Professional Documents
Culture Documents
Ventricular Tachycardia: History Signs and Symptoms Differential
Uploaded by
chr0m3b4tm4nOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ventricular Tachycardia: History Signs and Symptoms Differential
Uploaded by
chr0m3b4tm4nCopyright:
Available Formats
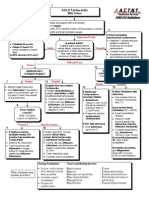
Ventricular Tachycardia
History
Past medical history /
medications, diet, drugs.
Syncope / near syncope
CHF
Palpitations
Pacemaker
Allergies: lidocaine / novacaine
Signs and Symptoms
Ventricular tachycardia on ECG
(Runs or sustained)
Conscious, rapid pulse
Chest pain, shortness of breath
Dizziness
Rate usually 150 - 180 bpm for
sustained V-Tach
QRS > .12 Sec
Differential
Artifact / Device failure
Cardiac
Endocrine / Metabolic
Drugs
Pulmonary
Legend
MR
EMT
EMT- I
EMT- P
Medical Control
Universal Patient Care Protocol
Appropriate
protocol
Palpable pulse ?
Wide, regular rhythm with QRS >0.12 s
No
B
I
Yes
I
IV Protocol
12 Lead ECG
Amiodarone,
Lidocaine, or
Procainamide
(consider in this
order if available)
Consider Sedation
Midazolam
or
Lorazepam
or
Diazepam
If Unsuccessful
Rapid Transport with Early
Destination Notification
Amiodarone,
Lidocaine, or
Procainamide
(consider in this
order if available)
12 Lead ECG
After Conversion
Becomes Unstable?
P
M
B
Repeat Dose or
Chose Another Drug
Amiodarone,
Lidocaine, or
Procainamide
Synchronized
Cardioversion
May Repeat as needed
Yes
No
Medical Protocols
Notify Destination or
Contact Medical Control
Pre-arrest
(No palpable BP,
Altered mental status)
Stable
Notify Destination or
Contact Medical Control
Pearls
Recommended Exam: Mental Status, Skin, Neck, Lung, Heart, Abdomen, Back, Extremities, Neuro
For witnessed / monitored ventricular tachycardia, try having patient cough.
Polymorphic V-Tach (Torsades de Pointes) may benefit from the administration of magnesium sulfate if available.
If presumed hyperkalemia (end-state renal disease, dialysis, etc.), administer Sodium Bicarbonate.
Procainamide (if available) is no longer second line agent although it should not be given if there is history of CHF.
Protocol 36
Any local EMS System changes to this document must follow the NC OEMS Protocol Change Policy and be approved by OEMS
2009
You might also like
- Cardiac DrugsDocument10 pagesCardiac DrugsNursePoor98% (47)
- Cardiac Failure: Definition: Compensatory Changes in Heart FailureDocument5 pagesCardiac Failure: Definition: Compensatory Changes in Heart FailureMatyie SmkasNo ratings yet
- Blueprints Primary Care TablesDocument40 pagesBlueprints Primary Care TablesAnne Lowry92% (13)
- Handbook of AnesthesiologyDocument176 pagesHandbook of AnesthesiologyarmelzahfauziNo ratings yet
- ACLS MneumonicsDocument4 pagesACLS MneumonicsnaranothNo ratings yet
- Percutaneous InterventionsDocument55 pagesPercutaneous InterventionsShannon Bellamy-FoggNo ratings yet
- Cardiac Arrythmias in The ED Menbeu Edited From AnaDocument106 pagesCardiac Arrythmias in The ED Menbeu Edited From AnaTemesgen Geleta100% (1)
- ACLS Algorithms SlideDocument26 pagesACLS Algorithms SlidehrsoNo ratings yet
- ACLS Tachycardia Algorithm For Managing Unstable TachycardiaDocument2 pagesACLS Tachycardia Algorithm For Managing Unstable TachycardiaLady MuffinsNo ratings yet
- Pro32 SupraventricularTachycardiaDocument1 pagePro32 SupraventricularTachycardiaRonald KendallNo ratings yet
- Assessment of The Acutely Ill PatientDocument10 pagesAssessment of The Acutely Ill PatientZacmilo Dela TorreNo ratings yet
- Life Threatening Arrhythmia and ManagementDocument40 pagesLife Threatening Arrhythmia and ManagementRuki HartawanNo ratings yet
- Pulmonary HTNDocument51 pagesPulmonary HTNMuhammad HaekalNo ratings yet
- Hemodynamics Basic Concepts 1204053445109897 4Document115 pagesHemodynamics Basic Concepts 1204053445109897 4valeriesolidum100% (1)
- Tachyarrhythmias When Should I Refer?Document25 pagesTachyarrhythmias When Should I Refer?Cindy Seow Sieng TengNo ratings yet
- Pedal EdemaDocument45 pagesPedal Edemafirdaushassan2112No ratings yet
- DYSRHYTHMIASDocument9 pagesDYSRHYTHMIASgudobenNo ratings yet
- Lecture - 2 Advanced Cardiac Life SupportDocument28 pagesLecture - 2 Advanced Cardiac Life SupportJixon GeorgeNo ratings yet
- Arrhythmic PatientsDocument15 pagesArrhythmic PatientsBen ScottNo ratings yet
- Peri Arrest ArrhythmiasDocument40 pagesPeri Arrest ArrhythmiasDestiAriyaniNo ratings yet
- Management of Symptomatic Bradycardia and TachycardiaDocument55 pagesManagement of Symptomatic Bradycardia and TachycardiaDewintha Airene NoviantiNo ratings yet
- CHFalgorithm Univ of MSDocument1 pageCHFalgorithm Univ of MSDominique Excelsis J. DegamoNo ratings yet
- Tachy/賸)Document28 pagesTachy/賸)Jason LinNo ratings yet
- Sample Medical Guidelines: ACLS-BradycardiaDocument2 pagesSample Medical Guidelines: ACLS-BradycardiaCheewin KhawprapaNo ratings yet
- Ecg NotesDocument16 pagesEcg NotesAszhiNo ratings yet
- Atrial Fibrillation: Dr. Zirath + Dr. MehtaDocument29 pagesAtrial Fibrillation: Dr. Zirath + Dr. MehtaAjayNo ratings yet
- Synthesis: History Report SBAR Complete PA Know Your Patho!!! Don't Get Caught W/drawersDocument30 pagesSynthesis: History Report SBAR Complete PA Know Your Patho!!! Don't Get Caught W/drawersmmcgee002No ratings yet
- ACLS-Pediatric Wide Complex Tachycardia: Sample Medical GuidelinesDocument2 pagesACLS-Pediatric Wide Complex Tachycardia: Sample Medical GuidelinesFebrialitaFatoniNo ratings yet
- Pulseless Arrest Algorythm: Symptoms PersistDocument1 pagePulseless Arrest Algorythm: Symptoms PersistMeita ReligiaNo ratings yet
- Hypertensive Emergency: Beny Ghufron Dept. of Internal Medicine June 2011Document31 pagesHypertensive Emergency: Beny Ghufron Dept. of Internal Medicine June 2011Dendian Berlia JelitaNo ratings yet
- Crisis of Hypertension Revised 1Document57 pagesCrisis of Hypertension Revised 1Ratna Puspa RahayuNo ratings yet
- Arrhythmia 3Document2 pagesArrhythmia 3Nikey LimNo ratings yet
- "Pulmonary Hypertension": Jimmy Ford, MD Pulmonary and Critical CareDocument51 pages"Pulmonary Hypertension": Jimmy Ford, MD Pulmonary and Critical CareSohil ElfarNo ratings yet
- Arrhythmias: Nightfloat Curriculum 2010-2011 LPCH Pediatric Residency ProgramDocument26 pagesArrhythmias: Nightfloat Curriculum 2010-2011 LPCH Pediatric Residency Programkamel6No ratings yet
- Atrial Dysrhythmias: Etiology, Physical Assessment, and TreatmentDocument2 pagesAtrial Dysrhythmias: Etiology, Physical Assessment, and TreatmentMelissaNo ratings yet
- Acute HFDocument36 pagesAcute HFeman roshdyNo ratings yet
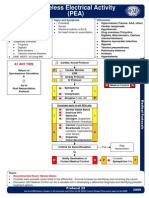
- Pro29 PulselessElectricalActivityDocument1 pagePro29 PulselessElectricalActivityZen Firhan ShahabNo ratings yet
- Think Link Ecg Notes: Normal Sinus Rhythm at 70 Beats/minDocument3 pagesThink Link Ecg Notes: Normal Sinus Rhythm at 70 Beats/minWillington CuaresmaNo ratings yet
- Chest PainDocument2 pagesChest PaindrsmiNo ratings yet
- Chapter3Shock CirculationDocument13 pagesChapter3Shock CirculationSri AgustinaNo ratings yet
- Pulmonary Hypertension - LITFL - CCC CardiologyDocument1 pagePulmonary Hypertension - LITFL - CCC CardiologymyaqanithaNo ratings yet
- Vasopressors: Jennifer & Joshua Chalk Talk 1/17/2014 Go Hawks!Document44 pagesVasopressors: Jennifer & Joshua Chalk Talk 1/17/2014 Go Hawks!pattumkp100% (1)
- Reviewer For DutyDocument4 pagesReviewer For DutyBenedict James BermasNo ratings yet
- Final Copy HTN EmergencyDocument13 pagesFinal Copy HTN EmergencyabrarNo ratings yet
- Arrhythmias: Domina Petric, MDDocument22 pagesArrhythmias: Domina Petric, MDMwaba PeterNo ratings yet
- Departemen Kardiologi FK USU RSUP. H. Adam Malik MedanDocument64 pagesDepartemen Kardiologi FK USU RSUP. H. Adam Malik MedanBonitavanyNo ratings yet
- Approach To Tachyarrhythmia: SVT - VT - VF - Torsa de PointesDocument17 pagesApproach To Tachyarrhythmia: SVT - VT - VF - Torsa de PointesAmir Izzuddin SuibNo ratings yet
- Pharm Final ReviewDocument8 pagesPharm Final ReviewKasey C. PintoNo ratings yet
- ATrial FibrillationDocument21 pagesATrial FibrillationMohammad Farouq OmarNo ratings yet
- Approach To Dyspnea: Dr. Ghulam Hussain Baloch Associate Professor of Medicine LUMHS, JamshoroDocument48 pagesApproach To Dyspnea: Dr. Ghulam Hussain Baloch Associate Professor of Medicine LUMHS, JamshoroAndita Delifauzan SyabanaNo ratings yet
- 6 BradycardiaDocument20 pages6 BradycardiaTejas Vivek WaghNo ratings yet
- Treatment Protocol For Hypertension: Criteria For Diagnosing High Blood PressureDocument3 pagesTreatment Protocol For Hypertension: Criteria For Diagnosing High Blood PressureHarshitha LokeshNo ratings yet
- Acls TachiDocument1 pageAcls TachiratnawkNo ratings yet
- Dysrhythmias NotesDocument23 pagesDysrhythmias NoteskmimmackNo ratings yet
- Cardiology FMDocument25 pagesCardiology FMtrushaNo ratings yet
- Cardiac Care and COVID-19: Perspectives in Medical PracticeFrom EverandCardiac Care and COVID-19: Perspectives in Medical PracticeNo ratings yet
- Guide to Canine and Feline ElectrocardiographyFrom EverandGuide to Canine and Feline ElectrocardiographyRuth WillisNo ratings yet
- Daftar Pustaka PreliminaryDocument1 pageDaftar Pustaka Preliminarychr0m3b4tm4nNo ratings yet
- BoaDocument2 pagesBoachr0m3b4tm4nNo ratings yet
- ExoDocument1 pageExochr0m3b4tm4nNo ratings yet
- 1Document3 pages1nikojoeNo ratings yet
- LuisDocument3 pagesLuischr0m3b4tm4nNo ratings yet
- ExoDocument2 pagesExochr0m3b4tm4nNo ratings yet
- ExoDocument1 pageExochr0m3b4tm4nNo ratings yet
- SubmarineDocument1 pageSubmarinechr0m3b4tm4nNo ratings yet
- ExoDocument2 pagesExochr0m3b4tm4nNo ratings yet
- ExoDocument1 pageExochr0m3b4tm4nNo ratings yet
- Daftar PustakaDocument1 pageDaftar Pustakachr0m3b4tm4nNo ratings yet
- DenadaDocument3 pagesDenadachr0m3b4tm4nNo ratings yet
- New Text DocumentDocument1 pageNew Text Documentchr0m3b4tm4nNo ratings yet
- New Text DocumentDocument1 pageNew Text Documentchr0m3b4tm4nNo ratings yet
- BOTRDocument1 pageBOTRchr0m3b4tm4nNo ratings yet
- Atrial Fibrillation: The Most Common ArrhythmiaDocument2 pagesAtrial Fibrillation: The Most Common Arrhythmiachr0m3b4tm4nNo ratings yet
- 14 CTN CelebiDocument3 pages14 CTN Celebichr0m3b4tm4nNo ratings yet
- Pi Catheter Ablation Ventricular TachycardiaDocument16 pagesPi Catheter Ablation Ventricular Tachycardiachr0m3b4tm4nNo ratings yet
- Atrial Fibrillation: The Most Common ArrhythmiaDocument2 pagesAtrial Fibrillation: The Most Common Arrhythmiachr0m3b4tm4nNo ratings yet
- TachalgoDocument1 pageTachalgochr0m3b4tm4nNo ratings yet
- Daftar PustakaDocument1 pageDaftar Pustakachr0m3b4tm4nNo ratings yet
- Ellie Goulding Love Me Like You DoDocument1 pageEllie Goulding Love Me Like You Dochr0m3b4tm4nNo ratings yet
- Dora Dora - Alex MicaDocument2 pagesDora Dora - Alex Micachr0m3b4tm4nNo ratings yet
- Imagine Dragon - DemonsDocument2 pagesImagine Dragon - Demonschr0m3b4tm4nNo ratings yet