Professional Documents
Culture Documents
Case Scenario: Prostate Cancer
Uploaded by
24 PAULINO ALDRIN MUJAROriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case Scenario: Prostate Cancer
Uploaded by
24 PAULINO ALDRIN MUJARCopyright:
Available Formats
ALDRIN M.
PAULINO BSN 3A
Case Scenario: Prostate Cancer
Mr. Delgado is a 64-year old Caucasian male who comes into the clinic of his family physician with complaints of back pain, blood in the semen
during intercourse and weakness and numbness in his legs and feet for 2 months. His past medical history is notable only for hypertension and
gallstones. The examination reveals a 1 cm hard nodule palpated on the right side of his prostate. His PSA was checked 2 months ago and was
found to be 4.6ng/ml. Because of the presence of palpable nodule, he was referred to a urologist for prostate needle biopsy to rule out prostate
cancer. Mr. Degado looks horrified and afraid about the explanation given by his physician. The physician explains the procedure and reassures
Mr. Delgado about the procedure, he agreed to undergo the procedure. Mr. Delgado tells the doctor that he cannot have prostate cancer
because he feels just “fine” and look great. Mr. Delgado meets the urologist who repeats the prostate examination and concurs that there is a
1.0 cm nodule contained within the right side of his prostate. He recommends that he undergo a transrectal ultrasound (TRUS) guided prostate
needle biopsy to determine if the nodule contains prostate cancer. Three days later, the prostate needle biopsy is performed. The pathology
results show that he has Gleason 3+3=6 prostate cancer in 5 of the 12 biopsy cores with all the positive cores on the right side of the prostate.
The urologist explains to Mr. Delgado that (1) his relatively low PSA of 4.6ng/dl, (2) his small localized nodule on prostate exam, and (3) the low
volume Gleason 6 cancer on the biopsies together strongly suggest that his prostate cancer has not spread and is still confined to the prostate.
Radiation therapy (external beam radiotherapy or brachytherapy), radical prostatectomy, and active surveillance are all the options given to Mr.
Delgado. Mr. Delgado decides to undergo radical prostatectomy and radiation therapy for 12 cycles. The operation and radiation therapy went
well, and Mr. Delgado has an uneventful recovery. He is pleased to learn that the pathology report indicates that all of cancer was removed. His
PSA level is checked 6 weeks after the surgery and is undetectable, consistent with complete excision of the prostate and the tumor. Mr.
Delgado prescribe dutasteride (Avodart) as his maintenance drug and was given Sipuleucel-T (Provenge) vaccine.
NCP: Focus on post radical prostatectomy.
ALDRIN M. PAULINO BSN 3A
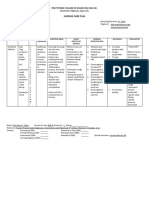
CUES NURSING SCIENTIFIC PLANNING IMPLEMENTATIO SCIENTIFIC EVALUATION
DIAGNOSIS EXPLANATION N RATIONALE
Subjective: Risk for Deficient Surgery may be Short term: Monitor Input & Indicator of fluid GOAL MET
fluid volume r/t done through After 1 hour of Output balance and
“Felt relief and Vascular nature several small or nursing replacement Short term:
contented” as of surgical area large incisions in intervention, the needs. With After 1 hour of
the abdomen or
stated by the patient will be bladder nursing
behind the scrotum
patient able to maintain irrigations, intervention, the
adequate fluid monitoring is patient was able
“Felt thirsty” as May remove and volume essential for to maintain
stated by the check the lymph estimating blood adequate fluid
patient nodes near the Long term: loss and volume
prostate After 24 hours of accurately
nursing assessing urine Long term:
Objective: intervention, the output. After 24 hours of
Prostate, the
patient will be nursing
seminal vesicles,
Muscle weakness able to maintain Monitor vital signs, Dehydration or intervention, the
and a portion of
urethra will then be adequate fluid noting increased hypovolemia patient was able
Dizziness removed volume as pulse and requires prompt to maintain
evidenced by respiration, intervention to adequate fluid
Dry mouth, dry good skin turgor decreased BP, prevent volume as
skin Nerve-sparing and balance diaphoresis, pallor, impending shock evidenced by
methods may be intake and output delayed capillary good skin turgor
Low urine output used to try to refill, and dry and balance
preserve erectile mucous intake and output
function
membranes.
After surgery, Investigate May reflect
catheter will be restlessness, decreased
placed to drain confusion, changes cerebral
urine from bladder. in behavior perfusion
Urine will flow (hypovolemia) or
through the indicate cerebral
catheter into a edema from
sterile bag
ALDRIN M. PAULINO BSN 3A
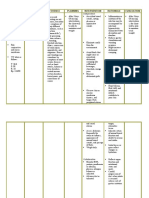
excessive solution
absorbed into the
venous sinusoids
during TUR
procedure (TURP
syndrome)
Encourage fluid Flushes kidneys
intake to 3000 and/or bladder of
mL/day unless bacteria and
contraindicated debris (clots).
Note: Water
intoxication or
fluid overload
may occur if not
monitored closely
Movement or
Anchor catheter, pulling of
avoid excessive catheter may
manipulation cause bleeding or
clot formation
and plugging of
the catheter, with
bladder
distension
Observe catheter Bleeding is not
drainage, noting unusual during
excessive or first 24 hr for all
continued but the perineal
bleeding approach
Evaluate color, Usually indicates
ALDRIN M. PAULINO BSN 3A
consistency of arterial bleeding,
urine clotting, or
irritation that
requires
aggressive
therapy
Monitor To evaluate blood
laboratory studies losses or
as indicated replacement
needs
Administer IV May need
therapy or blood additional fluids,
products as if oral intake
indicated. inadequate, or
blood products, if
losses are
excessive
Maintain traction Traction on the
on indwelling 30-mL balloon
catheter; tape positioned in the
catheter to inner prostatic urethral
thigh fossa creates
pressure on the
arterial supply of
the prostatic
capsule to help
prevent and
control bleeding
ALDRIN M. PAULINO BSN 3A
Release traction Prolonged
within 4–5 hr. traction may
Document period cause permanent
of application and trauma or
release of traction, problems with
if used urinary control
Administer stool Prevention of
softeners, laxatives constipation
as prescribed and/or straining
for stool reduces
risk of rectal-
perineal bleeding
You might also like
- Cancer Nursing Care Plan (NCP) - Risk For InfectionDocument2 pagesCancer Nursing Care Plan (NCP) - Risk For InfectionAngie MandeoyaNo ratings yet
- NURSING-CARE-PLAN-Lung-Cancerxxx 1Document3 pagesNURSING-CARE-PLAN-Lung-Cancerxxx 1Caroline ChaNo ratings yet
- NCP Modified Radical MastectomyDocument5 pagesNCP Modified Radical MastectomyIvan Jules P. PALMARESNo ratings yet
- NCPDocument2 pagesNCPsphinx809100% (2)
- NCPDocument2 pagesNCPJhel NabosNo ratings yet
- Health Teaching PlanDocument7 pagesHealth Teaching PlanJack Bangcoyo100% (1)
- Constipation LeukemiaDocument1 pageConstipation LeukemiamawelNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanKath RubioNo ratings yet
- Drug StudyDocument8 pagesDrug StudyzenNo ratings yet
- NCP LymphomaDocument3 pagesNCP LymphomaJohn Emmanuel Tatad TudNo ratings yet
- Comprehensive Nursing Care PlanDocument3 pagesComprehensive Nursing Care PlanJaylord VerazonNo ratings yet
- Nursing Care Plan (NCP) For A Patient With Acute Renal FailureDocument3 pagesNursing Care Plan (NCP) For A Patient With Acute Renal FailureKian HerreraNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanAldrein GonzalesNo ratings yet
- Nursing Care Plan For Breast Cancer NCP PDFDocument2 pagesNursing Care Plan For Breast Cancer NCP PDFMaina BarmanNo ratings yet
- Ovarian Cancer NCPDocument7 pagesOvarian Cancer NCPAsterlyn Coniendo100% (1)
- Risk For Acute ConfusionDocument2 pagesRisk For Acute ConfusionChar PereaNo ratings yet
- Prostate Cancer NCPDocument1 pageProstate Cancer NCPKathleen Dimacali0% (1)
- NCP LymphedemaDocument1 pageNCP Lymphedemayasira50% (2)
- Goboy - Risk For Infection NCPDocument3 pagesGoboy - Risk For Infection NCPLouise GermaineNo ratings yet
- NCP PryllDocument6 pagesNCP PryllpjcolitaNo ratings yet
- Management For OsteosarcomaDocument2 pagesManagement For OsteosarcomakyawNo ratings yet
- Nursing Care PlanDocument5 pagesNursing Care PlanJohn Paul Delos Santos100% (1)
- NCP For ConcussionDocument3 pagesNCP For Concussiontamtam_antonio100% (1)
- Thyroidectomy NCPDocument1 pageThyroidectomy NCPkzbreakerrNo ratings yet
- Vii. Nursing Care Plan: Secretions in The AirwaysDocument5 pagesVii. Nursing Care Plan: Secretions in The AirwaysJai - Ho100% (2)
- Chemotherapy Care PlanDocument5 pagesChemotherapy Care PlanAaLona Robinson50% (2)
- Assessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveDocument3 pagesAssessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveMaverick Lim100% (1)
- Nursing Care PlanDocument10 pagesNursing Care PlanMalou SanNo ratings yet
- NCP CvaDocument3 pagesNCP CvaJey PangilinanNo ratings yet
- Or Write Up 52611Document14 pagesOr Write Up 52611babydumplingsNo ratings yet
- Pathophysiology of Colon Cancer 1Document3 pagesPathophysiology of Colon Cancer 1Katherine Clarisse Carvajal Lavarias100% (1)
- NCP SviDocument4 pagesNCP SviEjie Boy IsagaNo ratings yet
- Assessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationDocument10 pagesAssessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationJobelle Acena100% (2)
- Ii. NCP: Black, Et - Al. (2005) .Me Dical Surgical Nursing. 7 Edition - Elsevie R Pte LTD.P 927Document4 pagesIi. NCP: Black, Et - Al. (2005) .Me Dical Surgical Nursing. 7 Edition - Elsevie R Pte LTD.P 927Lecery Sophia Wong75% (4)
- Discharge PlanDocument2 pagesDischarge PlanRoxanne_Buenaf_5285No ratings yet
- Nursing Diagnosis of Prostate CancerDocument3 pagesNursing Diagnosis of Prostate CancerSyafiqAzizi100% (1)
- Self Care DeficitDocument4 pagesSelf Care DeficitEllaine RamirezNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanInah Arcellana100% (2)
- Aminogen Drug StudyDocument2 pagesAminogen Drug Studymilesmin100% (1)
- Why Join PNADocument2 pagesWhy Join PNADarren CariñoNo ratings yet
- Discharge PlanDocument1 pageDischarge PlanBernalene SyNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationAbdallah AlasalNo ratings yet
- NCP Skin IntegrityDocument3 pagesNCP Skin IntegrityAlfie Ayro50% (2)
- NCP MastectomyDocument1 pageNCP MastectomyFaye Dianne Damian-BuenafeNo ratings yet
- NCP - Pulmonary TuberculosisDocument6 pagesNCP - Pulmonary TuberculosisastrijuNo ratings yet
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationDocument1 pageNovilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationCharina AubreyNo ratings yet
- NCP 2Document2 pagesNCP 2Neil Abraham Mendoza Lalap100% (2)
- NCPDocument2 pagesNCPjoyce_albertoNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanSharmaine Grace Florig100% (2)
- Nursing DX: Acute Pain Related To Surgical Manipulation (Laminectomy) As Manifested by Reports of Pain On The Lumbar Area Rated As 7/10Document1 pageNursing DX: Acute Pain Related To Surgical Manipulation (Laminectomy) As Manifested by Reports of Pain On The Lumbar Area Rated As 7/10YESSAMIN GUADIZ100% (2)
- Nursing Care Plan: CancerDocument6 pagesNursing Care Plan: Cancerneuronurse71% (7)
- Discharge PlanningDocument2 pagesDischarge PlanningSasa QuinaNo ratings yet
- NCP LymphomaDocument3 pagesNCP Lymphomamahmoud fuqahaNo ratings yet
- BSN 3e Duropan Ncp-Knowledge DeficitDocument12 pagesBSN 3e Duropan Ncp-Knowledge DeficitJane DuropanNo ratings yet
- Case Scenario 1: Benign Prostatic Hyperplasia: Aldrin M. Paulino BSN 3ADocument4 pagesCase Scenario 1: Benign Prostatic Hyperplasia: Aldrin M. Paulino BSN 3A24 PAULINO ALDRIN MUJARNo ratings yet
- Benign Prostatic Hyperplasia (NCP)Document4 pagesBenign Prostatic Hyperplasia (NCP)24 PAULINO ALDRIN MUJARNo ratings yet
- Final Nursing Care PlanDocument7 pagesFinal Nursing Care PlanKatherine BellezaNo ratings yet
- Nursing Care Plan: RationaleDocument5 pagesNursing Care Plan: Rationalerona-chanNo ratings yet
- Impaired Urinary EliminationDocument2 pagesImpaired Urinary EliminationSiafei RabeNo ratings yet
- NCP Post PartumDocument2 pagesNCP Post PartumsteffiNo ratings yet
- ORTHODocument3 pagesORTHO24 PAULINO ALDRIN MUJARNo ratings yet
- M2L1: Tracing Rizal's Historical Roots - While Task 1Document1 pageM2L1: Tracing Rizal's Historical Roots - While Task 124 PAULINO ALDRIN MUJARNo ratings yet
- M3 Post Task: Critical ThinkingDocument1 pageM3 Post Task: Critical Thinking24 PAULINO ALDRIN MUJARNo ratings yet
- Case Scenario 1: Benign Prostatic Hyperplasia: Aldrin M. Paulino BSN 3ADocument4 pagesCase Scenario 1: Benign Prostatic Hyperplasia: Aldrin M. Paulino BSN 3A24 PAULINO ALDRIN MUJARNo ratings yet
- Nursing Care Plan Cues Nursing Diagnosis Scientific Explanation Planning Implementation Scientific Rationale Evaluation Subjective CuesDocument4 pagesNursing Care Plan Cues Nursing Diagnosis Scientific Explanation Planning Implementation Scientific Rationale Evaluation Subjective Cues24 PAULINO ALDRIN MUJARNo ratings yet
- Allergic Rhinitis (NCP)Document3 pagesAllergic Rhinitis (NCP)24 PAULINO ALDRIN MUJAR50% (2)
- Deep Vein Thrombosis (NCP)Document4 pagesDeep Vein Thrombosis (NCP)24 PAULINO ALDRIN MUJAR0% (1)
- Assignment 6 Cardiovascular Agent Study QuestionsDocument1 pageAssignment 6 Cardiovascular Agent Study Questions24 PAULINO ALDRIN MUJARNo ratings yet
- Benign Prostatic Hyperplasia (NCP)Document4 pagesBenign Prostatic Hyperplasia (NCP)24 PAULINO ALDRIN MUJARNo ratings yet
- Case Study On Prostate CancerDocument16 pagesCase Study On Prostate Cancerferdz02100% (5)
- Benign Prostatic Hyperplasia BPH Transurethral Resection of The Prostate TurpDocument8 pagesBenign Prostatic Hyperplasia BPH Transurethral Resection of The Prostate TurpayamNo ratings yet
- The 14th Uro-Oncology Program at GlanceDocument2 pagesThe 14th Uro-Oncology Program at GlanceApitiya PaskariniNo ratings yet
- Surgery LMRP 2019Document65 pagesSurgery LMRP 2019skNo ratings yet
- Care of The Patient With Renal and Urinary Disorders - HandoutDocument52 pagesCare of The Patient With Renal and Urinary Disorders - HandoutAaron Ramirez LuNo ratings yet
- ProstateDocument42 pagesProstateMegawati Abubakar100% (1)
- TouijerDocument7 pagesTouijerVinko GrubišićNo ratings yet
- Surgical Audit Peer ReviewDocument46 pagesSurgical Audit Peer ReviewHarish BorraNo ratings yet
- Anaesthesia For Major Urological SurgeryDocument23 pagesAnaesthesia For Major Urological SurgeryDianita P Ñáñez VaronaNo ratings yet
- Medical Transcription WorkbookDocument30 pagesMedical Transcription Workbookpbowen22333% (3)
- Suprapubic ProstatectomyDocument12 pagesSuprapubic ProstatectomySaumitra JoshiNo ratings yet
- Download textbook Complications Of Urologic Surgery Prevention And Management 5Th Edition Samir S Taneja ebook all chapter pdfDocument53 pagesDownload textbook Complications Of Urologic Surgery Prevention And Management 5Th Edition Samir S Taneja ebook all chapter pdfchristina.young492100% (3)
- Urology Complete Qbank PDFDocument58 pagesUrology Complete Qbank PDFPanda Panda100% (1)
- Canine Prostatic Diseases: Reproduction and Periparturient CareDocument13 pagesCanine Prostatic Diseases: Reproduction and Periparturient CareSatria Adi MarhendraNo ratings yet
- Cghs RatesDocument25 pagesCghs RatesKi MuNo ratings yet
- ProstatectomyDocument9 pagesProstatectomymardsz100% (1)
- Iraqi BOARDDocument14 pagesIraqi BOARDNasser AlbaddaiNo ratings yet
- Prostate CancerDocument26 pagesProstate Cancerkhadzx100% (2)
- Actas Urológicas Españolas: Robotic Surgery: History and Teaching ImpactDocument6 pagesActas Urológicas Españolas: Robotic Surgery: History and Teaching ImpactMohammed Wazeem NNo ratings yet
- Med Surg (Oncology)Document169 pagesMed Surg (Oncology)DardarConstantinoNo ratings yet
- ASSESSMENT-OF-THE-CYTOTOXICITY-EXHIBITED-BY-ACTIVE-COMPONENTS-PRESENT-IN-CRUDE-EXTRACTS-TAKEN-FROM-THE-DIFFERENT-PARTS-OF-COLOCASIA-ESCULENTA-(CORM,STEM,LEAF)-AGAINST-PROSTATE-CANCER_OBRERO, NC, REYES, RJ, SESPENE JCDocument26 pagesASSESSMENT-OF-THE-CYTOTOXICITY-EXHIBITED-BY-ACTIVE-COMPONENTS-PRESENT-IN-CRUDE-EXTRACTS-TAKEN-FROM-THE-DIFFERENT-PARTS-OF-COLOCASIA-ESCULENTA-(CORM,STEM,LEAF)-AGAINST-PROSTATE-CANCER_OBRERO, NC, REYES, RJ, SESPENE JCellaNo ratings yet
- Ebook Hinmans Atlas of Urologic Surgery PDF Full Chapter PDFDocument67 pagesEbook Hinmans Atlas of Urologic Surgery PDF Full Chapter PDFwayne.edwardson742100% (27)
- Particular Cancer Power PointDocument101 pagesParticular Cancer Power PointKoRnflakesNo ratings yet
- Care of Clients With Problems of The Male Reproductive SystemDocument18 pagesCare of Clients With Problems of The Male Reproductive SystemwakswafuNo ratings yet
- A Century of Prostatic SurgeryDocument7 pagesA Century of Prostatic SurgeryLjubomirErdoglijaNo ratings yet
- Mechanisms, Mitigation, and Management of Urinary Toxicity From Prostate RadiotherapyDocument10 pagesMechanisms, Mitigation, and Management of Urinary Toxicity From Prostate RadiotherapyZuriNo ratings yet
- EAU EANM ESTRO ESUR SIOG Guidelines On Prostate Cancer 2020v4 PDFDocument182 pagesEAU EANM ESTRO ESUR SIOG Guidelines On Prostate Cancer 2020v4 PDFFlorencia GuerraNo ratings yet
- Latihan Soal MCQ UrologiDocument43 pagesLatihan Soal MCQ Urologidytul100% (1)
- TUVRPDocument56 pagesTUVRPGolovastik NujabesNo ratings yet
- Niyats Proposal DraftDocument35 pagesNiyats Proposal DraftrobelNo ratings yet