Professional Documents
Culture Documents
Running Head: Organizational Is Budgeting 1
Uploaded by
api-307874398Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Running Head: Organizational Is Budgeting 1
Uploaded by
api-307874398Copyright:
Available Formats
RUNNING HEAD: ORGANIZATIONAL IS BUDGETING
Article Paper: Organizational IS Budgeting Criteria and Solutions
Ashley Winans
CIS 101
May 30, 2015
Professor Rell Snyder
RUNNING HEAD: ORGANIZATIONAL IS BUDGETING
Article Paper: Organizational IS Budgeting Criteria and Solutions
When tasked with assessing the value of an Information System project, it is essential to
first calculate both the costs and potential benefits. Even in cases where the benefits outweigh the
costs additional financial analysis is required to determine whether the project represents a good
return on the firms invested capital (Laudon & Laudon, 2014, P.539). One method of
determining this is by using a capital budgeting model, which relies upon the measures of cash
flow in and out of a firm. Investing in an information system is an immediate cash outflow;
however, information systems can also generate an inflow of cash if they prove to be beneficial
to the company. In the healthcare industry, information technology and information systems have
been essential in not only been effective in reducing costs, IT has gone beyond cost saving and
has numerous benefits for facilities as well as patients.
Information Systems
Information systems have been defined as online, interactive tools deeply involved in
the minute-to-minute operations and decision making of large organization (Laudon & Laudon,
P. 89). Information Technology, in business as well as in other industries, has the power to
change the costs of information and capital. The amount that a company can spend on IT is often
less than the expenses that would be allocated elsewhere. The cost of IT tends to decrease with
time, and has been associated with saving on the cost of more expensive costs of capital such as
machinery and buildings. Information technology has also played an important role in helping
medical facilities as well as corporations lower the cost of market participation, which will allow
for outsourcing and ultimately saving money. However, financial models can sometimes
overlook and overshadow the social and organizational dimensions of information systems that
may affect the true costs and benefits of the investment (Laudon & Laudon, 2014, P.541).
RUNNING HEAD: ORGANIZATIONAL IS BUDGETING
Cost-Benefit Analysis
Cost-Benefit Analysis, or CBA, is the process of estimating and calculating the
equivalent money value of the benefits and costs of projects to establish whether they are
worthwhile from a financial perspective. CBA is used in planning for numerous fields, including
health care. One example of cost-benefit analysis is utilized as a tool to decide whether a practice
should invest in an electronic health record or other information system. Although CBA assists in
budgeting and planning (where the most financial gains will be had), it fails to measure more
intangible factor, such as provider and patient satisfaction. The long-term benefits of an EHR are
also difficult to project. CBA also underestimates the risks of doing nothing. Especially in health
care, the cost of doing nothing may be the most harmful choice of all. (Tan, 2010).
If a medical practice had not adopted and implemented an EHR, they may have seen
additional costs in some other ways. For example, average monthly revenues increased by 11
percent in the first year following EHR implementation and 20 percent in the second year,
compared with the baseline year (Tan, 2010, P. 367). There are numerous other profits that a
practice may miss out upon. For example, providers and facilities who see Medicare and
Medicaid patients are eligible for Meaningful Use funding to help offset the cost of adopting an
EHR system. However, if these same facilities do not use an EHR system at all, they will start to
face government penalties that will increase every year. (Tan, 2010)
Practice Fusion. One EHR company, Practice Fusion, offers their services for free with
ad banners. This allows smaller practices an affordable way to adopt an EHR when it wouldve
been an unrealistic possibility for them otherwise. Practice Fusion, as of 2014, is one of the top
20 EHR systems used in the United States. According to Ryan Howard, CEO and Founder of
RUNNING HEAD: ORGANIZATIONAL IS BUDGETING
Practice Fusion, "Not only do we remove the cost barriers to technology adoption for doctors, we
also help them pocket $44,000 or more in EMR incentives" (Practice Fusion). Practice Fusions
goal has even been called the catalyst that will enable the 90 percent of US doctors who are still
using paper health records to modernize; leading to more efficiency, enabling greater access to
patient information and empowering doctors to take the best care of patients (Practice Fusion,
2010).
Integrated Billing
InJulyof2009,thestateofMinnesotaimplementedelectronicbillingforallhealthcare
agencies.KeybillingfeatureswithinEHRsystemsorbyclearinghousesmaywellhavesetthe
stageforprovidersacrossthenation.TheMinnesotaDepartmentofHealthstatesthateach
year,morethan55millionmedicalbills,knownashealthcareclaims,fromthesehealthcare
providersareprocessedinMinnesota,resultinginsignificanttransactionscostsand
opportunitiesforsavings(Eisele,2009).
AccordingtoEisele,therearetenkeybillingfeatureswithinasuccessfulEHRthatcan
helppracticesrealizesimilarsavingstothoseofMinnesota.ThesefeaturesareConsiderthese10
billingsystemfeatures:
1. Adaptivesoftwareemphasizingpracticespecifications
2. Conversionof"superbills"toclaims
3. Electronicsubmissionandverificationofclaims
4. Comprehensiveaccounting/billingreports
5. Electronictrackingofpayments;transparentpaymentprocess
6. Claimsrejectionanalysisinrealtimedisplayingclearerrorcodes
7. Integrationofcopaymentsintoschedulingfeatures
8. BillingcodespulleddirectlyfromEHRdocumentation
9. Multiuser,secure,anduserfriendlyinterfacecapabilities
10. Servermonitoring,backups,anddatarecovery
RUNNING HEAD: ORGANIZATIONAL IS BUDGETING
Return On Investment and Analysis
ROI analysis for EHRs is not always used as a management tool, but is instead frequently
used by a CFO to justify a project. These analyses benefit when they receive accurate input from
those responsible for achieving the results and should ideally be used in a formal benefit
realization study that holds people accountable for results. (Amatayakul, 2007)
True Costs and Benefits of EHRs. AccordingtoAmatayakul, identifying the costs and
benefits that contribute to the EHR ROI analysis should begin with defining measurable goals
and setting expectations (Amatayakul, 2007, P. 146).Mostorganizations do not anticipate the
longer-term effects of a single goal as well as its associated costs and do not at all address how
they will ensure that their intended users will actually use the systems that are being
implemented. Although the process of change must be accounted for as a cost, but preparing for
this in the long term can lead to better benefits.
Additionally, a medical organization may need to invest in computer skills building for
physicians, formal work flow analysis, physician activities to develop standing orders in support,
a clinical data analyst to build standing order templates and CDS rules, as well as
troubleshooting and backup plans for the new systems. When both end users and providers are
engaged in the process of defining the goals and understanding the expectations associated with
them, they are more likely to comply. (Amatayakul, 2007)
According to Amatayakul, when an organization develops an ROI without adequate
resources or specific expectations of the benefits it hopes to achieve, the organization is setting
itself up to fail (Amatayakul, 2007, P. 147). When it comes to EHR adoption, organizations
must be willing to address the true costs and benefits associated with effecting change. The best
RUNNING HEAD: ORGANIZATIONAL IS BUDGETING
way to achieve this is to devote the proper resources resources to it and setting expectations clear
for accomplishment of goals. (Amatayakul, 2007)
System Analysis. Likewise, system analysis creates road maps of existing organizations
and their systems. It would then be the job of the systems analyst to examine the problems of the
current system in order to better implement a new one. End users are often critical in redesigning
systems to flow properly in the workplace. For successful HER implementation, often times
organization will hire a System Analyst or similarly qualified individual in order to ease the
stress of the transition as well as impart knowledge and experience on the company. (Laudon &
Laudon, 2014)
EHR Implementation
Implementation is the process wherein organizational activities work towards the
adoption, management, and routinization of an innovation, such as a new formation system
(Laudon & Laudon, 2014, P.542). The implementation system greatly benefits from the active
role of end users.
EHR implementation also has a major effect on patient care, workflow, and an eventual
return on investment. There are several key factors to consider when implementing an EHR in
order to make to process as productive as possible. The first is to put together a multidisciplinary
team, as the EHR process involves numerous individuals and processes. It is better to get
perspective on the process from start to finish in order to troubleshoot and gain different
perspectives. A process analysis should also be not only drawn, but also reviewed by staff who
will actually be performing the tasks. This will also give everyone a chance to see how different
job duties have evolved and what tasks will be designated to different staff members. It is also
RUNNING HEAD: ORGANIZATIONAL IS BUDGETING
important NOT to adopt the workflow design, which is recommended by the EHR vendor, and to
remember that clinic employees are the best experts of overall workflow as well as job duty
specificity. A project manager or point person should also be put in change and empowered to
keep things moving and be aware of the need for continual updates. It is also important to match
your actual practice and workflow to the template you have designed for your office.
Perhaps most importantly, workflow analysis is a human interaction-driven process
which must also adhere to the belief that the fact that workflow and job duties are constantly
changing and evolving. The role of end users is often essential to a successful system
implementation as incorporating user knowledge and expertise leads to better solutions
(Laudon & Laudon, 2014, P. 542). There sometimes exists a user-designation gap, which
constitutes the differences between the end-users and information systems specialists. The
success of project implementation decreases with the larger the gap is between the technical
specialists and end users.
Decision-Support Systems
Many health information systems contain or are associated with a DSS, or DecisionSupport System, DSS, like other IS, is a tool that is effective only when the business context is
well understood (Tan, 2009, P. 381). The DSS provides structured decisions to providers, which
can be essential at times. By contrast, unstructured decisions are those in which the decision
maker must provide judgment, evaluation, and insight to solve the problem and this is often due
to the fact that unstructured decisions are novel, important, and nonroutine, and there is no wellunderstood or agreed-on procedure for making them (Laudon & Laudon, 2014, P. 456).
If a DSS can inform you to make better decisions, there can be a positive financial aspect
as well. Even thousands of smaller, but better informed decisions could add up to large savings.
RUNNING HEAD: ORGANIZATIONAL IS BUDGETING
Decision Support System ROI. Measuring the cost of a return on the investment in the
DSS is no small task. Information paradox is a term that refers to the lack of conclusive evidence
of IT payoff. Investing in IT can sometimes be an absolute necessity, but other times may seem
difficult to quantify. In recent times, there have been increased efforts towards analyzing IT pay
off, which include analyzing three years of monthly actual DSS usages at various hospitals where
it was implemented. This method has become a promising place to start in determining how to
measure this sort of investment. Some facilities have designed strategic formulas in order to
measure the financial outcome.
EHR Financial Incentives
Aside from the potential financial gains that a hospital or practice will experience through
using an EHR, financial incentives for the implementation and meaningful use of electronic
health records exist through the American Recovery and Reinvestment Act of 2009. The
potential financial benefits of EHR use are much greater than the incentives healthcare
organizations could stand to gain from the government. Documented case studies have proven
that EHRs can help control hospital costs. However, although published examples support the
idea that implementation of EHRs can save hospitals money, one recent study found that
computerization, in general, does not appear to have helped most hospitals reduce clinical
resource utilization and costs. The reason maybe that most hospitals with EHRs have not yet
implemented the two key elements that drive most of an EHR's financial benefits: clinical
decision support and performance management, the latter of which can also be thought of as
operational decision support. (Thompson, 2010)
Value Planning
RUNNING HEAD: ORGANIZATIONAL IS BUDGETING
Many hospitals estimate the financial benefits of their EHRs to calculate an expected
return on investment for internal financial planning or to or in order to influence health care
leaders on an EHR purchase. Numerous hospitals are going beyond this approach in order to
carefully plan for the clinical and financial benefits of their EHR systems. EHR value planning
includes:
1. Value framework development
2. Value modeling
3. Benefit requirement identification and risk mitigation
4. Integrated planning
5. Value measurement
6. Organizing for value.
This may seem like a daunting task for many people faced with it. However, according to
Thompson, if system benefits are the reason people buy information systems, if failure to
realize those benefits puts organizations at risk, and if understanding and measuring benefits
increases the odds of realizing them, then they have a duty to use a value planning approach
(Thompson, 2006, P. 108).
Tangible and Intangible Benefits
Whereas tangible benefits can be quantified and given a monetary value, intangible
benefits cannot have an exact value placed upon them. Intangible values include efficient
customer service or long-term company goals. However, the traditional focus on the financial
RUNNING HEAD: ORGANIZATIONAL IS BUDGETING
10
and technical aspects of an information system tends to overlook the social an organizational
dimensions of information systems that may affect the true costs and benefits of the investment
(Laudon & Laudon, 2014, P. 541).
Conclusion
As in any other industry, implementation of an information system in health care can be a
process that is financially beneficial when implemented correctly. There are numerous
considerations to be made when implementing a system such as an EHR or DSS. Oftentimes, a
return on investment cannot be seen right away so it is essential to make the proper projections
and plan accordingly.
RUNNING HEAD: ORGANIZATIONAL IS BUDGETING
11
References
Adler, K. (1995, July). Estimating software aids budgeting. American City & County, 110(8), 10.
Amatayakul, M. (2007). Do you plan not to achieve your EHR ROI? Healthcare Financial
Management, 61(11), 146-7.
Eisele, K. (2009, July 7). 10 Essential Billing Features Your EHR System Should Address.
Retrieved May 30, 2015, from http://www.ehrinstitute.org/articles.lib/items/10-EssentialBilling
Integrity of the Healthcare Record: Best Practices for EHR Documentation. (n.d.). Retrieved May
29, 2015, from
http://library.ahima.org/xpedio/groups/public/documents/ahima/bok1_050286.hcsp?
dDocName=bok1_050286
Laudon, K.C., & Laudon, J.P. (2014). Managing information systems: Managing the digital firm
(14th ed.). Upper Saddle River, NJ: Pearson Education, Inc.
Practice fusion secures new investors. (2011). Professional Services Close - Up, Retrieved from
http://search.proquest.com/docview/894142307?accountid=158660
Ransom, E.R., Joshi, M.S., Nash, D.B., & Ransom, S.B. (eds.). (2008). Healthcare quality book:
Vision, strategy, and tools (2nd ed.). Chicago, IL: Health Administration Press.
RUNNING HEAD: ORGANIZATIONAL IS BUDGETING
12
Tan, J. (2010). Adaptive Health Management Information Systems Concepts, Cases, and
Practical Applications, third edition (3rd ed.). Sudbury, Mass.: Jones and Bartlett.
Thompson, D., Velasco, F., Classen, D., & Raddemann, R. J. (2010). Reducing clinical costs with
an EHR. Healthcare Financial Management, 64(10), 106-8, 110, 112.
Thompson, D. (2006). EHR value: Don't expect what you don't plan for. Healthcare Financial
Management, 60(12), 58-62, 64, 66.
You might also like
- Hca 626 Casestudy 3Document7 pagesHca 626 Casestudy 3api-307874398No ratings yet
- Shared Services For HealthcareDocument9 pagesShared Services For HealthcareNeeraj SabhnaniNo ratings yet
- Hca 626 Casestudy 3Document7 pagesHca 626 Casestudy 3api-307874398No ratings yet
- EIA For Maize & Wheat Milling Plant DEI PDFDocument110 pagesEIA For Maize & Wheat Milling Plant DEI PDFSasira Fionah100% (2)
- Enlc 553 Strategic Business ProposalDocument18 pagesEnlc 553 Strategic Business Proposalapi-459703752No ratings yet
- Mid 185 - Pid 70 - Fmi 2Document3 pagesMid 185 - Pid 70 - Fmi 2Akbar100% (1)
- The Financial Implications of Electronic Health RecordsDocument13 pagesThe Financial Implications of Electronic Health Recordsapi-612297093No ratings yet
- Data Work Feb12Document8 pagesData Work Feb12James WaigwaNo ratings yet
- Henry Nnorom. Electronic Health Records (2021SU) Summer 2021Document4 pagesHenry Nnorom. Electronic Health Records (2021SU) Summer 2021henry nnoromNo ratings yet
- Outsourcing Technology In the Healthcare Industry: In Depth Research to Protect the Security, Technology, and Profitability of Your BusinessFrom EverandOutsourcing Technology In the Healthcare Industry: In Depth Research to Protect the Security, Technology, and Profitability of Your BusinessNo ratings yet
- Thesis On Hospital Management Information SystemDocument4 pagesThesis On Hospital Management Information Systemfygynejoheg2No ratings yet
- Payroll Full SystemDocument32 pagesPayroll Full SystemSaurabh Agarwal0% (1)
- A Cost Based Analysis of Implementing An Electronic System Versus Using A Paper Based System.Document6 pagesA Cost Based Analysis of Implementing An Electronic System Versus Using A Paper Based System.paulineNo ratings yet
- Project Management ProblemsDocument5 pagesProject Management Problemsapi-655123959No ratings yet
- Running Head: Cost-Benefit Analysis of Electronic Health RecordsDocument11 pagesRunning Head: Cost-Benefit Analysis of Electronic Health RecordsBilal Ahmad BhatNo ratings yet
- Textbook of Urgent Care Management: Chapter 23, Choosing the Electronic Health RecordFrom EverandTextbook of Urgent Care Management: Chapter 23, Choosing the Electronic Health RecordNo ratings yet
- Unifying Governance For: Disparate Healthcare TechnologiesDocument4 pagesUnifying Governance For: Disparate Healthcare Technologiesjagan ReddyNo ratings yet
- "Cost-Benefit" Analysis Applied To Personnel/ Human Resource Management DecisionsDocument13 pages"Cost-Benefit" Analysis Applied To Personnel/ Human Resource Management DecisionsAman KumarNo ratings yet
- Htm660casestudy17 1Document6 pagesHtm660casestudy17 1api-307874398No ratings yet
- White PaperDocument9 pagesWhite Paperapi-273331267No ratings yet
- Ehr ThesisDocument8 pagesEhr Thesisjenniferlopezhayward100% (1)
- Implementing Electronic Health Records in Hospitals A Systematic Literature ReviewDocument5 pagesImplementing Electronic Health Records in Hospitals A Systematic Literature Reviewc5p8vze7No ratings yet
- HCD WP 2012 CommunityHospitalsCanBenefitDocument8 pagesHCD WP 2012 CommunityHospitalsCanBenefitPatBickleyNo ratings yet
- Erp Word VersionDocument6 pagesErp Word VersionTrisha Mae KhoNo ratings yet
- At WP 3 Keys HospitalsDocument4 pagesAt WP 3 Keys HospitalsftuckingNo ratings yet
- Electronic Medical Records Research Paper TopicsDocument9 pagesElectronic Medical Records Research Paper Topicsc9rz4vrm100% (1)
- HCD WP 2012 HowaBusinessIntelligenceRoadmapSavesDocument7 pagesHCD WP 2012 HowaBusinessIntelligenceRoadmapSavesPatBickleyNo ratings yet
- Information System Research PaperDocument5 pagesInformation System Research Papervvomvqwgf100% (1)
- Literature Review On Hospital Management System ProjectDocument6 pagesLiterature Review On Hospital Management System Projectea46krj6No ratings yet
- 10 Necessary ToolsDocument8 pages10 Necessary ToolsNofeestickets AmericaNo ratings yet
- Health Information Systems Acquisition and ImplementationDocument10 pagesHealth Information Systems Acquisition and ImplementationKenson KipchumbaNo ratings yet
- HIMSS EHR Reporting Program RFI Comment LetterDocument9 pagesHIMSS EHR Reporting Program RFI Comment LetterSpit FireNo ratings yet
- 10 1 1 199Document10 pages10 1 1 199Pavel TudorNo ratings yet
- Chapter 2 Dental ClinicDocument5 pagesChapter 2 Dental ClinicJunard Dominguez100% (1)
- Health Software Here 178Document23 pagesHealth Software Here 178Morgan OkothNo ratings yet
- Each Section of The Format Has Been Mentioned in A Separate PageDocument22 pagesEach Section of The Format Has Been Mentioned in A Separate PageSurbhi PalNo ratings yet
- Case Innova 2022Document17 pagesCase Innova 2022Aashay JainNo ratings yet
- Literature Review On Accounting Information SystemDocument8 pagesLiterature Review On Accounting Information SystemafdtzwlzdNo ratings yet
- Design and Implementation of Financial and Budget Planning Expert SystemDocument53 pagesDesign and Implementation of Financial and Budget Planning Expert SystemMajestyNo ratings yet
- Business Proposal FinalDocument19 pagesBusiness Proposal Finalapi-408489180No ratings yet
- Research Paper On Hospital Management SystemDocument8 pagesResearch Paper On Hospital Management Systemafmcdeafl100% (1)
- Case Study Setting in SDLCDocument6 pagesCase Study Setting in SDLCMaria Cleofe MangaoangNo ratings yet
- ZEN Automation of Healthcare Product (1) .Docx - ERANNA - UPDATEDDocument7 pagesZEN Automation of Healthcare Product (1) .Docx - ERANNA - UPDATEDShrigouri JumnalkarNo ratings yet
- Health Care Example - Adopting Agile Principles in Health CareDocument13 pagesHealth Care Example - Adopting Agile Principles in Health CareAlexsandro LechnerNo ratings yet
- Healthcare Information System Fortis Hospital Case StudyDocument4 pagesHealthcare Information System Fortis Hospital Case StudySateesh MoreNo ratings yet
- Recommendations Focus Criteria On Value and Achievability - Meaningful Use MeasuresDocument5 pagesRecommendations Focus Criteria On Value and Achievability - Meaningful Use MeasuresDavid HarlowNo ratings yet
- Template For FormattingDocument9 pagesTemplate For FormattingKade ArtiagaNo ratings yet
- Ehr Thesis StatementDocument7 pagesEhr Thesis Statementlizhernandezalbuquerque100% (2)
- ch1 PDFDocument18 pagesch1 PDFCliffordBeniNo ratings yet
- Olu Sanye Leg Be Dean Do Guns EyeDocument6 pagesOlu Sanye Leg Be Dean Do Guns EyeItz HarlartiseyNo ratings yet
- Final PaperDocument4 pagesFinal PaperEricka SimmonsNo ratings yet
- WP Six Steps To Lead IT Transformation 2014Document4 pagesWP Six Steps To Lead IT Transformation 2014burnslNo ratings yet
- Hospital Information System Research PaperDocument9 pagesHospital Information System Research PaperaflbojhoaNo ratings yet
- Health Information System Design, Implementation & EvaluationDocument7 pagesHealth Information System Design, Implementation & EvaluationHazman Aziz100% (2)
- White PaperDocument8 pagesWhite Paperapi-533780039No ratings yet
- Effect of Management Information SystemDocument23 pagesEffect of Management Information Systemsujata bhartiNo ratings yet
- Steven Mitchell Report 8 Lis 4776 Advanced Health InformaticsDocument7 pagesSteven Mitchell Report 8 Lis 4776 Advanced Health InformaticsSteven Napoleon MitchellNo ratings yet
- A Practical Guide To Meaningful Use: Federal Register, 75 (144), Wednesday, July 28, 2010, Pp. 44589-44654Document6 pagesA Practical Guide To Meaningful Use: Federal Register, 75 (144), Wednesday, July 28, 2010, Pp. 44589-44654dnice408No ratings yet
- Literature Review On Hospital Management SystemDocument7 pagesLiterature Review On Hospital Management SystemafdtsxuepNo ratings yet
- 1 PBDocument6 pages1 PBNdamze Ndamale NicholasNo ratings yet
- Healthcare Process Management GuideDocument5 pagesHealthcare Process Management Guideapi-388173202No ratings yet
- Service Plan Brief For Wellness Program - EditedDocument10 pagesService Plan Brief For Wellness Program - EditedMaina PeterNo ratings yet
- Literature Review On Online Medical Billing SystemDocument6 pagesLiterature Review On Online Medical Billing Systemc5sd1aqjNo ratings yet
- Running Head: FINAL EXAMDocument7 pagesRunning Head: FINAL EXAMapi-307874398No ratings yet
- HTM 680 Practice FusionDocument9 pagesHTM 680 Practice Fusionapi-307874398No ratings yet
- Ashleyelisawinansresume032116web Docx 1Document1 pageAshleyelisawinansresume032116web Docx 1api-307874398No ratings yet
- Running Header: Ethical Issues in Health It 1Document6 pagesRunning Header: Ethical Issues in Health It 1api-307874398No ratings yet
- Hca 663 Group Presentation 1Document14 pagesHca 663 Group Presentation 1api-307874398No ratings yet
- Hca 622 LeadershipDocument7 pagesHca 622 Leadershipapi-307874398No ratings yet
- 1 Data Analysis: Smoking and DeathDocument9 pages1 Data Analysis: Smoking and Deathapi-307874398No ratings yet
- Mercyhospitalpatientportalproposal1 1Document36 pagesMercyhospitalpatientportalproposal1 1api-307874398No ratings yet
- Running Header: Iom: Quality in Health Care 1Document20 pagesRunning Header: Iom: Quality in Health Care 1api-307874398No ratings yet
- HTM 660 Final PresentationDocument27 pagesHTM 660 Final Presentationapi-307874398No ratings yet
- Htm660casestudy17 1Document6 pagesHtm660casestudy17 1api-307874398No ratings yet
- HTM 680 Lakeland HealthcareDocument11 pagesHTM 680 Lakeland Healthcareapi-307874398No ratings yet
- HTM 680 OpendoorfamilymedicalcentercasestudyDocument6 pagesHTM 680 Opendoorfamilymedicalcentercasestudyapi-307874398No ratings yet
- Hca 600 KingvsburwellDocument5 pagesHca 600 Kingvsburwellapi-307874398No ratings yet
- GT Protection Type TestDocument24 pagesGT Protection Type Testashwani2101100% (1)
- Annul. Press. Bleed Off Proced.Document3 pagesAnnul. Press. Bleed Off Proced.eng7mohamed7hashimNo ratings yet
- IELTS PART 1 (Autoguardado)Document8 pagesIELTS PART 1 (Autoguardado)CARLOS CAICEDONo ratings yet
- Services Marketing Chapter-9Document15 pagesServices Marketing Chapter-9Orko AhmedNo ratings yet
- ConclusionDocument1 pageConclusionSAVITHRINo ratings yet
- Tesco AnalysisDocument12 pagesTesco Analysisdanny_wch7990No ratings yet
- Sub Engineer Test Model PaperDocument8 pagesSub Engineer Test Model PaperZeeshan AhmadNo ratings yet
- Tutorial 6 - SolutionsDocument8 pagesTutorial 6 - SolutionsNguyễn Phương ThảoNo ratings yet
- Ratio & Proportion - Important Maths For BankDocument9 pagesRatio & Proportion - Important Maths For BankXpired ZoneNo ratings yet
- Automotive Transmission-ShaftDocument7 pagesAutomotive Transmission-Shaftfileuse.fNo ratings yet
- Business Plan ForbesDocument4 pagesBusiness Plan ForbesMoiz AhmedNo ratings yet
- Colonial Comparison Powerpoint TemplateDocument10 pagesColonial Comparison Powerpoint TemplateGraham NicholsNo ratings yet
- Ideal Home - Complete Guide To Christmas 2016 PDFDocument148 pagesIdeal Home - Complete Guide To Christmas 2016 PDFpetru555100% (2)
- Hello World in FortranDocument43 pagesHello World in Fortranhussein alsaedeNo ratings yet
- Harvard Algorithms cs124 NotesDocument6 pagesHarvard Algorithms cs124 NotesYamini DasguptaNo ratings yet
- Digital Transducers: Group 3Document76 pagesDigital Transducers: Group 3Jasmine RaiNo ratings yet
- 8959C4F253F33BB139F788350D0E6D0035455AB9A56BFAC9F3070E66F25AC10EDocument20 pages8959C4F253F33BB139F788350D0E6D0035455AB9A56BFAC9F3070E66F25AC10Edroping cowsNo ratings yet
- DATACOM Multiple Choice Question 6Document1 pageDATACOM Multiple Choice Question 6girijamohapatraNo ratings yet
- Literature Review On School AdministrationDocument6 pagesLiterature Review On School Administrationea7sfn0f100% (1)
- Prismatic Oil Level GaugeDocument2 pagesPrismatic Oil Level GaugevipulpanchotiyaNo ratings yet
- Combinational CircuitsDocument18 pagesCombinational CircuitsSalil TimalsinaNo ratings yet
- International Journal of Biopharmaceutics: Formulation and Evaluation of Ibuprofen Loaded Maltodextrin Based ProniosomeDocument7 pagesInternational Journal of Biopharmaceutics: Formulation and Evaluation of Ibuprofen Loaded Maltodextrin Based ProniosomeNeng NurtikaNo ratings yet
- Performance Appraisal at UFLEX Ltd.Document29 pagesPerformance Appraisal at UFLEX Ltd.Mohit MehraNo ratings yet
- Evolution of Highrise Buildings: Architectural Design - 7 SEMDocument41 pagesEvolution of Highrise Buildings: Architectural Design - 7 SEMVismithaNo ratings yet
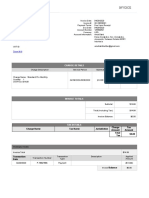
- InvoiceDocument2 pagesInvoiceamalNo ratings yet
- Easergy PS100 48VDC Power SupplyDocument2 pagesEasergy PS100 48VDC Power SupplyRichard SyNo ratings yet
- Job - Details - Grant Acquisition Management (GAM) Manager - 5219Document4 pagesJob - Details - Grant Acquisition Management (GAM) Manager - 5219Salman DigaleNo ratings yet
- Chapter - 1 NetworksDocument61 pagesChapter - 1 NetworksSummiya JangdaNo ratings yet