Professional Documents
Culture Documents
Skills of Physical Assessment
Uploaded by
NDJCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Skills of Physical Assessment
Uploaded by
NDJCopyright:
Available Formats
Auscultation (listening to body sounds) is used frequently, most often to assess the heart, lungs, and abdomen.
A stethoscope is required to heat soft sounds, but in some cases, loud sounds, such as those associated with intestinal hyperactivity, are audible with gross hearing (i.e., listening without any instrumentation). It is a technical term for listening to the internal sounds of the body, usually using a stethoscope; based on the Latin verb auscultare "to listen". Auscultation is performed for the purposes of examining the circulatory system and respiratory system (heart sounds and breath sounds), as well as the gastrointestinal system (bowel sounds). Nurses must practice auscultation repeatedly on various healthy and ill people to gain proficiency with the equipment and experience in interpreting data. To ensure the accuracy of findings, it is best to eliminate or reduce environmental noise as much as possible.
Assessment using sense of hearing (auscultation) It is important that a nurse learns to listen effectively, so that not only what a client says is registered but also the tone of voice, which often conveys a great deal. A nurse must also learn how to recognize abnormal sounds. In client care, recognizing abnormal sounds involves the ability to detect: Abnormalities of breathing: for example, respirations that are wheezing, or noisy or distressed Abnormalities of heart sounds, blood pressure, bowel sounds or fetal heart sounds, when using stethoscope Manifestation of a clients distress for example, coughing, expectorating sputum, vomiting, crying or moaning Changes in the sound or rhythm of technical equipment such as suction artificial ventilation apparatus Auscultation is listening with a stethoscope to sounds produced by the body. To auscultate correctly, listen in a quiet environment. To be successful, the nurse must be first able to recognize normal sounds from each body structure, including the passage of blood through artery, heart sounds and movement of air through the lungs.
Assessment using the sense of smell (offaction) A well-developed sense of smell enables a nurse to detect odors that are characteristic of certain conditions. Some alterations in body functions and certain bacteria create characteristic odors, for example: The fishy smell of infected urine The ammonia odor associated with concentrated or decomposed urine The musty or offensive odor of an infected wound The offensive rotting odor associated with gangrene (tissue necrosis) The smell of ketones on the breath of ketoacidosis (accumulation of ketones in the body) The smell of alcohol on the breath due to ingestion of alcohol Halitosis (offensive breath) accompanying mouth infections; for example, gingivitis of certain disorders of the digestive system; for example, appendicitis The foul odor associated with steatorrhea (abnormal amount of fat in the feces) The characteristic odor associated with malaens (abnormal black tarry stool containing blood)
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Gut and Psychology Syndrome (GAPS) - Weston A Price Foundation"Document13 pagesGut and Psychology Syndrome (GAPS) - Weston A Price Foundation"shadhilidarqawi75% (4)
- Aromatherapy - 600 Aromatherapy Recipes For Beauty, Health & Home - Plus Advice & Tips On How To Use Essential Oils - Nodrm PDFDocument365 pagesAromatherapy - 600 Aromatherapy Recipes For Beauty, Health & Home - Plus Advice & Tips On How To Use Essential Oils - Nodrm PDFFernanda Rodriguez75% (4)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Autism Spectrum Disorder Symptoms Improve With Combination Therapy Directed at Improving Gut Microbiota and Reducing InflammationDocument7 pagesAutism Spectrum Disorder Symptoms Improve With Combination Therapy Directed at Improving Gut Microbiota and Reducing InflammationSarah Naomi Jeanett ObenhoferNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Board Exam PrimerDocument9 pagesBoard Exam PrimerEngr Jibril Naval Labiao67% (3)
- Aromatherapy Patient Intake Form-BlankDocument8 pagesAromatherapy Patient Intake Form-Blankapi-282993701100% (2)
- Abdominal AnatomyDocument7 pagesAbdominal Anatomysarguss14100% (2)
- A Study Course in Nutrition by DR Forrest ShakleeDocument89 pagesA Study Course in Nutrition by DR Forrest ShakleeEmpresario100% (1)
- Tips For The Physicians Licenszcdcxure Examination1Document7 pagesTips For The Physicians Licenszcdcxure Examination1filchibuff100% (2)
- Inflammatory Bowel DiseaseDocument42 pagesInflammatory Bowel DiseaseCarmelli Mariae Calugay100% (2)
- Anatomy and Physiology of The Digestive SystemDocument5 pagesAnatomy and Physiology of The Digestive SystemJesrel DelotaNo ratings yet
- Basic Bioethical Principles-2Document81 pagesBasic Bioethical Principles-2NDJNo ratings yet
- Carreograph: Medical Representative TrainingDocument72 pagesCarreograph: Medical Representative Trainingyo100% (1)
- Common Communicable DiseasesDocument86 pagesCommon Communicable DiseasesBenj VillanuevaNo ratings yet
- The Digestive System Powerpoint 1227698045024899 8Document44 pagesThe Digestive System Powerpoint 1227698045024899 8SunnyReduNo ratings yet
- Follow-Up Form: Name: - Age: - SexDocument1 pageFollow-Up Form: Name: - Age: - SexNDJNo ratings yet
- Post Disaster Advice To Prevent Leptospirosis in Children FinalDocument2 pagesPost Disaster Advice To Prevent Leptospirosis in Children FinalTrish Navarro-ParladeNo ratings yet
- Jezreel Deanne D. Nicolas: Characteristics of Hepatitis Viruses Virus HAV HBV HCV HDV HEVDocument1 pageJezreel Deanne D. Nicolas: Characteristics of Hepatitis Viruses Virus HAV HBV HCV HDV HEVNDJNo ratings yet
- PrinDocument7 pagesPrinNDJNo ratings yet
- Be Specific and Use Action Verbs: Science of Success Template For Creating Your Personalized Action PlanDocument2 pagesBe Specific and Use Action Verbs: Science of Success Template For Creating Your Personalized Action Planayman jummaNo ratings yet
- DX: Carry Outs: DX: Carry Outs: DX: Carry OutsDocument2 pagesDX: Carry Outs: DX: Carry Outs: DX: Carry OutsNDJNo ratings yet
- Roles in Client CareDocument11 pagesRoles in Client CareNDJNo ratings yet
- MEDTHERA 3.06 Drugs Used in Thyroid ConditionsDocument28 pagesMEDTHERA 3.06 Drugs Used in Thyroid ConditionsNDJNo ratings yet
- MDV 484Document26 pagesMDV 484NDJNo ratings yet
- HB CodDocument65 pagesHB CodranggadrNo ratings yet
- Study Every Day in Preparation For The Board Exam Start Date Completion Date Who Will I Tell How Will I Measure My SuccessDocument1 pageStudy Every Day in Preparation For The Board Exam Start Date Completion Date Who Will I Tell How Will I Measure My SuccessNDJNo ratings yet
- 01 WorkBookSolutionsDocument16 pages01 WorkBookSolutionsJodie BarasatianNo ratings yet
- Metastatic Renal Cell Carcinoma To The Thyroid 23 Years After NephrectomDocument2 pagesMetastatic Renal Cell Carcinoma To The Thyroid 23 Years After NephrectomNDJNo ratings yet
- 1.01c BP Measurement TakingDocument3 pages1.01c BP Measurement TakingNDJNo ratings yet
- EthicsDocument2 pagesEthicsNDJNo ratings yet
- Ojmm 2013030116424374 PDFDocument6 pagesOjmm 2013030116424374 PDFNDJNo ratings yet
- Core CompetenciesDocument10 pagesCore CompetenciesNDJNo ratings yet
- Quality and NursingDocument6 pagesQuality and NursingNDJNo ratings yet
- Biochem No5Document1 pageBiochem No5NDJNo ratings yet
- Roles in Client CareDocument11 pagesRoles in Client CareNDJNo ratings yet
- ComputerDocument3 pagesComputerNDJNo ratings yet
- Path o PhysiowlogyDocument1 pagePath o PhysiowlogyNDJNo ratings yet
- Teaching Plan - SPEDDocument8 pagesTeaching Plan - SPEDNDJNo ratings yet
- Purpose of EvaluationuDocument7 pagesPurpose of EvaluationuNDJNo ratings yet
- STATISTICAL DATADocument6 pagesSTATISTICAL DATANDJNo ratings yet
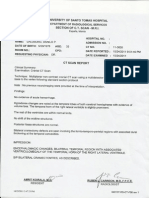
- CT Scan NewDocument1 pageCT Scan NewNDJNo ratings yet
- Multiple Hepatic Nodules and One Bleeding MassDocument2 pagesMultiple Hepatic Nodules and One Bleeding MassNDJNo ratings yet
- Digestion & Absorption-Study Material For NEET (AIPMT) & Medical Exams - askIITiansDocument6 pagesDigestion & Absorption-Study Material For NEET (AIPMT) & Medical Exams - askIITiansKapilNo ratings yet
- Jaycommss Anatomy and Physiology With PathophysiologyDocument91 pagesJaycommss Anatomy and Physiology With PathophysiologyCes GarciaNo ratings yet
- Chronic DiarrheaDocument66 pagesChronic DiarrheaJulita Yanti100% (1)
- Human Body StructureDocument72 pagesHuman Body Structuredeepak dwivedi94% (16)
- The Digestive System Parts and FunctionsDocument6 pagesThe Digestive System Parts and FunctionsDixie MerinNo ratings yet
- 411 ADocument14 pages411 AEjay SalengaNo ratings yet
- Summary Notes - Topic 7 Human Nutrition - CIE Biology IGCSEDocument6 pagesSummary Notes - Topic 7 Human Nutrition - CIE Biology IGCSEdavin gunawanNo ratings yet
- Soal Try Out Test of 12 Grade Code BDocument13 pagesSoal Try Out Test of 12 Grade Code BmarjohanusmanNo ratings yet
- Digestive System ReviewDocument47 pagesDigestive System ReviewMartina RizkiNo ratings yet
- About Human BodyDocument16 pagesAbout Human BodyApril Lavenia BarrientosNo ratings yet
- 2017 Digestive System Study Guide QuestionsDocument8 pages2017 Digestive System Study Guide QuestionsmgarciaNo ratings yet
- High Animal Protein Diet and Gut Microbiota in Human HealthDocument14 pagesHigh Animal Protein Diet and Gut Microbiota in Human HealthAntonio Rodríguez SánchezNo ratings yet
- Practice Paper (4) - 2020-2021Document10 pagesPractice Paper (4) - 2020-2021Sankalp PariharNo ratings yet
- A - Detailed - Lesson - Plan - in - Science - Grade - Rayge DemoDocument6 pagesA - Detailed - Lesson - Plan - in - Science - Grade - Rayge Demoraygelyn apostolNo ratings yet
- مذكرة شرح علوم الصف الرابع الابتدائي لغات 2015 science for primary 4 second term 2015 Prim 4secondTERM2015Document29 pagesمذكرة شرح علوم الصف الرابع الابتدائي لغات 2015 science for primary 4 second term 2015 Prim 4secondTERM2015rabei95% (55)
- Anatomy and Physiology of AbdomenDocument15 pagesAnatomy and Physiology of AbdomenElland Vhyerin LinggeNo ratings yet
- Spice English April 09Document44 pagesSpice English April 09Nishi TaraiNo ratings yet
- Chapter 11 Moyes ANSWERSDocument40 pagesChapter 11 Moyes ANSWERSCaleb DodgeNo ratings yet
- Introduction To Animal Science An Sci 1Document70 pagesIntroduction To Animal Science An Sci 1princesspuro966No ratings yet