Professional Documents
Culture Documents
Jurnal 1
Uploaded by
Agam ChekmatOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal 1
Uploaded by
Agam ChekmatCopyright:
Available Formats
new england journal of medicine
The
established in 1812
march 29, 2012
vol. 366
no. 13
Brodalumab, an AntiInterleukin-17Receptor Antibody for Psoriasis
Kim A. Papp, M.D., Ph.D., Craig Leonardi, M.D., Alan Menter, M.D., Jean-Paul Ortonne, M.D., James G. Krueger, M.D., Gregory Kricorian, M.D., Girish Aras, Ph.D., Juan Li, Ph.D., Chris B. Russell, Ph.D., Elizabeth H.Z. Thompson, Ph.D., and Scott Baumgartner, M.D.
A bs t r ac t
Background
In this phase 2, randomized, double-blind, placebo-controlled, dose-ranging study, we assessed the efficacy and safety of brodalumab (AMG 827), a human anti interleukin-17receptor monoclonal antibody, for the treatment of moderate-tosevere plaque psoriasis.
Methods
We randomly assigned patients with a score of 12 or higher on the psoriasis area-andseverity index (PASI, on which scores range from 0 to 72, with higher scores indicating more severe disease) and with 10% or more of their body-surface area affected by psoriasis to receive brodalumab (70 mg, 140 mg, or 210 mg at day 1 and weeks 1, 2, 4, 6, 8, and 10 or 280 mg monthly) or placebo. The primary end point was the percentage improvement from baseline in the PASI score at week 12. Secondary end points included improvement of at least 75% and at least 90% in the PASI score and the score on the static physicians global assessment at week 12.
Results
From Probity Medical Research, Waterloo, ON, Canada (K.A.P.); Saint Louis University, St. Louis (C.L.); Baylor University Medical Center, Dallas (A.M.); Hopital de lArchet, Nice, France (J.-P.O.); Rockefeller University, New York (J.G.K.); Amgen, Thousand Oaks, CA (G.K., G.A., J.L., E.H.Z.T., S.B.); and Amgen, Seattle (C.B.R.). Address reprint requests to Dr. Papp at Probity Medical Research, 135 Union St., East Waterloo, ON N2J 1C4, Canada, or at kapapp@probitymedical.com. N Engl J Med 2012;366:1181-9.
Copyright 2012 Massachusetts Medical Society.
A total of 198 patients underwent randomization. At week 12, the mean percentage improvements in the PASI score were 45.0% among patients receiving 70 mg of brodalumab, 85.9% among those receiving 140 mg, 86.3% among those receiving 210 mg, 76.0% among those receiving 280 mg, and 16.0% among those receiving placebo (P<0.001 for all comparisons with placebo). An improvement of at least 75% and at least 90% in the PASI score at week 12 was seen in 77% and 72%, respectively, of the patients in the 140-mg brodalumab group and in 82% and 75%, respectively, of the patients in the 210-mg group, as compared with 0% in the placebo group (P<0.001 for all comparisons). The percentage of patients with a static physicians global assessment of clear or minimal disease was 26%, 85%, 80%, and 69% with the 70-mg, 140-mg, 210-mg, and 280-mg doses, respectively, of brodalumab, as compared with 3% with placebo (P<0.01 for all comparisons with placebo). Two cases of grade 3 neutropenia were reported in the 210-mg brodalumab group. The most commonly reported adverse events in the combined brodalumab groups were nasopharyngitis (8%), upper respiratory tract infection (8%), and injection-site erythema (6%).
Conclusions
Brodalumab significantly improved plaque psoriasis in this 12-week, phase 2 study. (Funded by Amgen; ClinicalTrials.gov number, NCT00975637.)
n engl j med 366;13 nejm.org march 29, 2012
1181
The New England Journal of Medicine Downloaded from nejm.org on October 8, 2012. For personal use only. No other uses without permission. Copyright 2012 Massachusetts Medical Society. All rights reserved.
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
soriasis is a chronic T-cellmediated autoimmune disease1 that affects 2 to 3% of the U.S. population2,3 and 0.6 to 6.5% of the European population.4 Emerging data identify a subset of helper T cells, Th17, that preferentially produce interleukin-17 and play a major role in orchestrating inflammation in psoriasis.5-7 Levels of interleukin-17 are elevated in the lesional skin and blood of patients with psoriasis5,8-10 and correlate with disease severity.11 The interleukin-17 cytokine family consists of six cytokines (interleukins 17A to 17F) and five receptors (interleukins 17RA to 17RE).12 The interleukin 17A, 17F, and 17A/F heterodimer ligands share a common receptor subunit (interleukin17RA) for signaling.12-14 Levels of interleukin 17A, 17C, and 17F messenger RNA (mRNA) are elevated in the lesional skin of patients with psoriasis,15 and levels of interleukin-17Apositive cells are elevated and localized in psoriatic skin lesions.16 The formation of imiquimod-induced skin lesions resembling psoriasis (accompanied by epidermal expression of interleukins 17A, 17F, and 23) is blocked in mice that are deficient in interleukin17RA.17 These data suggest that cytokine-targeting strategies aimed at blocking signaling through interleukin-17RA may be beneficial in the treatment of psoriasis. Brodalumab (AMG 827) is a human, antiinterleukin-17RA monoclonal antibody that antagonizes the interleukin-17 pathway. Brodalumab binds with high affinity to human interleukin-17RA and blocks the biologic activity of interleukins 17A, 17F, 17A/F heterodimer, and 17E (interleukin-25).18,19 Results from a phase 1, proof-of-concept study involving 10 patients with psoriasis showed that a single 700-mg intravenous dose of brodalumab produced substantial improvements in clinical and histopathological variables at 6 weeks.18,19 The main objective of our study was to establish a doseresponse profile for brodalumab and to assess its short-term efficacy and safety in patients with moderate-to-severe plaque psoriasis.
fected by psoriasis, and had a score of 12 or higher on the psoriasis area-and-severity index (PASI, on which scores range from 0 to 72, with higher scores indicating more severe disease20,21). Patients were required to have negative test results for hepatitis B virus surface antigen, hepatitis C virus antibody, the human immunodeficiency virus, and tuberculosis (as assessed with the use of a tuberculin skin test) and could not be pregnant or nursing. Each patient provided written informed consent before participating in the study. Patients with nonplaque or drug-induced psoriasis, a recent serious infection or history of recurrent infections, or a serious concurrent medical illness and patients with an active cancer or a history of cancer, other than in situ cervical or nonmelanoma skin cancers that had been successfully treated, were excluded. Patients who had received systemic therapy, phototherapy, or treatment with biologic agents (other than efalizumab and rituximab) were allowed to participate after specified washout periods. The use of topical therapy during the study was limited to class III to VII glucocorticoids on the scalp, axillae, and groin only; other topical therapies had to be discontinued, and a washout period was required (4 weeks for class I or II glucocorticoids and 2 weeks for all others) before the study drug could be initiated.
Study Design and Oversight
Me thods
Patients
Patients 18 to 70 years of age were eligible for the study if they had had stable plaque psoriasis for at least 6 months, had received or were candidates for phototherapy or systemic psoriasis therapy, had a minimum of 10% of their body-surface area af1182
We conducted a randomized, double-blind, placebo-controlled, dose-ranging study to evaluate the efficacy and safety of brodalumab in patients with moderate-to-severe plaque psoriasis. Patients were randomly assigned to receive placebo or to receive brodalumab, at a dose of 70 mg, 140 mg, or 210 mg, administered subcutaneously on day 1 and at weeks 1, 2, 4, 6, 8, and 10, or at a dose of 280 mg administered subcutaneously on day 1 and at weeks 4 and 8. Patients were enrolled at 23 international sites. Biopsy specimens were obtained from 20 patients before the first dose of study drug was administered and at week 12 for an optional skinbiopsy substudy that was conducted at 7 sites. The study protocol (available with the full text of this article at NEJM.org) was approved by the institutional review board or ethics committee at each participating site. The first patient was enrolled on December 9, 2009, and the enrollment period ended on April 26, 2010. The study was funded by Amgen. Representatives of Amgen, in collaboration with the first
march 29, 2012
n engl j med 366;13
nejm.org
The New England Journal of Medicine Downloaded from nejm.org on October 8, 2012. For personal use only. No other uses without permission. Copyright 2012 Massachusetts Medical Society. All rights reserved.
Brodalumab for Psoriasis
author, designed the study. Amgen conducted the data analyses. All the authors interpreted the data and collaborated in the preparation of the manuscript with support from a professional medical writer funded by Amgen. All the authors made the decision to submit the manuscript for publication and vouch for the completeness and accuracy of the data and analyses and for the fidelity of the study to the protocol.
Efficacy and Safety Evaluations
The primary efficacy evaluation was the percentage improvement in the PASI score at week 12. Secondary efficacy evaluations included the percentages of patients with a 50%, 75%, 90%, and 100% improvement from baseline in the PASI score; the percentage of body-surface area affected by psoriasis (0 to 100%); and the score on the static physicians global assessment, a 6-point scale with scores ranging from 0 (clear, or no apparent disease) to 5 (severe disease). Patient-reported outcomes included the Dermatology Life Quality Index (DLQI, on which scores range from 0 to 30, with lower scores indicating a lesser effect of the disease on healthrelated quality of life22) and the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) physical and mental summary scores (which range from 0 to 100, with higher scores indicating better well-being23). Safety was evaluated by assessing adverse events, serious adverse events, and routine hematologic and laboratory values. The National Cancer Institutes Common Terminology Criteria for Adverse Events, version 4.0, was used to grade the severity of adverse events.24 All patients who remained in the study completed an additional visit at week 16 for efficacy and safety assessments.
Statistical Analysis
was based on the efficacy end point of 75% improvement in the PASI score; we estimated that with a sample size of 35 in each group, the study would have at least 90% power to detect a difference among the groups in this end point, at a 5% level of significance (two-sided test). The primary end point (percentage improvement in the PASI score at 12 weeks) was analyzed by means of an analysis of covariance with the use of a linear trend test, with baseline body-mass index and PASI score as the covariates. Under the order-restricted inference, multiple hypotheses concerning all the doses were tested with the use of a closed testing procedure,25 allowing for the assessment of each comparison at the significance level of 0.025 (one-sided) while still maintaining a family-wise false positive rate at 0.025. The t-statistic was used for comparing various dose levels that were based on ordinal scaling.26 All secondary efficacy end points were summarized, and P values were determined. Safety end points were summarized descriptively. Missing data were handled by means of the baseline-value-carriedforward method or the imputation of no response. We graphed the PASI responses from all patients as a cumulative percentage curve by ordering the responses and plotting the results as a percentage of the population.
R e sult s
Patient Characteristics
The analyses of demographic and baseline characteristics and efficacy end points (except patientreported outcomes) were performed on data from all patients who underwent randomization (full analysis set), according to the intention-to-treat principle. Analyses of safety end points were performed on all patients who underwent randomization and who received at least one dose of a study drug. Patient-reported outcome analyses were performed on data from all patients who underwent randomization and who completed at least one postbaseline assessment. The planned enrollment of 175 patients (about 35 patients in each group)
n engl j med 366;13
A total of 188 of the 198 patients who underwent randomization completed the week 16 study evaluation. The numbers of patients, according to study group, who underwent randomization and completed the follow-up and the reasons for discontinuation in the case of patients who did not complete the week 16 evaluation are provided in Figure 1 in the Supplementary Appendix, available at NEJM .org. The baseline demographic and disease characteristics were similar among the five study groups (Table 1). In the total cohort, 66% of the patients were men, the mean age was 43 years, the mean duration of psoriasis was 19 years, the mean percentage of body-surface area affected by psoriasis was 24%, and the mean PASI score was 19. The percentage of patients with marked or severe psoriasis, as assessed by means of the static physicians global assessment, was 26% in the placebo group and ranged from 36 to 48% in the various brodalumab groups, although other measures of
march 29, 2012
nejm.org
1183
The New England Journal of Medicine Downloaded from nejm.org on October 8, 2012. For personal use only. No other uses without permission. Copyright 2012 Massachusetts Medical Society. All rights reserved.
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
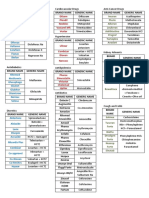
Table 1. Baseline Characteristics of the Patients.* Variable Placebo N = 38) 70 mg (N = 39) Age yr Male sex no. (%) White race no. (%) Weight kg Body-mass index Duration of psoriasis yr Psoriatic arthritis no. (%) Percentage of body-surface area affected PASI score Marked or severe psoriasis on the basis of the static physicians global assessment no. (%)** Prior topical treatment no. (%) Prior phototherapy no. (%) PUVA UVB Prior systemic therapy no. (%) Nonbiologic therapy Methotrexate Oral or intramuscular glucocorticoids Cyclosporine Oral retinoids Biologic therapy Etanercept Adalimumab Ustekinumab DLQI score SF-36 score Physical component Mental component 48.69.8 45.214.5 50.29.4 45.412.8 50.68.2 47.512.8 48.18.9 48.712.6 50.18.5 45.611.4 49.78.7 46.812.3 7 (18) 4 (11) 5 (13) 13.37.0 7 (18) 3 (8) 6 (15) 12.47.2 3 (8) 5 (13) 2 (5) 11.16.7 4 (10) 7 (18) 6 (15) 11.46.4 7 (17) 8 (19) 4 (10) 10.86.6 21 (13) 23 (14) 18 (11) 11.46.7 9 (24) 5 (13) 3 (8) 2 (5) 19 (49) 4 (10) 3 (8) 2 (5) 16 (41) 3 (8) 4 (10) 6 (15) 16 (40) 4 (10) 4 (10) 7 (18) 17 (40) 5 (12) 6 (14) 6 (14) 68 (42) 16 (10) 17 (11) 21 (13) 7 (18) 17 (45) 27 (71) 9 (23) 18 (46) 31 (79) 8 (21) 12 (31) 25 (64) 8 (20) 15 (38) 32 (80) 10 (24) 24 (57) 36 (86) 35 (22) 69 (43) 124 (78) 41.814.4 22 (58) 32 (84) 86.920.6 29.36.8 18.311.5 7 (18) 23.512.8 18.95.9 10 (26) 42.111.1 22 (56) 36 (92) 88.822.0 30.37.1 20.711.8 8 (21) 24.112.8 18.85.7 14 (36) 140 mg (N = 39) 44.011.7 28 (72) 37 (95) 92.423.7 30.87.0 19.29.7 11 (28) 24.916.9 19.48.0 16 (41) Brodalumab 210 mg (N = 40) 42.112.2 25 (62) 34 (85) 90.420.4 29.86.6 17.110.1 12 (30) 25.015.5 20.67.8 19 (48) 280 mg (N = 42) 42.312.2 30 (71) 36 (86) 91.522.9 31.06.3 19.312.4 8 (19) 21.311.0 17.95.5 15 (36) Total (N = 160) 42.611.7 105 (66) 143 (89) 90.822.1 30.56.7 19.111.0 39 (24) 23.814.1 19.26.8 64 (40)
34 (89)
37 (95)
39 (100)
37 (92)
40 (95)
153 (96)
* Plusminus values are means SD. There were no significant differences among the groups with respect to baseline characteristics. PUVA denotes psoralen and ultraviolet A, and UVB ultraviolet B. The 70-, 140-, and 210-mg doses of brodalumab were administered on day 1 and at weeks 1, 2, 4, 6, 8, and 10; the 280-mg dose was administered once a month. Race was self-reported. The body-mass index is the weight in kilograms divided by the square of the height in meters. Patients were included if a diagnosis of psoriatic arthritis was reported in a disease-specific medical history. The psoriasis area-and-severity index (PASI) score (which ranges from 0 to 72, with higher scores indicating more severe disease) is based on the extent of involvement and the degree of erythema, scaling, and induration of psoriatic plaques in four separate body areas (head, trunk, arms, and legs). ** The static physicians global assessment (a 6-point scale, with 0 indicating clear of disease and 5 indicating severe disease) is an assessment by the physician of the patients psoriasis on the basis of the severity of erythema, scaling, and induration. The Dermatology Life Quality Index (DLQI) is a skin-diseasespecific instrument that is scored on a scale from 0 to 30, with higher scores indicating more impairment of quality of life. The Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36), which measures general health status, includes physical and mental component scores. The scores range from 0 to 100, with higher scores indicating better well-being.
1184
n engl j med 366;13
nejm.org
march 29, 2012
The New England Journal of Medicine Downloaded from nejm.org on October 8, 2012. For personal use only. No other uses without permission. Copyright 2012 Massachusetts Medical Society. All rights reserved.
Brodalumab for Psoriasis
disease severity at baseline, including PASI score and percentage of body-surface area affected, were generally similar across the groups. Most of the patients had received prior topical treatments (96% of the patients in the combined brodalumab groups and 90% in the placebo group) and prior systemic therapy (78% in the combined brodalumab groups and 71% in the placebo group) (Table 1). The majority of patients (55%) had received prior phototherapy, and 35% of the patients had received prior biologic therapy. Overall, 92% of the patients in the brodalumab groups and 84% in the placebo group received all the planned doses of the study drug. A total of eight patients used concomitant topical glucocorticoids before the week 12 assessment of the primary end point: seven patients (one in the placebo group, one in the 70-mg brodalumab group, one in the 140-mg brodalumab group, two in the 210-mg brodalumab group, and two in the 280-mg brodalumab group) used various formulations of hydrocortisone cream, and one patient in the 210-mg brodalumab group used a disallowed product (betamethasone dipropionate, which is a class II glucocorticoid).
Efficacy
At week 12, the mean percentage improvement in the PASI score was significantly greater in all the brodalumab groups than in the placebo group (P<0.001) (Fig. 1). The mean improvements in the PASI score were significantly greater in the 140-mg brodalumab group, the 210-mg brodalumab group, and the 280-mg brodalumab group than in the 70-mg brodalumab group (85.9%, 86.3%, and 76.0%, respectively, vs. 45.0%; P<0.001); in addition, the mean improvement in the PASI score was significantly greater in each brodalumab group than in the placebo group (16.0%) (P<0.001). The clinical response was rapid, with improvements relative to placebo observed in all brodalumab groups as early as 2 weeks, which was the time of the first postbaseline efficacy measurement (Fig. 2 and Fig. 3 in the Supplementary Appendix). The mean improvement in the PASI score was similar regardless of whether patients had received prior biologic therapy. The percentages of patients with a 50%, 75%, 90%, or 100% improvement in the PASI score at week 12 were significantly higher among patients who received brodalumab (taking into account all doses) than among patients who received placebo (Table 2). The median percentage improvement in
n engl j med 366;13
the PASI score was 96.3% in the 140-mg brodalumab group, as compared with 11.8% in the placebo group (Fig. 3 in the Supplementary Appendix). Moreover, about 30% of the patients in the placebo group had worsening psoriasis, as shown by negative values for the percentage improvement in the PASI score (Fig. 3 in the Supplementary Appendix). As was the case with the primary end point, the results for the secondary PASI end points of at least 50% and at least 75% improvement in the PASI score were significant at 2 weeks in all brodalumab groups, and substantial improvement was observed for all secondary PASI end points between week 2 and week 4 (data not shown). Patients who received brodalumab, as compared with placebo, also had a significant decrease in the percentage of body-surface area affected by psoriasis (Table 2). Similarly, a significantly higher percentage of patients in the brodalumab groups than in the placebo group were assessed as being clear of psoriasis (score of 0 on the static physicians global assessment) or as having minimal disease (score of 1) at week 12 (Table 2). Scores on the DLQI were significantly lower (indicating a lesser effect of the disease on healthrelated quality of life) in the brodalumab groups than in the placebo group (Table 2). The scores on the physical component of the SF-36 were significantly higher (indicating improved well-being) in the 140-mg brodalumab group than in the placebo group, and scores on the SF-36 mental component were significantly higher in the 140-mg and 210-mg brodalumab groups than in the placebo group; the comparisons between the placebo group and the groups receiving the other doses of brodalumab were not significant. Improvements in skin biomarker measurements were observed in the brodalumab groups (Table 2, and Fig. 4 in the Supplementary Appendix), although the statistical power was limited by the small numbers. Of the 20 pairs of biopsy specimens (obtained before the first dose of study drug was administered and at week 12), 19 could be evaluated by histologic analysis. Keratin 16 (K16) staining of the upper epidermis was reduced in all samples from the 140-mg, 210-mg, and 280-mg groups, with 11 of the 12 samples from these groups having K16 staining confined to the basal keratinocytes at week 12. Epidermal thickness and dermal CD3 counts decreased significantly from baseline in the 140-mg and 210-mg brodalumab groups. Dermal CD3 counts also decreased significantly in the 70-mg brodalumab group, and
march 29, 2012
nejm.org
1185
The New England Journal of Medicine Downloaded from nejm.org on October 8, 2012. For personal use only. No other uses without permission. Copyright 2012 Massachusetts Medical Society. All rights reserved.
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
100
Percentage Improvement in PASI Score
90 80 70 60 50 40 30 20 10 0
0 2 4 6 8 10 12
All P<0.001 vs. placebo and vs. 70-mg dose of brodalumab
P<0.001 vs. placebo 210-mg brodalumab group 140-mg brodalumab group 280-mg brodalumab group 70-mg brodalumab group Placebo group
Week
Figure 1. Percentage Improvement in PASI Scores over Time. The P value for the comparison of the 70-mg dose of brodalumab with placebo (P<0.001) is for all the time points except week 2, for which the P value was 0.002. PASI denotes psoriasis area-and-severity index.
epidermal thickness decreased significantly in the 280-mg group. At the week-16 assessment (6 weeks after the last dose of study drug in the 70-mg, 140-mg, and 210-mg brodalumab groups and 8 weeks after the last dose in the 280-mg group), the mean percentage improvements in the PASI score were 40.2%, 72.0%, 75.5%, and 58.5% in the 70-mg, 140-mg, 210-mg, and 280-mg brodalumab groups, respectively, as compared with 13.5% in the placebo group (P<0.001 for the comparison of all brodalumab groups with the placebo group); these improvements were lower than those observed at week 12. Similarly, the percentages of patients with a 50%, 75%, 90%, or 100% improvement in the PASI score at week 16 (data not shown) in all brodalumab groups were lower than the percentages at week 12 (Table 2). A similar trend was observed with respect to the other secondary efficacy end points and with respect to the patientreported outcomes.
Safety
During the first 12 weeks of the trial, 68% of the patients in the 70-mg brodalumab group, 69% in the 140-mg group, 82% in the 210-mg group, 73% in the 280-mg group, and 62% in the placebo group had at least one adverse event (Table 3). The most commonly reported adverse events were nasopharyngitis, upper respiratory tract infection, arthralgia, and erythema at the injection site (Table 3). The
1186
study drug was discontinued in one patient in the 280-mg brodalumab group, who reported mild urticaria on study day 26. Three serious adverse events were reported during the study: renal colic in one patient in the 70-mg brodalumab group on study day 121, which resolved (with no change in the study-drug regimen) on day 134 after hospitalization and surgical intervention; an ectopic pregnancy in one patient in the placebo group on study day 87, which led to hospitalization and surgical intervention but required no change in the study-drug regimen; and grade 3 asymptomatic neutropenia on study day 16 in one patient in the 210-mg brodalumab group. A second case of grade 3 asymptomatic neutropenia was reported on study day 13 in another patient in the 210-mg group. In the case of both patients with neutropenia, the abnormal laboratory values were seen at the first assessment after initiation of the study drug (week 2) and resolved when the study drug was withheld. The second patient restarted the study drug on day 41, after normalization of the absolute neutrophil count, and grade 3 asymptomatic neutropenia developed again 12 days later (study day 53). The study drug was discontinued, and the patients absolute neutrophil count normalized 17 days later (day 70). The cumulative incidence of brodalumab binding antibodies (in samples obtained at baseline and at weeks 4, 16, and 22) was similar in all the
n engl j med 366;13
nejm.org
march 29, 2012
The New England Journal of Medicine Downloaded from nejm.org on October 8, 2012. For personal use only. No other uses without permission. Copyright 2012 Massachusetts Medical Society. All rights reserved.
Brodalumab for Psoriasis
Table 2. Clinical Responses at Week 12.* Response Placebo (N = 38) 70 mg (N = 39) Improvement in PASI score no. of patients (%) 50% 75% 90% 100% Static physicians global assessment of clear or minimal disease no. (%) Body-surface area affected Mean percentage Mean improvement from baseline percentage points DLQI score SF-36 score Physical component Mental component Skin biomarkers Change from baseline in epidermal thickness m Negative staining for keratin-16 no. of specimens/total no. Change from baseline in dermal CD3 cells/mm 24126 1/4 48190 93246 2/4 16892 4/5 22325 3/3 19588 16277 3/3 18284 50.110.5 46.911.2 51.98.4 47.812.0 54.86.1 51.99.1 52.17.8 53.87.5 52.58.2 50.99.1 22.513.4 0.99.7 10.37.6 14.817.2 6.56.9 3.85.5 2.03.1 3.05.6 2.03.9 5.27.4 3.95.1 9.211.2 21.116.9 22.115.0 16.111.4 6 (16) 0 0 0 1 (3) 20 (51) 13 (33) 7 (18) 4 (10) 10 (26) 35 (90) 30 (77) 28 (72) 15 (38) 33 (85) 36 (90) 33 (82) 30 (75) 25 (62) 32 (80) 34 (81) 28 (67) 24 (57) 12 (29) 29 (69) Brodalumab 140 mg (N = 39) 210 mg (N = 40) 280 mg (N = 42)
304229 201136
* Plusminus values are means SD. P<0.001 for the comparison with placebo. P<0.01 for the comparison with placebo. P<0.05 for the comparison with placebo. Biopsy specimens were obtained from 20 patients at baseline and at week 12 for an optional skin-biopsy substudy at seven sites; 19 pairs could be evaluated by histologic analysis: 4 each in the placebo and 70-mg brodalumab groups, 5 in the 140-mg brodalumab group, and 3 each in the 210-mg and 280-mg brodalumab groups. All available baseline samples stained positive for keratin-16.
brodalumab groups: 7.9%, 7.7%, 5.0%, and 9.8% in the 70-mg, 140-mg, 210-mg, and 280-mg groups, respectively. However, no neutralizing antibodies were detected by bioassay.
Discussion
Increased understanding of the immunopathogenesis of psoriasis has led to the development of multiple biologic drugs targeting specific molecules that are essential for the development of psoriatic plaques.27 Overproduction of interleukins 17A, 17F, and 17A/F induces the expression of proinflammatory cytokines with pathologic consequences, including the proliferation of keratinocytes and inflammation of epithelial cells in psoriasis. Therapies targeting this pathway, including interleukin-17 and interleukin-17R, are currently under investigation for the treatment of
n engl j med 366;13
inflammatory conditions, such as psoriasis and rheumatoid arthritis.19,28-30 Brodalumab, which targets interleukin-17RA, blocks signaling of interleukins 17A and 17F and the interleukin-17A/F heterodimer, all of which play a role in the inflammation of psoriasis. Findings from this study support interleukin17RA as a viable target for the treatment of psoriasis. Patients in the 140-mg and 210-mg brodalumab groups had a mean improvement in the PASI score of about 85% at week 12. Brodalumab, as compared with placebo, was associated with a benefit with respect to the outcomes of 50%, 75%, 90%, and 100% improvement in the PASI score; extent of body-surface area affected; score on the static physicians global assessment; score on the DLQI; and skin biomarker measurements. In 11 of 12 biopsy specimens from patients in the three higher-dose brodalumab groups, the histomarch 29, 2012
nejm.org
1187
The New England Journal of Medicine Downloaded from nejm.org on October 8, 2012. For personal use only. No other uses without permission. Copyright 2012 Massachusetts Medical Society. All rights reserved.
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
Table 3. Adverse Events. Variable Placebo (N = 37) 70 mg (N = 38) Adverse events Any Serious* Leading to withdrawal from study Leading to discontinuation of study drug Grade 3, 4, or 5 Common adverse events Nasopharyngitis Upper respiratory tract infection Arthralgia Injection-site erythema Pain in extremity Nausea 3 (8) 2 (5) 1 (3) 1 (3) 0 1 (3) 6 (16) 3 (8) 1 (3) 1 (3) 1 (3) 4 (11) 1 (3) 3 (8) 2 (5) 1 (3) 0 1 (3) 4 (10) 2 (5) 0 3 (8) 3 (8) 1 (2) 2 (5) 5 (12) 4 (10) 4 (10) 4 (10) 0 13 (8) 13 (8) 7 (4) 9 (6) 8 (5) 6 (4) 23 (62) 1 (3) 0 1 (3) 2 (5) 26 (68) 1 (3) 0 0 1 (3) 27 (69) 0 0 0 1 (3) 33 (82) 1 (2) 0 2 (5) 3 (8) 30 (73) 0 1 (2) 1 (2) 2 (5) 116 (73) 2 (1) 1 (1) 3 (2) 7 (4) 140 mg (N = 39) Brodalumab 210 mg (N = 40) 280 mg (N = 41) Total (N = 158)
number of patients (percent)
* A serious adverse event was defined as an event that was fatal or life threatening, required or prolonged hospitalization, or caused persistent or substantial disability or incapacity or a congenital anomaly or birth defect or an event that was considered by the investigator to be a medically important event. The severity of adverse events was graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0. Common adverse events were those that were reported in at least four patients in any treatment group.
logic and diagnostic features of psoriasis, including T-cell infiltration and suprabasal expression of K16, were no longer seen. This finding indicates a reversal of regenerative epidermal maturation, which is the essential pathological characteristic of psoriasis that causes epidermal hyperplasia and abnormal differentiation, with scaling and thickness as the clinical correlates. Although patients in all the brodalumab groups had significant improvement in efficacy measures as compared with patients in the placebo group, the efficacy results were generally better for patients in the higher-dose groups than for those in the 70-mg group, suggesting that there is a doseresponse effect. Overall, adverse events occurred with greater frequency in the brodalumab groups than in the placebo group. Two cases of grade 3 asymptomatic neutropenia (one of which was a serious adverse event) were reported in the 210-mg brodalumab group. Neutropenia and leukopenia have been observed during treatment with other anti interleukin-17 biologic therapies (monoclonal antibodies to interleukin-17A) in patients with rheu1188
matoid arthritis.28 The exact mechanism for neutropenia is not known; however, in animal models, interleukin-17 is involved in neutrophil homeostasis through granulocyte colony-stimulating factor, and interleukin-17Rdeficient mice have lower levels of neutrophils than do wild-type mice.31,32 This trial was not large enough or of long enough duration to assess the risk of infection or cardiovascular events in the brodalumab groups as compared with the placebo group. In summary, in this phase 2 study, brodalumab showed a high level of efficacy in patients with moderate-to-severe plaque psoriasis, with a rapid onset of action. These findings also support the important role of interleukin-17RA in the pathogenesis of psoriasis.
Supported by Amgen. Dr. Papp reports receiving consulting fees from Abbott, Amgen, Astellas, Celgene, Centocor, Eli Lilly, Galderma, Graceway Pharmaceuticals, Janssen, Johnson & Johnson, Merck, Norvartis, Pfizer, and UCB, lecture fees from Abbott, Amgen, Astellas, Celgene, Centocor, Galderma, Janssen, LEO Pharma, Merck, Novartis, Pfizer, and Stiefel, and grant support from Abbott, Amgen, Astellas, Celgene, Centocor, Eli Lilly, Galderma, GlaxoSmithKline, Graceway Pharmaceuticals, Janssen, Johnson & Johnson, Medimmune, Merck, Novartis, Pfizer, Stiefel, and
n engl j med 366;13
nejm.org
march 29, 2012
The New England Journal of Medicine Downloaded from nejm.org on October 8, 2012. For personal use only. No other uses without permission. Copyright 2012 Massachusetts Medical Society. All rights reserved.
Brodalumab for Psoriasis
UCB; Dr. Leonardi, receiving consulting fees from Abbott, Amgen, Centocor, Eli Lilly, and Pfizer, lecture fees from Abbott and Amgen, and investigator fees from Abbott, Amgen, Celgene, Centocor, Galderma, GlaxoSmithKline, Incyte, Maruho, Novartis, Novo Nordisk, Pfizer, Schering-Plough (now Merck), Sirtris, Stiefel, Vascular Biogenics, and Wyeth (now Pfizer); Dr. Menter, receiving consulting fees from Abbott, Amgen, Astellas, Centocor, Galderma, Genentech, and Wyeth, lecture fees from Abbott, Amgen, Centocor, Galderma, and Wyeth, and fees for expert testimony from Galderma; Dr. Krueger, receiving consulting fees from Centocor, Eli Lilly, and Pfizer and grant support from References
1. Ghoreschi K, Weigert C, Rocken M.
Amgen, Centocor, Eli Lilly, Merck, and Pfizer; and Drs. Krikorian, Aras, Li, Russell, Thompson, and Baumgartner being fulltime employees of Amgen. No other potential conflict of interest was relevant to this article was reported. Disclosure forms provided by the authors are available with the full text of this article at NEJM.org. We thank Rick Davis, M.S., R.Ph., of Complete Healthcare Communications (whose work was funded by Amgen) and Edward Mancini, D.P.M., and Meera Kodukulla, Ph.D., of Amgen for assistance with the writing of the manuscript; and Ryan Athearn of Amgen for assistance with clinical-trial management.
Immunopathogenesis and role of T cells in psoriasis. Clin Dermatol 2007;25:57480. 2. Stern RS, Nijsten T, Feldman SR, Margolis DJ, Rolstad T. Psoriasis is common, carries a substantial burden even when not extensive, and is associated with widespread treatment dissatisfaction. J Investig Dermatol Symp Proc 2004;9:136-9. 3. Kurd SK, Gelfand JM. The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003-2004. J Am Acad Dermatol 2009;60:218-24. [Erratum, J Am Acad Dermatol 2009;61:507.] 4. Chandran V, Raychaudhuri SP. Geoepidemiology and environmental factors of psoriasis and psoriatic arthritis. J Autoimmun 2010;34:J314-J321. 5. Lowes MA, Kikuchi T, Fuentes-Duculan J, et al. Psoriasis vulgaris lesions contain discrete populations of Th1 and Th17 T cells. J Invest Dermatol 2008;128:120711. 6. Miossec P, Korn T, Kuchroo VK. Interleukin-17 and type 17 helper T cells. N Engl J Med 2009;361:888-98. 7. Pne J, Chevalier S, Preisser L, et al. Chronically inflamed human tissues are infiltrated by highly differentiated Th17 lymphocytes. J Immunol 2008;180:742330. 8. Zaba LC, Cardinale I, Gilleaudeau P, et al. Amelioration of epidermal hyperplasia by TNF inhibition is associated with reduced Th17 responses. J Exp Med 2007; 204:3183-94. 9. Kryczek I, Bruce AT, Gudjonsson JE, et al. Induction of IL-17+ T cell trafficking and development by IFN-gamma: mechanism and pathological relevance in psoriasis. J Immunol 2008;181:4733-41. 10. Kagami S, Rizzo HL, Lee JJ, Koguchi Y, Blauvelt A. Circulating Th17, Th22, and Th1 cells are increased in psoriasis. J Invest Dermatol 2010;130:1373-83. 11. Zhang L, Yang XQ, Cheng J, Hui RS, Gao TW. Increased Th17 cells are accom-
panied by FoxP3(+) Treg cell accumulation and correlated with psoriasis disease severity. Clin Immunol 2010;135:108-17. 12. Gaffen SL. Structure and signalling in the IL-17 receptor family. Nat Rev Immunol 2009;9:556-67. [Erratum, Nat Rev Immunol 2009;9:747.] 13. Rickel EA, Siegel LA, Yoon BR, et al. Identification of functional roles for both IL-17RB and IL-17RA in mediating IL-25induced activities. J Immunol 2008;181: 4299-310. 14. Wright JF, Bennett F, Li B, et al. The human IL-17F/IL-17A heterodimeric cytokine signals through the IL-17RA/IL-17RC receptor complex. J Immunol 2008;181: 2799-805. 15. Johansen C, Usher PA, Kjellerup RB, Lundsgaard D, Iversen L, Kragballe K. Characterization of the interleukin-17 isoforms and receptors in lesional psoriatic skin. Br J Dermatol 2009;160:319-24. 16. Harper EG, Guo C, Rizzo H, et al. Th17 cytokines stimulate CCL20 expression in keratinocytes in vitro and in vivo: implications for psoriasis pathogenesis. J Invest Dermatol 2009;129:2175-83. 17. van der Fits L, Mourits S, Voerman JS, et al. Imiquimod-induced psoriasis-like skin inflammation in mice is mediated via the IL-23/IL-17 axis. J Immunol 2009; 182:5836-45. 18. Russell C, Kerkof K, Bigler J, et al. Blockade of the IL-17R with AMG 827 leads to rapid reversal of gene expression and histopathologic abnormalities in psoriatic skin, including substantial pathwayspecific effects within one week. J Invest Dermatol 2011;131:S11. abstract. 19. Russell C, Kerkof K, Bigler J, et al. Blockade of the IL-17R with AMG 827 leads to rapid reversal of gene expression and histopathologic abnormalities in human psoriatic skin. J Invest Dermatol 2010; 130:S46. abstract. 20. Feldman SR, Krueger GG. Psoriasis assessment tools in clinical trials. Ann Rheum Dis 2005;64:Suppl 2:ii65-ii73. 21. Fredriksson T, Pettersson U. Severe
psoriasis oral therapy with a new retinoid. Dermatologica 1978;157:238-44. 22. Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI) a simple practical measure for routine clinical use. Clin Exp Dermatol 1994;19:210-6. 23. Ware J, Kosinski M. SF-36 physical and mental health summary scales: a manual for users of version 1. 2nd ed. Lincoln, RI: QualityMetric, 2001. 24. Common Terminology Criteria for Adverse Events (CTCAE) v4.0. 2011 (http:// ctep.cancer.gov/protocolDevelopment/ electronic_applications/ctc.htm#ctc_40). 25. Marcus R, Peritz E, Gabriel KR. On closed testing procedures with special reference to ordered analysis of variance. Biometrika 1976;63:655-60. 26. Tukey JW, Ciminera JL, Heyse JF. Testing the statistical certainty of a response to increasing doses of a drug. Biometrics 1985;41:295-301. 27. Nestle FO, Kaplan DH, Barker J. Psoriasis. N Engl J Med 2009;361:496-509. 28. Genovese MC, Van den Bosch F, Roberson SA, et al. LY2439821, a humanized anti-interleukin-17 monoclonal antibody, in the treatment of patients with rheumatoid arthritis: a phase I randomized, doubleblind, placebo-controlled, proof-of-concept study. Arthritis Rheum 2010;62:929-39. 29. Hueber W, Patel DD, Dryja T, et al. Effects of AIN457, a fully human antibody to interleukin-17A, on psoriasis, rheumatoid arthritis, and uveitis. Sci Transl Med 2010;2(52):52ra72. 30. Leonardi C, Matheson R, Zachariae C, et al. Antiinterleukin-17 monoclonal antibody ixekizumab in chronic plaque psoriasis. N Engl J Med 2012;366:1190-9. 31. Smith E, Stark MA, Zarbock A, et al. IL-17A inhibits the expansion of IL-17Aproducing T cells in mice through shortloop inhibition via IL-17 receptor. J Immunol 2008;181:1357-64. 32. von Vietinghoff S, Ley K. Homeostatic regulation of blood neutrophil counts. J Immunol 2008;181:5183-8.
Copyright 2012 Massachusetts Medical Society.
n engl j med 366;13
nejm.org
march 29, 2012
1189
The New England Journal of Medicine Downloaded from nejm.org on October 8, 2012. For personal use only. No other uses without permission. Copyright 2012 Massachusetts Medical Society. All rights reserved.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 2016 Sarcopenia in Patients With Chronic Liver Disease PDFDocument7 pages2016 Sarcopenia in Patients With Chronic Liver Disease PDFAgam ChekmatNo ratings yet
- KDIGO Gitelman Conf ReportDocument10 pagesKDIGO Gitelman Conf Reportfelix tanzilNo ratings yet
- EASL Clinical Practice Guidelines for the Management of Hepatocellular CarcinomaDocument55 pagesEASL Clinical Practice Guidelines for the Management of Hepatocellular CarcinomaAgam ChekmatNo ratings yet
- Decompensated Cirrhosis: Clinical Practice GuidelinesDocument96 pagesDecompensated Cirrhosis: Clinical Practice GuidelinesJULIANo ratings yet
- 2016 Sarcopenia From Mechanism To Diagnosis and Treatment in Liver Disease PDFDocument32 pages2016 Sarcopenia From Mechanism To Diagnosis and Treatment in Liver Disease PDFAgam ChekmatNo ratings yet
- 2015 Liver Cirrhosis Nutritional Regimen On Patients Outcome PDFDocument14 pages2015 Liver Cirrhosis Nutritional Regimen On Patients Outcome PDFAgam ChekmatNo ratings yet
- Management of Cirrhosis and Portal Hypertension - 2009Document28 pagesManagement of Cirrhosis and Portal Hypertension - 2009BENNo ratings yet
- 2015 Liver Cirrhosis Nutritional Regimen On Patients Outcome PDFDocument14 pages2015 Liver Cirrhosis Nutritional Regimen On Patients Outcome PDFAgam ChekmatNo ratings yet
- 2015 Sarcopenia in Liver Cirrhosis PDFDocument8 pages2015 Sarcopenia in Liver Cirrhosis PDFAgam ChekmatNo ratings yet
- 2015 Sarcopenia in Non-Alcoholic Fatty Liver Disease PDFDocument7 pages2015 Sarcopenia in Non-Alcoholic Fatty Liver Disease PDFAgam ChekmatNo ratings yet
- 2015 Hepatic Cirrhosis - Disease Burden PDFDocument4 pages2015 Hepatic Cirrhosis - Disease Burden PDFAgam ChekmatNo ratings yet
- 2008 Liver Sirosis PDFDocument14 pages2008 Liver Sirosis PDFAgam ChekmatNo ratings yet
- 2015 Sarcopenia in Non-Alcoholic Fatty Liver Disease PDFDocument7 pages2015 Sarcopenia in Non-Alcoholic Fatty Liver Disease PDFAgam ChekmatNo ratings yet
- 2015 Assessment of Dietary Management of Patients With Cirrhosis Liver PDFDocument7 pages2015 Assessment of Dietary Management of Patients With Cirrhosis Liver PDFAgam ChekmatNo ratings yet
- 2016 Sarcopenia in Patients With Chronic Liver Disease PDFDocument7 pages2016 Sarcopenia in Patients With Chronic Liver Disease PDFAgam ChekmatNo ratings yet
- 2016 Sarcopenia From Mechanism To Diagnosis and Treatment in Liver Disease PDFDocument32 pages2016 Sarcopenia From Mechanism To Diagnosis and Treatment in Liver Disease PDFAgam ChekmatNo ratings yet
- 2015 Hepatic Cirrhosis - Disease Burden PDFDocument4 pages2015 Hepatic Cirrhosis - Disease Burden PDFAgam ChekmatNo ratings yet
- Typhoid FeverDocument38 pagesTyphoid Feverwilliamjhon57100% (1)
- Management of Cirrhosis and Portal Hypertension - 2009Document28 pagesManagement of Cirrhosis and Portal Hypertension - 2009BENNo ratings yet
- 2015 Assessment of Dietary Management of Patients With Cirrhosis Liver PDFDocument7 pages2015 Assessment of Dietary Management of Patients With Cirrhosis Liver PDFAgam ChekmatNo ratings yet
- 2008 Liver Sirosis PDFDocument14 pages2008 Liver Sirosis PDFAgam ChekmatNo ratings yet
- 2015 Sarcopenia in Liver Cirrhosis PDFDocument8 pages2015 Sarcopenia in Liver Cirrhosis PDFAgam ChekmatNo ratings yet
- 2015 Sarcopenia in Non-Alcoholic Fatty Liver Disease PDFDocument7 pages2015 Sarcopenia in Non-Alcoholic Fatty Liver Disease PDFAgam ChekmatNo ratings yet
- 2016 Sarcopenia From Mechanism To Diagnosis and Treatment in Liver Disease PDFDocument32 pages2016 Sarcopenia From Mechanism To Diagnosis and Treatment in Liver Disease PDFAgam ChekmatNo ratings yet
- Buku Pedoman Nasional Penanggulangan TBCDocument131 pagesBuku Pedoman Nasional Penanggulangan TBCHasrapriliana Hersya100% (1)
- 2016 Sarcopenia in Patients With Chronic Liver Disease PDFDocument7 pages2016 Sarcopenia in Patients With Chronic Liver Disease PDFAgam ChekmatNo ratings yet
- WHO Dengue Guidelines 2013Document160 pagesWHO Dengue Guidelines 2013Jason MirasolNo ratings yet
- Nej Mo A 1105594Document11 pagesNej Mo A 1105594Dubi BiduNo ratings yet
- Jurnal 4Document9 pagesJurnal 4Agam ChekmatNo ratings yet
- Hepatite B CoinfeçãoDocument31 pagesHepatite B Coinfeçãojefferson2392No ratings yet
- Ectopic PregnancyDocument50 pagesEctopic PregnancyJose BernelNo ratings yet
- A Randomized Trial of Inhaled Levodopa (CVT-301) For Motor Fluctuations in Parkinson's DiseaseDocument12 pagesA Randomized Trial of Inhaled Levodopa (CVT-301) For Motor Fluctuations in Parkinson's DiseaseFarida AfifahNo ratings yet
- Example of Delivery NoteDocument1 pageExample of Delivery NoteRuDy RaviNo ratings yet
- Intensive Care Ventilator MV200: Safety - Reliability - ComfortDocument7 pagesIntensive Care Ventilator MV200: Safety - Reliability - ComfortFathur ArRahmanNo ratings yet
- Osteosarcoma and Its Variants Compressed PowerpointDocument126 pagesOsteosarcoma and Its Variants Compressed PowerpointSehrish SiddiqueNo ratings yet
- Caie As Level Geography 9696 Core Human Geography v1Document13 pagesCaie As Level Geography 9696 Core Human Geography v1BrizzyNo ratings yet
- Ts 410 420 Product Instruction ManualDocument112 pagesTs 410 420 Product Instruction ManualRosario GonzalesNo ratings yet
- 2020 Eagle Practical CardiologyDocument24 pages2020 Eagle Practical CardiologyaeliasgvNo ratings yet
- Growel Dairy Farming ManualDocument52 pagesGrowel Dairy Farming ManualGrowel Agrovet Private Limited.No ratings yet
- Blood SamplingDocument11 pagesBlood Samplingwiodi nazhofatunnisa umami swNo ratings yet
- Cambridge International AS & A Level: BIOLOGY 9700/21Document20 pagesCambridge International AS & A Level: BIOLOGY 9700/21jamalNo ratings yet
- Documentation On Medicinal Plants Sold I PDFDocument9 pagesDocumentation On Medicinal Plants Sold I PDFGbadeyanka O WuraolaNo ratings yet
- Radionics - Lowe Chronically IllDocument6 pagesRadionics - Lowe Chronically IllE Paty VázquezNo ratings yet
- MMSE Vs MocaDocument3 pagesMMSE Vs MocaIrene Olivia SalimNo ratings yet
- 1 Administering OxygenDocument6 pages1 Administering OxygentlokingNo ratings yet
- Written Report Bio 150Document7 pagesWritten Report Bio 150hyebibieNo ratings yet
- CDC 2017 0019 0010 - ContentDocument156 pagesCDC 2017 0019 0010 - ContentTrey Martin-EllisNo ratings yet
- Colds and Their BenefitsDocument105 pagesColds and Their BenefitsAlmiranteAckbarNo ratings yet
- Thesis Topics in Interventional RadiologyDocument7 pagesThesis Topics in Interventional Radiologygjfcp5jb100% (2)
- Recombinant Dna TechnologyDocument15 pagesRecombinant Dna TechnologyManish kumarNo ratings yet
- Medical Surgical Nursing Exam 1Document23 pagesMedical Surgical Nursing Exam 1Zymer Lee AbasoloNo ratings yet
- Nursing Care Plan - Docx For CVD (Midterm Case Study)Document8 pagesNursing Care Plan - Docx For CVD (Midterm Case Study)Charisma NecesarioNo ratings yet
- Significance of Study-Denguesummer2012Document2 pagesSignificance of Study-Denguesummer2012Mark Remuel Cruz FinezNo ratings yet
- Chest Tube Critical SeminarDocument7 pagesChest Tube Critical SeminarRuqia Al-matrouk100% (1)
- Anembryonic Pregnancy/ Gestation (O02.0)Document137 pagesAnembryonic Pregnancy/ Gestation (O02.0)Marvin Mark AbamongaNo ratings yet
- Medicinal plants guide with uses and preparationsDocument6 pagesMedicinal plants guide with uses and preparationsCaroline Kim100% (1)
- Dispensing DrugsDocument1 pageDispensing DrugsIan CalalangNo ratings yet
- Single Patch Test PDFDocument17 pagesSingle Patch Test PDFmimienamNo ratings yet
- Oral and Maxillo-Facial Surgery Clinic RequirementsDocument7 pagesOral and Maxillo-Facial Surgery Clinic Requirementsal gulNo ratings yet