Professional Documents
Culture Documents
EMRA Sepsis Card 2013
EMRA Sepsis Card 2013
Uploaded by
zoccer01Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
EMRA Sepsis Card 2013
EMRA Sepsis Card 2013
Uploaded by
zoccer01Copyright:
Available Formats
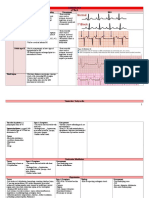
Sepsis Card
Authors: Stephen Boone, MD; Christian Coletti, MD; John Powell, MD
Severe sepsis affects approximately one million patients and claims more than 250,000 lives
each year in the U.S. It is the second leading cause of death in non-cardiac ICU patients. Early
and aggressive therapy influences outcomes. Utilizing the Surviving Sepsis Campaign Guidelines
improves morbidity and can decrease mortality by 25%.
INFECTION
Defined as a pathologic process caused by the invasion of normally sterile tissue, fluid or body cavity
by pathogenic microorganisms.
SEPSIS
Defined as a suspected or documented infection and two or more of the following variables:
Temperature: > 38.3C (> 101F) or < 36C (< 96.8F)
Heart Rate > 90 bpm
Respiratory Rate > 20 breaths/min
Acutely altered mental status
Hyperglycemia (glucose > 140 mg/dL OR 7.7 mmol/L) in the absence of diabetes
WBC > 12,000/mm3, < 4000/mm3, OR > 10% immature (band) forms
Plasma C-reactive protein more than two SD above the normal value
Plasma procalcitonin more than two SD above the normal value
SEVERE SEPSIS
Defined as sepsis-induced organ dysfunction or tissue hypoperfusion. Organ system dysfunction must
be remote to the site of infection with the exception of pulmonary criteria.
Cardiovascular
Hypotension (SBP < 90 mm Hg, MAP < 70 mm Hg OR an SBP decrease > 40 mm Hg)
Pulmonary
Acute Respiratory Distress Syndrome:
PaO2/FiO2 < 250 in absence of PNA as source
PaO2/FiO2 < 200 with PNA as source
Renal
Acute oliguria (UO < 0.5 mL/kg/hr for 2 hrs despite adequate fluid resuscitation)
Creatinine increase > 0.5 mg/dL from baseline
Hemotologic
Coagulation dysfunction (INR > 1.5 OR PTT > 60 secs absent anticoagulant usage)
Thrombocytopenia (platelet count < 100,000/mm3)
Hepatic/GI
Hyperbilirubinemia (total bilirubin > 2 mg/dL)
Systemic
Hyperlactemia > 2 mmol/L (18.0 mg/dL)
Decreased capillary refill or skin mottling
SEPSIS-INDUCED TISSUE HYPOPERFUSION
Defined as (1) sepsis-induced persistent hypotension (SBP < 90 mmHg, a MAP < 70 or a SBP decrease
> 40 mmHg from baseline) or (2) lactate 4.0 mg/dL or (3) oliguria.
Septic shock is sepsis-induced tissue hypoperfusion not responding to 30 mL/kg crystalloid bolus.
CONSIDERATION FOR A NON-INVASIVE APPROACH
The literature supporting a bundled approach to sepsis management that includes CVC insertion
is robust and must not be minimized; however, evidence for a non-invasive approach is available.
Evidence is available that may support a practitioners decision to utilize such an approach in selected
patients. Rather than using CVP and ScVO2, proponents of this approach suggest use of dynamic IVC
ultrasound to guide fluid administration along with lactate clearance of greater than 10% to guide
further therapy. Although further trials comparing the two approaches are in order, a non-invasive
strategy should be considered in selected patients for whom placement of a central line is not feasible
or incongruent with the patients goals of care.
Addressing Goals of Care Despite optimal medical therapy, severe sepsis is a devastating illness
that often results in either death or survival with poor quality of life. It is essential that goals of care be
addressed with patients and their families as early as is feasible. Physicians should establish realistic
treatment goals and incorporate these goals of care into the treatment plan. In some cases, provision
of less aggressive treatments or withdrawal of life-sustaining measures may be in the patients best
interest.
Antibiotics and Source Control Broad spectrum intravenous anti-infective therapy should be
started as soon as possible and within the first hour of recognition of severe sepsis. Initial empiric
therapy should include one or more drugs that have activity against all likely pathogens (to include
antifungals) that penetrate in adequate concentrations into the presumed source of sepsis. Consider
your community and hospital microorganism susceptibility patterns. Before starting antibiotics, obtain
two or more blood cultures. At least one blood culture should be percutaneous. Evaluate for a focus of
infection and initiate source control, e.g. abscess drainage or tissue debridement. Potentially infected
catheters should be removed promptly after other access is established.
Fluid Therapy Initial fluid resuscitation should consist of rapid delivery of at least 30 mL/kg of
crystalloid. Additional fluid resuscitation should be guided by clinical assessment of need and tolerance.
Albumin may be used in the initial resuscitation of patients who require substantial amounts of
crystalloids. A more conservative fluid strategy should be considered for patients with acute respiratory
distress syndrome without evidence of tissue hypoperfusion.
Vasopressors Start vasopressor therapy when fluid challenge fails to restore mean arterial pressure
to 65 mmHg or prior to fluid resuscitation in the presence of very low MAP. A target MAP greater
than 65 mm Hg may be required in patients with baseline hypertension showing persistent signs of
inadequate perfusion despite meeting MAP goal.
Norepinephrine infused via central access is the initial vasopressor of choice. Vasopressin
0.03 units/min may be started as adjunct to norepinephrine at a non-titrated dose. Epinephrine,
substituted for or in addition to norepinephrine, should be the first alternative agent in septic shock that
is poorly responsive to first-line therapy. Dopamine should only be used in highly selected patients with
bradycardia and low risk of tachyarrhythmia.
Once vasopressors are initiated, an arterial catheter should be placed as resources and time permit.
Inotropic Therapy Consider dobutamine in patients with ongoing evidence of hypoperfusion
despite achieving adequate volume resuscitation and adequate mean arterial pressure. Do not
arbitrarily increase cardiac index to achieve an elevated level of oxygen delivery.
Steroids Patients with persistent hypotension despite fluid resuscitation and vasopressor support
should receive hydrocortisone 200 mg/day. Administration as a continuous infusion may lower the
incidence of hyperglycemia and hypernatremia. Routine ACTH stimulation testing is not recommended.
Gradually taper steroid therapy when vasopressors are no longer needed.
Blood Product Administration
Transfuse red blood cells when hemoglobin is < 7.0 g/dL to a target of 7.0-9.0 g/dL. Consider
higher transfusion thresholds for patients with severe hypoxemia, active ischemic coronary
disease, or acute hemorrhage.
Transfuse blood products to correct coagulopathy only in patients with active bleeding or
planned invasive procedures.
Transfuse platelets when count is <10,000/mm3 regardless of bleeding, or if count is
< 20,000/mm3 with significant bleeding risk. Consider higher platelet goal (50,000/mm3)
for surgery or invasive procedures.
Lung Protective Strategy: Ventilation with Low Tidal Volumes
Avoid high tidal volume coupled with high plateau pressures by decreasing tidal volumes to
6 mL/kg (based on ideal body weight) with the goal of maintaining end-inspiratory plateau
pressures < 30 cm H2O.
Set PEEP based on the severity of oxygenation deficit.
Consider permissive hypercapnia (allowing PaCO2 to increase above its pre-morbid baseline) in
patients with ARDS if needed to minimize plateau pressures and tidal volumes.
Consider alternative ventilation modes, e.g. PCV or APRV for potentially injurious FiO2 or plateau
pressure > 30 cm H2O. Proning the patient is another option.
Raise head of bed 30-45 degrees (unless contraindicated) to prevent ventilator-acquired
pneumonia.
Glucose Control After the first six hours, maintain blood glucose <180 mg/dL using continuous or
intermittent insulin. Monitor blood glucose every 60 minutes until stabilized, then every 4 hours.
Lactate Clearance The inability to clear lactate during sepsis is associated with a higher mortality
rate compared to patients who are able to clear their serum lactate early in resuscitation. The use of
lactate clearance may be a feasible option for patients in whom ScVO2 is unavailable, or may be used in
combination with ScVO2 normalization.
Deep Vein Thrombosis and Stress Ulcer Prophylaxis Administer prophylactic low molecular
weight heparin or unfractionated heparin. Use a mechanical compression device for patients with a
contraindication to LMWH or UFH. Provide stress ulcer prophylaxis with either H2 receptor or proton
pump inhibitors. More recent analyses have provided evidence suggesting improved prophylaxis with
proton pump inhibitors compared to H2 receptor blockers.
Angus DC, et al., CCM 2001(29)7
Martin GS et al., NEJM 2003 (348)16
Hotchkiss RS et al., NEJM 2003, (348)2
Dellinger RP, et al., CCM 2013 (41)2
SSC: survingsepsis.org
References
Bendjelid K, Romand JA: Fluid responsiveness in mechanically ventilated patients: A review of indices used in intensive care.
Intensive Care Med 2003; 29:352360
Gaieski D, McCoy J, Zeserson E, Chase M, Goyal M. Mortality benefit after implementation of early goal directed therapy protocol
for the treatment of severe sepsis and septic shock. Ann Emerg Med. 2005;46:S4.
Jones AE, Shapiro NI, et al.; Emergency Medicine Shock Research Network (EMShockNet) Investigators. Lactate clearance vs
central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010 Feb;303(8)
Multicenter study of early lactate clearance as a determinant of survival in patients with presumed sepsis. Arnold RC, Shapiro
NI, Jones AE, Schorr C, Pope J, Casner E, Parrillo JE, Dellinger RP, Trzeciak S; Emergency Medicine Shock Research Network
(EMShockNet) Investigators. Shock. 2009 Jul;32(1):35-9.
Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Nguyen HB, Rivers EP, Knoblich BP,
Jacobsen G, Muzzin A, Ressler JA, Tomlanovich MC. Crit Care Med. 2004 Aug;32(8):1637-42.
Derived from the Levy MM et all CM 2003 (3)4
Osborn TM et al AEM 2005 (46)3
Dillenger RP et al, CCM 2013 (41)2
2013 This card should be used only as a guideline. In each individual case, the user must ultimately rely on current literature
and the manufacturers product and package insert for additional information on the products recommended use, warnings
and contraindications.
SEPSIS BUNDLE GOALS FOR SEVERE SEPSIS/SEPTIC SHOCK:
(PROTOCOL-DRIVEN SYSTEM RECOMMENDED)
TO BE COMPLETED WITHIN 3 HOURS
1) Measure lactate level.
2) Obtain blood cultures prior to administration of antibiotics.
3) Administer broad spectrum antibiotics.
4) Administer 30 mL/kg crystalloid for hypotension or lactate 4mmol/L.
TO BE COMPLETED WITHIN 6 HOURS
5) Apply vasopressors (for hypotension that does not respond to initial fluid resuscitation) to
maintain a mean arterial pressure (MAP) 65 mm Hg.
6) In the event of persistent arterial hypotension despite volume resuscitation (septic shock) or
initial lactate 4 mmol/L (36 mg/dL):
Measure central venous pressure (CVP).*
Measure central venous oxygen saturation (ScvO2).*
7) Remeasure lactate if initial lactate was elevated.*
*Targets for quantitative resuscitation included in the guidelines are CVP of 8 mm Hg, ScvO2 of 70%, and normalization
of lactate.
Bendjelid K, et al. ICM 2003; 29:352360
Gaieski D, et al. AEM 2005;46:S4
Sepsis Pathway
Lactate 4 mmol/L or persistent hypotension
despite 30 mL/kg crystalloid or colloid equivalent
Broad Spectrum
Antibiotics
< 8 mm Hg
CVP
CVP
8-12 mm Hg
Central Line Placement for
CVP/Scv02 Monitoring
Fluid Bolus
If CVP < 8 (< 12 if mechanically ventilated);
Give Fluid: Give 500-1000 mL crystalloid boluses q30 minutes until CVP goal
achieved, then 150 mL/hr. Consider albumin boluses for patients requiring
substantial amounts of crystalloid.
MAP < 65 mm Hg
Vassopressor
MAP
MAP 65 mm Hg
Scv02
< 70%
70%
Goal Achieved
Rivers E, et al. NEJM, 2001;345:1368-1377
If MAP <65, initiate vasopressors.
Norepinephrine: NE is the vasopressor of choice in the treatment of septic shock.
Vasopressin: 0.03 units/min IV as adjunct to NE
Epinephrine: Preferred 2nd line agent added to or substituted for NE
Place arterial catheter as time and resources allow.
Oxygen Delivery
If ScVO2 remains < 70%, oxygen delivery must be further optimized
with pRBC transfusion and/or inotrope therapy:
Transfuse two units pRBCs for Hgb < 7g/dl or consider for Hgb
< 10g/dl if ischemic heart disease or hypoxia.
Initiate inotrope therapy: Dobutamine 2-5 mcg/kg/min
You might also like
- Critical Care Intravenous DrugsDocument1 pageCritical Care Intravenous DrugsMarynel Dixie Izon Brao91% (11)
- Bouncebacks! Critical Care: Avoid Serious Mistakes in the EDFrom EverandBouncebacks! Critical Care: Avoid Serious Mistakes in the EDRating: 5 out of 5 stars5/5 (2)
- UCSF Hospitalist HandbookDocument58 pagesUCSF Hospitalist Handbookniharjhatn100% (2)
- Electrocardiography in Emergency, Acute, and Critical Care, 2nd EditionFrom EverandElectrocardiography in Emergency, Acute, and Critical Care, 2nd EditionRating: 5 out of 5 stars5/5 (1)
- Emergency Department Resuscitation of the Critically Ill, 2nd Edition: A Crash Course in Critical CareFrom EverandEmergency Department Resuscitation of the Critically Ill, 2nd Edition: A Crash Course in Critical CareNo ratings yet
- Emra Medical Student Survival Guide 2edDocument288 pagesEmra Medical Student Survival Guide 2edtamikanji50% (2)
- EMRA Antibiotic Guide EMRADocument2 pagesEMRA Antibiotic Guide EMRAPaoNu0% (3)
- Icu GuidebookDocument43 pagesIcu Guidebookdrimran570100% (5)
- Advanced Medicine Recall A Must For MRCP PDFDocument712 pagesAdvanced Medicine Recall A Must For MRCP PDFKai Xin100% (2)
- Bedside Critical Care Guide PDFDocument91 pagesBedside Critical Care Guide PDFAyu Rahmatullah100% (4)
- Rapid Interpretation of EKG's 6th EdDocument14 pagesRapid Interpretation of EKG's 6th EdDenise De Los Reyes100% (2)
- Anesthesiology Resident Manual of Procedures: A Step-by-Step GuideFrom EverandAnesthesiology Resident Manual of Procedures: A Step-by-Step GuideNo ratings yet
- Prehospital Practice: hypothetically speaking: From classroom to paramedic practice Volume 1 Second editionFrom EverandPrehospital Practice: hypothetically speaking: From classroom to paramedic practice Volume 1 Second editionNo ratings yet
- Carol Rivers'board Review FlashcardsDocument440 pagesCarol Rivers'board Review FlashcardsJennelle CadoganNo ratings yet
- Drug Infusions in ICU Made Simple 2016 by MansdocsDocument28 pagesDrug Infusions in ICU Made Simple 2016 by Mansdocsabdullah almatary0% (1)
- Intern Survival Guide: Because You Got ThisDocument26 pagesIntern Survival Guide: Because You Got ThisCatalina Borquez100% (8)
- UCLA Intern Survival GuideDocument57 pagesUCLA Intern Survival GuideKevin Lewis100% (3)
- Critical Care NotesDocument18 pagesCritical Care NotesjulieNo ratings yet
- MGH Handbook of Neurology 2ndDocument355 pagesMGH Handbook of Neurology 2nddoctorhousemedNo ratings yet
- Critical Care - ICU Skills ChecklistDocument2 pagesCritical Care - ICU Skills ChecklistRandi Brown0% (1)
- Trauma Case Studies: Teamwork Leading To Great SavesDocument46 pagesTrauma Case Studies: Teamwork Leading To Great SavesBrett DoddNo ratings yet
- Sajjan M MBBS Learn ECG in A Day A Systemic ApproachDocument99 pagesSajjan M MBBS Learn ECG in A Day A Systemic Approachv@r0_5100% (9)
- Absite Review VascularDocument183 pagesAbsite Review Vascularsgod34No ratings yet
- How To Read A Medical ReportDocument3 pagesHow To Read A Medical ReportpinkuNo ratings yet
- Icu Survival Guide: SUNY Upstate Medical UniversityDocument36 pagesIcu Survival Guide: SUNY Upstate Medical UniversitySAUMOJIT MAJUMDERNo ratings yet
- Starting Out - New in The ICUDocument30 pagesStarting Out - New in The ICUashdmb217100% (1)
- Rapid Sequence Intubation ReportDocument55 pagesRapid Sequence Intubation Reportlorkan19100% (1)
- Pocket Manual in Critical CareDocument356 pagesPocket Manual in Critical CareTahir Uddin Qazi86% (7)
- Electrolyte CompleteDocument6 pagesElectrolyte CompleteTofan Ana100% (2)
- Intern Survival Guide 2012-2013Document23 pagesIntern Survival Guide 2012-2013alaa100% (1)
- Icu Cheat Sheet Working FileDocument7 pagesIcu Cheat Sheet Working FileBhumiShahNo ratings yet
- Intern Survival Guide 2014-2015Document145 pagesIntern Survival Guide 2014-2015PreaisNo ratings yet
- Residents Critical Care HandbookDocument135 pagesResidents Critical Care Handbookjonathanrubin0921No ratings yet
- Critical Care Reviews Book 2017Document356 pagesCritical Care Reviews Book 2017Herbert Baquerizo VargasNo ratings yet
- Hopkins Intern Survival Guide PDFDocument43 pagesHopkins Intern Survival Guide PDFsgod34No ratings yet
- Orientation ResidenecyDocument18 pagesOrientation ResidenecyReeMii AngeLa100% (1)
- Critical Care Survival GuideDocument2 pagesCritical Care Survival Guidetringalama100% (4)
- Study Notes Internal MedicineDocument2 pagesStudy Notes Internal MedicineBob0% (2)
- Critical Care PhysiologyDocument287 pagesCritical Care Physiologyashdmb217100% (7)
- Emergency Care Algorithms 2018 PDFDocument77 pagesEmergency Care Algorithms 2018 PDFFranklin Correa100% (2)
- Surgical Critical Care and Emergency Surgery: Clinical Questions and AnswersFrom EverandSurgical Critical Care and Emergency Surgery: Clinical Questions and AnswersForrest "Dell" MooreNo ratings yet
- EMRA 101 Info For Med StudentsDocument15 pagesEMRA 101 Info For Med StudentsEMRANo ratings yet
- Intern Ward Survival Guide 2009Document5 pagesIntern Ward Survival Guide 2009mediquest100% (1)
- Approach To Emergency PatientDocument18 pagesApproach To Emergency PatientJuan Pablo Gallardo ContrerasNo ratings yet
- ED Study GuideDocument59 pagesED Study Guidemmmmz100% (1)
- Utmck Survival Guide 2010Document46 pagesUtmck Survival Guide 2010sha89No ratings yet
- UVa Trauma PearlsDocument130 pagesUVa Trauma Pearlssgod34No ratings yet
- ACLS Advanced Cardiovascular Life Support Provider Manual 2023From EverandACLS Advanced Cardiovascular Life Support Provider Manual 2023No ratings yet
- EFCCSSUDocument785 pagesEFCCSSUchepebetosmNo ratings yet
- Critical CareDocument40 pagesCritical Carenkuligowski100% (6)
- Intern Survival Guide The UNC Department of MedicineDocument22 pagesIntern Survival Guide The UNC Department of MedicinecmirceaNo ratings yet
- Acute Resuscitation and Crisis Management: Acute Critical Events Simulation (ACES)From EverandAcute Resuscitation and Crisis Management: Acute Critical Events Simulation (ACES)David NeilipovitzNo ratings yet
- PALS Algorithms 2019 (Pediatric Advanced Life Support)Document1 pagePALS Algorithms 2019 (Pediatric Advanced Life Support)darlingcarvajalduque100% (1)
- EMRA SportsMedicine Splint GuideDocument4 pagesEMRA SportsMedicine Splint Guidehppyduck32No ratings yet
- Surgery Preround Template SkeletonDocument2 pagesSurgery Preround Template Skeletonsgod34No ratings yet
- Nutrition Support: Sean P Harbison MDDocument42 pagesNutrition Support: Sean P Harbison MDsgod34No ratings yet
- NOAC ChartDocument2 pagesNOAC Chartsgod34No ratings yet
- Master Schedule 10-22Document65 pagesMaster Schedule 10-22sgod34No ratings yet
- Modes of Mechanical VentilationDocument4 pagesModes of Mechanical Ventilationsgod34100% (1)
- 7 MedEd Vascular Jonny Hodgkinson 12.11.12 1Document35 pages7 MedEd Vascular Jonny Hodgkinson 12.11.12 1sgod34No ratings yet
- Veins More DistensibleDocument27 pagesVeins More Distensiblesgod34No ratings yet
- Anast Bleed MMDocument17 pagesAnast Bleed MMsgod34No ratings yet
- HD Monitoring ColoradoDocument28 pagesHD Monitoring Coloradosgod34No ratings yet
- Venous DiseaseDocument50 pagesVenous Diseasesgod34No ratings yet
- Endoscopy TechniqueDocument8 pagesEndoscopy Techniquesgod34No ratings yet
- Resident Hernia LectureDocument106 pagesResident Hernia Lecturesgod34No ratings yet
- Riker ABSITE ReviewDocument36 pagesRiker ABSITE Reviewsgod34No ratings yet
- Oligotherapy RemediesDocument9 pagesOligotherapy RemediesLuiz AlmeidaNo ratings yet
- The Many Presentations of Inherited Metabolic DiseasesDocument31 pagesThe Many Presentations of Inherited Metabolic DiseasesMateen ShukriNo ratings yet
- JC 2014 Home Economics Food Culinary Skills - Assessment FormatDocument4 pagesJC 2014 Home Economics Food Culinary Skills - Assessment FormatCharlie RNo ratings yet
- Tube Thoracostomy Chest Tube Implantation and Follow Up: Review ArticleDocument10 pagesTube Thoracostomy Chest Tube Implantation and Follow Up: Review ArticleAnasthasia hutagalungNo ratings yet
- NAPZA Is The Abbreviation of DrugsDocument24 pagesNAPZA Is The Abbreviation of DrugsFahmi ArdianNo ratings yet
- D and CDocument3 pagesD and Cclide11No ratings yet
- CPR PresentationDocument11 pagesCPR PresentationPriyanka TripathiNo ratings yet
- Acupuncture PDFDocument61 pagesAcupuncture PDFAsha Mahal PandikkadNo ratings yet
- Nutritional Management of Chyle Leaks: An Update: Nutrition Issues in Gastroenterology, Series #94Document13 pagesNutritional Management of Chyle Leaks: An Update: Nutrition Issues in Gastroenterology, Series #94mmmdeandradeNo ratings yet
- A Cesarean SectionDocument9 pagesA Cesarean SectionmejulNo ratings yet
- Anterior Cruciate Ligament ReconstructionDocument10 pagesAnterior Cruciate Ligament ReconstructionRaquel Brasil (Haki)No ratings yet
- Diagnostic Tests: Neisseria Meningitidis CapsularDocument2 pagesDiagnostic Tests: Neisseria Meningitidis CapsularCherry Mae JasoNo ratings yet
- Hackmann 2011 Imagery Rescripting in PTSDDocument9 pagesHackmann 2011 Imagery Rescripting in PTSDAna FerreiraNo ratings yet
- Municipal Wastewater Management NotesDocument20 pagesMunicipal Wastewater Management NotesMa Teresa Quintos100% (1)
- MSDS Medical Carbon DioxideDocument4 pagesMSDS Medical Carbon DioxideRachel LeeNo ratings yet
- Trojan Uv Swiftect UvphoxDocument6 pagesTrojan Uv Swiftect UvphoxMonicaRossetimNo ratings yet
- Anzhela Fedoronchuk Resume 2Document3 pagesAnzhela Fedoronchuk Resume 2api-315294234No ratings yet
- Drugs Affecting Respiratory SystemDocument62 pagesDrugs Affecting Respiratory Systemyunita ekawatiNo ratings yet
- PT NotesDocument19 pagesPT NotesVenice Marie CordetaNo ratings yet
- Module 14: Substance-Related and Addictive DisordersDocument5 pagesModule 14: Substance-Related and Addictive DisordersLiz EvermoreNo ratings yet
- GENENTECH INC 10-K (Annual Reports) 2009-02-20Document224 pagesGENENTECH INC 10-K (Annual Reports) 2009-02-20http://secwatch.comNo ratings yet
- Happiness Flush EmpowermentDocument18 pagesHappiness Flush EmpowermentHealing Heaven Australia100% (2)
- Personalised MedicineDocument25 pagesPersonalised MedicineRevanti MukherjeeNo ratings yet
- Case 101 Blue Economy Clusters 1-2015Document10 pagesCase 101 Blue Economy Clusters 1-2015Kenaia AdeleyeNo ratings yet
- 0501 Skin CareDocument9 pages0501 Skin CarekinayungNo ratings yet
- 1326 FNLDocument3 pages1326 FNLNaveenbabu SoundararajanNo ratings yet
- 3.2 TheophyllineDocument3 pages3.2 TheophyllinesarahabdullahNo ratings yet
- Chapter 17 About Digestive SystemDocument4 pagesChapter 17 About Digestive SystemArash DhillonNo ratings yet
- PetrofskyDocument15 pagesPetrofskyNestor BalboaNo ratings yet