Professional Documents
Culture Documents
Running Head: Final Paper: Putting Evidence-Based Practice Into 1
Uploaded by
api-292717295Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Running Head: Final Paper: Putting Evidence-Based Practice Into 1
Uploaded by
api-292717295Copyright:
Available Formats
Running head: FINAL PAPER: PUTTING EVIDENCE-BASED PRACTICE INTO
Final Paper: Putting Evidence-Based Practice into Action
Jessica Foster
University of Saint Mary
FINAL PAPER: PUTTING EVIDENCE-BASED PRACTICE INTO
Final Paper: Putting Evidence-Based Practice into Action
Evidence-based practice (EBP) is the cornerstone of the nursing profession. EBP is
developing scholarly statistical data to help deliver high quality health care (American Nurses
Association [ANA], 2010). Even with numerous databases and national guideline organizations
studies show that up to 40% of patients are not receiving care according to statistical data (Grol
& Grimshaw, 2003). Literature throughout the years identify different barriers impeding on
nurses ability to implement EBP. Identifying barriers then implementing strategic organizational
infrastructures will increase nurses' time, knowledge, motivation and skill into putting evidencebased practice into action.
During a literature review of barriers to implementing EBP the data began to intertwine.
Fifteen studies were analyzed and reviewed. The top barriers identified were lack of time,
organizational support and autonomy. Allowing increased time away from bedside care,
knowledge and organizational support will motivate nurses to explore evidence-based practice
guidelines and investigate research databases to gain confidence in their practice. The Scope and
Standards of Practice states that nurses will "integrate evidence and research findings into
practice" (ANA, 2010, p. 51). When nurses integrate evidence into practice they are helping the
patient, the nursing community and the organization. Education is a powerful tool that can create
leaders within the profession and future nurses to take example for implementing EBP.
One of the most crucial findings throughout literature was the lack of evidence to support
the success and failures of programs for implementing EBP. Solomons & Spross, (2011)
established that most nurses obtain their information from other nurses even if this knowledge is
or is not EBP. This was also established in a study designed by Newman, Papadopoulos, &
Sigsworth, (1998) concluded only focusing on individual knowledge improvement and skill
FINAL PAPER: PUTTING EVIDENCE-BASED PRACTICE INTO
would not be sufficient because without utilizing this knowledge at work they would be
unsuccessful. Nurses also must have autonomy to address practice issues, review the literature
for the problem then identify where changes could be made. This empowers nurses with
knowledge and moral to participate in quality improvement and patient safety initiatives. Direct
and indirect patient care is based on scientific research that is then created into policies that
improve patient outcomes.
In order for change to occur more research is needed to identify the success of
educational programs as clinical ladder programs. Although the literature is useful in identifying
common barriers to practice each organization will have their own barriers due to cultural
differences. Collecting data to identify the barriers and facilitators becomes the first step to
implementing EBP. Next would be to create a program that would decrease or delete the barriers
identified. Most organizations stop here and do not bother to investigate the effectiveness of the
program. Researching the success or failure of the program becomes the crucial last step. If the
program designed does not make a change then there is no effect for anyone from the patient to
the organization. This is where the research is lacking. The literature review was extensive on
identifying barriers but minimal evidence to guide changes and the effects of these changes.
Sherriff, Wallis, & Chaboyer, (2007) state that further research needs to be done to evaluate the
effectiveness of educational programs and the incorporation of EBP in patient care.
More organizations have begun to develop clinical ladder programs to encourage and
support educational advancements. These clinical ladder programs encourage nurses to utilize
critical thinking skills to research and analysis data to incorporate into practice. These programs
will help nurses gain knowledge into the latest EBP guidelines then educate the staff on research
found. This also motivates nurses by including financial incentives. Not only does this show
FINAL PAPER: PUTTING EVIDENCE-BASED PRACTICE INTO
great educational support by the organization but it improves the quality of care for patients
when the evidence is implemented. The limitations on some of these programs still hold to some
of the same barrier; no extra time away from bedside care to work on the project, no autonomy to
implement new evidence due to the need for policy changes and non-congratulatory
organizational support.
Every stakeholder has their own ethical considerations that need to be addressed to avoid
a potential harmful domino effect. Without nurses implementing EBP at the bedside the patient
is the greatest effected. When the patient does not receive the best quality of care this reflects
poorly on the organization which then goes into possible financial and policy changes. These
changes may not be in tune with best nursing practice and according to the Guide to the Code of
Ethics for Nurses, nurses are to mandate the profession and the standards that support patient
care (American Nurses Association [ANA], 2010). The number one objective for implementing
EBP is to mitigate risk and improve outcomes. When the nurse and organization work in a
collaborative manner to implement EBP the Hospital Quality Institute (HQI) standards will be
met.
While numerous data supports that barriers exist to implementing EBP there is little
research to support changes can make a statistical difference in the health-care setting. Evidencebased practice is the standard nurses' oath to patients and their organizations. When this is not
implemented then all key stakeholders are at risk. Making changes to organizational
infrastructures and empowering nurses with knowledge will put evidence-based practice into
action.
FINAL PAPER: PUTTING EVIDENCE-BASED PRACTICE INTO
References
American Nurses Association. (2010). Guide to the code of ethics for nurses: Interpretation and
Application [reissue of 2008 with new cover]. Silver Spring, MD: Nursebooks.org.
American Nurses Association. (2010). Nursing: Scope and standards of practice (2nd ed.).
Silver Spring, MD: Nursebooks.org.
Grol, R., & Grimshaw, J. (2003). From best evidence to best practice: effective implementation
of change in patients care. The Lancet, 362, 1225-1230. Retrieved from
http://web.b.ebscohost.com/ehost/detail/detail?vid=6&sid=ac0b4988-849a-4f15-b78e95856ec17501%40sessionmgr111&hid=107&bdata=JnNpdGU9ZWhvc3QtbGl2ZQ%3d
%3d#db=ccm&AN=2005026921
Newman, M., Papadopoulos, I., & Sigsworth, J. (1998). Barriers to evidence-based practice.
Intensive & Critical Care Nursing, 14, 231-238. Retrieved from
http://share.worldcat.org/ILL/articleexchange/FileDownload/JHtpeJuo8;jsessionid=AC19
F9D6A7AEEBCE9A13625B86F5CBE2
Sherriff, K. L., Wallis, M., & Chaboyer, W. (2007). Nurses attitudes to and perceptions of
knowledge and skills regarding evidence-based practice. International Journal of Nursing
Practice, 13, 363-369. http://dx.doi.org/10.1111/j.1440-172X.2007.00651.x
Solomons, N. M., & Spross, J. A. (2011). Evidence-based practice barriers and facilitators from a
continuous quality improvement perspective: an integrative review. Journal of Nursing
Management, 19, 109-120. http://dx.doi.org/10.1111/j.1365-2834.2010.01144.x
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Digital Maturity Model: + 179 Specific Digital Criteria To Test Your Organizational MaturityDocument1 pageDigital Maturity Model: + 179 Specific Digital Criteria To Test Your Organizational MaturityDaiani Roberti100% (1)
- Home Economics PDFDocument29 pagesHome Economics PDFalpha100% (2)
- Time Log For PracticumDocument4 pagesTime Log For Practicumapi-292717295No ratings yet
- Ne Specialty Outcomes Evaluation ChecklistDocument2 pagesNe Specialty Outcomes Evaluation Checklistapi-292717295No ratings yet
- Jessica Foster ResumeDocument3 pagesJessica Foster Resumeapi-292717295No ratings yet
- Hanh Nguyen1Document10 pagesHanh Nguyen1api-292717295No ratings yet
- Amy Cooper1Document12 pagesAmy Cooper1api-292717295No ratings yet
- AddressingmandatoryovertimeDocument4 pagesAddressingmandatoryovertimeapi-292717295No ratings yet
- MynursingphilosophyDocument4 pagesMynursingphilosophyapi-292717295No ratings yet
- Joshua's Return On Investment of Competency Mapping 1.123456pptDocument31 pagesJoshua's Return On Investment of Competency Mapping 1.123456pptSubin NelluvaleelNo ratings yet
- Physical Education Practical 1Document10 pagesPhysical Education Practical 1Mitul LovrasNo ratings yet
- A Guide To The Linguistic and Stylistic Analysis of A Passage From ChaucerDocument3 pagesA Guide To The Linguistic and Stylistic Analysis of A Passage From ChaucerNasrullah AliNo ratings yet
- Francis Bacon of TruthDocument2 pagesFrancis Bacon of Truthpetroleja0% (1)
- Grade 7 Exam 9 PDFDocument16 pagesGrade 7 Exam 9 PDFShane Rajapaksha100% (2)
- Secondary Courses - The National Institute of Open Schooling (NIOS)Document1 pageSecondary Courses - The National Institute of Open Schooling (NIOS)Subhankar BasuNo ratings yet
- Galileo The Father of Modern Science Process PaperDocument3 pagesGalileo The Father of Modern Science Process Paperapi-122027419No ratings yet
- Got It Starter Unit 1 PDFDocument2 pagesGot It Starter Unit 1 PDFSebas Tovo100% (1)
- So v. Republic (2007)Document17 pagesSo v. Republic (2007)enggNo ratings yet
- RPT 2022 Bahasa Inggeris Tahun 2 CEFR SumberpendidikanDocument35 pagesRPT 2022 Bahasa Inggeris Tahun 2 CEFR SumberpendidikanNG SIAW MOI MoeNo ratings yet
- 11 Reasons Why Quo Warranto Decision On Sereno Was CorrectDocument3 pages11 Reasons Why Quo Warranto Decision On Sereno Was CorrectMelvin PernezNo ratings yet
- USMLE StepDocument1 pageUSMLE StepAscend KannanNo ratings yet
- Rubrik Solving ProblemDocument10 pagesRubrik Solving ProblemSjkt TajulNo ratings yet
- Kami Export - Worksheet-College Research 4Document1 pageKami Export - Worksheet-College Research 4api-535006987No ratings yet
- Doe v. Oklahoma City University, 10th Cir. (2010)Document13 pagesDoe v. Oklahoma City University, 10th Cir. (2010)Scribd Government DocsNo ratings yet
- Broadcasting WorkshopDocument9 pagesBroadcasting WorkshopRyan De la TorreNo ratings yet
- College Tuition Cost Research PaperDocument8 pagesCollege Tuition Cost Research Paperhjuzvzwgf100% (1)
- MAGKLASE!!!" But The Positive Side of Me Reminded Myself That I Am ADocument2 pagesMAGKLASE!!!" But The Positive Side of Me Reminded Myself That I Am ADo DoNo ratings yet
- Life Vision IntPlus Student Book Table of ContentsDocument2 pagesLife Vision IntPlus Student Book Table of ContentsDave GrammarsNo ratings yet
- Anju BalaDocument2 pagesAnju BalaSANDEEP SinghNo ratings yet
- Assessment of The Knowledge Attitude and PracticeDocument7 pagesAssessment of The Knowledge Attitude and PracticeAamirNo ratings yet
- Rizal in The Contemporary Era Relevance of Dr. Rizals Life and Works To The Present GenerationDocument2 pagesRizal in The Contemporary Era Relevance of Dr. Rizals Life and Works To The Present Generationkaji cruzNo ratings yet
- Hadleigh Markun - 2019 Vertical Articulation Sample and Activity No DirectionsDocument1 pageHadleigh Markun - 2019 Vertical Articulation Sample and Activity No Directionsapi-510451077100% (1)
- Position Paper About James Soriano's ArticleDocument2 pagesPosition Paper About James Soriano's ArticleAnah May100% (3)
- The Scandal of Social Work EducationDocument12 pagesThe Scandal of Social Work EducationPeehu GuptaNo ratings yet
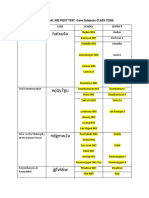
- SHS CORE DIAL ME POST TEST CLASS CODEDocument2 pagesSHS CORE DIAL ME POST TEST CLASS CODEEmmanuel Paul JimeneaNo ratings yet
- 3 New Literacies, 21st Century SkillsDocument66 pages3 New Literacies, 21st Century Skillsirene apiladaNo ratings yet
- Name of Social Venture: Nominated Host Country (Team Number + Name)Document13 pagesName of Social Venture: Nominated Host Country (Team Number + Name)SaketNo ratings yet