Professional Documents
Culture Documents
Basic Principles of Enteral Feeding: Hale Akbaylar
Uploaded by
Abdul NazirOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Basic Principles of Enteral Feeding: Hale Akbaylar
Uploaded by
Abdul NazirCopyright:
Available Formats
Turk J Gastroenterol 2002; 13 (4): 186-191
Basic principles of enteral feeding
Hale AKBAYLAR
Dokuz Eyll University School of Medicine, Department of Internal Medicine, Izmir
INTRODUCTION The maintenance of appropriate nutrition in patients with acute and chronic illness is known to be a fundemental part of patient care. Some patients require specialized nutrition support. A meta analysis of 30 randomized controlled trials found that patients receiving nutritional support showed improvements in body weight and anthropometrical measurements and a reduced risk of death compared to control group cases. The indications for nutritional support are as follows: 1. Preexisting nutritional deprivation: This is probably the most common indication for nutritional support. Malnutrition is common in clinical practice and such patients have impaired physiological funchoning high risk of complications and infections and poorer clinical outcomes. Many patients are also subject to iatrogenic starvation. 2. Inadequate oral energy intake: This results in breakdown of glycogen stores gluconeogenesis, peripheral lypolysis and amino acid oxidation from muscle stores. Although the optimal time for commencment of nutritional support is controversial it seems reasonable to start in patients with a history of inadequate oral intake for 7-14 days or in those patients in whom inadequate oral intake is expected over a 7- 14 day period. 3. Significant multiorgan system disease: This is the third most common indication for nutritional support. Renal, hepatic, cardiac, pulmonary, gastrointestinal or hematologic diseases can preclude adequate intake of oral nutrition and cause hypercatabolism.
Both enteral and parenteral routes can be used for nutritional support but there are insufficient randomised controlled trials comparing these routes in various disease states. Enteral nutrition (EN) has a number of advantages such as reduced cost, better maintenance of gut integrity, reduced infection rates and decreased length of hospital stay. Critically ill patients not receiving EN, bacterial translocation and associated endotoxin release can activate inflammatory pathways and this activation can be a contributory factor in multisystem organ failure. However, it can not be concluded that EN is superior to parental nutrition (PN) in other diseases. In this study the basic principles of EN will be reviewed in detail. INDICATIONS FOR ENTERAL NUTRITION Enteral nutrition is indicated for patients with a functional gastrointestinal tract whose oral nutritional intake is insufficient to meet estimated needs. Various types of enteral feeding can be considered. CONTRAINDICATIONS OF ENTERAL NUTRITION Evaluation of the most appropriate route for nutritional support should take account of the adage " If the gut works, use it ". However, although the enteral route should be the method of choice whore possible, there may be occasions when it is contraindicated. These include: - Absence of intestinal function due to failure, severe inflammation or, in some instances, post operative stasis - Complete intestinal obstruction
Address for correspondence: Dr. Hale AKPINAR Dokuz Eyll University School of Medicine Department of Internal Medicine, Inciralti 35340 Izmir Tel: 0 232 277 77 77 / 3705 E-mail: hale.akbaylar@deu.edu.tr
Basic principles of enteral feeding
187
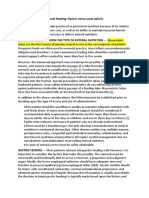
Nasogastric Pharyngostomy Supplementation Sip feeding Oesophagostomy
t
Oral Enteral nutrition
Gastrostomy Nasoduodenal Ext. gastrostomy
Tube feeding
Duodenal Naso jejunal Jejunal Ext. gastrostomy Sur. jejunostomy Direct access Fine needle catheter
Figure 1. Routes for enteral feeding (6)
- Inability to access the gut eg. severe burns - High loss intestinal fistulae - Ethical considerations eg. terminal care. ENTERAL ACCESS Selection of the proper enteral access device is dependent on the patients' gastrointestinal anatomy and function, expected duration of EN and the potential risk of aspiration (Figure 1). The nasoenteric tube is the most commonly used method of enteral access and it can be inserted into the stomach, duodenum or the jejunum. Tubes placed past the third portion of the duodenum, and especially past the ligament of Treitz, are associated with a decreased risk of aspiration. These tubes are indicated for short term use (less than four weeks) and can usually be placed into the gastrointestinal tract at the bedside. After inserting the tube into the stomach, it is allowed to migrate spontaneously into the small bowel. Instead of large-bore nasogastric tubes, small bore feeding tubes made from polyurethane or silicone, in sizes from 6 F to 12 F are more suitable since they are associated with greater tolerance and comfort.
Correct tube placement is confirmed by air insufflation and ascultation, aspiration of gastric and small bowel contents and by X-ray. Prokinetic agents given before the procedure, pH sensors, use of weighted tubes, magnets and bioelectrical detection devices can also facilitate and confirm tube placement. If the blind method fails, fluoroscopic, sonographic and endoscopic guidance can be used to place the tube beyond the pylorus. Their success rate is around 85-95 %. Patients requiring long term (more than four weeks) EN, more permanent access routes should be used. Tube enterostomies (gastrostomy or jejunostomy) are used for long term EN and when obstruction makes nasal intubation impossible, gastrostomy being the most common method for long term access. The insertion of gastric tubes can be performed nonsurgically such as by percutaneous endoscopic gastrostomy (PEG) or fluoroscopic guidance or surgically. Several PEG placement techniques such as pull (Gauderer-Ponsky), push (Sachs-Vine), introducer (Russell), Versa (t-fastener) and primary button method can be used and PEG is more cost effective than surgical placement. Complications related to PEG place-
188
AKBAYLAR et al
ment are variable. Major complications, occurring in 1-4 % of patients, include necrotising fasciitis, buried bumper syndrome, colo-cutaneous fistula, inadvertent PEG tube removal and pulmonary aspiration. The most common minor complications occur in 4-33 % of patients and are peristomal infection and leakage, pneumoperitoneum, temporary ileus, wound bleeding, cutaneous and gastric ulceration, tube clogging and tube dysfunction. A jejunal feeding tube can be placed endoscopically or surgically. One endoscopic method is passing a jejunal feeding tube (J tube) through a preexisting PEG tube (PEG/J). A second endoscopic method of J-tube placement is known as percutaneous endoscopic jejunostomy (PEJ) which involves direct percutaneous endoscopic small bowel puncture. This technique requires specific training and is technique dependent. The small intestine is more difficult to puncture as it tends to be pushed away from the abdominal wall. Success rates with this procedure are 80-90 %. Complications include skin infections, small bowel abscess and wound infections. Surgical techniques for EN are reserved for patients in whom an endoscopy and PEG procedure can not be performed safely such as in tumour obstruction or for patients on whom another surgical procedure will be performed anyway. Surgical techniques can be classified as either permanent or temporary. Temporary surgical enterostomies can also be performed laparoscopically. During major surgery to the upper gastrointestinal tract, the preferred surgical feeding technique is the needle catheter jejunostomy, which can also be done laparoscopically. The advantage of this technique is early enteral nutrition in in the initial 6-12 hours after surgery. Surgical jejunostomy complications are rare and include tube obstruction, wound infection, peritoneal leakage and inadvertent tube removal. EQUIPMENT FOR ENTERAL NUTRITION Feeding tubes: As mentioned above, small bore naso-enteric feeding tubes are usually preferred for patients' comfort. Large bore tubes (14 F-22 F) made from PVC, which are used for gastric drainage, aspiration stomach deflation and are uncomfortable for patients and also cause dilation of the nostrils and throat. Enteral feeding pumps: These are specifically designed pumps which vary in weight and can be
used at the bedside, attached to a drip stand or placed in a carry-sack for patients wishing to be mobile. Pump use instructions should be carefully followed and specific training for users should be given. The pumps should be kept very clean. These pumps can be especially useful in the following circumstances; - If the feed is thick and viscous, - If the feed has to be given on a timed basis - If it is necessary to avoid giving a large volume of feed in a short period of time. Delivery systems: These include a reservoir, which is usually the feeding solutions' container and a giving set. Giving sets may have an optional drug port. When this equipment is used, the following protocol should be used to avoid bacterial contamination risk. - The equipment should never be used on more than one patient. - Giving sets should be changed every 24 hours. - Reservoirs should be used for 24 hours. - Hands should be washed before handling feeds. - Feeds should not be left in the container for longer than the recommended period. - Feeding tubes should be washed regularly. ENTERAL NUTRITION DIETS Home made diets: These diets are still used in some cases if the commercial enteral formulations are not available due to cost and logistics. Home made diets can not be given through small bore enteral feeding tubes because of blockage due to coagulation of proteins and minerals. Bacterial contamination is more likely to be a problem with home made diets than commercial enteral formulas. Commercial enteral formulas: These are divided into four separate groups; polymeric, oligomeric, elemental and special formulas. Polymeric formulas: These are nutritionally complete commercial formulas which contain whole protein as a nitrogen source, oligosaccharides, maltodextrins or starch as a carbohydrate source, vegetable oil as a fat source and minerals, vitamins and trace elements. They require some degree of digestion and absorption. They do not contain lactose, they are palatable and can be
Basic principles of enteral feeding
189
used for oral supplementation (sipping) for enteral tube feeding. They generally have caloric density of 1 kcal/1 mL and are isotonic, but may be concentrated to 1.5- 2 kcal/1 mL. In a standard formulation, 15 to 25 % of the calories are protein, the sources being cow milk (casein, casemate and whey protein), eggs (egg white), soy (soy protein) and wheat (wheat protein, gluten and gliadin). The sources of fat include corn oil, sunflower oil, soybean, butter fat or beef fat. Diets which are enriched with medium chain triglycerides (MCTs) are isolated from coconut oil. In these formulas the main source of carbohydrates is maltodextrin. The content of electrolytes and micronutrients (vitamins and trace elements) is within the range of recommended daily allowances (RDA). Oligomeric formulas: These are designed for use in patients suffering from maldigestion and malabsorption such as Crohn's disease, short bowel syndrome, exocrine pancreatic insufficiency, intestinal fistulas and radiation enteritis. They contain dipeptides, tripeptides and some free amino acids as nitrogen source that can be absorbed via active transport mechanisms without intraluminal hydrolysis. They also contain variable doses of fat in the form of long chain triglycerides and MCTs, carbohydrates, minerals, vitamins and trace elements. Thus they are nutritionally complete and have a lower osmolality than elemental diets. Elemental formulas: These formulas contain amino acids, monosaccharides and disaccharides and variable amounts of fat in the form of MCTs and/or essential fatty acids. They generally have caloric density of 1 kcal/ 1 mL and nitrogen concentration of 6-8 g/1 L. Because of the presence of multiple small particles they are highly osmotic (500-900 mOsm/L) and may therefore cause osmotic diarrhea. They can not be given orally because of their taste. Special formulas: - Modular diets: Most of the commercial enteral formulas are nutritionally complete. In addition to these formulas, there are also feeding modules which provide a single macronutrient. According to the patient's needs, not only the amount of nutrients, but also the type of nutrients can be changed. Carbohydrate, protein and fat modules are present. Indications for modular diets are organ dysfuntions such as renal failure, cardiac failure and acid-base, electrolyte disturbances. Carbohydrate modules are used to increase caloric
density and improve palatability, while protein modules are used to increase nitrogen intake and fat modules are given to increase energy intake and essential fatty acid content in a diet. - Specialized enteral formulas: Organ or disease specific formulas are enteral diets which are designed specifically to meet metabolic abnormalities and altered nutrient requirements according to diseases. Liver formulas: There is an abnormal pattern of circulating amino acids in chronic liver disease; the concentrations of aromatic chain amino acids (ACAA) are increased and branched chain amino acids (BCAA) are decreased. It has been postulated that this imbalance can lead to hepatic encephalopathy by producing false neurotransmitters. Thus BCAA-enriched and ACAA-deficient nutrition supplements have been an extensively utilized nutrition therapy in patients with liver disease. However randomised, controlled trials of the use of these supplements to treat hepatic encephalopathy have shown that they are only indicated in chronic encephalopathy unresponsive to pharmacotherapy. Renal formulas: In acute renal failure(ARF), the primary aim of nutritional therapy is to reduce toxic product accumulation, reduce serum urea nitrogen, and maintain water and electrolyte balance and nutritional status. Patients with ARF who are malnourished or hypercatabolic should receive 1.5 to 1.8 gr of protein/kg per day. In chronic renal failure (CRF), the kidney has a limited ability to excrete urea and electrolytes, which are the major contributors to the renal solute load. The greater the renal solute load, the greater is the obligatory water loss through the kidneys. With increased renal function impairment, there is also an increased obligatory water loss for a given solute load. A number of commercial enteral formulas have been developed for patients with CRF. These formulas, which have a relatively low protein content to limit urea production and a high percentage of essential amino acids to allow for adequate protein synthesis with minimal urea production are preferred in patients with CRF who are not on dialysis. Patients with CRF on hemodialysis and peritoneal dialysis should receive 1.2 to 1.3 g of protein/kg per day. Pulmonary formulas: Because the metabolism of a calorie of carbohydrate produces more CO2 than the metabolism of a calorie of fat, modified carbo-
190
AKBAYLAR et al.
Complications of enteral nutrition
Gastrointestinal (30-38%) Abdominal cramping Abdominal distention Nausea and vomiting Gastroesophageal reflux Diarrhea Malabsorbtion GI bleeding Ileus Figure 2. Complications of enteral nutrition (7)
Mechanical (2-10%) Rhinitis, otitis, parotitis Pharingitis, oesophagitis Pulmonary aspiration Esophageal erosions Tube dislodgement Tube obstruction Perforation
Metabolic and Infectious Ca , Mg, P alterations Fluid-electrolyte disturbances Hyperosmolar states Hyperglycemia, hypoglycemia Microbial contamination Colonisation and invasion
hydrate and fat nutrition formulas have been produced for patients with pulmonary diseases. However the amount of CO2 produced is dependent on the the number of calories consumed, not on the source of the calories. Routine use of these modified formulas is therefore not warranted and energy intake should be kept at or below estimated needs in patients with pulmonary disease and CO2 retention. Immunomodulatory (immune enhancing) formulas: These formulas contain glutamine, arginine, omega-3 fatty acids, nucleotides and BCAA. They are designed to modify the inflammatory response and to enhance resistance to infection by reducing bacterial translocation and enhancing gut associated lymphoid tissue. Gastrointestinal dysfunction formulas: Patients with gastrointestinal disease may benefit from oligomeric formulas. Gut recovery may be accelerated by supplementation of glutamine and fiber, which is a precursor of short chain fatty acids (SCFA). Glutamine and SCFA are metabolic fuels of enterocytes and colonocytes respectively. Diabetes formulas: Most diabetic patients can be managed using standard formulas. However, for long term feeding, the following dietary protocol should be followed: 15 % of calories from protein, 30 % from fat and 55 % from carbohydrates.
- Intermittent: the feed is given over a 24 hour period with intervals of rest (e.g. three hours feeding two hours rest) - Overnight: the feed is given overnight. - Continuous: The feed is given for up to 20 hours without interruption.
Feeds should be administered according to the following guidelines:
- Elevate the head of the patient's bed at least 30 degrees from the horizontal before initiating feeding - Begin a feeding schedule at a rate of 50 ml/hr in adults to promote tolerance. The administration rate of isotonic formulas can usually be increased in 20-25 ml/hr increments every eight hours until the desired rate is achieved. - Flush the tube regularly with 20 to 30 ml of warm water every four hours during continuous feeding and before and after intermittent feeding and medication administration. - Check the gastric residual volume every 4-6 hr routinely. If residual volumes exceed 200 mL on two successive assessments, feeding should be stopped. Gastroesophageal reflux and pulmonary aspiration are potential complications of EN. Significant aspiration can lead to pneumonia and death. Postpyloric placement of feeding tubes should be considered in patients at high risk of aspiration. These risk factors include previous aspiration pneumonia, impaired mental status, neurologic injury, absence of a cough or gag reflex, mechanical ventilation and age.
ADMINISTRATION OF ENTERAL TUBE FEEDING Once the route of feeding has been chosen and the enteral formula identified, feeds can be delivered in the following ways:
- Bolus: a measured amount is given by syringe over an identified time period (usually 30 ml/minute)
Basic principles of enteral feeding
191
The incidence of diarrhea occurs in patients receiving EN is between 21% and 72%. Common causes of diarrhea are medications, underlying illness predisposing to malabsorption and C. difficile
colitis. Tube feeding related causes include enteral feeding formula content, administration technique or contamination of equipments and formula.
REFERENCES
1. Potter J, Langhorne P, Roberts M. Routine protein energy supplementation in adults: systematic review. BMJ 1998; 317: 495. 2. http://www.uptodate.com 3. http://www.medsape.com 4. ASPEN: Board of Directors and The Clinical Guidelines Task Force. Guidelines for the use of parenteral and enteral nutrition in adults and pediatric patients. JPEN 2002; 26(1) (Suppl) 5. Braunshweic C, Levy P, Sheean P, et al. Enteral versus parenteral nutrition. A meta analysis. Am J Clin Nutr 2001; 74: 534-42. 6. Lipman TO. Grains or veins: is enteral nutrition really better than parenteral nutrition? A look at the evidence. JPEN 1998; 22: 167-82. 7. Basics in clinical nutrition. Sobotka L, Allison SP, Frst P, meier R, Pertiewicz M, Soeters P, Stanga Z (eds). 2000, 2nd edition, House of Galen, Prague. 8. Manual of nutritional therapeutics. Alpers DH, Stenson WF, Bier DM (eds). 1995,3rd edition, Little Brown and Company, Boston, pp.281-320. 9. American Gastroenterological Association Technical Review on Tube Feeding for Enteral Nutrition. Gastroenterology 1995; 108: 1282-301.
You might also like
- Gavage, Enteral Feeding or Tube Feeding. Placement May Be Temporary For TheDocument5 pagesGavage, Enteral Feeding or Tube Feeding. Placement May Be Temporary For TheWillen May Delopere Lomarda100% (1)
- Percutaneous Endoscopic Gastroscopy (Peg) : Indications For Peg InsertionDocument3 pagesPercutaneous Endoscopic Gastroscopy (Peg) : Indications For Peg InsertionRicher John PolicarpioNo ratings yet
- Peg & TPNDocument23 pagesPeg & TPNapi-3722454100% (1)
- Enteral Nurtrition Written ReportDocument59 pagesEnteral Nurtrition Written ReportKyle UyNo ratings yet
- Return Residual Fluid To Stomach Via Tube and Proceed To FeedingDocument7 pagesReturn Residual Fluid To Stomach Via Tube and Proceed To FeedingMhae De GuzmanNo ratings yet
- Enteral Feeding: Gastric Versus Post-Pyloric: Table 1Document22 pagesEnteral Feeding: Gastric Versus Post-Pyloric: Table 1tasmeow23No ratings yet
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Gastrostomy and Jejunostomy Feeding Tube CareDocument43 pagesGastrostomy and Jejunostomy Feeding Tube CareLeslie Anne Alcibar TababaNo ratings yet
- Enteral NutritionDocument16 pagesEnteral Nutritionshannon c. lewisNo ratings yet
- Tube FeedingDocument55 pagesTube Feedingrhimineecat71No ratings yet
- Enteral FeedingDocument10 pagesEnteral Feedingkitsilc100% (2)
- Gastrostomy FeedingDocument9 pagesGastrostomy FeedingJovil PajaronNo ratings yet
- Enteral Nutrition Support Assignment 72618Document8 pagesEnteral Nutrition Support Assignment 72618api-341835458100% (1)
- Maintaining Nutritional Status with Enteral FeedingDocument22 pagesMaintaining Nutritional Status with Enteral FeedinganuNo ratings yet
- Access and Complications of Enteral Nutrition Support For Critically Ill PatientsDocument17 pagesAccess and Complications of Enteral Nutrition Support For Critically Ill Patientsribka sinurayaNo ratings yet
- Enteral NutritionDocument74 pagesEnteral NutritionHenno HenoNo ratings yet
- Enteral and Parenteral NutritionDocument7 pagesEnteral and Parenteral Nutritiongembul31No ratings yet
- TPN Care Guide Explains Parenteral NutritionDocument5 pagesTPN Care Guide Explains Parenteral NutritionkhalidicuNo ratings yet
- Enteral and Parenteral NutritionDocument7 pagesEnteral and Parenteral NutritionTimNo ratings yet
- Techniques of Enteral Nutrition PDFDocument18 pagesTechniques of Enteral Nutrition PDFary9quinn9hurtadoNo ratings yet
- NDT LecDocument6 pagesNDT LecV infiresmenNo ratings yet
- Feeding Alternative for Gastrostomy PatientsDocument3 pagesFeeding Alternative for Gastrostomy PatientsAndikaNo ratings yet
- NUTRI LEC CalaraDocument6 pagesNUTRI LEC CalaracalarasheanNo ratings yet
- Fistula Enterokutan 1Document8 pagesFistula Enterokutan 1Amalia GrahaniNo ratings yet
- Fistula Enterokutan 1Document8 pagesFistula Enterokutan 1Amalia GrahaniNo ratings yet
- Medication Administration Through Enteral Feeding Tubes: PrimerDocument11 pagesMedication Administration Through Enteral Feeding Tubes: PrimerAnna Karla Do Nascimento SouzaNo ratings yet
- Nutritional SupportDocument3 pagesNutritional Supportlentini@maltanet.netNo ratings yet
- Esophageal Surgery in Newborns, Infants and Children: and K.L.N. RaoDocument5 pagesEsophageal Surgery in Newborns, Infants and Children: and K.L.N. RaoDonny Artya KesumaNo ratings yet
- Percutaneous Endoscopic GastrostomyDocument27 pagesPercutaneous Endoscopic GastrostomyDoha EbedNo ratings yet
- Early Enteral NutritionDocument55 pagesEarly Enteral NutritionAdya ArradikhaNo ratings yet
- Advanced Medical Nutrition Therapy: Enteral Nutrition InitiationDocument65 pagesAdvanced Medical Nutrition Therapy: Enteral Nutrition InitiationﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞﱞNo ratings yet
- Lecture No 02 Dietetics IIDocument16 pagesLecture No 02 Dietetics IImaryam khanNo ratings yet
- Enteral Nurtrition Written ReportDocument48 pagesEnteral Nurtrition Written Reportleemon.mary.alipao8695No ratings yet
- Clinical Nutrition: Original ArticleDocument7 pagesClinical Nutrition: Original ArticleBby AdelinaNo ratings yet
- Tube FeedingDocument34 pagesTube FeedingHalima IliyasuNo ratings yet
- En - Enteral Nutrition Administration IssuesDocument77 pagesEn - Enteral Nutrition Administration IssuesNers SenNo ratings yet
- TPN Total Parenteral Nutrition Recovered..Document17 pagesTPN Total Parenteral Nutrition Recovered..sakhawatNo ratings yet
- Percutaneus Endoscopic Gatrotomy PDFDocument15 pagesPercutaneus Endoscopic Gatrotomy PDFJosé Moreira Lima NetoNo ratings yet
- Post-Oesophagectomy Early Enteral Nutrition Via A Needle Catheter Jejunostomy: 8-Year Experience at A Specialist UnitDocument8 pagesPost-Oesophagectomy Early Enteral Nutrition Via A Needle Catheter Jejunostomy: 8-Year Experience at A Specialist UnitEssoulaymani FirdawsNo ratings yet
- PDF Document 5Document28 pagesPDF Document 5Kirstin del CarmenNo ratings yet
- Nutritional support through feeding tubesDocument76 pagesNutritional support through feeding tubesKryzza LeizellNo ratings yet
- Enteral Feeding PumpDocument9 pagesEnteral Feeding PumpPrimedeqNo ratings yet
- A Literature Review of Percutaneous Endoscopic Gastrostomy: Dealing With ComplicationsDocument9 pagesA Literature Review of Percutaneous Endoscopic Gastrostomy: Dealing With ComplicationsHenry BarberenaNo ratings yet
- BSG Guideline On The Provision of A Percutaneously Placed Enteral Tube Feeding ServiceDocument14 pagesBSG Guideline On The Provision of A Percutaneously Placed Enteral Tube Feeding ServiceStef AnNo ratings yet
- D02 GASTRIC-LAVAGE NewDocument9 pagesD02 GASTRIC-LAVAGE NewSam TullyNo ratings yet
- Clinical Topic # 5: Gastric Tubes Student GuideDocument3 pagesClinical Topic # 5: Gastric Tubes Student Guidetripj33No ratings yet
- Guide to Drug Therapy in Patients with Enteral Feeding TubesDocument13 pagesGuide to Drug Therapy in Patients with Enteral Feeding TubesCecep Dicki HeriyandiNo ratings yet
- 8 9 FistulasDocument9 pages8 9 FistulascystanarisaNo ratings yet
- 2014 A Tutorial On Enteral Access in Adult Patients in The Hospitalized SttingDocument14 pages2014 A Tutorial On Enteral Access in Adult Patients in The Hospitalized SttingJesus GarciaNo ratings yet
- Post Whipple, Nutrition ManagementDocument9 pagesPost Whipple, Nutrition ManagementHinrich DoradoNo ratings yet
- Esophagostomy Feeding Tubes: Procedures Pro Surgery / Critical CareDocument7 pagesEsophagostomy Feeding Tubes: Procedures Pro Surgery / Critical CareEl OnNo ratings yet
- 8.8) Inpatient Placement and Management of Nasogastric and Nasoenteric Tubes in Adults - UpToDateDocument16 pages8.8) Inpatient Placement and Management of Nasogastric and Nasoenteric Tubes in Adults - UpToDatefedericoNo ratings yet
- Nutrition HealthDocument62 pagesNutrition HealthMiraNo ratings yet
- Nutrients 14 03831Document11 pagesNutrients 14 03831Laura PiastrelliniNo ratings yet
- C 1+ 2 Surgicl Pathology of OesophagusDocument91 pagesC 1+ 2 Surgicl Pathology of OesophagusMerry LeeNo ratings yet
- Tube FeedingDocument47 pagesTube FeedingArlyn Mendenilla0% (1)
- CASE STUDY (Gastro)Document3 pagesCASE STUDY (Gastro)Jake Yvan DizonNo ratings yet
- Oral Nutrition Support NotesDocument28 pagesOral Nutrition Support Notesleemon.mary.alipao8695No ratings yet
- Nutritional Support after Gastrointestinal SurgeryFrom EverandNutritional Support after Gastrointestinal SurgeryDonato Francesco AltomareNo ratings yet
- Colitis: A Practical Approach to Colon and Ileum Biopsy InterpretationFrom EverandColitis: A Practical Approach to Colon and Ileum Biopsy InterpretationAnne Jouret-MourinNo ratings yet