Professional Documents
Culture Documents
NCP Again - Liver Cirrhosis
Uploaded by
Kristine Mae Lee AceboOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP Again - Liver Cirrhosis
Uploaded by
Kristine Mae Lee AceboCopyright:
Available Formats
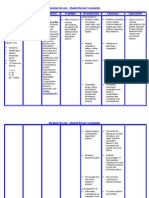
Nursing Care Plan
Assessment Subjective: Napansin ko na lumalaki ang tiyan ko as verbalized Objective: Pallor Weak in appearance Jaundice Abdominal distention noted Bipedal edema Irritability noted DOB with RR of 29 bpm Abdominal girth of 32
Diagnosis Fluid volume excess r/t compromised regulatory mechanism secondary to cirrhosis of the liver as manifested by pallor, weak in appearance, jaundice, abdominal distention, edema, irritability, DOB with RR of 29 and abdominal girth of 32
Planning After 6 hours of nursing interventions, patient will demonstrate stabilized fluid volume and decreased edema and abdominal girth.
Interventions Monitor vital sign Measure intake and output
Rationale Established baseline data Reflects circulating volume status, developing fluid shifts, and in response to therapy BP elevations are usually associated with fluid volume excess Indicative of pulmonary congestion/edema Reflects accumulation of fluid (ascites) Decreases sensation of thirst, especially when fluid intake is restricted Sodium may be restricted to minimize fluid retention in extravascular spaces. Fluid
Evaluation
After 6 hours of
nsg. interventions, the patient demonstrated stabilized fluid volume and decreased edema and abdominal girth. Goal met.
Monitor BP Assess respiratory status Monitor abdominal girth Provide occasional ice chips if NPO Restrict sodium and fluids as ordered
Administer medications as indicated: Diuretics
restriction may be necessary to prevent dilutional hyponatremia
Potassium
Assist with paracentesis procedure
Used with caution to control edema and ascites, block effect of aldosterone, and increase water excretion while sparing potassium Serum and cellular potassium are usually depleted because of liver disease Done to remove ascites fluid
Nursing Care Plan
Assessment Subjective: Wala akong ganang kumain as verbalized Objective: Weak in appearance Refusal to eat Irritability noted Poor muscle tone Jaundice noted Emaciated Abdominal distention noted Pallor noted
Diagnosis Imbalance nutrition: less than body requirements r/t loss of appetite secondary to ascites as evidenced by refusal to eat, weak in appearance, irritability, poor muscle tone, emaciated and abdominal distention
Planning After 5 hrs of nsg. Interventions, patients appetite will improve from 2 tbsp to at least 5 tbsp per meal.
Interventions Monitor vital signs Assist in oral hygiene before meals. Discuss eating habits including food preferences. Serve favorite foods that are not contraindicated. Prevent or minimize unpleasant odors during meal time. Serve foods that are attractive and palatable. Recommend small, frequent meals
Rationale For baseline data A clean mouth enhances appetite To appeal to client likes and dislikes To stimulate the appetite May have negative effect on appetite To stimulate the appetite Poor tolerance to larger meals may be due to increased intraabdominal pressure/ascites Aids in reducing gastric irritation & abdominal discomfort that may impair oral intake/digestion
Evaluation After 8 hours of nursing interventions, patients appetite improved from 2 tbsp to 5 tbsp per meal. Goal met.
Restrict intake of caffeine, gasproducing or spicy and excessively hot or cold foods
Provide assistance with activities as needed. Promote undisturbed rest periods, especially before meals Advise to consume nutritious foods
Conserving energy reduces metabolic demands on the liver and promotes cellular regeneration.
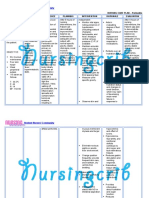
Nursing Care Plan
Assessment Subjective: Sumasakit ang tiyan ko as verbalized with a pain scale of 6 out of 10 where in: 0 - no pain 1 2 mild pain 3 4 moderate pain 5 6 severe pain 7 8 very severe pain 9 10 worst possible Objective: Facial grimace noted Irritability noted Restlessness noted Anxiety noted Fatigued Clenched fist Beaten look Agitation noted Pallor Grunting Guarding of body part (right hypochondriac)
Diagnosis Acute pain related to liver enlargement secondary to ascites as evidenced by facial grimace, irritability, restlessness, anxiety, fatigued, clenched fist, beaten look, agitation, pallor, grunting, guarding of body part and verbalization of pain with a pain scale of 6/10
Planning After 2 hours of nursing interventions, pain will be lessened with a scale of 1-10, from 6/10 to 1/10.
Interventions Monitor VS Perform pain assessment (COLDSPA) every time pain occurs
Rationale Pain alters VS To rule out development of complications by knowing alleviating and precipitating factors Pain is subjective & cant be assessed through observation alone Promotes relaxation and diverts attention from pain To prove nonpharmacological management To alleviate pain Noisy environment stimulates irritation
Evaluation After 2 hours of nursing interventions, patient was relieved from pain Goal met.
Encourage verbalization of feeling of pain Instruct use of relaxation exercise such as listening to music Provide comfort measures such as back rubbing & changing position Teach the patient relaxation techniques like deep breathing Provide quiet and calm environment
Nursing Care Plan
Assessment Subjective: Nahihirapan akong huminga as verbalized Objective: Dyspnea Tachypnea with RR of 30, irregular, shallow Weak in appearance Anxiety noted Irritability noted Restlessness noted Lethargic Pallor
Diagnosis Altered breathing pattern r/t decreased lung expansion secondary to intraabdominal fluid collection (ascites) as manifested by dyspnea, tachypnea with RR of 30, irregular and shallow, weak in appearance, anxiety, irritability, restlessness, lethargy and pallor
Planning After 6 hours of nursing interventions, patient will be relieved from dyspnea and breathing pattern will return to normal.
Interventions Monitor V/S Monitor respiratory rate, rhythm and depth
Rationale For baseline data Rapid shallow respirations/dyspn ea may be present because of hypoxia or fluid accumulation in the abdomen Indicates developing complications and increasing risk of infection Changes in mentation may reflect hypoxemia and respiratory failure Facilitates breathing by reducing pressure on the diaphragm Aids in lung expansion and mobilizing secretions May be necessary to treat/prevent
Evaluation After 6 hours of nsg. interventions, patient was relieved from dyspnea and breathing pattern returned to normal Goal met.
Auscultate breath sounds, noting crackles, wheezes and rhonchi Investigate changes in LOC Keep head of bed elevated. Position on sides Encourage frequent repositioning and deep-breathing exercises Provide supplemental O2 as indicated
hypoxia
Nursing Care Plan
Assessment
Diagnosis
Planning
Interventions
Rationale
Evaluation
Subjective: Nanghihina na ako, ayoko na mag-gagalaw as verbalized Objective: Pallor Body malaise noted Diaphoresis Inability to concentrate Inability to perform usual ADLs Weak in appearance Limited ROM Difficulty initiating movements
Activity intolerance r/t generalized body weakness secondary to progressive disease state as manifested by pallor, body malaise, diaphoresis, inability to concentrate, inability to perform usual ADLs, weak in appearance, limited ROM and difficulty initiating movements
After 8 hours of nursing interventions, patient will participate willingly in necessary activity, will learn how to conserve energy and verbalize relief from fatigue.
Evaluate pts current activity tolerance Adjust activity and reduce intensity of task that may cause undesired physiological changes Increase exercise and activity levels gradually Teach methods to conserve energy such as sitting than standing while dressing Demonstrate/Assis t the patient while doing ADL Give the patient information that provides evidence progress Encourage client to do whatever possible e.g. selfcare
Provide cooperative baseline To prevent over exertion
Enhances activity tolerance Helps minimize waste of energy
After 8 hours of nursing interventions, patient participated willingly in necessary activities, learned how to conserve energy and verbalized relief from fatigue Goal met
Protect patient from injury To sustain pts motivation Provides for sense of control and feeling of accomplishment
Nursing Care Plan
Assessment Subjective: Mawawala ba pa tong laki ng tiyan ko? as verbalized Objective: Anxiety noted Fear of rejection Irritability noted Restlessness noted Feeling of helplessness Negative feelings about body
Diagnosis Disturbed body image r/t altered physical appearance as evidenced by anxiety, fear, irritability, restlessness, feeling of helplessness and negative feelings about the body
Planning After 8 hours of nursing interventions, patient will verbalize understanding of changes and acceptance of self in the present situation.
Interventions Discuss situation/encourag e verbalization of fears and concerns. Explain relationship between nature of disease and symptoms. Support and encourage patient; provide care with a positive, friendly attitude
Rationale Patient is very sensitive to body changes and may also experience feelings of guilt when cause is related to alcohol (70%) or other drug use. Caregivers sometimes allow judgmental feelings to affect the care of patient and need to make every effort to help patient feel valued as a person.
Family members may feel guilty about patients condition and may be fearful of impending death. They need nonjudgmental emotional support and free access to patient. Participation in care
Evaluation After 8 hours of nursing interventions, patient verbalized understanding of changes and acceptance of self in the present situation. Goal met
Encourage family to verbalize feelings, visit freely/participate in care
helps them feel useful and promotes trust between staff, patient.
Nursing Care Plan
Assessment
Diagnosis
Planning
Interventions
Rationale
Evaluation
Subjective: Lagi akong nangangati at parang mahapdi balat ko as claimed Objective: Pruritus noted Dry skin Erythema noted Scaly skin
Risk for impaired skin integrity r/t altered circulation secondary to accumulation of bile salts as evidenced by pruritus, erythema, dry and scaly skin
After 7 hours of nursing interventions, patient will maintain skin integrity and identify individual risk factors and demonstrate behaviors/techniqu e to prevent skin breakdown.
Inspect skin surface/pressure points routinely. Gently massage bony prominences or areas of continued stress
Encourage/assist with repositioning on a regular schedule while in bed, chair and active passive ROM exercises as appropriate Keep linen dry and free of wrinkles Suggest clipping finger nails short
Edematous tissues are more prone to breakdown and to the formation of decubitus ulcers. Ascites may stretch the skin to the point of tearing in severe cirrhosis Repositioning reduces pressure on edematous tissues to improve circulation. Exercises enhance circulation and improve, maintain, joint mobility Moisture aggravates pruritus and increases risk of skin breakdown
Prevents client from inadvertently injuring the skin especially while sleeping
After 3 hours of nursing interventions, patient maintained skin integrity and identified individual risk factors and demonstrated behaviors/techniqu es to prevent skin breakdown. Goal met
Nursing Care Plan
Assessment Subjective: Nahiirapan akong umihi as verbalized Objective: Anxiety noted Irritability noted Restlessness noted Small, frequent voiding Facial grimace noted upon urination Excessive diaphoresis when trying to void Urgency
Diagnosis Impaired urinary elimination r/t bladder distention secondary to ascites as evidenced by anxiety, irritability, restlessness, small and frequent voiding, facial grimace upon urination, excessive diaphoresis when trying to void, and urgency
Planning After 8 hours of nursing interventions, patient will empty bladder regularly with decrease pain and difficulty.
Interventions Palpate bladder. Investigate reports of discomfort, fullness, inability to void
Rationale Perception of bladder fullness, distention of bladder above symphysis pubis indicates urinary retention Promotes relaxation urinary muscles and may facilitate voiding efforts
Evaluation After 8 hours of nursing interventions, patient voided regularly and without difficulty. Goal met
Provide routine voiding measures like privacy, normal positioning, running water in sink, pouring warm water over abdomen
Nursing Care Plan
Assessment Subjective: Anu kaya tong sakit ko, san ko nakuha to? as verbalized Objective: Restlessness noted Irritability noted Confused look Statement of misconception Development of preventable complications Frequent questions
Diagnosis Knowledge deficit regarding condition, prognosis, treatment and discharge needs r/t information misinterpretation as evidenced by restlessness, irritability, confused look, statement of misconception, development of preventable complications and frequent questions
Planning After 8 hours of nursing interventions, patient will verbalize understanding of disease process, prognosis, potential complications and identify necessary lifestyle changes and participate in care.
Interventions Review disease process/prognosis and future expectations Stress importance of avoiding alcohol. Give information about community services available to aid in alcohol rehabilitation if indicated. Emphasize the importance of good nutrition. Recommendavoida nce of highprotein/salty foods, onions, and strongcheeses. Provide written dietary instructions
Rationale Provides knowledge base from which patient can make informed choices Alcohol is the leading cause in the development of cirrhosis
Evaluation After 8 hours of nursing interventions, patient verbalized understanding of disease process, prognosis, potential complications and identified necessary lifestyle changes and participate in care. Goal met
Proper dietary maintenance and avoidance of foods highin sodium and protein aid in remission of symptoms andhelp prevent ammonia buildup and further liver damage.Written instructions are helpful for patient to refer to at home
Nursing Care Plan
Assessment Subjective: Hirap ako makatulog as claimed Objective: Sunken eyeballs Fatigue Mood alterations Agitated Body weakness noted Lethargic
Diagnosis Disturbed sleep pattern r/t changes in activity pattern secondary to psychologic stress as evidenced by sunken eyeballs, fatigue, mood alterations, agitation, body weakness, lethargy
Planning After 4 hours of nursing interventions, patient will establish adequate sleep pattern and report rested.
Interventions Evaluate level of stress
Rationale Increasing confusion, disorientation, and uncooperative behavior may interfere with attaining restful sleep
Decreases need to get up to go to bathroom during sleep Reduces sensory stimulation by blocking out other environmental sounds that could interfere with restful sleep
Evaluation After 4 hours of nursing interventions, patient established adequate sleep pattern and reported rested. Goal met
Advise to reduce fluid intake at night Provide soft music or white noise if available
You might also like
- NCP Liver CirrhosisDocument2 pagesNCP Liver Cirrhosismarlx5100% (3)
- NURSING CARE PLAN - Liver CirrhosisDocument2 pagesNURSING CARE PLAN - Liver Cirrhosisderic100% (27)
- NCP For Liver CirrhosisDocument25 pagesNCP For Liver CirrhosisWendy Escalante100% (1)
- Nursing Care Plan For Liver Cirrhosis NCPDocument14 pagesNursing Care Plan For Liver Cirrhosis NCPderic92% (12)
- NCP Liver CirrhosisDocument7 pagesNCP Liver CirrhosisIris Jimenez-BuanNo ratings yet
- Liver Cirrhosis NCP 1Document6 pagesLiver Cirrhosis NCP 1Paolo Rafael D EsguerraNo ratings yet
- Liver NCPDocument5 pagesLiver NCPMerrill HansNo ratings yet
- Nursing Care Plan TBIDocument5 pagesNursing Care Plan TBIChester Manalo87% (15)
- 8 Liver Cirrhosis Nursing Care PlansDocument4 pages8 Liver Cirrhosis Nursing Care PlansAngie MandeoyaNo ratings yet
- Liver Cirrhosis - NCPDocument18 pagesLiver Cirrhosis - NCPIshmael Solamillo83% (6)
- Case: Liver Cirrhosis Assessment:: Nursing InferenceDocument7 pagesCase: Liver Cirrhosis Assessment:: Nursing InferenceLovelyn GanirNo ratings yet
- Liver Cirrhosis Nursing Care PlansDocument17 pagesLiver Cirrhosis Nursing Care Plansmarsan12No ratings yet
- Renal Failure NCPDocument3 pagesRenal Failure NCPJet Ray-Ann GaringanNo ratings yet
- Nursing Care Plan-AscitesDocument10 pagesNursing Care Plan-AscitesKayki Louise75% (4)
- Nursing Care Plan For Myocardial InfarctionDocument7 pagesNursing Care Plan For Myocardial InfarctionjamieboyRN88% (8)
- 5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care PlansDocument3 pages5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care Plansjustin_sane40% (5)
- Subdural HematomaDocument4 pagesSubdural Hematomarodamel gundanNo ratings yet
- NCP-Esophageal Varices Pleural EffusionDocument6 pagesNCP-Esophageal Varices Pleural Effusiontinatin98933% (3)
- NURSING CARE PLAN - Lung CancerDocument3 pagesNURSING CARE PLAN - Lung Cancerderic80% (15)
- Nursing Diagnosis For Intestinal ObstructionDocument2 pagesNursing Diagnosis For Intestinal ObstructionYoga Mesi58% (19)
- NCP On Electrolyte ImbalanceDocument4 pagesNCP On Electrolyte Imbalancefreyah_bc67% (3)
- Case Scenario: Prostate CancerDocument5 pagesCase Scenario: Prostate Cancer24 PAULINO ALDRIN MUJARNo ratings yet
- NCP For Diabetic KetoacidosisDocument2 pagesNCP For Diabetic KetoacidosisLovely Cacapit100% (1)
- Nursing Care Plan For A Patient With Pleural EffusionDocument5 pagesNursing Care Plan For A Patient With Pleural Effusionmac042250% (4)
- Nursing Care Plan For "Hepatitis"Document12 pagesNursing Care Plan For "Hepatitis"jhonroks86% (14)
- NCP of Renal CalculiDocument3 pagesNCP of Renal Calculidextroid1289% (9)
- Anatomy and Physiology-Liver CirrhosisDocument2 pagesAnatomy and Physiology-Liver CirrhosisHilmi Ramos100% (3)
- NCP. FistulectomyDocument2 pagesNCP. Fistulectomymitchelley80% (10)
- Diarrhea NCPDocument2 pagesDiarrhea NCPNoriel FabrosNo ratings yet
- Nursing Care Plan For Peritonitis NCPDocument2 pagesNursing Care Plan For Peritonitis NCPderic86% (7)
- Nursing Care Plan - GastritisDocument4 pagesNursing Care Plan - Gastritisapi-371817467% (27)
- NCP For RS-HF (Cor PulmonaleDocument5 pagesNCP For RS-HF (Cor PulmonaleMika Saldaña100% (1)
- Nursing Care PlanDocument5 pagesNursing Care PlanAnju Luchmun100% (2)
- NCP Loss of AppetiteDocument5 pagesNCP Loss of AppetiteStenneli Gumban Trojillo50% (2)
- Nursing Care Plan Hemorrhagic StrokeDocument8 pagesNursing Care Plan Hemorrhagic StrokeJeffrey Dela Cruz50% (4)
- NURSING CARE PLAN For Myocardial InfarctionDocument16 pagesNURSING CARE PLAN For Myocardial InfarctionFreisanChenMandumotan100% (1)
- Case Study BPHDocument31 pagesCase Study BPHyhanne95% (84)
- NCP - Excess Fluid Volume (Aortic Stenosis)Document3 pagesNCP - Excess Fluid Volume (Aortic Stenosis)Daniel Vergara Arce100% (3)
- 2 Nanda Nursing Diagnosis and Interventions For LeukemiaDocument6 pages2 Nanda Nursing Diagnosis and Interventions For LeukemiaGeraldine Gallaron - Casipong67% (3)
- Nursing Care Plan For CHFDocument7 pagesNursing Care Plan For CHFRosemarie Carpio100% (5)
- CholecystitisDocument60 pagesCholecystitistammycristobalmd100% (15)
- Ineffective Renal Tissue PerfusionDocument2 pagesIneffective Renal Tissue PerfusionHendra Tanjung100% (4)
- NCP Gastric CancerDocument7 pagesNCP Gastric CancerAnonymous XvwKtnSrMR100% (4)
- Acute Renal FailureDocument59 pagesAcute Renal Failurepaul_v_44440% (1)
- CASE STUDY Intestinal ObstructionDocument68 pagesCASE STUDY Intestinal ObstructionMaria Paula Bungay91% (22)
- Subjective: "Napansin Ko Na Lumalaki Ang Tiyan Ko" As Verbalized by The Patient. ObjectiveDocument5 pagesSubjective: "Napansin Ko Na Lumalaki Ang Tiyan Ko" As Verbalized by The Patient. ObjectiveJobelle AcenaNo ratings yet
- Liver Cirrhosis NCPDocument3 pagesLiver Cirrhosis NCPSharmaine MadlaNo ratings yet
- Nursing Care PL WPS OfficeDocument3 pagesNursing Care PL WPS OfficeDhan IvanNo ratings yet
- Overview of The DiseaseDocument12 pagesOverview of The DiseasePresciousNo ratings yet
- Chronic Renal Failure Nursing Care PlanDocument6 pagesChronic Renal Failure Nursing Care PlanRuva Oscass JimmyNo ratings yet
- NCP - Activity Intolerance & Excess Fluid VolumeDocument2 pagesNCP - Activity Intolerance & Excess Fluid VolumeCindy MariscotesNo ratings yet
- NCPDocument3 pagesNCPranee diane0% (1)
- NCP 1Document5 pagesNCP 1Denisse Shazz Mae MaretNo ratings yet
- Congestive Cardiac FailureDocument22 pagesCongestive Cardiac FailureSampada GajbhiyeNo ratings yet
- Global City Innovative CollegeDocument3 pagesGlobal City Innovative CollegemadypadNo ratings yet
- Ncp-Liver CirrhosisDocument3 pagesNcp-Liver CirrhosisNorbelisa Tabo-ac CadungganNo ratings yet
- NCP Excess Fluid VolumeDocument4 pagesNCP Excess Fluid VolumeIngrid Nicolas100% (1)
- NCP With DsDocument11 pagesNCP With DsMissDyYournurseNo ratings yet
- NCP Liver CirDocument2 pagesNCP Liver CirBhabykhrishNo ratings yet
- Acute Renal Failure Nursing Care PlanDocument4 pagesAcute Renal Failure Nursing Care PlanKrisianne Mae Lorenzo Francisco80% (5)
- Nursing ManagementDocument6 pagesNursing ManagementkenNo ratings yet
- Meig'sDocument10 pagesMeig'skenNo ratings yet
- Kawasaki DiseaseDocument14 pagesKawasaki Diseaseken100% (2)
- Causes of Spontaneous Abortion 2Document23 pagesCauses of Spontaneous Abortion 2kenNo ratings yet
- High Risk PregnancyDocument35 pagesHigh Risk PregnancykenNo ratings yet
- Basic Nutrition 2009 RevisedDocument25 pagesBasic Nutrition 2009 Revisedken100% (3)
- Case Study of BronchitisDocument34 pagesCase Study of Bronchitisken83% (29)
- Gum PaintDocument3 pagesGum PaintAni GuptaNo ratings yet
- Article II Protection Rights of Children: Child Abuse, Exploitation, and DiscriminationDocument12 pagesArticle II Protection Rights of Children: Child Abuse, Exploitation, and DiscriminationMicky MoranteNo ratings yet
- 118 A Chapter 2.1 - RESPONSES TO ALTERED VENTILATORY FUNCTION (CARDIOMYOGRAPHY)Document8 pages118 A Chapter 2.1 - RESPONSES TO ALTERED VENTILATORY FUNCTION (CARDIOMYOGRAPHY)Joanna Taylan100% (1)
- Orientation L2F - April 6Document5 pagesOrientation L2F - April 6JD AguilarNo ratings yet
- Covid-19 Rat Common-List enDocument27 pagesCovid-19 Rat Common-List enNavneet ValechaNo ratings yet
- Rural Water SupplyDocument4 pagesRural Water SupplyDaaZy LauZahNo ratings yet
- Dental HygieneDocument3 pagesDental Hygieneapi-507354264No ratings yet
- Aneurysmal Bone CystDocument5 pagesAneurysmal Bone CystAustine OsaweNo ratings yet
- LIPASE Kinetic Method: BiolaboDocument2 pagesLIPASE Kinetic Method: Biolabowindy ajengNo ratings yet
- Psych History ScriptDocument8 pagesPsych History ScriptRyan Loyd MarquezNo ratings yet
- Post Traumatic Stress Disorder (PTSD)Document114 pagesPost Traumatic Stress Disorder (PTSD)Gugus EkaNo ratings yet
- Wound Dressing ChecklistDocument2 pagesWound Dressing ChecklistCARL ANGEL JAOCHICONo ratings yet
- Association of Streptococcus Mutans Collagen Binding GenesDocument9 pagesAssociation of Streptococcus Mutans Collagen Binding GenesSITI AZKIA WAHIDAH RAHMAH ZEINNo ratings yet
- Vestibular Neuritis HandoutDocument3 pagesVestibular Neuritis HandoutPrisilia QurratuAiniNo ratings yet
- BSCMLT Syllabus FinalDocument56 pagesBSCMLT Syllabus FinalRajkishor YadavNo ratings yet
- Peptic Ulcer DiseaseDocument75 pagesPeptic Ulcer DiseaseSarah Gaile Tio Inac100% (4)
- Apraxia ScreeningDocument9 pagesApraxia Screeningceci MOLARONo ratings yet
- Occupational Problems and Barriers Reported by Individuals With ObesityDocument10 pagesOccupational Problems and Barriers Reported by Individuals With ObesityGraciela SeveriniNo ratings yet
- Lab Trematodea 3Document9 pagesLab Trematodea 3mustofa13basketNo ratings yet
- Casti2017 PDFDocument186 pagesCasti2017 PDFAnson JohnNo ratings yet
- Dam-It, It's Easy: Handbook of Basic Dental Dam ProceduresDocument32 pagesDam-It, It's Easy: Handbook of Basic Dental Dam ProceduresNonoNo ratings yet
- The Relationship Between Social Support and Psychological Problems AmongDocument8 pagesThe Relationship Between Social Support and Psychological Problems Amongltomic_1No ratings yet
- Malaria and Some Polyomaviruses (Sv40, BK, JC, and Merkel Cell Viruses)Document365 pagesMalaria and Some Polyomaviruses (Sv40, BK, JC, and Merkel Cell Viruses)zahidNo ratings yet
- Development of The ToothDocument22 pagesDevelopment of The ToothJoyce LimNo ratings yet
- Competency Assessment Tier1-Completed-2021Document20 pagesCompetency Assessment Tier1-Completed-2021api-439027462No ratings yet
- Malaria Treatment TableDocument9 pagesMalaria Treatment Tableاحمد عرفاتNo ratings yet
- RH Blood Group SystemDocument61 pagesRH Blood Group SystemValdez Francis ZaccheauNo ratings yet
- Acid WashDocument20 pagesAcid WashAhmedJumanNo ratings yet
- 10.neurological Assessment Cont...Document33 pages10.neurological Assessment Cont...Chenii RoyNo ratings yet
- Cancer 1-S2.0-S2468125323001462-MainDocument16 pagesCancer 1-S2.0-S2468125323001462-MainBîkes NâçarNo ratings yet