Professional Documents
Culture Documents
Malignant Lymphoma
Uploaded by
Kakaa KakaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Malignant Lymphoma
Uploaded by
Kakaa KakaCopyright:
Available Formats
Malignant Lymphoma
Print this Page
Updated 7 March 2012
1. Diagnosis and Pathologic Classification
The diagnosis of malignant lymphoma requires the presence of malignant lymphocytes in a biopsy of lymph node or extra-lymphatic tissue. An excisional lymph node biopsy is essential for complete diagnostic assessment. If a whole lymph node is not obtainable, sufficient incised tissue from an extra-lymphatic site can be diagnostic but is less desirable. Fine needle aspiration biopsy (see Appendix I: Biopsy Procedures) is not sufficient for the initial diagnosis of malignant lymphoma. The following histologic sub-classification of the malignant lymphomas is an adaptation of the Working Formulation and the WHO/REAL classification (Jaffe E, Tumours of Hematopoietic and Lymphoid Tissues, World Health Organization Classification of Tumours, IARC Press, 2001) and is based on the light microscopic interpretation complemented by special stains, immunophenotyping, cytogenetics and other information as available. The specific lymphomas are divided into three major groups for treatment planning. Table 3.1 A clinically oriented classification of the lymphomas based on similar natural histories, modes of presentation and responses to treatment using the terminology of the REAL classification scheme: Grade Indolent B-cell Small lymphocytic* Lymphoplasmacytic** Follicular, grade 1, 2 or 3 A Marginal zone MALT*** nodal splenic T-cell Mycoses fungoides
Aggressive Follicular, grade 3 B Mantle cell Diffuse large cell+, any type Burkitt-like (small noncleaved cell)
Peripheral T cell, unspecified Peripheral T-cell, specified Angioimmunoblastic (AIL) Nasal T/NK cell Subcutaneous panniculitic Enteropathy associated Anaplastic large cell (CD30 positive) including null cell Lymphoblastic
Special
Burkitt
* Small lymphocytic lymphoma is biologically similar to chronic lymphocytic leukemia and is treated the same as CLL
** Includes Waldenstroms Macroglobulinemia *** Mucosa-associated lymphoid tissue + Includes primary mediastinal, T-cell rich B-cell, immunoblastic and intravascular variants of diffuse large B-cell lymphoma
2. Staging
The stage of disease is of major therapeutic and prognostic significance in the management of malignant lymphoma. The staging system used at the BC Cancer Agency is based on the Ann Arbor system with additional consideration of the bulk or size of individual tumours. The formal stage is assigned using the following system. Stage Involvement 1 2 3 4 Single lymph node region (1) or one extralymphatic site (1 E). Two or more lymph node regions, same side of the diaphragm (2) or local extralymphatic extension plus one or more lymph node regions same side of the diaphragm (2 E) Lymph node regions on both sides of diaphragm (3) which may be accompanied by local extralymphatic extension (3E) Diffuse involvement of one or more extralymphatic organs or sites
Symptoms A= B= no B symptoms presence of at least one of these: 1) 2) 3) Bulk Bulky = any tumour diameter > 10 cm Non bulky =all tumour diameters < 10 cm For treatment planning purposes patients with malignant lymphoma are divided into two groups by stage: Limited Stage: Stage 1 or Stage 2 confined to 3 or fewer adjacent lymph node regions No B symptoms and Non-bulky tumour (<10 cm) Advanced Stage: unexplained weight loss > 10% baseline during 6 months prior to staging unexplained fever > 38oC/font> night sweats
Stage 2 with disease beyond 3 adjacent lymph node regions or Stage 3 or 4 or B symptoms or Bulky tumour (> 10 cm)
Mandatory Staging Procedures
Pathology review 1. 2. 3. 4. 5. All patients should receive the immunizations recommended in Appendix III Complete history and physical examination including rectal and gynecological examinations Complete blood count Serum creatinine, alkaline phosphatase, LDH, AST (SGOT), bilirubin, protein electrophoresis, calcium Hepatitis B surface antigen (HBs-Ag) and hepatitis B core antibody (HBcoreAb) (positive results should be prominently noted in the patient's chart, usually in the Allergy/Alert section. Anti-viral agents should be given if any systemic anti-lymphoid cancer treatment is given see section 13 under Special Problems) Hepatitis C antibody (positive results should be prominently noted in the patient's chart, usually in the Allergy/Alert section) Human immunodeficiency virus (HIV) antibody Bone marrow aspiration and biopsy Chest radiograph, PA and lateral views CT scan of the abdomen and pelvis PET/CT scan should be performed at staging for patients with curable aggressive nonHodgkin lymphoma, including diffuse large B-cell lymphoma (all types, including primary mediastinal Bcell lymphoma) and peripheral T-cell lymphomas (specified and unspecified). Test
6. 7. 8. 9. 10. 11.
Presentation/ Condition
Primary lymphoma of brain, epidural lymphoma, any lymphoma Cerebrospinal fluid cytology with neurologic abnormalities referable to the brain or spinal cord Primary lymphoma of brain Supra-hyoid cervical lymph node or gastrointestinal tract involvement Waldeyer's ring involvement IgM associated lymphoid cancer including lymphoplasmacytic and other types often referred to as Waldenstroms macroglobulinemia Ophthalmologic examination ENT examination Upper gastrointestinal and small bowel follow-through contrast radiographs Serum viscosity
You might also like
- ESMO Follicular LymphomaDocument11 pagesESMO Follicular LymphomaRonald WiradirnataNo ratings yet
- Ann Oncol-2014-Dreyling-iii83-92 PDFDocument10 pagesAnn Oncol-2014-Dreyling-iii83-92 PDFHessler Hannsen Zambrano CondoriNo ratings yet
- Pediatric Non-Hodgkin Lymphoma Workup - Approach Considerations, Laboratory Studies, Imaging StudiesDocument5 pagesPediatric Non-Hodgkin Lymphoma Workup - Approach Considerations, Laboratory Studies, Imaging StudiestopNo ratings yet
- Bladder CancerFrom EverandBladder CancerJa Hyeon KuNo ratings yet
- Chronic Lymphocytic LeukemiaFrom EverandChronic Lymphocytic LeukemiaMichael HallekNo ratings yet
- Hodgkin Lymphoma KlapperDocument17 pagesHodgkin Lymphoma KlapperAthika RodhyaNo ratings yet
- Advances in Management of NHLDocument34 pagesAdvances in Management of NHLMohammed Abd ElfattahNo ratings yet
- EBM Surgery CWU - Testicular CancerDocument5 pagesEBM Surgery CWU - Testicular CancerFaiz TaqiuNo ratings yet
- Problems in Bone Marrow PathologyDocument29 pagesProblems in Bone Marrow PathologymaurocznNo ratings yet
- Lymphomas of The Head and Neck - Practice Essentials, Background, PathophysiologyDocument6 pagesLymphomas of The Head and Neck - Practice Essentials, Background, Pathophysiologymiranddaelvira02No ratings yet
- Imaging Features of Combined Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma in Patients Undergoing Liver SurgeryDocument19 pagesImaging Features of Combined Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma in Patients Undergoing Liver SurgeryNarakusuma WirawanNo ratings yet
- American J Hematol - 2023 - Cheah-2Document14 pagesAmerican J Hematol - 2023 - Cheah-2salman mehriNo ratings yet
- Gastric Marginal Zone Lymphoma of MALT TypeDocument5 pagesGastric Marginal Zone Lymphoma of MALT TypegiulioNo ratings yet
- Management of Urologic Cancer: Focal Therapy and Tissue PreservationFrom EverandManagement of Urologic Cancer: Focal Therapy and Tissue PreservationNo ratings yet
- Current Status of PET/CT in The Diagnosis and Follow Up of LymphomasDocument8 pagesCurrent Status of PET/CT in The Diagnosis and Follow Up of LymphomassigitNo ratings yet
- Guidelines For The Diagnosis and Treatment of Hepatocellular Carcinoma (HCC) in AdultsDocument13 pagesGuidelines For The Diagnosis and Treatment of Hepatocellular Carcinoma (HCC) in AdultsBlack Hack HakerNo ratings yet
- International Journal of Surgery Case ReportsDocument7 pagesInternational Journal of Surgery Case Reportshussein_faourNo ratings yet
- KT Kanker PayudaraDocument5 pagesKT Kanker PayudaraMayang CendikiaNo ratings yet
- Ann Oncol 2012 Verslype Vii41 8Document8 pagesAnn Oncol 2012 Verslype Vii41 8medusineNo ratings yet
- Malignant Lymphoma: 1. Diagnosis and Pathologic ClassificationDocument3 pagesMalignant Lymphoma: 1. Diagnosis and Pathologic ClassificationohsnapitsleiNo ratings yet
- Thomas Klasifikasi SezaryDocument9 pagesThomas Klasifikasi SezaryPramita SariNo ratings yet
- Hodgkin Lymphoma: ESMODocument11 pagesHodgkin Lymphoma: ESMOBima Saphien AlpanaceaNo ratings yet
- Histology - of - March Criteria PDFDocument21 pagesHistology - of - March Criteria PDFAnonymous edCRfWflqNo ratings yet
- View Media GalleryDocument9 pagesView Media GallerynandaNo ratings yet
- Medicine Seminar Combined-1Document30 pagesMedicine Seminar Combined-1Deepanshu KumarNo ratings yet
- Casereport Open Access: Case ReportsDocument4 pagesCasereport Open Access: Case ReportsRaswijayanti RusliNo ratings yet
- Hepatocellular Carcinoma 2009Document58 pagesHepatocellular Carcinoma 2009ctsakalakisNo ratings yet
- Colorectal Cancer: Section 7Document3 pagesColorectal Cancer: Section 7MANGNo ratings yet
- Advances in LymphomaDocument20 pagesAdvances in LymphomaSaiKrishnaReddySeemalaNo ratings yet
- Slide RTD SymbicortDocument11 pagesSlide RTD SymbicortsigitNo ratings yet
- Lecture 21: End of Lecture 20 and Lecture 21: The Rational Treatment of Cancer Reading: Chapter 15: 778-795 and First Half ofDocument64 pagesLecture 21: End of Lecture 20 and Lecture 21: The Rational Treatment of Cancer Reading: Chapter 15: 778-795 and First Half ofVibhav SinghNo ratings yet
- Neoplasia 6: Dr. Eman Krieshan, M.D. 5-1-2022Document34 pagesNeoplasia 6: Dr. Eman Krieshan, M.D. 5-1-2022MOHA BANATNo ratings yet
- Gestational Trophoblastic Disease IIDocument8 pagesGestational Trophoblastic Disease IIVictor Nugroho WijayaNo ratings yet
- Fast Facts: CAR T-Cell Therapy in Diffuse Large B-Cell Lymphoma: A practical resource for nursesFrom EverandFast Facts: CAR T-Cell Therapy in Diffuse Large B-Cell Lymphoma: A practical resource for nursesNo ratings yet
- Anticancer Therapeutics: From Drug Discovery to Clinical ApplicationsFrom EverandAnticancer Therapeutics: From Drug Discovery to Clinical ApplicationsNo ratings yet
- Cytopathology of the Head and Neck: Ultrasound Guided FNACFrom EverandCytopathology of the Head and Neck: Ultrasound Guided FNACNo ratings yet
- Uncommon Gynecologic CancersFrom EverandUncommon Gynecologic CancersMarcela del CarmenNo ratings yet
- Ann Oncol 2011 Aebi Vi12 24Document13 pagesAnn Oncol 2011 Aebi Vi12 24Yipno Wanhar El MawardiNo ratings yet
- Bridging ChemotherapyDocument4 pagesBridging Chemotherapy49qmzqdpndNo ratings yet
- Non-Hodgkin Lymphoma of The Breast: MD MD MD PHD MDDocument6 pagesNon-Hodgkin Lymphoma of The Breast: MD MD MD PHD MDlPiNGUSlNo ratings yet
- Aggressive LymphomasFrom EverandAggressive LymphomasGeorg LenzNo ratings yet
- CA HepatocelularDocument36 pagesCA HepatocelularLUCIAMELENDEZSNo ratings yet
- Hodgkins Disease Case StudyDocument7 pagesHodgkins Disease Case StudyLyonsGraham100% (1)
- Bladder NCCNDocument17 pagesBladder NCCNJoriza TamayoNo ratings yet
- Treatment Metastatic Ca ColonDocument9 pagesTreatment Metastatic Ca ColonBurhan MinervaNo ratings yet
- Acute Lymphoblastic Leukemia Treatment RegimensDocument14 pagesAcute Lymphoblastic Leukemia Treatment RegimensPrashant PandeyNo ratings yet
- Baudin 2015Document24 pagesBaudin 2015barbara liuva chia policarpoNo ratings yet
- Childhood Malignancies - Hodgkin's LymphomaDocument6 pagesChildhood Malignancies - Hodgkin's Lymphomavictortayor_26105009No ratings yet
- Burkitts Lymphoma 2015 PDFDocument9 pagesBurkitts Lymphoma 2015 PDFAffra CahyoNo ratings yet
- Radical Orchiectomy: Signs and SymptomsDocument4 pagesRadical Orchiectomy: Signs and SymptomsGede Mei PutraNo ratings yet
- Burkit LymphomaDocument9 pagesBurkit LymphomaEva Paula Badillo SantosNo ratings yet
- Oligometastasico PulmonDocument9 pagesOligometastasico PulmonMaria Hernandez MiguelNo ratings yet
- Fast Facts: Managing immune-related Adverse Events in Oncology: Early recognition, prompt intervention, effective managementFrom EverandFast Facts: Managing immune-related Adverse Events in Oncology: Early recognition, prompt intervention, effective managementNo ratings yet
- Understanding Non-Hodgkin Lymphoma. A Guide for Patients, Survivors, and Loved Ones. September 2015From EverandUnderstanding Non-Hodgkin Lymphoma. A Guide for Patients, Survivors, and Loved Ones. September 2015No ratings yet
- Diagnosis & DetectionDocument1 pageDiagnosis & DetectionRj MagalingNo ratings yet
- Howto Companion August2009Document4 pagesHowto Companion August2009lybrakissNo ratings yet
- Peripheral Lymphedema - Ling - 2021Document307 pagesPeripheral Lymphedema - Ling - 2021Fercho MedNo ratings yet
- Fly Detox KitDocument2 pagesFly Detox Kitapi-203993890No ratings yet
- Automated Leukemia Detection by Using Contour Signature MethodDocument8 pagesAutomated Leukemia Detection by Using Contour Signature MethodIJAFRCNo ratings yet
- Injectable Biochip For Sars-CoV-2 DetectionDocument8 pagesInjectable Biochip For Sars-CoV-2 Detectionvojkan73No ratings yet
- Lab 5 Spotters 7Document7 pagesLab 5 Spotters 7madura cNo ratings yet
- Nothing To DoDocument11 pagesNothing To DoDiana Muela MoraNo ratings yet
- Lymphatic SystemDocument44 pagesLymphatic SystemAzizaNo ratings yet
- The Human Circulatory System.Document3 pagesThe Human Circulatory System.CHANON KIATKAWINWONGNo ratings yet
- Assessment Management of Patients With Peripheral Vascular Disorders HypertensionDocument17 pagesAssessment Management of Patients With Peripheral Vascular Disorders HypertensionJhosita Flora LarocoNo ratings yet
- CiullahemaDocument60 pagesCiullahemaMariel AbatayoNo ratings yet
- Copyright © The McGraw-Hill Companies, Inc. Permission Required For ReproductionDocument33 pagesCopyright © The McGraw-Hill Companies, Inc. Permission Required For ReproductionKvaleramNo ratings yet
- Human Anatomy Physiology Laboratory Manual Cat Version 13th EditionDocument62 pagesHuman Anatomy Physiology Laboratory Manual Cat Version 13th Editionnaomi.parker972100% (44)
- HematopoiesisDocument8 pagesHematopoiesisCassandra Grace Labial PaynterNo ratings yet
- Intranet Tdmu Edu Ua Data Kafedra Internal Anatomy Classes SDocument97 pagesIntranet Tdmu Edu Ua Data Kafedra Internal Anatomy Classes SManisanthosh KumarNo ratings yet
- Non HodgkinsDocument2 pagesNon HodgkinstapNo ratings yet
- SPM 4551 2005 Biology k2Document24 pagesSPM 4551 2005 Biology k2pss smk selandarNo ratings yet
- BSc-rguhs Nursing Syllabus-2006Document212 pagesBSc-rguhs Nursing Syllabus-2006Praveen LoniNo ratings yet
- Mammo Sir OjeDocument10 pagesMammo Sir OjeAron JaroNo ratings yet
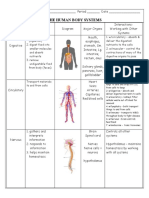
- Body Systems Interactions ChartDocument5 pagesBody Systems Interactions Chartapi-293216402100% (1)
- Biology Form 5 Notes Chapter 1Document39 pagesBiology Form 5 Notes Chapter 1Mayghen SelvanayagamNo ratings yet
- AnatomyDocument286 pagesAnatomyAbbyramy NNo ratings yet
- 2010 KUHS B.SC (N) SyllabusDocument254 pages2010 KUHS B.SC (N) SyllabusJMCON LibraryNo ratings yet
- 100 Mcqs of AnatomyDocument13 pages100 Mcqs of Anatomydrusmansaleem100% (1)
- Anatomy and Physiology: Prelim Laboratory Quiz 1Document35 pagesAnatomy and Physiology: Prelim Laboratory Quiz 1Aubrey Rosales100% (1)
- GNM Nursing SyllabusDocument97 pagesGNM Nursing SyllabusRavi RajanNo ratings yet
- Notes From Dental Articles ANATOMYDocument6 pagesNotes From Dental Articles ANATOMYpatelpurvivNo ratings yet
- Non Hodgkin Lymphoma Complete PDFDocument104 pagesNon Hodgkin Lymphoma Complete PDFelika dwiNo ratings yet
- Tuberculous Lymphadenitis: History PathogenesisDocument6 pagesTuberculous Lymphadenitis: History PathogenesisMochamad BilalNo ratings yet
- Lymphatic SystemsDocument11 pagesLymphatic SystemsMakiato MaureenNo ratings yet
- Introduction To Animal Science An Sci 1Document70 pagesIntroduction To Animal Science An Sci 1princesspuro966No ratings yet