Professional Documents
Culture Documents
Integration Activity 4 2013
Uploaded by
Frankie LiuCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Integration Activity 4 2013
Uploaded by
Frankie LiuCopyright:
Available Formats
Integration Activity 4
March 13, 2013
Group Members: Yap, Vincent Yerro, Jayson Zaragoza, Gian Carlo Garcia, Rowena Liu, Francesca
Questions: 1. What is the most likely diagnosis? The patient presents bilateral parietal throbbing non-radiating headache with PAS 6/10 not associated with nausea and vomiting, a week after, it was observed that the progression of the pain and severity of the headache was persistent with PAS 8/10, with associated with nausea and vomiting. In addition, the patient also experienced sudden onset of stiffening of the right upper extremities with head turning towards the right. Hence, the patient was confused after an episode of stiffening, and could not recall what happened, this shows that the patient has developed neurological deficit. It was also stated that the attacks or episodes has increased 3-4x per day with the same character, we may say that the patient has been having seizures. The patient has a history of working in a slaughterhouse in Masbate. Physical examination showed drowsy, in post-ictal state, papilledema on both fundus, pupils 3mm equally reactive to light, with Dolls eye reflex. The history, symptoms and physical examination stated above, leads us to cysticercosis, which is usually asymptomatic in the acute phase, although rare patients experience cramping, diarrhea, and weight loss. Some patients develop fever and headache during tissue invasion by the larvae; however, most patients do not become symptomatic until 5-7 years after the initial infection. In this case, it affects the central nervous system (CNS) or the eyes, so called Neurocysticercosis. It is the most common parasitic disease of the CNS, affecting thousands of persons living in developing countries and in industrialized nations with large immigrant poplulations grom endemic areas. There are different kinds of neurocysticersosis, which are based on whether or not the disease is symptomatic and on the location of the organisms:
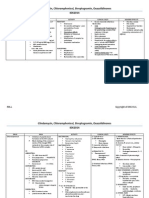
Form of Neurocysticercosis Asymptoatic
Character It has unknown true incidence. Studies from mexico and south America have found that up to 50% of patients with evidence of neurocysticercosis by laboratory testing or neuroimaging are neurologically and systematically asymptomatic. Occurs when cysticerci develop within the brain, predominantly at the junction between the gray and white matter. Patients may develop a variety of neutologic manifestations, particularly seizures, focal
Parenchymal
Subarachnoid
neurologic deficits, and alterations of mental status. Seizures occurs in 35-96% patients; focal seizures are the most common type of symptom There may be motor or sensory depending on the location of the lesion Generalized tonic-clonic (grand mal) seizures are also seen and preceded by focal symptoms May include non-specific symptoms and signs of associated increased ICP also may occur. Neuro-ophthalmologic manifestations include visual hallucnations, homonymous visual field defects, cortical blindness,optic neuropathy papilledema, nystagmus, oculoar motor dysfunction from damage to intrinsic pathways for ocular motro control within the brainstem and cranial neuropathis including ocular motor, trigeminal and facial nerve pareses. Deterioration in mental status, progressive lethargy and coma may occur. Characterized initially by seizures, then meningitis and increased ICP Usually results from obstruction of the basilar cisterns, but may also produced when a cyst obstructs the flow of CSF in the ventricular system May complain of headache, nausea and neck stiffness May experience seizures, papilledema and secondary optic atrophy (result from inc ICP), and cranial neuropathies and hyperfunction of certain cranial nerves
Neurocysticercosis is a preventable parasitic infection caused by larval cysts (enclosed sacs containing the immature stage of a parasite) of the pork tapeworm (Taenia solium). The larval cysts can infect various parts of the body causing a condition known as cysticercosis. Larval cysts in the brain cause a form of cysticercosis called neurocysticercosis which can lead to seizures. Neurocysticercosis, which affects the brain and is the most severe form of the disease, can be fatal. Neurocysticercosis is considered a Neglected Parasitic Infection, one of a group of diseases that results in significant illness among those who are infected and is often poorly understood by health care providers.
2. What are the risk factors for this diagnosis? People are at a higher risk for getting neurocysticercosis by accidentally ingesting parasite eggs if they: Have a pork tapeworm infection (autoinfection) Live in a household with someone who has a pork tapeworm Eat food prepared by someone with a pork tapeworm infection In our patients case, he worked in a slaughterhouse in Masbate, and surely is exposed to swine or pigs that can be the source of Taenia solium eggs and caused the disease. The patient is also a smoker ad alcoholic which contributes to the decrease in immune response which leads to decrease in platelet and leukocyte counts. 3. Explain the pathophysiology of the illness based on your diagnosis. Humans are both definitive and intermediate hosts for Tania solium. They usually become definitive hosts after ingesting portk that is infested with cysticerci (eggs). Eggs hatch in the small intestines, which contain four suckers and two circular rows of hooklets. Where larvae invade mucosa and pass into the blood stream, which then seeds muscles, eyes, and the brain. In these sites, the larvae mature into cysts and remain asymptomatic for an average of 4-5 years. The person develops symptoms as the larvae begin to die, inciting an increased inflammatory response. Symptoms vary depending on the part of the brain infected; intraparenchymal neurocysticercosis (the most common manifestation) results in seizures and focal neurologic deficits. Cysts in the subarachnoid space can collect in the basilar cisterns and induce a chronic basilar meningitis with hydrocephalus. CSF shows a lymphocytic pleocytosis, and hypoglycorrhachia occurs in up to 25% of patients. Cysts can also occur in the ventricles, causing ventriculitis or internal hydrocephalus.
source: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1176337/figure/fig1/ 4. Discuss the patients signs and symptoms. a. The recurring stiffening of the right extremities and head turning The recurring stiffening of the right extremities and head turning may due to a perilesional inflammation caused by a seizure or an episode, or degenerating cysts and probably calcified granulomas. Secondary to neurocysticercosis may be generalized tonic-clonic manifestation to multiple lesions. b. the progressive headache with vomiting headaches may be associated with intracranial hypertension and may be an indicative of hydrocephalus ana may aldo result from meningitis. Chronic headaches may be associated with nausea and vomiting (simulating migraines). c. the papilledema this is primarily due to increased ICP that would lead to compression or entrapment of cranial nerves III, IV, or VI. It may present with visual loss, or disturbances, diplopia or papilledema. Patients with neurocysticercosis of the fourth ventricle may develop the Bruns syndrome with characteristics of a headach, papilledema, and even unconsciousness.
d. the preferential movement of the left extremities hemorrhage can happen may be due to a rupture of mycotic aneurysms of the basilar artery and lead to a stroke, and results to paresis, plegias and involuntary movements, gait disturbances or paresthesias. 5. What are the diagnostic tests available for this case? - Radiographic Studies Diagnostic is suggested by characteristic multiple cystic or calcified lesions detected by head CT scan or MRI in person who has been to an endemic area. Calcification may not be present in early infection. CT o Able to better define calcified lesions but MRI is the modality of choice for the evaluation of intraventricular cysticercosis, brain-stem cysts, and small cysts located over the convexity of the cerebral hemispheres MRI o Has high-contrast resolution that allows the recognition of many forms of cysticercosis not visualized in CT o Accurately defines the number, location, and viability of the parasites in the CNS This is important to individualize therapeutic decisions, including whether to use anti-parasitic drugs, and follow response to therapy. - Biopsy Diagnosis for larval tapeworm form subcutaneous cysts, which may be present in 25% of patients with neurocysticercosis. - Serologic Studies of Serum and CSF Helpful, but negative serology does not rule out neurocysticercosis because serum antibodies are negative in up to 50% of the cases. CSF yield is high (up to 84% positive serology findings) in patients with meningitis and hydrocephalus. CSF ELISA for detection of cysticercal antigens (sensitivity 86%) not only provides a diagnostic tool for viable metacestodes but also may guide drug treatment. Diagnostic criteria for neurocysticercosis have been proposed based on histology, neuroimaging findings, immunologic data, response to treatment, and epidemiologic data. - CSF Findings Shows a lymphocytic pleocytosis Hypoglycorrhachia occurs in up to 25% of patients.
6. What are the complications of the illness? The possible complications of neurocysticersosis depends on severity and its presenting symptoms: Epilepsy Most common presentation of neurocystercosis May be generalized or partial Simple and complex seizures may be associated with the presence of single lesion Generalized seizures are usually tonicclonic (related to multiple lesions) May be associated with intracranial hypertension Indicative of hydrocephalis May also result from meningitis Chronic headaches may be associated with nausea and vomiting (simulating migraines) Due to onstruction of CSF circulation caused by basal or ventricular cysticercosis May also result from large cysts displacing midline structiures, granular ependymitis, arachnoiditis May also result from intracranial hypertension or arachnoiditis producing entrapment or compression of cranial nerve III, IV, or VI. Includes lacunar infarcts and large cerebral infarcts due to occlusion or vascular damage Hemorrhage can also occur and has been reported as a result of mycotic aneurysms of the basilar artery May be responsoible for paresis or plegia, involuntary movements, gait disturbances, paresthesias Can range from poor performance on neuropsychologic tests to severe
Headache
Intracranial hypertension
Diplopia
Strokes
Neuropsychiatric disturbances
Hydrocephalus
dementia Symptoms appear to be related more to the presence of intracranial hypertension than to the number or location of parasites in the brain Develop communicating hydrocephalus due to inflammation and fibrosis of the arachnoid villi or inflammatory reaction to the meninges Noncommunicating hydropcephalus may be consequence of intraventricular cysts
7. Give other differential diagnoses for this case?
Glioblastoma Multiforme
This diagnosis is considered due to the relatively acute onset of symptoms as well as headache, symptoms of increased ICP such as papilledema, nausea and vomiting. Glioblastoma Multiforme is ruled out because etiology of it is often genetic, or a history of head trauma, both of which are absent in this patient. This diagnosis may be considered due to its insidious onset, over several weeks or months. Headache, seizures, nausea, vomiting, lethargy, hemiparesis and papilledema are also presented by the patient. This is ruled out because etiology is often in patients with trauma, and is highly suspect when there is unresolved frontal sinus symptoms, both of which are absent in the patient. This diagnosis is considered because onset is during daytime activity, there is an alteration in consciousness, nausea, vomiting, headaches and
Intracranial Epidural Abscess
Intracranial Hemorrhage
seizures. This diagnosis is ruled out because there is no history of hypertension or trauma to the patient. This may be considered because of the presence of focal neurologic deficits, headaches, seizures, nausea, vomiting and papilledema. This was ruled out because symptoms are usually present for 2 weeks or less. There is also no recent history of infection, skull trauma or surgery to promote spread of the etiologic agent to the brain. Considered because of seizures which is the most common presenting symptom, and headache, symptoms of increased ICP and focal neurological deficits. It is ruled out because there is no genetic history, transient ischemic attacks or intracerebral hemorrhage.
Brain Abscess
Oligodendroglioma
8. Discuss the management for this case. Treatment and management depends upon the viability of the cyst and its complications. Management includes both surgical and medical treatment modalities. a. Medical Management: i. Pharmacologic: 1. Praziquantel and Albendazole as Anti-cysticercal drugs Praziquantel 50-60mg/kg daily in three divided doses for 15-30 days o For the treatment of patients with brain parenchymal cysticerci Albendazole 15 mg/kg per day for 8-28 days 2. Immunosurpressants to alleviate vasculitis, encephalitis and arachnoiditis in cases of live worms. Also, in use for the management of adverse immunologic effects caused
by Anti-cysticercal due the dead worm and hypersensivity due to the parasite. 3. Anticonvulsants and Anti-Epileptic drugs as management on other symptoms caused by the neurologic damage caused by the parasite. ii. Continuous follow-up by imaging after more than 3 months treatment. iii. Occupational and Physical Rehabilitation to recover and preserve intact physical and cognitive abilities. b. Surgical management: i. Surgical Extirpation of live or dead parasites ii. The use of surgical shuts after surgical extirpation to prevent builds up fluids in the body.
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Micro Exam Topics 2012Document1 pageMicro Exam Topics 2012Frankie LiuNo ratings yet
- Integ Activity 2012Document15 pagesInteg Activity 2012Frankie LiuNo ratings yet
- Integration Activity 4 2013Document10 pagesIntegration Activity 4 2013Frankie LiuNo ratings yet
- Evals 11 DiureticsDocument8 pagesEvals 11 DiureticsFrankie LiuNo ratings yet
- Clindamycin, Chloramphenicol, Streptogramin, Oxazolidinones IDK2014Document4 pagesClindamycin, Chloramphenicol, Streptogramin, Oxazolidinones IDK2014Frankie LiuNo ratings yet
- Output 4Document10 pagesOutput 4Frankie LiuNo ratings yet
- Patho Prax DemoDocument37 pagesPatho Prax DemoFrankie LiuNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Healthcare Domain Course MaterialDocument131 pagesHealthcare Domain Course Materialdovesnest_in100% (3)
- Epifisiolisis 4Document66 pagesEpifisiolisis 4Eliana Umba PeñaNo ratings yet
- Career GoalsDocument3 pagesCareer GoalsAnalisa PodgorskiNo ratings yet
- Orientee Evaluation SheetDocument5 pagesOrientee Evaluation Sheetjommelryanclumibao2048No ratings yet
- Chlorpromazine Drug StudyDocument3 pagesChlorpromazine Drug StudyPeyjey100% (1)
- Critical Appraisal of Harm/Association StudiesDocument26 pagesCritical Appraisal of Harm/Association Studiesmirfanjee89No ratings yet
- Guideline Chronic Stable AnginaDocument21 pagesGuideline Chronic Stable AnginarinadillaNo ratings yet
- NuplazidDocument14 pagesNuplazidRaquelNo ratings yet
- Lung Center v. Quezon CityDocument8 pagesLung Center v. Quezon CityMassabielleNo ratings yet
- 09 Lec NotesDocument9 pages09 Lec NotesEvilasio CostaNo ratings yet
- Jewish Standard, September 28, 2018Document52 pagesJewish Standard, September 28, 2018New Jersey Jewish StandardNo ratings yet
- The Health Anxiety Inventory - Development and Validation of Scales For The Measurement of Health Anxiety and Hypochondriasis 2002Document11 pagesThe Health Anxiety Inventory - Development and Validation of Scales For The Measurement of Health Anxiety and Hypochondriasis 2002Catalina NedelciuNo ratings yet
- Marinella Justine L. Payawal: ObjectiveDocument2 pagesMarinella Justine L. Payawal: Objectiveapi-401676443No ratings yet
- Prosthodontics Inroductory Lecture (Lecture #0)Document5 pagesProsthodontics Inroductory Lecture (Lecture #0)JustDen09No ratings yet
- Dental Assistant Practice ExamDocument5 pagesDental Assistant Practice ExamFaye Nervanna Alecha Alferez100% (8)
- Vaginismo EmdrDocument5 pagesVaginismo EmdrGisela Lucía BachNo ratings yet
- Clinical Examination of A Case of ParaplegiaDocument27 pagesClinical Examination of A Case of Paraplegiaswathi bs0% (2)
- Claim Form Word FrontDocument1 pageClaim Form Word FrontRovic MongcalNo ratings yet
- Dental Management of Patient With Leukemia PedoDocument26 pagesDental Management of Patient With Leukemia PedoFourthMolar.comNo ratings yet
- July 2012 Nle Tips-Chn and CDDocument7 pagesJuly 2012 Nle Tips-Chn and CDJerome Asuncion67% (3)
- Chapter 4 Powerpoint: AnxietyDocument45 pagesChapter 4 Powerpoint: AnxietyJoshNo ratings yet
- Hospital and Laboratory Services (Franz's 1st Update)Document7 pagesHospital and Laboratory Services (Franz's 1st Update)Franz CantaraNo ratings yet
- Toy Cleaning Policy GuideDocument11 pagesToy Cleaning Policy GuideVera IndrawatiNo ratings yet
- Female Male Pelvis Anatomy Radiology Student Version PDFDocument66 pagesFemale Male Pelvis Anatomy Radiology Student Version PDFVictoria MaidmanNo ratings yet
- Electrical SafetyDocument68 pagesElectrical SafetyRafaelAndresOspinoNo ratings yet
- Final Human Bone Morphogenetic ProteinDocument23 pagesFinal Human Bone Morphogenetic Proteinbiologicscorp100% (1)
- Dental Assisting Sample TestDocument26 pagesDental Assisting Sample TestFaye Nervanna Alecha Alferez100% (1)
- HyperbilirubinemiaDocument10 pagesHyperbilirubinemiachiboogs456100% (1)
- Consolidated List of Empanelled HospitalsDocument37 pagesConsolidated List of Empanelled HospitalsAdityaKumarNo ratings yet
- Eric Reichenbach Capstone PaperDocument11 pagesEric Reichenbach Capstone Paperapi-318762550No ratings yet