Professional Documents
Culture Documents
Diabetic Maternla
Uploaded by
Ade Gustina SiahaanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diabetic Maternla
Uploaded by
Ade Gustina SiahaanCopyright:
Available Formats
ORIGINAL REPORT
Evaluation of Excessive Pregnancy Weight Gain Effect in Non-Diabetic Women with Normal Pre-Pregnancy BMI on Macrosomia of Neonates
Leila Sekhavat1, Motaharah Golestan2, and Razieh Fallah2
1
Department of Obstetrics & Gynecology, Shaheed Sadoughi Hospital, Shaheed Sadoughi University of Medical Sciences and Health Services, Yazd, Iran Department of Pediateric, Shaheed Sadoughi Hospital, Shaheed Sadoughi University of Medical Sciences and Health Services, Yazd, Iran
Received: 18 Nov. 2009; Received in revised form: 19 May 2010; Accepted: 11 Sep. 2010
Abstract- The objective of this study was evaluation of excessive pregnancy weight gain effect in nondiabetic women with normal pre-pregnancy BMI on macrosomia of neonate. In a descriptive crosssectional study, neonate weighs of all term pregnancy in non-diabetic women with normal pre-pregnancy BMI delivered from 2002 to 2004 in Shaheed Sadoughi Hospital in Yazd, were evaluated. Compared with mothers with normal pregnancy weight gain, the risk of macrosomia in offsprings was significantly elevated in women who had excess weight gain. The odds ratio (OR) was 3.3 (95% confidence interval [CI] = 2.2 5.1, P = 0.0001). Given the complications associated with delivering large babies, women may benefit from not gaining excess weight in pregnancy. 2011 Tehran University of Medical Sciences. All rights reserved. Acta Medica Iranica, 2011; 49(1): 21-24.
Keywords: Weight gain; Diabetes mellitus; Women; Fetal macrosomia
It is already known that excess weight gain during pregnancy may associate with an increased risk of delivering large babies (1). In such deliveries, maternal and neonatal complications such as hemorrhage, infection, preeclampsia, perinatal mortality and rate of cesarean section are higher (1, 2). Although other studies about the effects of high maternal weight and excess weight gain on birth weight of newborns were done (3-6), but most of them focused on diabetic mothers (4, 6, 7) and based on maternal pre-pregnancy body mass index (BMI) (8, 9). Some researchers investigated the impact of maternal weight gain during pregnancy on selected obstetric outcomes, e.g., macrosomia, meconium staining and increased cesarean rate (10-12).Comparison of maternal BMI classes or the effect of gestational weight gain after adjustments for maternal pre-pregnancy BMI were concerned in other studies (5, 11). The influence of the amount of gestational weight gain on neonate birth weight had been less considered.
ch
ive
Introduction
Corresponding Author: Leila Sekhavat
Department of Obstetrics & Gynecology, Shaheed Sadoughi Hospital, Shaheed Sadoughi University of Medical Sciences and Health Services, Yazd, Iran Tel: +98 351 8224001, 913 1525637, Fax: +98 351 8224100, E-mail: sekhavat@ssu.ac.ir
Ar
of
SI
The purpose of the present study was to evaluate effects of excessive pregnancy weight gain in nondiabetic women with normal pre-pregnancy BMI ,on birth weights of their neonates and to answer the question that whether risk of newborn macrosomia is higher in heavier non-diabetic mothers or not.
Patients and Methods
In a descriptive crosssectional study, medical records of all term pregnancy delivered between March 2002 and March 2004 in Shaheed Sadoughi Hospital in Yazd, were reviewed. Variables such as age, educational level , economic condition, number of previous pregnancies , pre-pregnancy weight, height (based on midwife records in first visit at the maternity health care center) and BMI (weight in kilogram/square of height in meter), gestational weight gain, birth weight, sex and gestational age (GA) of her neonate were carefully recorded. Normal BMI (BMI=19.8 to 26) and normal pregnancy weight gain (11.5 to 16 kg), were as defined by the Institute of Medicine (IOM) guidelines
www.SID.ir
Excessive pregnancy weight Gain effect in non-diabetic women
of
N 59 43 14
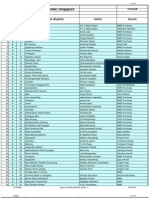
Table1. Frequency of macrosomia of neonate based on maternal and neonatal characteristics
Factor Mother age (year) < 20 20-29 30-40 >40 Poor Meduim Rich Male Female High school and less Bachelor Master and higher 37 38-39 40-42 Nullipara Multipara Total number 125 412 291 112 73 553 314 457 483 81 603 256 67 390 483 510 483 macrosomia 13 47 44 12 6 49 61 65 51 14 65 37 5 67 64 65 51 P value 0.5
Economic condition
ive
SI
OR (CI) % 25.9 9.1 6.1
(13). Gestational age was calculated using the first day of the last normal menstrual period (LMP) and macrosomia defined as a birth weight of 4000 grams (g) or more. Diabetic mothers, multiple pregnancies, under or overweight women (19.8< BMI> 26), preterm (gestational age less than 37 weeks) or post term (GA more than 42 weeks) labors and those with missing midwife data were excluded. The study population consisted of 940 deliveries. In our hospital (Shahid Sedughi hospital) the total delivery number during that period was about 6000. The data were analyzed using SPSS.15 statistical software. Chi-square and t student were used to compare was taken as P < 0.05 was statistical significance. The analyses made were corrected for the effect of gestational age on weight gain by dividing the observed weight gain by a factor that estimated what the weight gain should have been at 40th week of gestation. This factor was estimated for each gestational week (3742) by the quotient between mean gestational weight gain for that week and mean gestational weight gain for
infants born after 40 completed weeks.
Results
Large baby delivery accrued in 11.3% of women. Table 1 shows frequency of macrosomia of neonates based on maternal and neonatal characteristics. Women that delivered in 37th week of gestation, or had poor economic condition, had lowest proportion of macrosomia (7.4%, and 8.2%, respectively), while wealthy mothers had the highest proportion (19.4%). Twenty five percent (237/940) of women had excess weight gain during pregnancy. Table 2 illustrates the risk of macrosomia based on weight gain status and indicates that 25.9% of excess weight gain and 9.1% of normal weight gain women delivered macrosomic babies. The odds ratio (OR) was 3.3 (95% confidence interval [CI] = 2.2 5.1 and P value = 0.0001) for excess weight gain. In the other words, nearly 50% of macrosomic neonates deliveries occurred in excess pregnancy weight gained mothers.
0.03
Maternal education level
ch
Neonate Sex
0.2 0.6
Gestational age(week)
Ar
0.04
Parity
0.269
Table 2. Odds ratios for maternal weight gain in relation to risk of macrosomia
Maternal weight gain Excess Normal Low 22 Macrosomia N 237 473 230 % 25.2 50.3 24.5
3.3 (2.2- 5.1) 0.5 (0.2-1.2) 0.6 (0.3-1.2)
Acta Medica Iranica, Vol. 49, No. 1 (2011)
www.SID.ir
L. Sekhavat, et al.
Discussion
The prevalence of macrosomia has been increasing over the past decade (5, 8). Delivery complications such as perineal laceration, cesarean section, shoulder dystonia, and postpartum hemorrhage are higher in large baby deliveries, which can in turn result in longer hospital stays or even higher perinatal mortality (2, 5, 11) and therefore, it is important to identify predictive factors. In this study, rate of newborn macrosomia increased statistically significant in non-diabetic pregnant women with excess pregnancy weight gain which support other studies (2, 8, 14). In the present study, excess pregnancy weight gained women constituted approximately one forth of population study, but half of macrosomic babies born by these women. While avoidance of excess weight gain before pregnancy is surely advisable, but present study suggests that by avoidance of excess weight gain during the course of pregnancy, the likelihood of delivering a large baby and concomitant complications may be reduced. There are different ways to evaluate the relationship between maternal weight gain and macrosomia. A common way is to limit the study population to one maternal BMI class and evaluate gestational weight gain in relation with macrosomia (7). There are a few earlier studies that were able to show the risk of macrosomia at a specific pre-pregnancy BMI and different amounts of weight gain. Young et al. found an effect of excess weight gain on cesarean delivery rates due to large babies among underweight and normal weight women (11). Maddah et al. found no association between fetal growth or gestation duration and high gestational weight gain among 274 women with normal BMI (15). Contradictory results were recently presented from Iceland, where excess weight gain among average weight women was associated with more delivery of large babies (10). In contrast to our study, Kabali et al. reported macrosomia only in overweight women with excess weight gain, but increased risks of macrosomia for normal weight with excess weight gain, not observed (8). The reason may be that, they combined prepregnancy overweigh and excess weight gain in their study. Though statistically significant increased risk between macrosomia and excess weight gain was identified, it is important to consider study limitations. The dataset used in this analysis was intended for a different purpose and information were not collected on
ive
ch
Ar
of
1. 2. 3. 4. 5. 6.
other important covariates such as paternal height and weight, family history of obesity and birth weight of parents. Therefore, it is not possible to estimate the extent to which these factors could have influenced the results. Further, information was not collected on weight gain within trimester, which might have identified a specific pattern of weight gain that affects fetal growth. Although other studies have shown that retrospective recall of pre-pregnancy weight, weight gain in pregnancy, and birth weight are remarkably accurate (8, 12, 15), in this study, information were collected through postpartum interviews, which may open the opportunity for recall error. It is also worth noting that although BMI is considered as an excellent measure of body composition, it is not perfect and is possible that a small number of women be missed. Its large sample strengthened this study but other researchers are necessary for investigation of factors not considered here. In conclusion, non-diabetic women with normal pre-pregnancy BMI and excess pregnancy weight gain (more than 16 kg) have a greater risk of delivering a macrosomic baby. Given the significant complications associated with delivery of large babies, efforts to prevent excess pregnancy weight gain, may help reduce this problem.
SI
References
Rosenberg TJ, Garbers S, Chavkin W, Chiasson MA. Prepregnancy weight and adverse perinatal outcomes in an ethnically diverse population. Obstet Gynecol 2003;102(5 Pt 1):1022-7. Stotland NE, Hopkins LM, Caughey AB. Gestational weight gain, macrosomia, and risk of cesarean birth in nondiabetic nulliparas. Obstet Gynecol 2004; 104(4):671-7. Yin YZ, Chen XW, Li XM, Hou HY, Zhou SS. Relations of pre-pregnant weight and weight gain during pregnancy with pregnancy-induced hypertension and birth weight. Di Yi Jun Yi Da Xue Xue Bao 2005;25(2):226-8. Vtr M. Risk factors associated with high birthweight deliveries. Ceska Gynekol 2005;70(5):347-54. Bergmann RL, Richter R, Bergmann KE, Plagemann A, Brauer M, Dudenhausen JW. Secular trends in neonatal macrosomia in Berlin: influences of potential determinants. Paediatr Perinat Epidemiol 2003;17(3):2449. Bo S, Menato G, Signorile A, Bardelli C, Lezo A, Gallo ML, Gambino R, Cassader M, Massobrio M, Pagano G. Obesity or diabetes: what is worse for the mother and for the baby? Diabetes Metab 2003;29(2 Pt 1):175-8.
Acta Medica Iranica, Vol. 49, No. 1 (2011)
23
www.SID.ir
Excessive pregnancy weight Gain effect in non-diabetic women 7. Clausen T, Burski TK, yen N, Godang K, Bollerslev J, Henriksen T. Maternal anthropometric and metabolic factors in the first half of pregnancy and risk of neonatal macrosomia in term pregnancies. A prospective study. Eur J Endocrinol 2005;153(6):887-94. 8. Kabali C, Werler MM. Pre-pregnant body mass index, weight gain and the risk of delivering large babies among non-diabetic mothers. Int J Gynaecol Obstet 2007;97(2):100-4. 9. Ehrenberg HM, Durnwald CP, Catalano P, Mercer BM. The influence of obesity and diabetes on the risk of cesarean delivery. Am J Obstet Gynecol 2004;191(3):96974. 10. Thorsdottir I, Torfadottir JE, Birgisdottir BE, Geirsson RT. Weight gain in women of normal weight before pregnancy: complications in pregnancy or delivery and birth outcome. Obstet Gynecol 2002;99(5 Pt 1):799-806. 11. Young TK, Woodmansee B. Factors that are associated with cesarean delivery in a large private practice: the importance of prepregnancy body mass index and weight gain. Am J Obstet Gynecol 2002;187(2):312-8. 12. Cedergren M. Effects of gestational weight gain and body mass index on obstetric outcome in Sweden. Int J Gynaecol Obstet 2006;93(3):269-74. 13. Institute of Medicine. Meeting 2: Impact of Pregnancy Weight on Maternal and Child Health [Online]. 2006 May 2006 [cited 2011 Mar 1]; Available from: URL:http://www.iom.edu/Activities/SelectPops/pregweigh twrkshp/2006-MAY-30.aspx 14. Maddah M, Karandish M, Mohammadpour-Ahranjani B, Neyestani TR, Vafa R, Rashidi A. Social factors and pregnancy weight gain in relation to infant birth weight: a study in public health centers in Rasht, Iran. Eur J Clin Nutr 2005;59(10):1208-12. 15. Catov JM, Newman AB, Kelsey SF, Roberts JM, SuttonTyrrell KC, Garcia M, Ayonayon HN, Tylavsky F, Ness RB. Accuracy and reliability of maternal recall of infant birth weight among older women. Ann Epidemiol 2006;16(6):429-31. 16. Bush A, Alton E, Davies JC, Griesenbach U, Jaffe A, editors. Cystic Fibrosis in the 21st Century. Basel, Karger: Prog Respir Res; 2006. p 264-9.
24
Acta Medica Iranica, Vol. 49, No. 1 (2011)
Ar
ch
ive
of
www.SID.ir
SI
You might also like
- Ocrg So Form 1Document2 pagesOcrg So Form 1Jay Mark Albis Santos73% (84)
- Comments On The Manifestations and Objection To The Motion To Reset Hearing and Video-ConferencingDocument5 pagesComments On The Manifestations and Objection To The Motion To Reset Hearing and Video-ConferencingJaime GonzalesNo ratings yet
- Jurnal ViolenceDocument6 pagesJurnal ViolenceIris BerlianNo ratings yet
- Gestational Weight GainDocument3 pagesGestational Weight GainainindyaNo ratings yet
- Maternal Pregnancy Weight Gain and The Risk of Placental AbruptionDocument9 pagesMaternal Pregnancy Weight Gain and The Risk of Placental AbruptionMuhammad Aulia KurniawanNo ratings yet
- The Effect of Obesity On Pregnancy and Its Outcome in The Population of Oman, Seeb ProvinceDocument12 pagesThe Effect of Obesity On Pregnancy and Its Outcome in The Population of Oman, Seeb ProvinceHazley ZeeNo ratings yet
- Bmi PregnancyDocument11 pagesBmi PregnancyLilik AnggrainiNo ratings yet
- Contribution of Maternal Overweight and Obesity To The Occurrence of Adverse Pregnancy OutcomesDocument8 pagesContribution of Maternal Overweight and Obesity To The Occurrence of Adverse Pregnancy OutcomesMichael ThomasNo ratings yet
- Macrosmia and DMDocument4 pagesMacrosmia and DMAde Gustina SiahaanNo ratings yet
- Macrosomia Risk Factors and Labor Outcome Methal-A. Alrubae, Klood JaferDocument8 pagesMacrosomia Risk Factors and Labor Outcome Methal-A. Alrubae, Klood JaferKhuriyatun NadhifahNo ratings yet
- Research ArticleDocument11 pagesResearch ArticlemalyaNo ratings yet
- 08 AimukhametovaDocument10 pages08 AimukhametovahendraNo ratings yet
- JBR 26 04 235Document6 pagesJBR 26 04 235Khuriyatun NadhifahNo ratings yet
- BMI in PregnancyDocument4 pagesBMI in PregnancyCitra KristiNo ratings yet
- Pregnancy Weight GainDocument9 pagesPregnancy Weight GainKevin MulyaNo ratings yet
- Maternal Obesity, Gestational Hypertension, and Preterm DeliveryDocument8 pagesMaternal Obesity, Gestational Hypertension, and Preterm DeliveryGheavita Chandra DewiNo ratings yet
- Maternal and Perinatal Maternal and Perinatal Outcome of Maternal Obesity Outcome of Maternal Obesity at RSCM in 2014-2019 at RSCM in 2014-2019Document1 pageMaternal and Perinatal Maternal and Perinatal Outcome of Maternal Obesity Outcome of Maternal Obesity at RSCM in 2014-2019 at RSCM in 2014-2019heidi leeNo ratings yet
- Case Write UpDocument5 pagesCase Write UpAisyah Hamdan100% (1)
- Implications of Early Pregnancy Obesity On Maternal, Fetal and Neonatal Health PDFDocument7 pagesImplications of Early Pregnancy Obesity On Maternal, Fetal and Neonatal Health PDFAndhika Dimas ANo ratings yet
- Final Research Paper - Maternal Risks OutcomesDocument12 pagesFinal Research Paper - Maternal Risks Outcomesapi-354198040No ratings yet
- Obesity in Pregnancy - UPTO DATEComplications and Maternal Management - UpToDateDocument43 pagesObesity in Pregnancy - UPTO DATEComplications and Maternal Management - UpToDateCristinaCaprosNo ratings yet
- The Impact of Maternal Body Mass Index On The Phenotype of Pre-Eclampsia: A Prospective Cohort StudyDocument7 pagesThe Impact of Maternal Body Mass Index On The Phenotype of Pre-Eclampsia: A Prospective Cohort StudyAchmad Deza FaristaNo ratings yet
- D'Souza-2019-Maternal Body Mass Index and PregDocument17 pagesD'Souza-2019-Maternal Body Mass Index and PregMARIATUL QIFTIYAHNo ratings yet
- Trabajo Journal 2011Document5 pagesTrabajo Journal 2011Achmad Deza FaristaNo ratings yet
- Pregnancy Exercise Overweight MetaanalysisDocument11 pagesPregnancy Exercise Overweight MetaanalysisAisleenHNo ratings yet
- Fetal Macrosomia : Its Maternal and Neonatal ComplicationsDocument6 pagesFetal Macrosomia : Its Maternal and Neonatal ComplicationsTheresia Herestuwito NaruNo ratings yet
- The Relationship Between Weight Gain in Pregnancy and PreeclampsiaDocument7 pagesThe Relationship Between Weight Gain in Pregnancy and PreeclampsiaDea ameliaNo ratings yet
- Maternal Anthropometry and Low Birth Weight: A Review: G. Devaki and R. ShobhaDocument6 pagesMaternal Anthropometry and Low Birth Weight: A Review: G. Devaki and R. ShobhaJihan PolpokeNo ratings yet
- s12884 022 04542 0Document10 pagess12884 022 04542 0Risma Ripfandiana SariNo ratings yet
- Pre-Existing Diabetes Mellitus and Adverse PDFDocument5 pagesPre-Existing Diabetes Mellitus and Adverse PDFMetebNo ratings yet
- The Interactive Effect of Prepregnancy Overweight/Obesity and Isolated Maternal Hypothyroxinemia On MacrosomiaDocument8 pagesThe Interactive Effect of Prepregnancy Overweight/Obesity and Isolated Maternal Hypothyroxinemia On MacrosomiaAndres GallegosNo ratings yet
- Collares F 2017 HT y ObesityDocument8 pagesCollares F 2017 HT y ObesityYHOISS SMIHT MUNOZ CERONNo ratings yet
- Pregnant Women With Morbid Obesity: Pregnancy and Perinatal OutcomesDocument6 pagesPregnant Women With Morbid Obesity: Pregnancy and Perinatal OutcomesVince Daniel VillalbaNo ratings yet
- First-Trimester Prediction of Gestational Hypertension Through The Bioelectrical Impedance Analysis of The Body CompositionDocument6 pagesFirst-Trimester Prediction of Gestational Hypertension Through The Bioelectrical Impedance Analysis of The Body Compositionppdsobginunsrijan23No ratings yet
- Estimated Global Overweight and Obesity Burden in Pregnant Women Based On Panel Data ModelDocument14 pagesEstimated Global Overweight and Obesity Burden in Pregnant Women Based On Panel Data ModelJoe SoNo ratings yet
- Energy Requirements and Recommended Weight Gain in PregnancyDocument4 pagesEnergy Requirements and Recommended Weight Gain in PregnancyMegaNo ratings yet
- rtcog,+Journal+manager,+Korranat+Thanaratsiriworakul Vol.24 No.3 pp.161-168Document8 pagesrtcog,+Journal+manager,+Korranat+Thanaratsiriworakul Vol.24 No.3 pp.161-168Waode RadmilaNo ratings yet
- Weight: Maternal Body and Pregnancy Outcomel'2Document1 pageWeight: Maternal Body and Pregnancy Outcomel'2Sary ArisazNo ratings yet
- Obesidad y EmbarazoDocument5 pagesObesidad y EmbarazolandabureNo ratings yet
- Maria Grazia Dalfra Weight Gain During Pregnancy ADocument8 pagesMaria Grazia Dalfra Weight Gain During Pregnancy AErick HernandezNo ratings yet
- Gestational Birth Gain Outcomes, InterventionsDocument10 pagesGestational Birth Gain Outcomes, InterventionsAisleenHNo ratings yet
- Fetal Macrosomia UptodateDocument22 pagesFetal Macrosomia UptodateWinny Roman AybarNo ratings yet
- 6 UN Reddy EtalDocument6 pages6 UN Reddy EtaleditorijmrhsNo ratings yet
- Am J Clin Nutr 2000 Abrams 1233S 41SDocument9 pagesAm J Clin Nutr 2000 Abrams 1233S 41SSebastian Ignacio Vega GonzalezNo ratings yet
- Influence of Body Mass Index On The Incidence of Preterm LabourDocument6 pagesInfluence of Body Mass Index On The Incidence of Preterm LabourRizky MuharramNo ratings yet
- 02 003 ValsamakisDocument13 pages02 003 ValsamakisCostin VrabieNo ratings yet
- P ('t':'3', 'I':'668007329') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document5 pagesP ('t':'3', 'I':'668007329') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)niko4eyesNo ratings yet
- Pattern of Glucose Intolerance Among Pregnant Women With Unexplained IUFDDocument5 pagesPattern of Glucose Intolerance Among Pregnant Women With Unexplained IUFDTri UtomoNo ratings yet
- Maternal Obesity, Length of Gestation, Risk of Postdates Pregnancy and Spontaneous Onset of Labour at TermDocument6 pagesMaternal Obesity, Length of Gestation, Risk of Postdates Pregnancy and Spontaneous Onset of Labour at TermEdita Janet Yupanqui FlorianoNo ratings yet
- InformaciónDocument6 pagesInformaciónVIOLETA JACKELINE ARMAS CHAVEZNo ratings yet
- ACOG Committee Opinion On Weight Gain in PregnancyDocument0 pagesACOG Committee Opinion On Weight Gain in PregnancyKevin MulyaNo ratings yet
- Literature Review Obesity in PregnancyDocument6 pagesLiterature Review Obesity in Pregnancyafmzbdjmjocdtm100% (1)
- Risk Factors and Outcomes of Fetal Macrosomia in A Tertiary Centre in Tanzania: A Case-Control StudyDocument8 pagesRisk Factors and Outcomes of Fetal Macrosomia in A Tertiary Centre in Tanzania: A Case-Control StudyMarianella Saravia LopezNo ratings yet
- Effects of Prepregnancy Dietary Patterns On Infant Birth Weight A Prospective Cohort StudyDocument11 pagesEffects of Prepregnancy Dietary Patterns On Infant Birth Weight A Prospective Cohort StudyLola SantiaNo ratings yet
- Factors Associated With Gestational Weight Gain A Cross Sectional SurveyDocument11 pagesFactors Associated With Gestational Weight Gain A Cross Sectional SurveyJosé Zaim Delgado RamírezNo ratings yet
- Exercise in Pregnant Women and Birth WeightDocument4 pagesExercise in Pregnant Women and Birth WeightJelita SihombingNo ratings yet
- ResearchDocument20 pagesResearchtedypsNo ratings yet
- Maternal Obesity Class I-III Gestational Weight GaDocument8 pagesMaternal Obesity Class I-III Gestational Weight GaAbdirahman Yusuf AliNo ratings yet
- Maternal Waist To Hip Ratio Is A Risk Factor For Macrosomia: EpidemiologyDocument7 pagesMaternal Waist To Hip Ratio Is A Risk Factor For Macrosomia: EpidemiologyKhuriyatun NadhifahNo ratings yet
- Gestational Weight Gain Outcomes MetaanalysisDocument19 pagesGestational Weight Gain Outcomes MetaanalysisAisleenHNo ratings yet
- Bjo0118 0578 PDFDocument11 pagesBjo0118 0578 PDFwe sagara dewiNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsFrom EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsNo ratings yet
- Undiagnosed Abdominal Paraganglioma: An Anaesthetic ChallengeDocument3 pagesUndiagnosed Abdominal Paraganglioma: An Anaesthetic ChallengeAde Gustina SiahaanNo ratings yet
- Wilms' Tumour - The BasicsDocument2 pagesWilms' Tumour - The BasicsAde Gustina SiahaanNo ratings yet
- Neuroscience EDocument8 pagesNeuroscience EAde Gustina SiahaanNo ratings yet
- Syok HipovolemikDocument0 pagesSyok HipovolemikAde Gustina SiahaanNo ratings yet
- Neuro Prognosis Post Arrest PDFDocument8 pagesNeuro Prognosis Post Arrest PDFAde Gustina SiahaanNo ratings yet
- Vasoactive DrugsDocument61 pagesVasoactive DrugsAde Gustina SiahaanNo ratings yet
- Neuroscience: Why Study Neuroscience at Bristol?Document6 pagesNeuroscience: Why Study Neuroscience at Bristol?Ade Gustina SiahaanNo ratings yet
- Neonatal PneumoniaDocument8 pagesNeonatal PneumoniaAde Gustina SiahaanNo ratings yet
- Neuroscience EDocument8 pagesNeuroscience EAde Gustina SiahaanNo ratings yet
- NICE Guidelines of Genetic and DementiaDocument56 pagesNICE Guidelines of Genetic and DementiaAde Gustina SiahaanNo ratings yet
- Kista OvariumDocument4 pagesKista OvariumAde Gustina SiahaanNo ratings yet
- Varian Cysts: The Lebanese Society of Obstetrics and GynecologyDocument4 pagesVarian Cysts: The Lebanese Society of Obstetrics and GynecologyAde Gustina SiahaanNo ratings yet
- Kista OvariumDocument5 pagesKista OvariumAde Gustina SiahaanNo ratings yet
- Kista OvariumDocument3 pagesKista OvariumAde Gustina SiahaanNo ratings yet
- Massa OavriumDocument3 pagesMassa OavriumAde Gustina SiahaanNo ratings yet
- Cystic Ovarian Disease: Dairy Integrated Reproductive ManagementDocument4 pagesCystic Ovarian Disease: Dairy Integrated Reproductive ManagementAde Gustina SiahaanNo ratings yet
- Bible EssayDocument3 pagesBible Essayapi-377552614No ratings yet
- Case 8:24-cv-00753-DLB Document 1 Filed 03/13/24 Page 1 of 20Document20 pagesCase 8:24-cv-00753-DLB Document 1 Filed 03/13/24 Page 1 of 20Ryan D.No ratings yet
- Reported SpeechDocument2 pagesReported SpeechJosue HerreraNo ratings yet
- Nintendo Power 001Document114 pagesNintendo Power 001Jonh RiberosNo ratings yet
- Curfew Presentation Final 8 18 20 Item 21.1 and 21.2Document23 pagesCurfew Presentation Final 8 18 20 Item 21.1 and 21.2Erika EsquivelNo ratings yet
- Muawiya Ibn Abi Sufyan 3rd EdDocument174 pagesMuawiya Ibn Abi Sufyan 3rd EdtociphNo ratings yet
- London HistoryDocument18 pagesLondon HistoryСоломія КорольNo ratings yet
- G.R. No. 163705 July 30, 2007 NOMER OCAMPO, Petitioner, People of The Philippines, RespondentDocument7 pagesG.R. No. 163705 July 30, 2007 NOMER OCAMPO, Petitioner, People of The Philippines, RespondentElmer LucreciaNo ratings yet
- Arigo, Et Al VS Swift, Et AlDocument1 pageArigo, Et Al VS Swift, Et AlChristine JungoyNo ratings yet
- (Perez vs. Monetary Board, 20 SCRA 592 (1967) ) PDFDocument6 pages(Perez vs. Monetary Board, 20 SCRA 592 (1967) ) PDFJillian BatacNo ratings yet
- Assignment 1 NegligenceDocument12 pagesAssignment 1 NegligenceKimberly Mwansa MushotaNo ratings yet
- Dr. Ram Manohar Lohia National Law University: Subject:-Intellectual Property Rights-IDocument12 pagesDr. Ram Manohar Lohia National Law University: Subject:-Intellectual Property Rights-IDarpan MaganNo ratings yet
- RavanaDocument8 pagesRavanaArjun UpendraNo ratings yet
- SP - Mam Allien Mar GutibDocument38 pagesSP - Mam Allien Mar Gutibkarl credoNo ratings yet
- RevisionOF Promotion Policy 2007Document43 pagesRevisionOF Promotion Policy 2007Abdul Samad ShaikhNo ratings yet
- United States v. Gilberto Orozco-Rodriguez, 60 F.3d 705, 10th Cir. (1995)Document4 pagesUnited States v. Gilberto Orozco-Rodriguez, 60 F.3d 705, 10th Cir. (1995)Scribd Government DocsNo ratings yet
- 250 GK Questions Second EditionDocument8 pages250 GK Questions Second EditionmimayilpeeliNo ratings yet
- The Role of Political Parties in Political Development of PakistanDocument15 pagesThe Role of Political Parties in Political Development of PakistanBahiNo ratings yet
- (The Yale Cultural Sociology Series) Farhad Khosrokhavar - Inside Jihadism - Understanding Jihadi Movements Worldwide-Routledge (2008)Document342 pages(The Yale Cultural Sociology Series) Farhad Khosrokhavar - Inside Jihadism - Understanding Jihadi Movements Worldwide-Routledge (2008)Faisal MuhammadNo ratings yet
- 1.4 Middle Colonies HistorysageDocument7 pages1.4 Middle Colonies HistorysageDonald KingNo ratings yet
- 7 Years Lukas GrahamDocument2 pages7 Years Lukas Grahamaldo galloNo ratings yet
- Teaching Beginners Latin With Text and Translations 3-TranslationsDocument12 pagesTeaching Beginners Latin With Text and Translations 3-Translationsluyckxj0% (1)
- Saludo, Jr. V CADocument50 pagesSaludo, Jr. V CACathy BelgiraNo ratings yet
- Mmslibrarybooks 13feb09Document37 pagesMmslibrarybooks 13feb091gouNo ratings yet
- Second Division Chico-Nazario, JDocument68 pagesSecond Division Chico-Nazario, JSuzy NaeNo ratings yet
- Roman Polanski (/P Raymond Thierry LieblingDocument36 pagesRoman Polanski (/P Raymond Thierry LieblingFrancisco Mistral Francisco LagardaNo ratings yet
- Third Division G.R. No. 120915. April 3, 1998 THE PEOPLE OF THE PHILIPPINES, Plaintiff-Appellee, Decision Romero, J.Document38 pagesThird Division G.R. No. 120915. April 3, 1998 THE PEOPLE OF THE PHILIPPINES, Plaintiff-Appellee, Decision Romero, J.Leeanji GalamgamNo ratings yet
- Cambridge English Readers Level2 Elementary Logans Choice Lesson PlanDocument4 pagesCambridge English Readers Level2 Elementary Logans Choice Lesson Planpatrix_rNo ratings yet