0% found this document useful (0 votes)
927 views7 pagesBronchiolitis
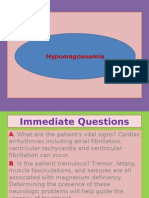
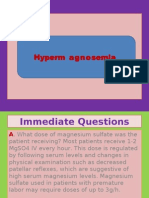
Bronchiolitis is a common lung infection in infants caused by viruses like RSV. It starts with cold-like symptoms and progresses to coughing and wheezing. For most healthy infants, symptoms last about a week. However, premature infants or those with heart/lung conditions may require hospitalization if symptoms are severe like difficulty breathing or blue-colored skin. Doctors diagnose based on symptoms and lung exams. Treatment focuses on relieving symptoms until it resolves on its own.
Uploaded by
Nader SmadiCopyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
927 views7 pagesBronchiolitis
Bronchiolitis is a common lung infection in infants caused by viruses like RSV. It starts with cold-like symptoms and progresses to coughing and wheezing. For most healthy infants, symptoms last about a week. However, premature infants or those with heart/lung conditions may require hospitalization if symptoms are severe like difficulty breathing or blue-colored skin. Doctors diagnose based on symptoms and lung exams. Treatment focuses on relieving symptoms until it resolves on its own.
Uploaded by
Nader SmadiCopyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd