratory Journal, August 2002, Vol.3, No.2
69
Figure 5. Computed tomography of chest showing bilaterally abscess and pneumatoceles formation.
Complete blood count yielded a white blood cell count 30.1/mL with 64.7% neutrophils and 4.5/mL eosinophilia (normal:0.0-0.2). Hemoglobin and hematocrit 98 g /L and 0.32 respectively, with hipochromic anemia. Serum electrolytes were normal. Tests for cystic fibrosis (sweat cloride) were negative. The serum Ig E level was 19.300 IU/ml. Other serum immunoglobulin levels were within normal limits and a normal result for nitroblue tetrazolium reduction test (NBT), thus suggesting normal leucocyte chemotaxis. Based on the clinical history and the elevated level of Ig E, the diagnosis of hyperimmunoglobulin E (Jobs) syndrome was made. Chest X-ray revealed bilaterally lung abscess, pneumatoceles and patchy areas of consolidation (Fig. 3). Thorax ultrasound revealed right pleural effusion. Radiography of the upper extremity revealed a scatris of left distal humerus fracture (Fig 4). Computed tomography of the chest showed bilaterally abscess and pneumatocele formation (Fig 5). The culture from thoracentesis and sputum grew staphylococcus aureus. The patient was treated again with an intravenous antistaphylococcal antibiotic and drainage by closed tube thoracostomy for 6 weeks with complete resolution of the empyema. The sputum culture was negative at the end of the 6 weeks. During the 3-month-follow-up, she was doing well with intermittant prophylactic antibiotic therapy except for intermittant eczamatoid skin dermatitis although antieczematoid medications.
pneumatoceles formation, and markedly elevated serum Ig E (1-6). First reported by Davis and colleques in 1966 (1). They described a clinical syndrome in 2 unrelated girls with red hair and fair skin who, from birth, experienced chronic eczema, recurrent staphylococcal infections of the sinopulmonary tract, and in abnormal inflamatory response with the formation of cold staphylococcal abscesses. Davis and colleques referred to this syndrome as Jobs syndrome because of its resemblance to the affliction of the biblical figure. Buckley and co-workers (2) linked these clinical findings with markedly elevated serum Ig E levels and coarse facies. Hill and co-authors (3) reported hyperimmunoglobulinemia E and defective chemotaxis of polymorphonuclear leukocytes in the 2 original girls with Jobs syndrome. In addition to elevations in Ig E levels, defects in neutrophil chemotaxis have been reported by several authors (3,10,11). It is possible that the patient described by Swim et al. (12) had the clinical manifestatios of the hyperimmunoglobulin E syndrome but with normal neutrophil chemotaxis. Our patient was found to have a normal neutrophil chemotaxis. It is not possible to infer from currently available data whether an abnormality of neutrophil chemotaxis has a prominent role in the pathophysiology of the recurrent infection in this syndrome. A primary defect in the function of polymorphonuclear lekocytes as evaluated by chemotaxis is not always demonstrated in these patients (8). A review of the National Institute of Health experience of 13 patients with Jobs syndrome suggested that recurrent bronchitis is a common pulmonary complication of the syndrome. Empyema developed in many of these patients (6). Our patient also had a reccurent tharocic empyema which required a chest tube placement for 6 weeks. Additionally, intrapleural lavage was performed through chest tube with vancomisin. The pneumatoceles may persist for varying period of time, enlarging rapidly, or they may regres over time. The treatment for this condition is adequate chronic antistaphylococcal therapy which, in some cases, may cause spontaneous remission of the cysts (4). In our patient, pneumatoceles were present with gradual decrease in their size, therefore, surgical intervention was not required n a remarkable series, 11 patients with HIE reported by Merten and associates (14) all had lung cysts were reported to have spontaneously resolved after continuous antibiotic therapy. The unusual natural history of pneumatoceles in patients
Turkish Respiratory Journal, August 2002, Vol.3, No.2
Discussion
Hyperimmunoglobin E (Jobs) syndrome is an extremely rare disorder that is characterized by recurrent staphylococcal pulmonary infections complicated by empyema, chronic eczema,
70
with this syndrome is stressed as well as the need for surgical intervention when complications occur (22,23). Furthermore, as our patient, percutaneous catheter drainage can be made for large pneumatoceles to remove succesfully. Kirchner emphasized recurrent bone fractures in some of the patients with HIE syndrome (9) and a case of osteogenesis imperfecta tarda with HIE syndrome was reported by Brestel (15). Leung et al. suggested that the monocytes from HIE syndrome patient cause osteopenia and osteclasts, may contribute to the osteoporosis (16). Our patient had a bone fracture resulting from a mild trauma at age of four but no recurrence. The patients with Jobs syndrome also seem to be preposed to unusual fungal infections such as cryptococcosis and histoplasmosis of the esophagus (21) and colon (22). Our patient also had a fungal infection of the mouth and groin, which treated easily. The primary defect in HIE syndrome is unknown, therefore, definitive therapy is not possible. Several investigators have studied the effects of normal plasma transfusions, histamine-2-receptor blocking agents, transfer factor, levamisole, ascorbic acid and interferon-alpha in the treatment of HIE syndrome (3,11,20). Normal plasma transfusions, cimetidine and ascorbic acid said to improve the chemotactic abnormalities of neutrophils and did not observed any severe infections in their patients (11,20). We used levamisole, ascorbic acid and histamine-2-receptor blocking agents in our patient which proved useful. Our patient had no any important lung disease except recurrent mild skin lesions on regular controls. Etzioni et al. reported that a small dose of cyclosporin A (3 to 5 mg/kg/d) is beneficial in patients with HIE syndrome (21). It should be considered in severe cases where other therapeutic modalities have failed.
The long-term outcome of this disease is unknown. Life long antistaphylococcal antibiotic therapy seems to be most succesful treatment and useful in preventing infections in these patients, but no definitive therapy is available.
References
1. Davis SD, Schaller J, Wedgwood RJ. Jobs syndrome recurrent cold staphylococcal abscesses. Lancet 1966;1:1013-1015. 2. Buckley RH, Wray BB, Belmaker EZ. Extreme hyperimmunoglobulinemia E and undue susceptibility to infection. Pediatrics 1972;49:59-70. 3. Hill HR, Quie PG. Raised serum-Ig E levels and defective neutrophil chemotaxis in three children with eczema and recurrent bacterial infections. Lancet 1974;1:183-197 4. Jhaveri KS, SahaniDV, Shetty PG. Hyperimmunoglobulinaemia E syndrome: Pulmonary imaging features. Australasin Radiology 2000;44:328-330 5. Borges WG, Hensley T, Carey JC et al. The face of Job.The Journal of Pediatrics 1998;133:303-305 6. Donabedian H, Gallin JI. The hyperimmunoglobulin E recurrentinfection (Jobs) syndrome: a review of the NIH experience and the litarature. Medicine 1983;62:195-208 7. Grimbacher B, Holland SM, Gallin JI, et al. Hyper-IgE syndrome with recurrent infections-an autosomal dominant multsystem disorder. The New England Journal of Medicine 1999;340:692702 8. Lui RC, Inculet RI. Jobs syndrome: A rare cause of recurrent lung abscess in childhood. Ann Thorac Surg 1990;50:992-994 9. Kirchner SG, Sivit CJ, Wright PF. Hyperimmunoglobulinemia E syndrome: association with osteoporosis and recurrent fractures. Radiology 1985;156:362 10. Ballard RW, Cummigs CW. Jobs syndrome. The Lryngoscope 1980;90:1367-1370 11. Mawhinney H, Killen M, Fleming WA, et al. The hyperimmunoglobulin E syndrome-A neutrophil chemotactic defect reversible by histamine H2 receptor blockade? Clinical Immunology and Immunopathology 1980;17:483-491 12. Swim AT, Bradac C, Craddock PR. Levamisole in Jobs syndrome. The New England Journal of Medicine 1982;307:1528-1529 13. Donabedian H, Gallin JI. Mononuclear cells from patients with the hyperimmunoglobulin E-reccurrent-infections syndrome produce an inhibitor of leukocyte chemotaxis. J Clin Invest 1982;69:11551163 14. Merten DF, Buckley RH, Pratt PC, et al. Hyperimmunoglobulinemia E syndrome: Radiographic observations. Radiology 1979;132:71-78 15. Brestel EP, Klinberg WG, Veltri RW, et al. Osteogenesis Imperfecta Tarda in a child with hyper-IgE syndrome. Am J Dis
Turkish Respiratory Journal, August 2002, Vol.3, No.2
71
Child 1982;136:774-776 16. Leung DM, Geha RS. Clinical and immunologic aspects of the hyperimmunoglobulin E syndrome. Hematology/Oncology Clinics of North America 1988;2:81-100 17. Jacobs DH, Macher AM, Handler R, et al. Esophageal cryptococcosis in a patient with the hyperimmunoglobulin Erecurrent infection (Jobs) syndrome. Gastroenterology 1984;87:201-203 18. Hutto JO, Bryan CS, Greene FL, et al. Cryptococcosis of the colon resembling crohns disease in a patient with the hyperimmunoglobulinemia E- recurrent infection(Jobs) syndrome. Gastroenterology 1988;94:808-812 19. Dreskin SC, Gallin JI. Evolution of the hyperimmunoglobulin E and recurrent infection (HIE,JOBS) syndrome in a young girl. J. Allergy Clin. Immunol 1987;80:746-751 20. Sanal , Gmen A, Tezcan I, et al. Hyper-IgE syndrome: A case report. The Turkish Journal of Pediatrics 1990;32:273-278 21. Etzioni A, Shehadeh N, Brecher A, et al. Cyclosporin A in hyperimmunoglobulin E syndrome. Annals of Allergy, Asthma,& Immunology 1997;78:413-414 22. Shamberger RC, Wohl ME, Atayde AP, et al. Pneumatocele complicating hyperimmunoglobulin E syndrome ( Jobs syndrome). Ann Thorac Surg 1992;54:1206-1208 23. Hall RA, Salhany KE, Lebel E, et al. Fungal Pulmonary abscess in an adult secondary to hyperimmunoglobulin E (Jobs) syndrome. Ann Thorac Surg 1995;59:759-761
00
Turkish Respiratory Journal, August 2002, Vol.3, No.2
Turkish Respiratory Journal, August 2002, Vol.3, No.2
00
You might also like
- Fungi52 52.9537Document6 pagesFungi52 52.9537Reza PutradinataNo ratings yet
- Pediatric Round PneumoniaDocument4 pagesPediatric Round PneumoniaSalwa Zahra TsamaraNo ratings yet
- A Rare Cause of Endocarditis: Streptococcus PyogenesDocument3 pagesA Rare Cause of Endocarditis: Streptococcus PyogenesYusuf BrilliantNo ratings yet
- Pulmonary Miliary Tuberculosis Complicated With Tuberculous Spondylitis An Extraordinary Rare Association: A Case ReportDocument5 pagesPulmonary Miliary Tuberculosis Complicated With Tuberculous Spondylitis An Extraordinary Rare Association: A Case ReportIsmail Eko SaputraNo ratings yet
- Jurnal Bronchitis Dengan AsmaDocument5 pagesJurnal Bronchitis Dengan AsmaMauLan SaputraNo ratings yet
- F - CMCRep 1 Assy Et Al - 1405Document2 pagesF - CMCRep 1 Assy Et Al - 1405faegrerh5ju75yu34yNo ratings yet
- Case Report: A 75-Year-Old Female With Hemoptysis and Recurrent Respiratory InfectionsDocument4 pagesCase Report: A 75-Year-Old Female With Hemoptysis and Recurrent Respiratory InfectionsIRa SyalalaNo ratings yet
- Necrotizing Pneumonitis Caused by Mycoplasma Pneumoniae in Pediatric PatientsDocument4 pagesNecrotizing Pneumonitis Caused by Mycoplasma Pneumoniae in Pediatric Patientswawa chenNo ratings yet
- 500 FullDocument4 pages500 FullAina NurlailaNo ratings yet
- Case Report: Systemic Steroid Treatment For Severe Expanding Pneumococcal PneumoniaDocument4 pagesCase Report: Systemic Steroid Treatment For Severe Expanding Pneumococcal PneumoniaadhiniNo ratings yet
- Pathophysiological Study of Chronic Necrotizing Pulmonary AspergillosisDocument5 pagesPathophysiological Study of Chronic Necrotizing Pulmonary AspergillosisSyaiful IslamNo ratings yet
- Recurrent Pneumonia Caused by Rare Granular Cell TumorDocument7 pagesRecurrent Pneumonia Caused by Rare Granular Cell TumorJoshua MendozaNo ratings yet
- Empyema Thoracis Caused by Drug-Resistant S. aureusDocument6 pagesEmpyema Thoracis Caused by Drug-Resistant S. aureuspqrsehunNo ratings yet
- Bronchitis Obliterans Due To Mycoplasma PneumoniaDocument7 pagesBronchitis Obliterans Due To Mycoplasma Pneumoniawawa chenNo ratings yet
- A Case of Pulmonary Aspergilloma and ActinomycosisDocument4 pagesA Case of Pulmonary Aspergilloma and ActinomycosisNova PurbaNo ratings yet
- Chronic Pulmonary Aspergillosis in A Patient With hyper-IgE SyndromeDocument3 pagesChronic Pulmonary Aspergillosis in A Patient With hyper-IgE SyndromeWalid AissaNo ratings yet
- Stevens-Johnson Syndrome Without Skin Lesions: Case ReportDocument4 pagesStevens-Johnson Syndrome Without Skin Lesions: Case ReportYona LadyventiniNo ratings yet
- Epiglotitis DCHDocument6 pagesEpiglotitis DCHLu BfNo ratings yet
- Pulmonary Tuberculosis Presenting with ARDSDocument5 pagesPulmonary Tuberculosis Presenting with ARDSCimol AgustinaNo ratings yet
- Pulmonary Interstitial Emphysema Complicating Pneumonia in An Unventilated Term InfantDocument3 pagesPulmonary Interstitial Emphysema Complicating Pneumonia in An Unventilated Term Infantindra_poetoetNo ratings yet
- Case Report Proteus Species Infection: A Diagnostic DilemmaDocument5 pagesCase Report Proteus Species Infection: A Diagnostic DilemmaTengku AdriansyahNo ratings yet
- Jurnal 7 BronkiolitisDocument7 pagesJurnal 7 BronkiolitisIrsanti sasmitaNo ratings yet
- Paediatric Empyema: A Case Report and Literature ReviewDocument5 pagesPaediatric Empyema: A Case Report and Literature ReviewphobicmdNo ratings yet
- Rhizomucor Scedosporium: Case ReportDocument6 pagesRhizomucor Scedosporium: Case ReportPaul ColburnNo ratings yet
- Early Diagnosis of Kartagener's SyndromeDocument8 pagesEarly Diagnosis of Kartagener's SyndromeHendra SusantoNo ratings yet
- Lesoes Cisticas HIVDocument5 pagesLesoes Cisticas HIVAndrey Barbosa PimentaNo ratings yet
- Eosinophilic Granulomatosis With Polyangiitis and Bowel Perforation: Case ReportDocument5 pagesEosinophilic Granulomatosis With Polyangiitis and Bowel Perforation: Case ReportSabrina JonesNo ratings yet
- Mediastinal Tuberculous Lymphadenitis Presenting With Insidious Back Pain in A Male Adult: A Case Report and Review of The LiteratureDocument7 pagesMediastinal Tuberculous Lymphadenitis Presenting With Insidious Back Pain in A Male Adult: A Case Report and Review of The Literaturez9tpwgb5nwNo ratings yet
- The Role of High-Resolution Chest CT in The Diagnosis of Neuroendocrine Cell Hyperplasia of Infancy - A Rare Form of Pediatric Interstitial Lung DiseaseDocument3 pagesThe Role of High-Resolution Chest CT in The Diagnosis of Neuroendocrine Cell Hyperplasia of Infancy - A Rare Form of Pediatric Interstitial Lung DiseaseWalid AissaNo ratings yet
- Case ARDSDocument16 pagesCase ARDSAida SiregarNo ratings yet
- Computed Tomography Findings of Community-Acquired Immunocompetent Patient: A Case ReportDocument4 pagesComputed Tomography Findings of Community-Acquired Immunocompetent Patient: A Case ReportDenta HaritsaNo ratings yet
- Case Report: Hydropneumothorax in Children: A Rare Complication of A Bacterial PneumoniaDocument5 pagesCase Report: Hydropneumothorax in Children: A Rare Complication of A Bacterial PneumoniaNadya NovianiNo ratings yet
- Pulmonary Histoplasmosis Halo Sign CTDocument2 pagesPulmonary Histoplasmosis Halo Sign CTSharom R. AlvarezNo ratings yet
- A 7-Year-Old Girl With Dyspnea and Rash: AnswertophotoquizDocument2 pagesA 7-Year-Old Girl With Dyspnea and Rash: AnswertophotoquizMateen ShukriNo ratings yet
- Fibrinolytic Treatment of Complicated Pediatric TDocument2 pagesFibrinolytic Treatment of Complicated Pediatric TDR GURDEEP SINGHNo ratings yet
- 51 Uysal EtalDocument4 pages51 Uysal EtaleditorijmrhsNo ratings yet
- Co-Existence of Pulmonary, Tonsillar and Laryngeal TuberculosisDocument4 pagesCo-Existence of Pulmonary, Tonsillar and Laryngeal TuberculosisSoeHorNo ratings yet
- Sinonasal Eosinophilic Angiocentric FibrosisDocument10 pagesSinonasal Eosinophilic Angiocentric FibrosisPriskila Marlen YoltuwuNo ratings yet
- Jchimp 5 26322Document4 pagesJchimp 5 26322Jongga SiahaanNo ratings yet
- Indian J Radiol Imaging Word 1Document14 pagesIndian J Radiol Imaging Word 1Adie BrianNo ratings yet
- Invasive Aspergillosis in A Patient With End StageDocument8 pagesInvasive Aspergillosis in A Patient With End StageDhurgham QuasimNo ratings yet
- Ofy 038Document5 pagesOfy 038Rosandi AdamNo ratings yet
- Fungal Origin of in Situ Pulmonary Artery Thrombosis: A Case ReportDocument5 pagesFungal Origin of in Situ Pulmonary Artery Thrombosis: A Case ReportIJAR JOURNALNo ratings yet
- X Linked GammaDocument3 pagesX Linked GammaWaseem RajaNo ratings yet
- Letter TO THE Editor: Secondary Organizing Pneumonia After Varicella-Zoster Virus Infection: A Rare AssociationDocument3 pagesLetter TO THE Editor: Secondary Organizing Pneumonia After Varicella-Zoster Virus Infection: A Rare AssociationfatimiahmastaNo ratings yet
- Caso Clinico Clnica Mayo 3Document6 pagesCaso Clinico Clnica Mayo 3Francisco HernandezNo ratings yet
- Chronic Cavitary and Fibrosing Pulmonary and Pleural Aspergillosis: Case Series, Proposed Nomenclature Change, and ReviewDocument16 pagesChronic Cavitary and Fibrosing Pulmonary and Pleural Aspergillosis: Case Series, Proposed Nomenclature Change, and ReviewYassine EssNo ratings yet
- Interstitial Lung Changes in Sjögren's Syndrome: Report of 3 CasesDocument5 pagesInterstitial Lung Changes in Sjögren's Syndrome: Report of 3 CasesRyl WonNo ratings yet
- Simultaneous Bilateral Primary Spontaneous Pneumothorax (2019)Document7 pagesSimultaneous Bilateral Primary Spontaneous Pneumothorax (2019)sandi_prawira_yudhaNo ratings yet
- A Case of Lupus Pneumonitis Mimicking As Infective PneumoniaDocument4 pagesA Case of Lupus Pneumonitis Mimicking As Infective PneumoniaIOSR Journal of PharmacyNo ratings yet
- CytomegaloDocument3 pagesCytomegaloYusi RizkyNo ratings yet
- Infected Pulmonary Infarction Case ReportDocument8 pagesInfected Pulmonary Infarction Case ReportSebastian Felipe Sierra UmañaNo ratings yet
- Rare Cutaneous Tuberculosis FormsDocument6 pagesRare Cutaneous Tuberculosis FormsinggitsiregarNo ratings yet
- A Case of Comorbidity of Complicated Infective Endocarditis and Severe Pneumonia Due To Legionella PneumophilaDocument5 pagesA Case of Comorbidity of Complicated Infective Endocarditis and Severe Pneumonia Due To Legionella PneumophilaSabrina JonesNo ratings yet
- Radiological Findings of Unilateral Tuberculous LuDocument7 pagesRadiological Findings of Unilateral Tuberculous LuSarah watiNo ratings yet
- Neonatal Chronic Bullous Disease and PneumoniaDocument2 pagesNeonatal Chronic Bullous Disease and PneumoniaCharissa Mia D. Salud-GniloNo ratings yet
- Diffuse Large B-Cell Lymphoma Arising From The Lesion ofDocument7 pagesDiffuse Large B-Cell Lymphoma Arising From The Lesion ofFadel AhmadNo ratings yet
- Diagnosis and Treatment of Chronic CoughFrom EverandDiagnosis and Treatment of Chronic CoughSang Heon ChoNo ratings yet
- Stem Cell-Based Therapy for Lung DiseaseFrom EverandStem Cell-Based Therapy for Lung DiseaseJanette K. BurgessNo ratings yet
- 2017 JAMA Review - Delirium in Older Persons Advances in Diagnosis and Treatment PDFDocument14 pages2017 JAMA Review - Delirium in Older Persons Advances in Diagnosis and Treatment PDFgiseladlrNo ratings yet
- Dog Bite Facts: 4.5 Million Occur Yearly in USDocument5 pagesDog Bite Facts: 4.5 Million Occur Yearly in USDesta KirosNo ratings yet
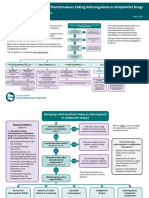
- Sdcep Anticoagulants Quick Reference Guide 2nd EditionDocument5 pagesSdcep Anticoagulants Quick Reference Guide 2nd EditionMeryem LahlouNo ratings yet
- Definition of Infiltration Phlebitis and ExtravasationDocument2 pagesDefinition of Infiltration Phlebitis and ExtravasationJessie YingNo ratings yet
- Clinical PharmacokineticsDocument31 pagesClinical PharmacokineticsArdiyanti Puspitasari100% (1)
- Hafizuddin Azfar (Els 1265)Document46 pagesHafizuddin Azfar (Els 1265)Mohd hafiz AzmiNo ratings yet
- AngiogenesisDocument1 pageAngiogenesisHazim rizkNo ratings yet
- 001 RCA FlipchartDocument40 pages001 RCA FlipchartAbd ZouhierNo ratings yet
- PHS 210 EpidemiologyDocument4 pagesPHS 210 EpidemiologySera GoldNo ratings yet
- Introduction to Pathology of the Skeletal SystemDocument69 pagesIntroduction to Pathology of the Skeletal SystemSoleil SierraNo ratings yet
- Literature Review On Hepatitis B and CDocument10 pagesLiterature Review On Hepatitis B and Cafmzyywqyfolhp100% (1)
- Qu Et Al. 2021Document9 pagesQu Et Al. 2021Kassila SantosNo ratings yet
- David Cesarini Registered Social Worker CV Curriculum VitaeDocument3 pagesDavid Cesarini Registered Social Worker CV Curriculum VitaeDave CesariniNo ratings yet
- Assignment 5.1 OHS Legislation - DiazDocument3 pagesAssignment 5.1 OHS Legislation - DiazADRIAN GABRIEL DIAZNo ratings yet
- Hospital Management System UML and Specification DocumentDocument16 pagesHospital Management System UML and Specification DocumentManish PareekNo ratings yet
- Artesunato MefloquinaDocument11 pagesArtesunato MefloquinaDavid CerrónNo ratings yet
- CroupDocument10 pagesCroupEl Justinson Puspos100% (1)
- Prevention of Waterborne DiseasesDocument2 pagesPrevention of Waterborne DiseasesRixin JamtshoNo ratings yet
- NmghjyjDocument108 pagesNmghjyjindahNo ratings yet
- ARI - Introduction To Medical Varmalogy For Parents of Special ChildrenDocument41 pagesARI - Introduction To Medical Varmalogy For Parents of Special ChildrenArts Research Institute100% (4)
- DysmenorrheaDocument28 pagesDysmenorrheaDr Munira MalikNo ratings yet
- The Coronally Advanced Flap in Combination With Platelet-Rich Fibrin (PRF) and Enamel Matrix Derivative in The Treatment of Gingival Recession: A Comparative StudyDocument15 pagesThe Coronally Advanced Flap in Combination With Platelet-Rich Fibrin (PRF) and Enamel Matrix Derivative in The Treatment of Gingival Recession: A Comparative StudyAnsh Veer ChouhanNo ratings yet
- Job Safety Analysis (JSA) - Painting DateDocument2 pagesJob Safety Analysis (JSA) - Painting DatenabeelNo ratings yet
- 17 TYPES OF GOOD BACTERIA - The List of Most Beneficial Species of Probiotics Lactobacillus and Bifidobacteria - Ecosh LifeDocument30 pages17 TYPES OF GOOD BACTERIA - The List of Most Beneficial Species of Probiotics Lactobacillus and Bifidobacteria - Ecosh LifeCarl MacCordNo ratings yet
- Scenar Testimonials (Updated)Document10 pagesScenar Testimonials (Updated)Tom Askew100% (1)
- Cabizares Handle CaseDocument8 pagesCabizares Handle CaseMae AbabonNo ratings yet
- Asante Teaching Hospital Activity Based CostingDocument3 pagesAsante Teaching Hospital Activity Based CostingMuskanNo ratings yet
- Importance of Health Appraisals for StudentsDocument10 pagesImportance of Health Appraisals for StudentsPantz Revibes PastorNo ratings yet
- AneurysmDocument22 pagesAneurysmRaymond SorianoNo ratings yet
- AOCase Control CohortstudydesignsDocument6 pagesAOCase Control CohortstudydesignsakshayajainaNo ratings yet